Abstract
Background:
There is a paucity of studies done on medically unexplained physical symptoms (MUPS) in Kerala, India. The objective of this study was to examine the sociodemographic and other clinical variables associated with this condition.
Materials and Methods:
The clinical sample was taken from the General Medicine Clinic of a tertiary care hospital, in Kerala. The referred cases meeting the criteria (N=48) for medically unexplained physical symptoms were enrolled for this cross-sectional study. The medical doctor with experience in psychiatry completed the questionnaire.
Results:
Most of the patients were middle-aged females from rural areas. The most common symptom reported was headache. Most of the patients had symptoms for five years or more and had seen two-to-five consultants. A majority of the patients had undergone special investigations and a few had expensive and invasive investigations. Cluster C personality disorders were the most common associated personality disorders with medically unexplained physical symptoms.
Conclusions:
To our knowledge this is the first psychosocioeconomic study on medically unexplained physical symptoms, done in Kerala, India. Medically unexplained physical symptoms cause loss of productivity and economic burden and are a major public health problem. Future studies are warranted focusing on non-pharmacological treatment, psycho-education on mind–body association, and medical models on specific cytokines associated with medically unexplained physical symptoms for personalized management, and to examine the effect of a combination of pharmacotherapy and cognitive behavioral therapy.
Keywords: Medically unexplained physical symptoms, psychosocioeconomic, economic burden
INTRODUCTION
A substantial proportion of patients who repeatedly present to hospitals with symptoms for which conventional pathology cannot be identified, show evidence of psychological distress that is either not expressed or is unrecognized in the general practice consultation.[1] The phenomena has two aspects: The expression of psychological illness through physical symptoms, and repeated medical help-seeking for multiple medical symptoms without organic disease.[2] Some individuals live their life through somatization.[3] Somatization diagnosis is a prevalent, expensive, and a difficult-to-treat problem for general practitioners.[4] It is also reported that some cultures stigmatize psychological disorder more than others.[5] To overcome the confusion around the term somatization, many researchers prefer the term medically unexplained physical symptoms (MUPS).[6] Neither somatized mental distress nor somatization disorders adequately account for most patients seen with MUPS.[7]
Patients show up at hospitals with symptoms for a variety of reasons,[8] including the disruption caused by the severity of the symptoms and the patients’ concerns about what they mean.[9] The meaning of physical experiences seems fundamental to these conditions.[10]
There was a paucity of studies done on MUPS in Kerala, a south Indian state. The objective of this study was to examine the sociodemographic and other clinical variables associated with MUPS.
MATERIALS AND METHODS
The clinical sample was taken from the General / Internal Medicine Outpatient Clinic of the Government Medical College, Thrissur, Kerala, India. We selected this particular tertiary care hospital, which was in a rural setting. The medical doctor, with psychiatry experience, saw the potential patients together with the physicians on Mondays in the clinic. The referred cases meeting the criteria for MUPS were enrolled for the study, for approximately three years. The medical doctor discussed the cases with the consultant psychiatrist (PK-second author) and confirmed the diagnosis. The criteria for MUPS were one or more physical symptoms after appropriate investigation, which could not be explained by a general medical condition, and the symptoms caused clinically significant distress or impairment in social and occupational functioning, in excess of what would be expected from the history and physical examination and laboratory findings. The medical doctor with psychiatry experience completed the questionnaire, which included the sociodemographic profile, with details regarding frequency of physical complaints, duration of symptoms, the number of visits to the doctor, investigations done, psychosocial and environmental stressors, and personality disorder. The symptoms were assessed using the symptom enquiry checklist used in the World Health Organization International study on somatoform disorders (1994), which had 73 questions. In this cross-sectional study, the interview duration was approximately 90 minutes. The study was approved by the Ethics Committee of Thrissur Medical College. We obtained oral informed consent from the patients. For the descriptive purpose, N (%) was done and is presented in the tables.
RESULTS
We provide descriptive information on the sociodemographic variables, summarized in Table 1, and clinical variables, summarized in Tables 2 and 3, of 48 participants enrolled in this exploratory study.
Table 1.
