Abstract
Gingival cyst of adult is an uncommon cyst of gingival soft tissue occurring in either the free or attached gingiva. This odontogenic epithelial cyst is most frequently seen near mandibular canine and premolar region, believed to represent the soft tissue counter part of the lateral periodontal cyst. This article presents a case of gingival cyst treated with exicisional biopsy followed by histopathological confirmation and an emphasis on the clinical aspects of this lesion.
Keywords: Cyst, excisional biopsy, gingival cyst, odontogenic
INTRODUCTION
Gingival cyst of adult is an uncommon, small, non inflammatory, developmental cyst of gingiva arising from the rests of dental lamina.[1] The relative incidence of a gingival cyst of adult in a large case series of cysts has been reported to be less than 0.5%.[2] They usually occur on the facial gingiva as a single small flesh colored swelling, sometimes with a bluish hue due to the cystic fluid, in the canine and premolar area of the mandible and less frequently in the maxilla. Rarely, it may occur in multiples, either unilaterally or bilaterally or on the lingual surface of the alveolar process. They are commonly seen in the canine and premolar regions of the mandible, and are sometimes confused with lateral periodontal cysts. Gingival cyst lesions in adults may appear bluish due to fluid and cause pressure resorption of the labial bone.[3] Although the gingival cyst is typically a solitary unicystic lesion, reports of multilocular (botryoid) variants and of lesions either presenting in a bilateral distribution or occurring together with the intrabony lateral periodontal cyst have been described.[4,5] The incidence of gingival cysts of adults show a racial predilection, with Asians revealing a much lower prevalence of the lesion than Caucasians; however, there is no gender difference in the incidence of the disease.[3]
CASE REPORT
A 16-year-old male patient presented to the central out-patient department (OPD), Department of Dental surgery, Armed Forces Medical College, Pune with a chief complaint of a swelling in the gum on the left side of the upper jaw from the past five to six months in Nov 2009. The patient was apparently normal before this. He could not recall any recent trauma, pain, or discharge from the swelling or an increase in size of the lesion. His medical history was non-significant, and he was not on any medication at that time. Prior to this visit, the patient had not received dental care for more than 10 years.
During intraoral examination, a smooth round pink colored nodule approximately 5 mm in diameter was noted. It was located on the attached gingiva in relation to the upper left canine and first premolar extending superiorly up to the mucogingival junction [Figure 1]. The nodule was non tender, soft, and cystic in consistency, fluctuant and non compressible. Probing of the adjacent teeth yielded pocket depths of 2-3 mm with all sites exhibiting bleeding on probing, without any communication between the sulci of the adjacent teeth and the lesion. Pulp testing of the canine and first premolar indicated that both were vital. Radiographically, there was no finding suggestive of osseous involvement [Figure 2]. Based on the clinical and radiographic findings, the provisional diagnosis of cystic lesion of the gingiva was made. The differential diagnosis included a lateral periodontal cyst, peripheral fibroma, parulis, and odontogenic keratocyst. Lateral periodontal cyst was ruled out because there was no radiographical finding suggesting of osseous involvement, peripheral fibroma was ruled since the lesion was soft and cystic consistency, parulis was ruled out since the lesion was not associated with periodontal pocket or pus discharge on probing and odontogenic keratocyst was ruled out since the lesion was not associated with pain or localized expansion of bone, and radiographically there was no osseous involvement.
Figure 1.

