Abstract
Context:
While some studies have found disparities between subtypes of irritable bowel syndrome (IBS), others did not found such differences.
Aim:
This study aimed to investigate whether there are differences in psychological features between the subtypes of IBS.
Settings and Design:
A cross-sectional study was performed on all consecutive outpatients IBS diagnosed (from Oct. 2010 to Oct. 2011) in Taleghani Hospital gastroenterology clinic, Tehran, Iran.
Materials and Methods:
A total of 153 consecutively diagnosed IBS patients (using Rome III criteria); including 80 constipation-predominant (IBS-C), 22 diarrhea-predominant (IBS-D), and 51 mixed IBS (IBS-M) were asked to complete the Symptom Checklist 90 Revised (SCL-90-R).
Statistical Analysis:
Pearson's chi-square test was used to compare nominal variables. One-way ANOVA was used to compare continuous variables.
Results:
Although IBS-C patients were more suffered from psychiatric disorders, there were no statistical differences between mean score of IBS-C, IBS-D, and IBS-M patients regarding to all of SCL-90-R subscales and three global indices including Global Severity Index (GSI), Positive Symptom Distress Index (PSDI) and Positive Symptom Total (PST) (P<0.05).
Conclusion:
Our finding showed that there are no different symptomatic profiles between IBS subtypes.
Keywords: Irritable bowel syndrome, psychiatric aspects, Rome III criteria, symptom checklist-90-revised
INTRODUCTION
Recent psychological studies on irritable bowel syndrome (IBS) - commonest functional bowel disorders seen by gastroenterologists - have suggested that there is evidence of an association with psychological factors, especially depression, anxiety, and somatization.[1–7] Some studies have shown that approximately up to 60% of IBS patients have major psychosocial problems.[5,6,8,9] According to Rome III criteria (the latest gastrointestinal symptom questionnaire), IBS was categorized to three groups including: constipation-predominant IBS (IBS-C), diarrhea-predominant IBS (IBS-D), and mixed-IBS (IBS-M). To our knowledge, a few studies on the association between the subtype of IBS patients and psychiatric comorbidity are published.
The Symptom Checklist-90-Revised (SCL-90-R) is a 90-item self-report symptom inventory developed by Leonard R. Derogatis in the mid-1970s to measure psychological symptoms and psychological distress.[10] In 1988, Whitehead's group[11] administered the Symptom SCL-90-R in order to comparing IBS patients with IBS non-patients and normal subjects. They revealed that the IBS patients have higher level of psychological symptoms compared to other two groups. Walker et al.[12] described an association of medically unexplained complaints with psychiatric comorbidity in IBS patients. Miller et al.[13] found that IBS patients with somatization disorder have more psychiatric symptoms and abnormal illness behaviors than in patients with only IBS. Whitehead et al.[14] reported no significant trait differences between IBS-D and IBS-C patients. They also found that there were no disparity in colonic motility and psychological testing between various subtypes of IBS. Whitehead and Crowell[15] suggested that observed association have seen between psychiatric illness and IBS might be due to inclusion of patients with somatization disorder in IBS samples. However, in Iran no similar study has been performed on determining the psychiatric pattern in IBS patients. We aimed to investigate whether psychopathological features differ between subtypes of IBS as defined by the Rome III criteria.
MATERIALS AND METHODS
A cross-sectional study was performed on all consecutive outpatients IBS diagnosed (from October 2010 to October 2011) in Taleghani Hospital gastroenterology clinic, Tehran, Iran. The previously validated Iranian version of the Rome III questionnaire was used for diagnosis of IBS.[16–19] IBS was defined as having abdominal pain or discomfort for at least 3 months in the previous 6 months, accompanied with at least two or more of the following symptoms: (1) pain improved with bowel movement, (2) symptoms associated with a change in stool frequency, and (3) symptoms associated with a change in the appearance of stool. Patients were interviewed by an experienced gastroenterologist and those who have another co-existing disease (e.g., malignancy; cardiovascular, pulmonary, hepatic, or renal disorder) were excluded. Then IBS patients were categorized into constipation predominant IBS (IBS-C) if they had hard or lumpy stools with no loose, watery mushy or watery stools in the past 3 months; diarrhea predominant IBS (IBS-D) if they had loose, mushy or water stools in the last 3 months with no hard or lumpy stools; and mixed IBS (IBS-M) if they had both loose and hard stools in the past 3 months.
