Abstract
Gingival recession may present problems that include root sensitivity, esthetic concern, and predilection to root caries, cervical abrasion and compromising of a restorative effort. When marginal tissue health cannot be maintained and recession is deep, the need for treatment arises. This literature has documented that recession can be successfully treated by means of a two stage surgical approach, the first stage consisting of creation of attached gingiva by means of free gingival graft, and in the second stage, a lateral sliding flap of grafted tissue to cover the recession. This indirect technique ensures development of an adequate width of attached gingiva. The outcome of this technique suggests that two stage surgical procedures are highly predictable for root coverage in case of isolated deep recession and lack of attached gingiva.
Keywords: Free soft tissue graft, gingival recession, root coverage
INTRODUCTION
In the current practice of periodontics, clinicians are faced with the challenge of not only addressing biological and functional problems present in the periodontium, but also providing therapy that result in acceptable esthetics. The presence of mucogingival problems and gingival recession around anterior, highly visible teeth exemplifies a situation in which a treatment modality that addresses both biological and esthetic demands is required from the therapist.[1]
Over the years, numerous surgical techniques have been introduced to correct labial gingival recession defect. Esthetic concerns are usually the reason to perform these procedures. Clinical studies have evaluated many of the techniques. The depths of the defects have been measured before surgery and at a follow-up examination after 6 months or later. Results in terms of mid surface root coverage have been expressed in millimeters and as the percentage of original defect that has been covered. Defects with complete coverage have also been reported.[2]
Gingival recession associated with root surface exposure is a complex phenomenon that may present numerous therapeutic challenges to the clinician. Recession may be accompanied by root caries or abraded surfaces, and patients may complain of esthetic defects or root hypersensitivity.
During the past decade, a variety of regenerative procedures with the potential to correct gingival recession defects via augmentation of the width and height of keratinized or attached gingiva as well as to obtain partial or complete root coverage have been proposed. Presence of gingival recession and gingival inflammation in areas with absence of, or narrow band of attached gingiva is identified as a mucogingival problem.[3] The choice of the technique depends on the defect size, localization in esthetic zone, and the need for augmentation of attached gingiva.
Free soft tissue graft followed by lateral sliding flap is preferred to increase the gingival height for root coverage of isolated deep and narrow recessions with inadequate width of attached gingiva.
CASE REPORT
A 27-year-old female patient reported to the department of periodontics with a chief complaint of tooth sensitivity and exposure of root surface in relation to lower front tooth.
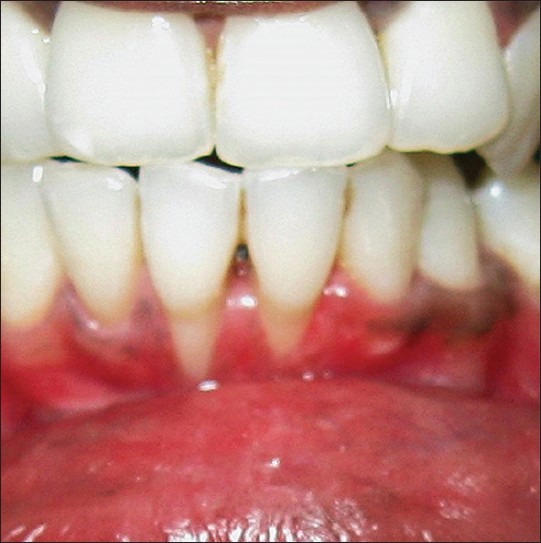
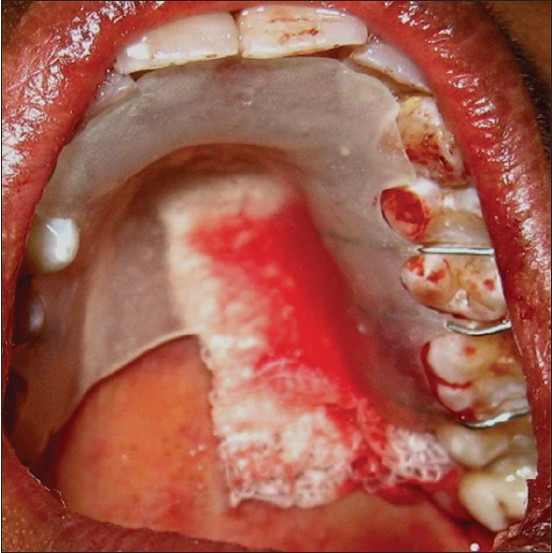
On examination, her oral hygiene status was fair and in the lower right central incisor area, gingiva was red in color with Grade I bleeding on probing. Miller's class II gingival recession was seen [Figure 1] in relation to 41 and attached gingiva was inadequate in relation to this tooth. Grade I mobility was also present and attachment loss was 6 mm in relation to 41 [Figure 2]. Probing depth was 2 mm. Many mucogingival problems such as recession, loss of attached gingival, and traumatic injuries are a result of vigorous brushing.[4] In this female patient of 27 years, the reason was faulty tooth brushing.
Figure 1a:
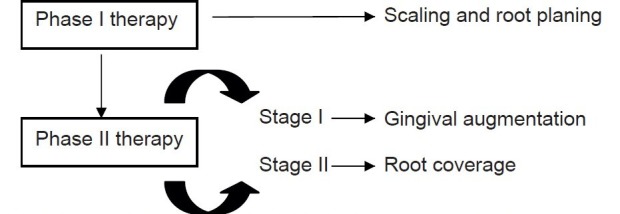
Treatment protocol
Figure 2.
Pre-treatment
Figure 1b:

Class II gingival recession Miller's classification
IOPA revealed crestal bone loss in relation to 41 in mesial aspect [Figure 3]
Figure 3.
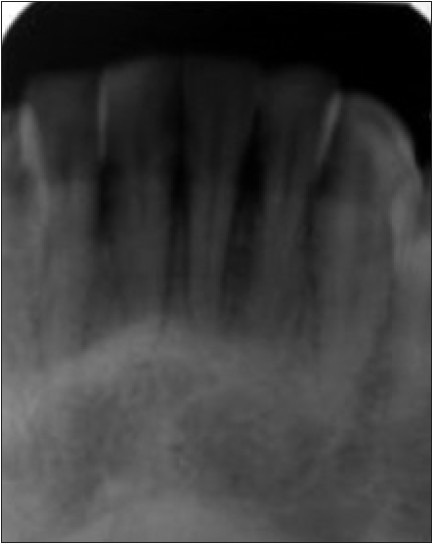
Intra oral periapical radiogragh
Routine hemogram revealed the parameters in their normal range.
Treatment protocol
Phase 1 therapy
Full mouth scaling, root planing, and polishing in relation to 41 area was performed. Patient was motivated to improve her oral hygiene status, chlorhexidine mouth rinse 0.2% was advised after phase 1 therapy [Figure 4].
Figure 4.

Phase I therapy
Phase 2 therapy
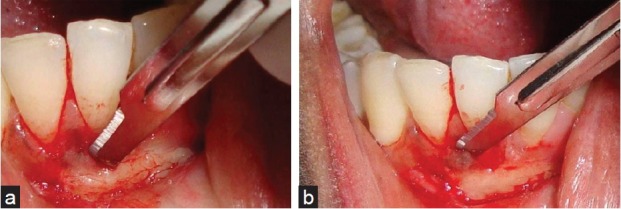
Surgical phase: Stage I: Gingival augmentation with free soft tissue graft
Surgical procedures were performed three weeks following phase 1 therapy. After disinfecting with 0.12% chlorhexidine mouth rinse, local anesthesia was given to the recipient site and donor site (palatal site). The first part of surgery involved preparation of the recipient site apical to recession area. A horizontal incision along the mucogingival junction extending one tooth mesially and distally from affected area was placed using a no:15 bard parker blade [Figure 5]. A tin foil template of the recipient site was prepared and was placed over the recipient site to facilitate the placement of incision [Figures 6 and 7]. Free soft tissue graft was harvested from the palate [Figure 8a and b] and was adapted to the recipient site [Figure 9]. Sutures were placed using 5-0 catgut and periodontal dressing was placed to protect the surgical site [Figures 10 and 11]. An acrylic stent was positioned at the donor site to protect the wound [Figure 12] and necessary instructions were given to the patient. Mechanical plaque control was avoided in the surgical site and dressing was removed after 10 days. Significant increase in the width of attached gingiva was appreciated in about 4 weeks and around 1 mm reduction in the recession height was observed [Figure 13]. A recall check up was done after 3 months.
Figure 5.

Preparation of recipient site
Figure 6.

Placement of the template over the recipient site
Figure 7.
Placement of the template over the donor site & preparation of the donor site
Figure 8.

Harvesting the free soft tissue epithelialized graft
Figure 9.

Graft adapted to the recipient site
Figure 10.

Sutures placed
Figure 11.

Protection of surgical site with periodontal dressing
Figure 12.
Acrylic stent placed on the donor site
Figure 13.