Sociodemographic data (N=48) presented

Table 2.
Frequency of physical complaints
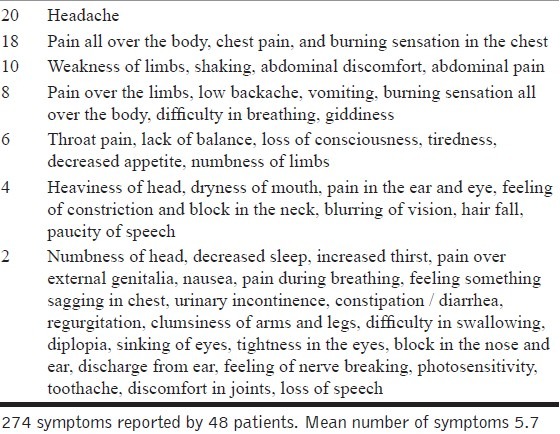
Table 3.
Clinical characteristics presented

DISCUSSION
There were a total of 274 symptoms, which is an average of 5.7 symptoms per patient. The most common symptom reported was headache.
In contrast to the female-to-male ratio of 5 : 1 (DSM-IV-TR), we found a female-to-male ratio of 7 : 1. This may be because of the difference in the Western population versus the Indian population.
A higher rural representation in the sample may be reflecting the hospital sample. Rural people may accept fewer psychological reasons, and hence, may not seek care. There could be more avenues for catharsis in an urban setting. The medical knowledge of urban people may be discouraging them from reporting psychological distress as a physical disease. They may find it difficult to explain MUPS to themselves and others.
Consistent with DSM-IV-TR, our study also showed that avoidant and obsessive compulsive personality disorders were commonly associated with MUPS. In contrast, we did not find an association between MUPS and paranoid, histrionic, and antisocial personalities.
The preponderance of females in this study is not consistent with the usual hospital data in India. In conditions where community data shows a higher prevalence of females, hospital data shows male predominance. More males get the benefit of treatment, overriding the higher need in females. This is understandable in the male-dominant Indian culture. However, the findings were contrary in case of MUPS in this study.
For physical manifestations arising from psychological distress, females getting treatment outnumber males. The severity, chronic nature, and social acceptance of symptoms may be the reasons for this discrepancy. It may be that the predominance of adults in this study reflects the usual hospital patient population. Seeking out treatment is perhaps encouraged in the breadwinning age group.
It may be that more patients in the married group reflect the hospital profile. The large number of sustained marital relationships in Indian culture is common. However, in the ECA study done in US, in 3,132 community respondents with somatization disorder, the majority was unmarried or divorced, which is consistent with the Western culture.[11] In India, women may be bearing the strain of marital conflict, expressing it through culturally acceptable physical symptoms. This has been reported in a study from the neighboring state of Tamil Nadu, another southern state in India.[3] Consistent with our results, headache was the most common symptom and obsession scores were also high in the quoted study done in Tamil Nadu.
A large number of patients in this study had to even undergo invasive investigations. A medical doctor in India has relatively insignificant exposure in psychiatry during the medical school / college training period. After the training they practically have no avenues to get further exposure to psychiatry as a mental health professional's work, in isolation. Hence, a physician who is not a psychiatrist is without adequate confidence to diagnose a psychiatric syndrome. They rely on a lot more investigations, probing for a physical diagnosis. The more the patient is investigated, the more a patient is convinced about the physical basis. On account of the psychogenic etiopathophysiology, non-pharmacological intervention becomes very difficult. Although it has been estimated that 5% of the patients in general practice present with severe forms of somatization,[12] this disorder is clearly underdiagnosed, and on many occasions physicians tend to repeatedly pursue an organic etiology for the patients’ complaints, using multiple test procedures, medication, and surgical operations instead of recognizing a somatization disorder.[12–16] Finally, patients with a somatization disorder tend to withdraw from pleasurable activities and have less productivity because of discomfort, fatigue or fear of exacerbation of their symptoms.[17]
In a review on somatizing and psychologizing patients, there were no consistent differences between people with psychiatric disorders, who presented with psychological symptoms versus who presented with physical symptoms.[18] Although 25% of the affected patients present with only psychological symptoms, the remainder may accept the possibility of a psychosocial component to their physical symptoms, even if they do not volunteer it during the consultation.[19] Practical reasons, such as lack of time, or a sense that problems are not relevant or amenable to treatment, seem more important than failure to recognize their own mental distress, which may explain why patients choose not to disclose psychological problems during consultations.[20] One of the few longitudinal studies identified a pattern whereby symptoms occurring at a time of newly increased stress tended to be attributed to stress. Patients came to doctors with MUPS only if the stress persisted.[21] In our study, a medical doctor with psychiatry experience who was not a psychiatrist easily elicited the stressors. Lack of time is not a restraining factor to elicit stressors / stress, only an orientation and an inclination for it is required.