In order to assess psychopathological features, patients were asked to complete the Symptom Checklist 90 Revised (SCL-90-R). SCL-90-R is appropriate for use in both normal and individuals with medical or psychiatric disorders and has shown good internal consistency (a coefficients range from 0.77 to 0.90) and test-retest reliability (range in r=0.68–0.83).[20,21] In one Iranian study, the Persian version of SCL-90-R had a Cronbach's alpha reliability of 0.95 and the split-half reliability was 0.88.[22] The questionnaire consists of 90 items concerning an individual's symptom distress in the previous week and the individual has to assign a five-point Likert scale from 0 to 4 -from “no problem” to “very serious”- depending on the degree of suffering related to the item. It has 9 subscales (somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychotics) and three global indices (Global Severity Index (GSI), Positive Symptom Distress Index (PSDI), and Positive Symptom Total (PST)). GSI, which represents the average severity score of all the 90 items, is thought to be a reliable measure of psychological distress.
After explanation of the study aim, patients were asked to give their written consent to participate. The study received approval from Ethics Committee.
Pearson's chi-square test was used to compare nominal variables. One-way ANOVA was used to compare continuous variables. Continuous variables are presented as mean±standard deviation and categorized data as frequency and percentage. All statistical tests were two-sided, and P values less than 0.05 were considered significant. All data were analyzed using SPSS 13.0 software.
RESULTS
One hundred fifty-three patients (37.5% males, 62.5% females) were enrolled to the study. Most of patients under study were low educated (lower than high school) (55, 35.9%), married (96, 58.9%), and employed (72, 47.1%).
IBS-C was the most frequent subtypes of IBS patients seen by gastroenterologist (52.3%), followed by IBS-M (33.3%), and IBS-D (14.4%). The psychopathological features of the different subtypes of IBS were compared using the SCL-90-R.
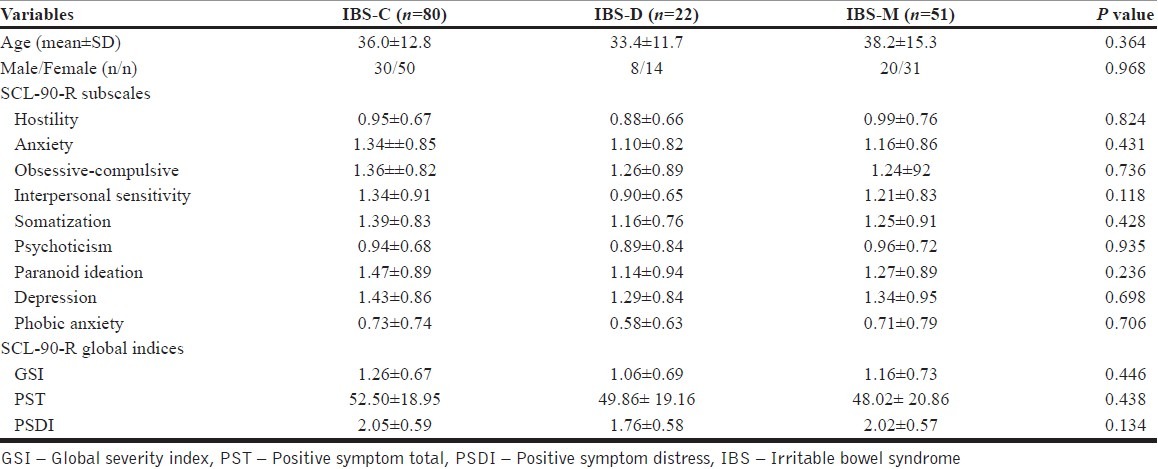
As shown in [Table 1], although IBS-C patients were more suffered from psychiatric symptoms, there were no statistical differences between mean score of IBS-C, IBS-D, and IBS-M patients regarding to all of SCL-90-R subscales and GSI, PST, and PSDI scores (P>0.05).