Post-operative stage I surgical phase (4 weeks)
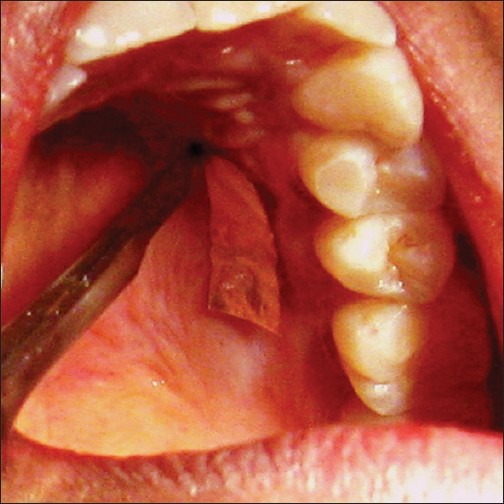
Surgical phase II: Root coverage with lateral sliding flap
After three months healing period, root planing was performed in relation to 41 area [Figure 14. The surgical site was anesthetized. Preparation of the recipient site was carried out [Figure 15a and b]. A partial thickness flap as wide as the defect was reflected [Figure 16a and b]. vertical incision was continued horizontally [Figure 17] and cut back incision was given to relieve the tissue tension [Figure 18]. The flap was moved laterally to cover the exposed root [Figure 19]. This flap was then secured with sutures (black braided silk size 3-0) and the site was protected by periodontal dressing [Figures 20 and 21]. Mechanical plaque control was avoided in surgical site for 10 days following surgery. Patient was advised the necessary instructions. Increase in the attached gingival width after the 1st surgical procedure [Figure 22] in relation to 41 and the root coverage achieved around 4 mm after 2nd surgical phase [Figure 23] could be appreciated.
Figure 14.

Root planing
Figure 15.
Preparation of recipient site
Figure 16.
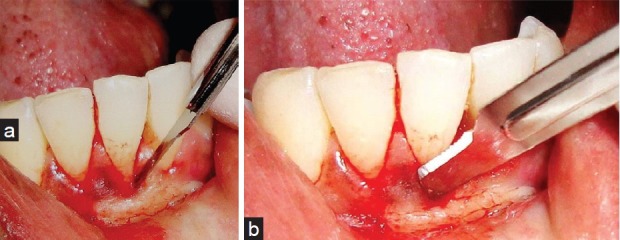
Preparation of partial thickness flap
Figure 17.

Vertical incision for sliding the flap
Figure 18.

Cut back incision for relieving the muscle tension
Figure 19.
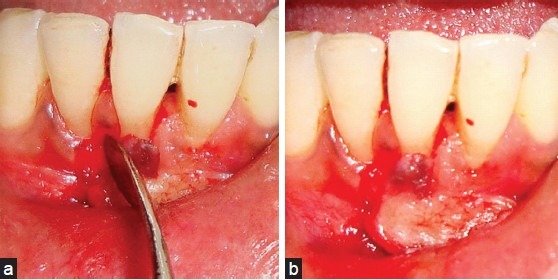
Lateral sliding of pedicle graft
Figure 20.

Sutures placed
Figure 21.

Protection of surgical site
Figure 22.

Post operative stage I (after gingival augmentation)
Figure 23.

