Abstract
Food allergies are emerging health risks in much of the Western world, and some evidence suggests prevalence is increasing. Despite lacking scientific consensus around prevalence and management, policies and regulations are being implemented in public spaces (e.g., schools). These policies have been criticized as extreme in the literature, in the media, and by the non-allergic population. Backlash appears to be resulting from different perceptions of risk between different groups. This article uses a recently assembled national dataset (n = 3,666) to explore how Canadians perceive the risks of food allergy. Analyses revealed that almost 20% self-report having an allergic person in the household, while the average respondent estimated the prevalence of food allergies in Canada to be 30%. Both of these measures overestimate the true clinically defined prevalence (7.5%), indicating an inflated public understanding of the risks of food allergies. Seventy percent reported food allergies to be substantial risks to the Canadian population. Multivariate logistic regression models revealed important determinants of risk perception including demographic, experience-based, attitudinal, and regional predictors. Results are discussed in terms of understanding emerging health risks in the post-industrial era, and implications for both policy and risk communication.
Keywords: risk perception, determinants, emerging risk, food allergies, Canada
INTRODUCTION
Food allergies (e.g., peanut, shellfish) are an emerging and important public health issue, affecting up to 4% of adults, and up to 6% of children; and there is some evidence that these rates are increasing (Grundy et al. 2002; Sicherer et al. 2003; Branum and Lukacs 2008). Allergic reactions to foods range in severity from swelling of the lips, rash, and hives to difficulty breathing, asthma, nausea, and diarrhea. The most severe form of allergic reaction, anaphylaxis, is life-threatening and affects the cardiovascular, respiratory, and gastrointestinal systems simultaneously. Due to a lack of curative therapies, allergic individuals must rely on strict avoidance of allergens, and symptomatic treatment of reactions (Kagan 2003). However, accidental exposures are frequent (Branum and Lukacs 2008), and fear of exposure can have significant psychosocial impacts on allergic individuals and their families (Uguz et al. 2005; Primeau et al. 2000), particularly in interactions with the world outside the home (e.g., schools, airplanes, restaurants).
The emergence of food allergies as health risks has been relatively recent, and its etiology remains unknown. The result has been growing interest from the mass media, science, and the commercial sector, particularly as policy-makers attempt to respond to the demands of affected individuals (Nettleton et al. 2009). There is also a perception among the general population that food allergies are much more prevalent than systematic estimates suggest, with lay estimates of prevalence often exceeding 30% (Rona et al. 2007). This inflated perception of risk has resulted in important policy debates related to protection versus rights, particularly around those developed in response to the disproportionate burden of food allergies in children. If the rates of food allergies are indeed increasing, it will be necessary to develop and integrate appropriate risk management strategies in a wide variety of settings. Understanding the perception of the risks of food allergies from the perspective of those directly and indirectly affected can inform emerging and future policy initiatives.
Food allergies are one of a number of emerging health risks defined as risks that are: (1) previously unknown (e.g., genetically modified organisms [GMOs]); (2) previously unrecognized (e.g., use of Bisphenol A in baby bottles); (3) new manifestations of existing risks (e.g., H1N1 flu virus); or (4) due to changes in public perception over time (e.g., lowered tolerance of pollution from heavy industry in post-industrial society (Beck 1992)). Investigations of the determinants of risk perceptions within the dominant econometric and psychometric approaches to risk perception have focused primarily on either demographic factors and/or characteristics of the hazard itself (e.g., catastrophic potential, knowledge about the risk, equitable distribution) (Slovic 2000). Alternative theories argue that risk perceptions are rooted in social and cultural contexts, and that individuals and social groups collectively select the risks to be concerned about based on threats to their worldviews or ways of life (Douglas and Wildavsky 1982). These approaches have contributed in important ways to understanding the perception of some risks (e.g., nuclear power), and the risk communication process (Kasperson et al. 1988). However, they have been limited in anticipating public response to emerging health risks (Sjöberg 2000), despite the fact that these have been recognized as requiring a unique risk management approach (Radandt and Renn 2008). This article seizes on a unique opportunity, using a recently assembled national dataset, to explore the determinants of the (perceived) risks of food allergies as they emerge.