Clinical presentation of the lesion
Figure 2.
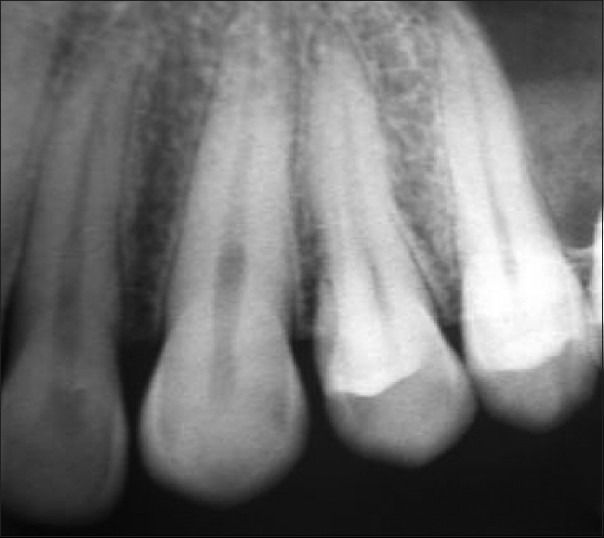
IOPA radiograph 23,24 showing no radiographic involvement
The periodontal treatment plan included scaling, root planing, re-evaluation, and excisional biopsy of the lesion. Two weeks after scaling and root planing, a re-evaluation and excisional biopsy were performed in Dec 2009. Anesthesia was obtained with local infiltration. An incision was placed on the mucosa overlying the lesion [Figure 3] and the lesion was separated from the adjacent tissues through blunt dissection and the lesion was removed [Figure 4]. The surgical specimen measuring 6 × 6 mm was placed in 10% neutral buffered formalin.
Figure 3.

Surgical exposure
Figure 4.

Excised lesion
After the lesion was removed and the area irrigated with sterile saline, it was apparent that a well defined, 2-3 mm deep, saucer-like defect was present in the alveolar process in relation to 23 and 24 [Figure 5]. Hydroxyapatite bone substitute hydrated with sterile saline was placed in the defect [Figure 6], the edges of the soft tissue were undermined and approximated to facilitate primary closure and was secured with a 3-0 black silk suture. Gentle pressure was applied with wet gauze to achieve hemostasis and the wound was covered with a periodontal dressing. The patient was given postoperative instructions and was dismissed with prescription for an analgesic (tab Ibuprofen-400 mg tds every four to six hours as needed for pain), antibiotic (capAmoxicillin-500 mg tds for three days) and antimicrobial rinse (0.2% chlorhexidine gluconate twice a day for one week).
Figure 5.

Bone defect after excision
Figure 6.

Hydroxyapatite bone substitute filled in the defect
The biopsy specimen microscopically consisted of a fibrovascular connective tissue associated with a cystic lining of stratified squamous epithelium. The histopathologic diagnosis was gingival cyst of adult [Figure 7].
Figure 7.
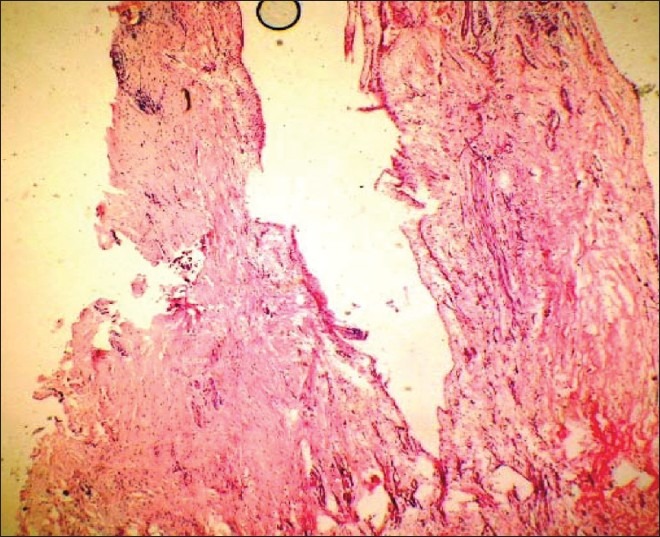
Histopathological slide showing a thin stratified squamous epithelium lining the lumen
At one week postoperative visit, the patient reported minimal discomfort. The sutures were removed. At one month post-surgery, the wound had completely reepithelialized [Figure 8]. The patient is on regular follow-up with a satisfactory healing at six months post-surgery [Figure 9].
Figure 8.

