Abstract
Subdural hematoma is a rare but serious complication following electroconvulsive therapy (ECT), a frequently used treatment modality in the management of various psychiatric morbidities including bipolar affective disorder (BAD). There are very few reports of intracranial bleeding following ECT in the literature. A 38-year-old female, known case of BAD for last fifteen years receiving ECT, presented with the symptoms of dysphasia, headache, left sided paresis, and sudden deterioration of sensorium. Computed tomography (CT) scan of the brain was suggestive of left-sided fronto parietal chronic subdural hematoma with midline shift that was drained successfully.
Keywords: Electroconvulsive therapy, subdural hematoma complication, rare
INTRODUCTION
Electro convulsive therapy (ECT) is an effective treatment modality in the management of depression, mania, bipolar affective disorder (BAD), schizophrenia as well as a number of psychiatric disorders since 1930s. Complications of ECT like subdural hematoma (SDH), intracerebral hemorrhage (ICH), have been reported in the literature sparsely. Few anecdotal cases of this neurological complication are described.[1] We report a case of chronic SDH in a 38-year-old lady resulting from ECT for management of BAD.
CASE REPORT
A 38-year-old lady who was a known case of BAD for last fifteen years presented with increasingly agitated behaviour along with intense mood fluctuations for last six months. She underwent ECT under anesthesia for the management of same. She had a total of 12 sessions over a period of six weeks when she developed frontal headache and frequent vomiting with increasing frequency for last three weeks. There was additional history of altered sensorium, agitation, slurring of speech (dysphasia), and weakness of the right side of the body without loss of consciousness or seizure.
On examination by the neurosurgeon and performance of computed tomography (CT) scan of the brain, a left temporo-parietal subdural hematoma with midline shift was revealed [Figures 1 and 2]. Craniotomy was performed under monitored anaesthesia care and the hematoma was evacuated. Postoperative period was uneventful.
Figure 1.
Computed tomography scan of the brain showing post electro convulsive therapy subdural hematoma
Figure 2.
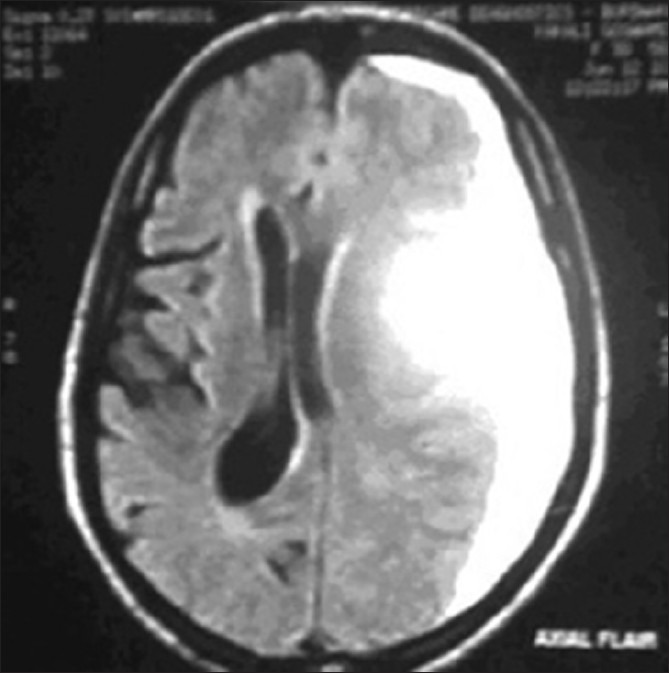
CT scan of the brain showing post ECT subdural hematoma
DISCUSSION
Owing to the similarity of symptoms with ECT, the diagnosis of chronic subdural hematoma following ECT is difficult in clinical practice. ECT is a well accepted treatment modality for severe mental illness in which a short application of electrical stimulus is used to produce a generalized motor seizure. The generalized seizure lasts several minutes and includes a short 10-15 seconds tonic phase followed by a more prolonged clonic phase, lasting for 30-60 seconds. This form of treatment increases cortical GABA concentrations and enhances serotonergic function. Neuronal structure and synaptic plasticity also appear to be influenced.
Most patients scheduled to undergo ECT are receiving tricyclic antidepressants (TCAs), monoamine, selective serotonine reuptake inhibitors (SSRIs), lithium carbonate, or a combination of these drugs. TCAs usually increase the sympathetic tone. The newer drugs such as trazodone and bupropion have lesser complications.[2–4] Lithium carbonate prolongs the action of neuromuscular blockade.[5] Patients receiving lithium may demonstrate more cognitive side effects after ECT. Therefore, pre-ECT workup should include a complete medical and neurologic evaluation of the patients. ECT can be used safely in elderly patients and in persons with cardiac pacemakers or implantable cardioverter-difibrillators. ECT can also be used safely during pregnancy in consultation with an obstetrician.