Post operative stage II (after root coverage)
DISCUSSION
The structure of the gingival tissues is the basis for healthy gingival function. The presence of a thick keratinized gingival covering serves as an effective barrier that is resistant to damage from the physical trauma of mastication and the thermal and chemical stimuli from the dietary components that have direct contact with the gingiva. The gingival sulcus provides a degree of flexibility to the marginal gingiva as well as maintains an effective epithelial seal against tooth which is essential for periodontal health.[1]
The free soft tissue graft used both as a one or a two-step procedure for the coverage of denuded roots is a versatile modality of treatment used in clinical situations. Problem areas with a lack of keratinized tissue and gingival recession can be effectively treated with free gingival graft to create an adequate zone of attached gingiva and coverage of the exposed root. Areas of gingival recession, in the absence of a mucogingival problem, in which there is an esthetic or root sensitivity consideration can be also treated with a free gingival graft.[1]
The present case with inadequate width of attached gingiva along with Miller's class II gingival recession was treated by a two stage surgical approach, stage I for increasing the zone of keratinized gingiva and stage II for root coverage.
The various treatment modalities available for increasing the zone of keratinized gingiva are free gingival grafts, connective tissue grafts, and apically positioned flaps. A free soft tissue autograft was harvested from the palatal tissue in this case for the same.
Bjorn in 1963 and Sullivan[5] and Atkins[5] in 1968 were the first to describe the free gingival autograft. The autograft was initially used to increase the amount of attached gingiva and extend the vestibular fornix. Later it was used to attempt coverage of exposed root surfaces. Free gingival graft procedure is simple and highly predictable when used to increase the amount of attached gingiva. In early phases, it is important to assure collateral circulation from the connective tissue bed bordering the defect.[5]
Marginal tissue recession may present problems like root sensitivity, esthetic concern to the patient, predilection to root caries, cervical abrasion, and compromising of a restorative effort. When recession is deep and marginal tissue health cannot be maintained, the need for treatment is obvious and various types of soft tissue grafts may be performed.[6]
The autogenous masticatory mucosa graft (free gingival graft) has been shown by Miller, Holbrook and Ochsenbein,[7] Tolme, and Borghetti, and Gardella[7] to produce predictable root coverage.[7]
The pedicle graft has been used to obtain root coverage. The results have been varied depending on the type of pedicle. Allen and Miller and Harris and Harris[7] reported high rates of success in shallow defects treated with pedicle grafts. Common and McFall demonstrated with human histology that a laterally positioned flap combined with citric acid conditioning resulted in new cementum and collagen fibers that were oriented parallel to the root.[7]
After complete healing of the stage I surgery, the second stage root coverage was performed by using lateral sliding flap as there was adequate tissue available adjacent to the recession site. Bjorn (1971) was the first to describe a technique in which a free gingival graft was first placed to enlarge the attached gingiva of the recipient area. One month later, a lateral sliding flap procedure was performed. The term "lateral sliding flap" was introduced by Grupe and Warren and cannot be performed unless there is significant gingiva lateral to the recession site.[8] Lateral sliding flap is often inadequate for the treatment of multiple recessions and its advantages are good vascularity, excellent color matching and involvement of single surgical site[5]
Later in 1975 Bernimoullin et al.[5] used free gingival graft followed by coronally advanced flap procedures in situations where there is need for gingival augmentation in cases with gingival recession in relation to multiple teeth.[5]
The utilization of free gingival graft in treating such cases aids in overcoming the limitations presented by the connective tissue graft as the gingival graft ensures the development of the adequate band of attached gingiva. The subepithelial connective tissue graft, on the other hand, may result in root coverage and results little, if any, increase in the apicocoronal dimension of the keratinized tissue.[1] Decisions regarding the need to perform a graft where narrow bands of gingival exists depend on clinical judgement. In case of anterior region more of esthetics is the concern from the patient's side. It is a belief of many clinicians that a minimum vestibular depth is required for proper oral hygiene maintenance.[9] Again this concept has been challenged. Except for prosthetic reasons involving retention of dentures, vestibular deepening procedures just to facilitate oral hygiene maintenance have been out of vogue.[10]
SUMMARY
Gingival recessions are one of the main esthetic concerns of the patient. A large variety of mucogingival graft procedures for coverage of exposed roots exist. These procedures are quite predictable and produce satisfactory solutions to the problems presented by gingival problems. The outcome of this surgical technique suggests that two stage surgical procedures are ideal for root coverage in case of isolated deep recession and lack of attached gingiva. Selection of the appropriate procedure, precise, and meticulous surgical technique will provide successful and highly predictable results in the treatment of gingival recession.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Camargo PM, Melnick PR, Kenney EB. The use of free gingival grafts for aesthetic purposes. Periodontol 2000. 2001;27:72–96. doi: 10.1034/j.1600-0757.2001.027001072.x. [DOI] [PubMed] [Google Scholar]
- 2.Bouchard P, Mallet J, Borghetti A. Decision-making in aesthetics: Root coverage revisited. Peridontol 2000. 2001;27:97–120. doi: 10.1034/j.1600-0757.2001.027001097.x. [DOI] [PubMed] [Google Scholar]
- 3.Newman MG, Takei HH, Carranza FA. Carranza's Clinical Periodontology. 10th ed. Philadelphia: Saunders; 2006. Periodontal plastic & esthetic surgery. [Google Scholar]
- 4.Allen EP. Aesthetics and plastic surgery in periodontics. Periodontol 2000. 1996;11:7–11. [PubMed] [Google Scholar]
- 5.Mohsin A, Hegde S, Rajesh KS, Arun Kumar MS. Two step surgical procedure for root coverage, Clinical dentistry. Periodontics. 2006;3:33–8. [Google Scholar]
- 6.Allen EA, Miller PD. Coronal positioning of existing gingiva. J Periodontol. 1989;60:316–9. doi: 10.1902/jop.1989.60.6.316. [DOI] [PubMed] [Google Scholar]
- 7.Harris RJ. Human histologic evaluation of root coverage obtained with a connective tissue graft with partial thickness double pedicle graft.A case report. J Periodontol. 1999;70:813–21. doi: 10.1902/jop.1999.70.7.813. [DOI] [PubMed] [Google Scholar]
- 8.Kassab MM, Cohen RE. Treatment of gingival recession. J Am Dent Assoc. 2003;134:220–5. doi: 10.14219/jada.archive.2003.0137. [DOI] [PubMed] [Google Scholar]
- 9.Nowzari H. Aesthetic periodontal therapy. Periodontol 2000. 2001;27:45–58. doi: 10.1034/j.1600-0757.2001.027001045.x. [DOI] [PubMed] [Google Scholar]
- 10.Lindhe J, Lang NP, Karrang T. Blackwell Munksguard. 5th ed 2008. Clinical Periodontology and Implant Dentistry. [Google Scholar]