Table 1.
Comparing mean scores of the SCL-90-R GSI, PST, and PSDI and subscales between subtypes of IBS
DISCUSSION
The purpose of this study was to ascertain if there were any differences between the subtypes of IBS with controls regarding to psychiatric symptoms. We used the Rome III criteria for diagnosing of IBS and SCL-90-R in order to screening for psychiatric symptoms. Our findings have shown that psychiatric scores, although higher in the IBS-C patients, was statistically similar in all subtypes of IBS.
Many studies have documented the higher prevalence of psychopathology (40%-60%) in IBS patients especially - depression, generalized anxiety disorder, somatization, panic disorder, agoraphobia, and post traumatic stress - in comparison with patients with organic digestive diseases and healthy controls.[4,12,23–25] Some researchers have hypothesized that specific types of psychological distress, especially anxiety, may be etiologically related to IBS.[26,27] Walker et al.[28] revealed that 82% of IBS patients affected by a psychiatric disorder, notably an anxiety disorder, before the development of the IBS symptoms. Lydiard et al.[29] using structured clinical interviews measuring DSM-III-R criteria reported that 40% of IBS patients fulfilled the diagnostic criteria for psychiatric disorder before the onset of IBS and 34% experienced both within the same year.
Our findings showed that there are no different symptomatic profiles between IBS subtypes. In line with the present study, Whitehead et al.[14] reported no significant trait differences between IBS patients with diarrhea and those with constipation. They also found that there was not any disparity in colonic motility and psychological testing between various subtypes of IBS. In contrast, some studies reported that IBS subtypes have different profiles in psychological symptoms, body awareness and somatic symptoms. In a recent study, Muscatello et al.[30] found that IBS-C patients more psychologically distressed than IBS-D subjects. IBS-C and IBS-A subtypes have a higher rate of depression and anxiety and lower quality of life comparing to IBS-D. Against to IBS-C and IBS-A, IBS-D associated with lowered body awareness, less psychological symptoms and a higher sense of coherence and elevated C-peptide values.[31] Others have suggested that there is a close association between the autonomic nervous system, predominant physical symptoms, colon transit time, and psychological factors in IBS patients and have found that the IBS-C subtype is associated with a cholinergic abnormality and the IBS-D with an adrenergic abnormality.[32] Although the association of IBS and psychological problems is well established,[33–38] it seems that there is no consistency among different studies aimed to investigate any potential disparities in psychopathological features between subtypes of IBS. We think that the main cause of difference between our results and the previous ones might be due to methodological differences in diagnosis of both IBS and psychiatric disorders.
While many studies have measured the comorbidity of psychiatric disorders and IBS, few have examined the timing of IBS onset in relation to the onset of psychiatric disorders. However, the exact nature of the relationship between psychological distress and IBS is unknown. Current models for explaining the relationship between psychological distress and IBS are: the “somatopsychic hypothesis” and the “psychosomatic hypothesis”.[27,28] The first hypothesis indicate that suffering from IBS for long time causes psychological problems and the other explain that IBS is a somatic expression of psychological problems. If suppose that second hypothesis is true and IBS is a psychophysiological disorder, effective management of the psychological problems should improve the attendant IBS symptoms. Some researchers with study on patients diagnosed with both panic disorder and IBD have reported that pharmacological treatment for panic disorder improved both panic and IBS symptoms.[39,40] Another study with investigation on thirty two patients with comorbid generalized anxiety disorder and IBS observed that Alprazolam reduced both acute anxiety and IBS symptoms.[41] Although the sample size of these three studies was very small, it seems that effective treatment of the anxiety disorder would be relieved the IBS symptoms.