The central nervous system response of ECT includes increased cerebral blood flow and ICP. Generalised autonomic nervous system stimulation causes an initial bradycardia and occasional asystole, followed by a more prominent sympathetic response of hypertension and tachycardia. Occasionally cardiac dysrrhythmia, myocardial ischaemia, infarction, or neurologic vascular events may be precipitated.
The adverse effects of ECT can be divided into two groups. First, the medical complications that can be substantially reduced by the use of appropriately trained staffs, best equipments, and best methods of administration of therapy. Other one being often expected transient memory loss and post treatment confusions. The mortality rate with ECT is about 0.002% per treatment and 0.01% per patient. These numbers are comparable with general anesthesia and childbirth.[6] Death due to ECT is mostly from cardiovascular and hemodynamic complications and occur most frequently in patients with already compromised cardiovascular profile. The adverse effects of ECT includes laryngospasm, circulatory insufficiency, headache, emergence agitation, tooth damage, vertebral compression fractures, status epilepticus, peripheral nerve palsy, skin burns, and prolonged apnea. Common adverse effects associated with ECT are headache, nausea, fatigue, confusion, and delirium, shortly after the seizure while the patient is recovering from anesthesia. Marked confusion may occur in up to 10% of patients within 30 minutes of the seizure and can be treated with barbiturates and benzodiazepines. Delirium is usually most pronounced in after the first few treatments and in patients who received bilateral ECT or those who have co-existing neurological disorders.[6] High risk group of patients for ECT include those with recent myocardial infarction and/or ischemia, uncontrolled blood pressure, intracranial SOL, and previous spinal injuries.[7,8] Memory loss is most often reported by patients who have experienced little improvement after ECT.
Intracranial hematoma is a serious but rare complication following ECT. The incidence of intracranial hematoma after ECT seems to be underestimated in the literature. Few cases of neurological complications such as ICH and SDH were not found to increase or deteriorate following ECT thereby establishing the safety of this procedure in patients with such neurological complications.[9,10] Although it is difficult to establish the diagnosis of intracranial hemorrhage as iatrogenic, but any change in mental status, worsening of symptoms, or development of focal neurological abnormality in patients undergoing ECT should be treated with utmost urgency and investigated with a CT scan of brain to rule out intracranial complications. CT scan really helped us in diagnosing and treating our case.
This case report and other publications suggest that one cannot rely only on clinical symptoms when symptoms worsen after ECT, although ECT is a safe procedure. Failure to recognize these rare cases of SDH can have permanent and fatal consequences.
CONCLUSION
ECT is a generally safe technique but having potentially dangerous complications. Therefore, it is important to investigate those patients who are having neurological signs and symptoms following ECT and a CT or magnetic resonance imaging (MRI) scan should be performed appropriately. Anticipation of complications along with their early diagnosis and treatment are the most important factors in delivering a comprehensive ECT.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Awasthy N, Chand K. Subdural hematoma- a complication of electroconvulsive therapy. Pak J Med Sci. 2005;21:491–3. [Google Scholar]
- 2.Potter WZ, Rudorfer MV, Manji H. The pharmacologic treatment of depression. N Engl J Med. 1991;325:633–42. doi: 10.1056/NEJM199108293250907. [DOI] [PubMed] [Google Scholar]
- 3.Pritchett JT, Bernstein HJ, Kellner CH. Combined ECT and antidepressant drug therapy. Convuls Ther. 1993;9:256–61. [PubMed] [Google Scholar]
- 4.Naguib M, Koorn R. Interactions between psychotropics, anaesthetics and electroconvulsive therapy: Implications for drug choice and patient management. CNS Drugs. 2002;16:229–47. doi: 10.2165/00023210-200216040-00003. [DOI] [PubMed] [Google Scholar]
- 5.Mukherjee S. Combined ECT and lithium therapy. Convuls Ther. 1993;9:274–84. [PubMed] [Google Scholar]
- 6.Kaplan and Sadock's Synopsis of Psychiatry. 9th ed. Lippincott Williams and Wilkins; Electroconvulsive Therapy; pp. 1138–44. 36.5. [Google Scholar]
- 7.Electroconvulsive Therapy. NIH Consensus Statement Online. 1985;5:1–23. [Google Scholar]
- 8.Nuttall GA, Bowersox MR, Douglass SB, McDonald J, Rasmussen LJ, Decker PA, et al. Morbidity and Mortality in the Use of Electro Convulsive Therapy. J ECT. 2004;20:237–41. doi: 10.1097/00124509-200412000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Malek-Ahmadi P, Beceiro JR, McNeil BW, Weddige RL. Electro Convulsive Therapy and Chronic Subdural Hematoma. Convuls Ther. 1990;6:38–41. [PubMed] [Google Scholar]
- 10.Wijeratne C, Shome S. Electroconvulsive therapy and subdural hemorrhage. J ECT. 1999;15:275–9. [PubMed] [Google Scholar]