Patients may often perceive doctors as denying the validity of their symptoms.[9,20–22] Even as doctors have medical models of illnesses; patients also have lay models, which are complex and broadly consistent. These include the name of the condition and its symptoms, the personal consequences of it, how long will it last, and the extent to which it can be controlled or cured.[22] Patients have health beliefs about individual symptoms as well as established diseases. There are eight dimensions proposed: four on the etiology (stress, environment, lifestyle, and weak constitution), three concerning mechanism (wearing out, internal structure, and internal function), and a final dimension of concern raised by the symptom proposed.[9] Patients are able to accept a medical opinion when doctors develop non-blaming models of conditions with their patients and form constructive alliances against the illness.[9,20–22]
Illness belief models explore how patients see illness as threatening. The doctors seek to reduce that threat through treatment and reassurance. Unfortunately, reassurance is not always effective; between a third and half of the patients report a continuing concern about serious illness after normal cardiac ultrasound or angiography.[23]
Psychological models of threat reduction suggest two separate processes: emotional-heuristic (calming, protecting, and threat-avoiding), and cognitive-systematic (information-seeking and threat-analyzing).[24] Although emotional, threat avoiding, verbal and non-verbal reassurance may be effective in alleviating distress in the short term, it may not be effective to weaken illness representations. If symptoms recur, repeated reassurance is likely to produce a cycle of reassurance seeking and giving that is self-perpetuating. In contrast, the cognitive model of threat analyzing is more threatening for patients in the short term, but more likely to produce long-term changes, which in turn, may be associated with improvement.
The physician tends to be initially concerned to rule out treatable medical conditions, and when none are found, leads to ‘excessive’ help-seeking behavior. This shift often marks deterioration in the physician–patient relationship, as the patients sense that their doctor has lost interest in them or view them as bothersome. Although many physicians are eager to refer the patient for psychiatric evaluation and treatment, patients might see the referral as their doctor's way of questioning the reality of their symptoms. This challenge has encouraged the development of treatment approaches for somatization disorder that meet the different demands of the patient and the referring physician.[25]
Kaiser-Permanente, a US health maintenance program has shown that somatizing patients could bankrupt the healthcare financing system[26] and these patients can be helped leading to reduced healthcare costs.[27]
The ‘Affective Cognitive Behavioral Therapy’ is recommended for physicians, for the treatment of MUPS, which includes the following: providing continuity of care, avoiding unnecessary tests and procedures, providing frequent, brief, and regular office visits, always performing a physical examination, avoiding making disparaging comments like, ‘Your symptoms are all in your head’, setting reasonable therapeutic goals like maintaining the functioning despite ongoing pain.[17]
In a review on human psychoneuroimmunology studies, authors found that immune modulation by psychosocial stressors or interventions could lead to actual health changes.[28]
STRENGTHS AND LIMITATIONS
The major strength of this study is the large sample size (N=48) in an Indian population. One more strength is the unique clinical sample having the features of both a rural setting and a tertiary care hospital. In our study, we could not calculate the prevalence, because we did not have the total number of patients who showed up at the medicine clinic on Mondays. Our study included subjects with MUPS and not with a DSM-IV-TR diagnosis of somatization or somatoform disorder. However, somatization disorder terminology will be changed to simple and complex somatic symptom disorders in DSM-V. Another limitation of this study was that we could not analyze an association between MUPS and comorbid psychiatric diagnoses. In the hospital where this study was done, the patients presenting to the clinics had only their prescriptions, without a documented diagnosis. Finally, this study was limited by the cross-sectional design.