In comparison with other similar studies, our study has some strength. Using standard instruments for diagnosing of both IBS and psychiatric disorders is one of the strengths of this study. Our study has also some limitations that may affect the interpretation of findings. First, we do not have any control group. Second, the IBS patients were selected from the treatment-seeking patients referred to a gastroenterology clinic and the study participants may not be fully representative of IBS patients in general population. Third, we did not investigate the timing of the onset of IBS and psychiatric disorders, and finally, our sample size was moderately low.
In conclusion, we could not find any significant differences between subtypes of IBS regarding to psychological features. Future researches are needed with larger sample size from both treatment-seeking and non-treatment-seeking to be able to generalize the results.
ACKNOWLEDGMENT
Funding was provided by University of Social Welfare and Rehabilitation Science, Tehran, Iran.
Footnotes
Source of Support: University of Social Welfare and Rehabilitation Science, Tehran, Iran.
Conflict of Interest: None.
REFERENCES
- 1.Fullwood A, Drossman DA. The relationship of psychiatric illness with gastrointestinal disease. Annu Rev Med. 1995;46:483–96. doi: 10.1146/annurev.med.46.1.483. [DOI] [PubMed] [Google Scholar]
- 2.Drossman D. Do psychosocial factors define symptom severity and patient status in irritable bowel syndrome? Am J Med. 1999;107:41S–50S. doi: 10.1016/s0002-9343(99)00081-9. [DOI] [PubMed] [Google Scholar]
- 3.Budavari AI, Olden KW. Psychosocial aspects of functional gastrointestinal disorders. Gastroenterol Clin North Am. 2003;32:477–506. doi: 10.1016/s0889-8553(03)00030-x. [DOI] [PubMed] [Google Scholar]
- 4.Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology. 2006;130:1447–58. doi: 10.1053/j.gastro.2005.11.057. [DOI] [PubMed] [Google Scholar]
- 5.Moser G. Psychosomatic aspects of bowel diseases. Z Psychosom Med Psychother. 2006;52:112–26. doi: 10.13109/zptm.2006.52.2.112. [DOI] [PubMed] [Google Scholar]
- 6.Moser G. Psychotherapy in somatic diseases--for example gastrointestinal disorders. Psychiatr Danub. 2007;19:327–31. [PubMed] [Google Scholar]
- 7.Whitehead WE. Psychosocial aspects of functional gastrointestinal disorders. Gastroenterol Clin North Am. 1996;25:21–34. doi: 10.1016/s0889-8553(05)70363-0. [DOI] [PubMed] [Google Scholar]
- 8.Drossman DA, Creed FH, Olden KW, Svedlund J, Toner BB, Whitehead WE. Psychosocial aspects of the functional gastrointestinal disorders. Gut. 1999;45(Suppl 2):II25–30. doi: 10.1136/gut.45.2008.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olden KW, Drossman DA. Psychologic and psychiatric aspects of gastrointestinal disease. Med Clin North Am. 2000;84:1313–27. doi: 10.1016/s0025-7125(05)70288-1. [DOI] [PubMed] [Google Scholar]
- 10.Derogatis LR, Unger R. The Corsini Encyclopedia of Psychology. Hoboken, New Jersey: John Wiley & Sons, Inc; 2010. Symptom Checklist-90-Revised. [Google Scholar]
- 11.Whitehead W, Bosmajian L, Zonderman A, Costa PT, Schuster M. Symptoms of psychologic distress associated with irritable bowel syndrome: Comparison of community and medical clinic samples. Gastroenterology. 1988;95:709–14. doi: 10.1016/s0016-5085(88)80018-0. [DOI] [PubMed] [Google Scholar]