RESEARCH CONTEXT
Food allergies are hypersensitive responses to food proteins where the immune system, through the production of specific IgE antibodies against these proteins, activates mast cells to release histamine (Kagan 2003). Histamine can affect with varying severity the respiratory and cardiovascular systems, the gastrointestinal tract, and the skin. Although they typically develop during childhood, allergies may develop at any time during the lifespan, and symptoms range from swelling of the lips, rash, and hives to diarrhea, vomiting, and difficult breathing. Eight foods are responsible for more than 90% of food allergies, and while some (egg, wheat, soy, and milk) resolve in childhood, allergies to peanut, tree nut, shellfish, and fish are typically lifelong (Al-Muhsen et al. 2003). Anaphylaxis is a life-threatening allergic reaction that affects more than one biological system and can be fatal. Foods are the primary cause of these reactions as well as associated hospitalizations (Liew et al. 2009). Currently, there is no cure for food allergies, and allergic individuals must rely on a strict avoidance diet, as well as symptomatic treatment of reactions (e.g., with the use of an epinephrine auto-injector). Psychosocial impacts including lower quality of life compound the risk of physical harm for food allergy sufferers and their caregivers (Uguz et al. 2005; Primeau et al. 2000).
Current estimates indicate that food allergies affect a substantial proportion of the Canadian population, with prevalence estimated to be up to 6% for children, and 1–3% for adults, with 1–2% of these individuals living with the potential risk of a fatal anaphylactic reaction (Health Canada 2009). These estimates are comparable to those in the United States (4 with varying severity 8% for children, 2% adults) and the United Kingdom (2 with varying severity 5% overall prevalence) (Branum and Lukacs 2008; Mills et al. 2007). However, estimates of prevalence are dependent on the methodologies used for diagnosis. For example, population-based studies using self-reported measures tend to overestimate allergy prevalence (in comparison with more objective diagnostic tools) (Rona et al. 2007). This overestimate is due to the propensity for individuals to classify all forms of eating discomfort (e.g., a food intolerance) as a food “allergy.” Although establishing precise population-based estimates has its difficulties, several time-series studies using rigorous diagnostic tests indicate that food allergies have become increasingly prevalent over the past few decades, and particularly in the Western world (Madsen 2005; Sicherer et al. 2003; Grundy et al. 2002). The recent and apparently substantial rise in the prevalence of food allergy has scientists perplexed about their etiology. Increases have occurred over too short a timeline to be explained by any genetic shift in the population (Bloomfield et al. 2006). This suggests that environmental factors, broadly defined, are interacting in some way with genetic susceptibility to produce the rising prevalence, however, investigations into establishing a causal pathway are ongoing (e.g., Subbaro et al. 2009).
As a result of (perceived) increases in prevalence and lack of scientific consensus regarding etiology (Ben-Shoshan et al. 2009; Venter et al. 2010), food allergies are gaining increasing interest in the media, political, and commercial sectors (Nettleton et al. 2009). Food allergies have become a central fixture on the regulatory agenda, particularly in Canada, the United States, New Zealand, Australia, and the United Kingdom (Schnieder Chafen et al. 2010). Perceived increases have prompted various responses from decision-makers, despite a lack of science-based management guidelines. This has resulted in inconsistent risk management strategies (e.g., precautionary statements on packaged foods, allergen bans in public spaces) that are often developed on a case-by-case basis (Madsen et al. 2010). For example, the school policy environment is incredibly varied with respect to anaphylaxis risk management policy. In Canada, for example, each province and territory has independent governance for schools, and each have approached allergies and anaphylaxis differently. For instance, the province of Ontario enacted a law in 2006 for all publicly funded schools. Known as Bill 3 (or Sabrina's Law, named for the 13-year-old who died in her school cafeteria from an anaphylactic reaction), this is designed to ensure that all schools are accountable for training and education of staff, and overall management of pupils with anaphylactic allergies. Policies in other provinces range widely, (some have no policy whatsoever), and often school boards or individual schools develop their own management plan. Despite the well-meaning nature of implemented policies, there has been tremendous backlash from the non-allergic population. Non-allergic individuals and/or parents of non-allergic children often oppose “allergen-free” environments (e.g., nut-free schools) due to their perception of severely limited food choices. In the case of peanut allergies in particular, banning peanut butter raises issues of equity for low-income populations, as peanut butter represents an accessible, affordable source of protein.