CONCLUSIONS AND FUTURE DIRECTIONS
To our knowledge this is the first psychosocioeconomic study of MUPS done in Kerala, India. More studies are warranted focusing on non-pharmacological treatment and psycho-education on mind–body association and medical models for this public health problem. Future studies should also shed light on specific cytokines associated with MUPS for personalized management, which is a National Institute of Mental Health mission and priority. There is also a need for studies to examine the effect of a combination of antidepressants and cognitive behavioral therapy on MUPS.
ACKNOWLEDGMENTS
Kerala Research Program on Local Level Development and the Center for Development Studies funded this study. The manuscript preparation by Maju Koola was supported by the NIMH funded T32 grant (MH067533-07; William T. Carpenter, MD, Principal Investigator). We acknowledge Dr. K. Anitha, the research staff, for enrolling and interviewing patients. We thank the services of Mr. Humayoon Kabeer, Librarian of Medical College Library for gathering the references of interest.
Footnotes
Source of Support: Kerala Research Program on Local Level Development and the Center for Development Studies; NIMH funded T32 grant (MH067533-07; William T. Carpenter, MD, Principal Investigator)
Conflict of Interest: None.
REFERENCES
- 1.Goldberg DP, Bridges K. Somatic presentations of psychiatric illness in primary care setting. J Psychosom Res. 1988;32:137–44. doi: 10.1016/0022-3999(88)90048-7. [DOI] [PubMed] [Google Scholar]
- 2.Escobar JI, Gara M, Silver RC, Waitzkin H, Holman A, Compton W. Somatisation disorder in primary care. Br J Psychiatry. 1998;173:262–6. doi: 10.1192/bjp.173.3.262. [DOI] [PubMed] [Google Scholar]
- 3.Hariharan G, Ramakrishnan AN, Mathrubootham N. A study of somatization disorder in an industrial hospital. Indian J Psychiatry. 1993;35:200–2. [PMC free article] [PubMed] [Google Scholar]
- 4.Bener A, Ghuloum S, Al-Mulla AA, Al-Marri S, Hashim MS, Elbagi IE. Prevalence of somatisation and psychologisation among patients visiting primary health care centres in the State of Qatar. Libyan J Med. 2010;16:5. doi: 10.3402/ljm.v5i0.5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Rufaie OE, Al Sabossy MM, Bener A, Ali TA, Abuzeid MS. Somatization among primary care Arab patients. J Psychosom Res. 1999;46:549–55. doi: 10.1016/s0022-3999(98)00101-9. [DOI] [PubMed] [Google Scholar]
- 6.Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59(Suppl 20):15–21. [PubMed] [Google Scholar]
- 7.Burton C. Beyond somatisation: A review of the understanding and treatment of medically unexplained physical symptoms (MUPS) Br J Gen Pract. 2003;53:231–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell SM, Roland MO. Why do people consult the doctor? Fam Pract. 1996;13:75–83. doi: 10.1093/fampra/13.1.75. [DOI] [PubMed] [Google Scholar]
- 9.Salmon P, Woloshynowych M, Valori R. The measurement of beliefs about physical symptoms in English general practice patients. Soc Sci Med. 1996;42:1561–7. doi: 10.1016/0277-9536(95)00263-4. [DOI] [PubMed] [Google Scholar]
- 10.Peters S, Stanley I, Rose M, Salmon P. Patients with medically unexplained symptoms: Sources of patients’ authority and implications for demands on medical care. Soc Sci Med. 2001;46:559–65. doi: 10.1016/s0277-9536(97)00200-1. [DOI] [PubMed] [Google Scholar]
- 11.Escobar JI, Burnam MA, Karno M, Forsythe A, Golding JM. Somatization in the community. Arch Gen Psychiatry. 1987;44:713–8. doi: 10.1001/archpsyc.1987.01800200039006. [DOI] [PubMed] [Google Scholar]