- 12.Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric diagnoses, sexual and physical victimization, and disability in patients with irritable bowel syndrome or inflammatory bowel disease. Psychol Med. 1995;25:1259–67. doi: 10.1017/s0033291700033225. [DOI] [PubMed] [Google Scholar]
- 13.Miller A, North C, Clouse R, Alpers D, Wetzel R. Irritable bowel syndrome, psychiatric illness, personality, and abuse: is somatization disorder the missing link? Ann Clin Psychiatry. 2001;13:25–30. doi: 10.1023/a:1009060731057. [DOI] [PubMed] [Google Scholar]
- 14.Whitehead W, Engel B, Schuster M. Irritable bowel syndrome: physiological and psychological differences between diarrhea-predominant and constipation-predominant patients. Dig Dis Sci. 1980;25:404–13. doi: 10.1007/BF01395503. [DOI] [PubMed] [Google Scholar]
- 15.Whitehead WE, Crowell MD. Psychologic considerations in the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:249–67. [PubMed] [Google Scholar]
- 16.Barzkar M, Pourhoseingholi MA, Habibi M, Moghimi-Dehkordi B, Safaee A, Pourhoseingholi A, et al. Uninvestigated dyspepsia and its related factors in an Iranian community. Saudi Med J. 2009;30:397–402. [PubMed] [Google Scholar]
- 17.Khoshkrood-Mansoori B, Pourhoseingholi MA, Safaee A, Moghimi-Dehkordi B, Sedigh-Tonekaboni B, Pourhoseingholi A, et al. Irritable bowel syndrome: a population based study. J Gastrointestin Liver Dis. 2009;18:413–8. [PubMed] [Google Scholar]
- 18.Solhpour A, Safaee A, Pourhoseingholi MA, Moghimi-Dehkordi B, Habibi M, Qafarnejad F, et al. Relationship between uninvestigated dyspepsia and body mass index: a population-based study. East Afr J Public Health. 2010;7:318–22. doi: 10.4314/eajph.v7i4.64755. [DOI] [PubMed] [Google Scholar]
- 19.Sorouri M, Pourhoseingholi MA, Vahedi M, Safaee A, Moghimi-Dehkordi B, Pourhoseingholi A, et al. Functional bowel disorders in Iranian population using Rome III criteria. Saudi J Gastroenterol. 2010;16:154–60. doi: 10.4103/1319-3767.65183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–9. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- 21.Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of interpersonal problems: psychometric properties and clinical applications. J Consult Clin Psychol. 1988;56:885–92. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- 22.Alavi SS, Maracy MR, Jannatifard F, Eslami M. The effect of psychiatric symptoms on the internet addiction disorder in Isfahan's University students. J Res Med Sci. 2011;16:793–800. [PMC free article] [PubMed] [Google Scholar]
- 23.Corsetti M, Caenepeel P, Fischler B, Janssens J, Tack J. Impact of coexisting irritable bowel syndrome on symptoms and pathophysiological mechanisms in functional dyspepsia. Am J Gastroenterol. 2004;99:1152–9. doi: 10.1111/j.1572-0241.2004.30040.x. [DOI] [PubMed] [Google Scholar]
- 24.Schwarz SP, Blanchard EB, Berreman CF, Scharff L, Taylor AE, Greene BR, et al. Psychological aspects of irritable bowel syndrome: comparisons with inflammatory bowel disease and nonpatient controls. Behav Res Ther. 1993;31:297–304. doi: 10.1016/0005-7967(93)90028-s. [DOI] [PubMed] [Google Scholar]
- 25.Blanchard EB, Scharff L, Schwarz SP, Suls JM, Barlow DH. The role of anxiety and depression in the irritable bowel syndrome. Behav Res Ther. 1990;28:401–5. doi: 10.1016/0005-7967(90)90159-g. [DOI] [PubMed] [Google Scholar]
- 26.Folks DG, Kinney FC. The role of psychological factors in gastrointestinal conditions. A review pertinent to DSM-IV. Psychosomatics. 1992;33:257–70. doi: 10.1016/S0033-3182(92)71964-1. [DOI] [PubMed] [Google Scholar]