Post operative 01 month
Figure 9.

Post operative 06 months
DISCUSSION
The present report documented a case of gingival cyst of adult treated with excisional biopsy followed by a regenerative approach to correct the associated bony defect. The outward appearance of gingival cyst of adult is typically an oval-to-round, firm, elevated swelling located on the attached gingiva. Mostly are <5 mm in diameter, but lesions >5 cm were also seen.[3] The lesions often demonstrate little or no color change in the overlying mucosa, but some appear bluish due to the cystic fluid. Eighty percent are found in the mandible, with the most common site being the canine premolar area. The gingival cyst of adult is believed to be of odontogenic derivation, specifically from the remnants of ectodermic tissue.[1] The gingival cyst of adult is not related to any inflammatory lesion, and the associated teeth tested are vital. The radiograph does not accurately depict the topography of this soft tissue-originating cyst, as the cyst may involve the alveolar bone surface and can often compromise the buccal or lingual plate with a shallow ′′saucer-like′′ defect.[2] Root exposure associated with this lesion is an extremely rare finding. Gingival cyst of adult is routinely treated with excisional biopsy and has a rare chance of recurrence. The differential diagnosis of gingival cyst of adult includes several lesions presenting as gingival swellings such as a lateral periodontal cyst and peripheral fibroma. The lesion that may be more difficult to differentiate is the lateral periodontal cyst, especially in the presence of both radiographic and gingival involvement. This is because both lateral periodontal cyst and gingival cyst of adult are non-inflammatory cystic lesions, typically present in the mandibular canine-premolar area, and share histopathological characteristics.[6,7] In the present case, the combined anatomic characteristics of the soft tissue presentation and the osseous destruction suggest that the lesion was gingival cyst of adult.
CONCLUSION
The gingival cyst of adult is a unique pathologic lesion of the oral cavity, typically localized in the mandibular canine and premolar region, appearing in adults in their fourth to fifth decades of life. Associated osseous involvement occurs <50% of the time and is often undetectable radiographically. Treatment by excisional biopsy is definitive. Exposure of the tooth root is an extremely rare feature of the gingival cyst of adult; in such cases, as in the present report, a combined regenerative treatment approach may be used to achieve resolution of the lesion-associated osseous defect and the excisional biopsy-associated soft tissue defect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Moskow BS, Bloom A. Embryogenesis of the gingival cyst. J Clin Periodontol. 1983;10:119–30. doi: 10.1111/j.1600-051x.1983.tb02200.x. [DOI] [PubMed] [Google Scholar]
- 2.Bhaskar SN, Laskin DM. Gingival cysts; Report of three cases. Oral Surg Oral Med Oral Pathol. 1955;8:803–7. doi: 10.1016/0030-4220(55)90237-1. [DOI] [PubMed] [Google Scholar]
- 3.Sato H, Kobayashi W, Sakaki H, Kimura H. Huge Gingival Cyst of the Adult: A Case Report and Review of the Literature. Asian J Oral Maxillofac Surg. 2007;19:176–8. [Google Scholar]
- 4.Nxumalo TN, Shear M. Gingival cyst in adults. J Oral Pathol Med. 1992;21:309–13. doi: 10.1111/j.1600-0714.1992.tb01017.x. [DOI] [PubMed] [Google Scholar]
- 5.Hegde U, Reddy R. Gingival cyst of adult a case report with unusual findings. Indian J Dent Res. 2004;15:78–80. [PubMed] [Google Scholar]
- 6.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. In: Neville BW, Damm DD, Allen CM, Bouquot JE, editors. Odontogenic cysts and tumors. 3rd ed. St. Louis: Saunders; 2009. p. 692. [Google Scholar]
- 7.Giunta JL. Gingival cysts in the adult. J Periodontol. 2002;73:827–31. doi: 10.1902/jop.2002.73.7.827. [DOI] [PubMed] [Google Scholar]