- 12.Aragones E, Labad A, Pinol JL, Lucena C, Alonso Y. Somatised depression in primary care attenders. J Psychosom Res. 2005;58:145–51. doi: 10.1016/j.jpsychores.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Noyes R, Holt CS, Kathol RG. Somatisation diagnosis and management. Arch Fam Med. 1995;45:790–5. doi: 10.1001/archfami.4.9.790. [DOI] [PubMed] [Google Scholar]
- 14.Hiller W, Rief W, Brähler E. Somatization in the population: From mild bodily misperceptions to disabling symptoms. Soc Psychiatry Psychiatr Epidemiol. 2006;41:704–12. doi: 10.1007/s00127-006-0082-y. [DOI] [PubMed] [Google Scholar]
- 15.Hessel A, Geyer M, Schumacher J, Brahler E. Somatoform complaints in the German population. Z Psychosom Med Psychother. 2002;48:38–58. doi: 10.13109/zptm.2002.48.1.38. [DOI] [PubMed] [Google Scholar]
- 16.Broers T, Hodgetts G, Batic-Mujanovic O, Petrovic V, Hasanagic M, Godwin M. Prevalence of mental and social disorders in adults attending primary care centers in Bosnia and Herzegovina. Croat Med J. 2006;47:478–84. [PMC free article] [PubMed] [Google Scholar]
- 17.Woolfolk R, Allen L. Treating somatization: A cognitive-behavioural Approach. New York: Guilford Press; 2007. [Google Scholar]
- 18.Garcia-Campayo J, Sanz-Carrillo C. A review of the differences between somatizing and psychologizing patients in primary care. Int J Psychiatry Med. 1999;29:337–45. doi: 10.2190/FMJ2-UK3Y-FKB8-DCGN. [DOI] [PubMed] [Google Scholar]
- 19.Kirmayer LJ, Robbins JM. Patients who somatize in primary care: A longitudinal study of cognitive and social characteristics. Psychol Med. 1996;26:937–51. doi: 10.1017/s0033291700035273. [DOI] [PubMed] [Google Scholar]
- 20.Cape J, McCulloch Y. Patients’ reasons for not presenting emotional problems in general practice consultations. Br J Gen Pract. 1999;49:875–9. [PMC free article] [PubMed] [Google Scholar]
- 21.Cameron L, Leventhal EA, Leventhal H. Seeking medical care in response to symptoms and life stress. Psychosom Med. 1995;57:37–47. doi: 10.1097/00006842-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Williams S, Weinman J, Dale J, Newman S. Patient expectations: What do primary care patients want from the GP and how far do meeting expectations affect patient satisfaction? Fam Pract. 1995;12:193–201. doi: 10.1093/fampra/12.2.193. [DOI] [PubMed] [Google Scholar]
- 23.Potts SG, Bass CM. Psychological morbidity in patients with chest pain and normal or near normal coronary arteries: A long-term follow-up study. Psychol Med. 1995;25:339–47. doi: 10.1017/s0033291700036242. [DOI] [PubMed] [Google Scholar]
- 24.Coia P, Morley S. Medical reassurance and patients’ responses. J Psychosom Res. 1998;45:377–86. doi: 10.1016/s0022-3999(98)00047-6. [DOI] [PubMed] [Google Scholar]
- 25.Dohrenwend A, Skillings J. Diagnosis-specific management of somatoform disorders: Moving beyond “vague complaints of pain”. J Pain. 2009;10:1128–37. doi: 10.1016/j.jpain.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Katon W, Ries RK, Kleinman A. The prevalence of somatization in primary care. Compr Psychiatry. 1984;25:208–15. doi: 10.1016/0010-440x(84)90009-9. [DOI] [PubMed] [Google Scholar]
- 27.Smith GR, Jr, Monson RA, Ray DC. Patients with multiple unexplained symptoms. Their characteristics, functional health, and health care utilization. Arch Intern Med. 1986;146:69–72. [PubMed] [Google Scholar]
- 28.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology and psychosomatic medicine: Back to the future. Psychosom Med. 2002;64:15–28. doi: 10.1097/00006842-200201000-00004. [DOI] [PubMed] [Google Scholar]