- 27.Blanchard EB, Scharff L. Psychosocial aspects of assessment and treatment of irritable bowel syndrome in adults and recurrent abdominal pain in children. J Consult Clin Psychol. 2002;70:725–38. doi: 10.1037//0022-006x.70.3.725. [DOI] [PubMed] [Google Scholar]
- 28.Walker EA, Roy-Byrne PP, Katon WJ. Irritable bowel syndrome and psychiatric illness. Am J Psychiatry. 1990;147:565–72. doi: 10.1176/ajp.147.5.565. [DOI] [PubMed] [Google Scholar]
- 29.Lydiard RB, Fossey MD, Marsh W, Ballenger JC. Prevalence of psychiatric disorders in patients with irritable bowel syndrome. Psychosomatics. 1993;34:229–34. doi: 10.1016/S0033-3182(93)71884-8. [DOI] [PubMed] [Google Scholar]
- 30.Muscatello MR, Bruno A, Pandolfo G, Mico U, Stilo S, Scaffidi M, et al. Depression, anxiety and anger in subtypes of irritable bowel syndrome patients. J Clin Psychol Med Settings. 2010;17:64–70. doi: 10.1007/s10880-009-9182-7. [DOI] [PubMed] [Google Scholar]
- 31.Eriksson EM, Andren KI, Eriksson HT, Kurlberg GK. Irritable bowel syndrome subtypes differ in body awareness, psychological symptoms and biochemical stress markers. World J Gastroenterol. 2008;14:4889–96. doi: 10.3748/wjg.14.4889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aggarwal A, Cutts TF, Abell TL, Cardoso S, Familoni B, Bremer J, et al. Predominant symptoms in irritable bowel syndrome correlate with specific autonomic nervous system abnormalities. Gastroenterology. 1994;106:945–50. doi: 10.1016/0016-5085(94)90753-6. [DOI] [PubMed] [Google Scholar]
- 33.Hazlett-Stevens H, Craske MG, Mayer EA, Chang L, Naliboff BD. Prevalence of irritable bowel syndrome among university students: the roles of worry, neuroticism, anxiety sensitivity and visceral anxiety. J Psychosom Res. 2003;55:501–5. doi: 10.1016/s0022-3999(03)00019-9. [DOI] [PubMed] [Google Scholar]
- 34.Rose JD, Troughton AH, Harvey JS, Smith PM. Depression and functional bowel disorders in gastrointestinal outpatients. Gut. 1986;27:1025–8. doi: 10.1136/gut.27.9.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Esler MD, Goulston KJ. Levels of anxiety in colonic disorders. N Engl J Med. 1973;288:16–20. doi: 10.1056/NEJM197301042880104. [DOI] [PubMed] [Google Scholar]
- 36.Nicholl BI, Halder SL, Macfarlane GJ, Thompson DG, O’Brien S, Musleh M, et al. Psychosocial risk markers for new onset irritable bowel syndrome--results of a large prospective population-based study. Pain. 2008;137:147–55. doi: 10.1016/j.pain.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62(Suppl 8):28–36. discussion 7. [PubMed] [Google Scholar]
- 38.Blanchard EB, Lackner JM, Jaccard J, Rowell D, Carosella AM, Powell C, et al. The role of stress in symptom exacerbation among IBS patients. J Psychosom Res. 2008;64:119–28. doi: 10.1016/j.jpsychores.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 39.Lydiard RB, Laraia MT, Howell EF, Ballenger JC. Can panic disorder present as irritable bowel syndrome? J Clin Psychiatry. 1986;47:470–3. [PubMed] [Google Scholar]
- 40.Noyes R, Jr, Cook B, Garvey M, Summers R. Reduction of gastrointestinal symptoms following treatment for panic disorder. Psychosomatics. 1990;31:75–9. doi: 10.1016/S0033-3182(90)72220-7. [DOI] [PubMed] [Google Scholar]
- 41.Tollefson GD, Luxenberg M, Valentine R, Dunsmore G, Tollefson SL. An open label trial of alprazolam in comorbid irritable bowel syndrome and generalized anxiety disorder. J Clin Psychiatry. 1991;52:502–8. [PubMed] [Google Scholar]