In recent decades, the politics around food have shifted from issues of access and nutrition, to issues of risk due to a number of key debates (e.g., use of genetically modified foods), and food-borne disease outbreaks (e.g., BSE) (Blue 2010; Pollan 2008). Such food-related hazards have resulted in increased and deserved involvement by the public in food risk governance (Krom and Mol 2010). Food allergies represent a new food-related risk that is altering the political landscape, and those responsible for regulation and manufacturing such emerging risks need to incorporate the public's perspective in their decisions (Scholz and Siegrist 2010). Madsen and colleagues (2010) have taken important steps toward developing a consensus on acceptable risk from a number of stakeholders in the food allergy debate. However, they exclude the general population due to lack of knowledge regarding how they perceive food allergy risk. In this article, we argue that as decisions continue to be made, the perspective of the general population needs to be understood and addressed to ensure successful uptake and long-term sustainability.
Although the non-allergic population is unaffected in terms of physical risk, they are indirectly affected by these decisions as general consumers, and should be considered important actors in the debate around food allergies (Shaw 2002). Thus, this article aims to establish a knowledge base for risk management policy by endeavoring to answer the following questions:
-
1.
How does the general Canadian population perceive the risks of food allergies, relative to other environmental hazards?
-
2.
What are the demographic, experiential, and attitudinal determinants of food allergy risk perception?
-
3.
Is there a potential role for the policy environment as a determinant of the perception of food allergy risk?
The first of these objectives will be addressed by situating the perceived risk of food allergies among 26 other environmental health hazards currently facing Canadians by ranking each of the hazards as “High,” “Moderate,” “Slight,” “Almost No,” and “No risk” to the general population. To address the second objective, regress the likelihood that respondents would rate the risks as “High” or “Moderate” versus lower ratings against demographic, attitudinal, and experiential independent factors. Finally, to explore the potential role of the policy environment as a determinant of risk perception, we investigate regional (provincial) differences in the perception of food allergy risk. The details of this methodology are explained in the following section of the article.
METHODS
The data used to answer the research questions posed by this article were collected as part of the Surveying Canadians to Assess the Prevalence of Common Food Allergies and Attitudes Towards Food Labeling and Risk (SCAAALAR) survey, funded by a Canadian research network (AllerGen 2011) in collaboration with Health Canada. The survey had three overarching objectives: (1) to assess the prevalence of food allergies in Canada, (2) to assess societal attitudes towards allergen precautionary statements on packaged foods, and (3) to explore the perception of food allergy and anaphylaxis risk. This article is informed primarily by the data collected for the third objective, but also uses the self-reported prevalence data collected in pursuit of the first objective.
The survey was administered in the 10 Canadian provinces between June 2008 and March 2009. Households were selected randomly from the electronic White Pages, and surveys were conducted in both official languages (French, English) using Computer Assisted Telephone Interviewing. Prior to first contact, letters of information were sent to each household. Of 10,596 households where contact was made, 3666 households responded resulting in an overall response rate of 35%. Recent trends indicate a general decline in survey response rates and current literature indicates that lower response rates do not necessarily indicate non-response bias (Lee et al. 2009). That is, while decreasing non-response rates reduces the risk of bias, it does not necessarily reduce the bias itself (Groves 2006). Potential bias related to self-selection in this research has been minimized by the random sampling strategy, and given the large sample size we are confident that the relationships reported are internally valid.
Allergic household status was measured within the survey in several ways: self-report, convincing history, physician diagnosis, and confirmatory follow-up with a physician (Ben-Shoshan et al. 2010). Given the focus in this article on the role of lay assessments of risk, as well as the documented similarities between possible and probable food allergies (Ben-Shoshan et al. 2010), self-report was an appropriate metric to use in this analysis for defining directly affected households. Respondents with no allergies in the household were further classified as being indirectly affected, if they had ever served, prepared, or bought food for an allergic person or an allergen-controlled environment.
The survey collected attitudinal data about health risks from the general to the specific. For example, respondents were asked to provide up to three open-ended responses about the greatest problems currently facing the Canadian population. Respondents were also asked about current health risks posed to themselves, their families, and the general Canadian public. As such, each of these items were constructed to measure concern about potential impacts of the environment on respondents’ health, to provide some insight into their general attitudes toward environmental health risks (as food allergies arise from gene-environment interactions, they are by definition an environmental health risk). In the interest of efficiency and data reduction, six of these eight survey items were used to construct a Health Risk Perception Scale, which had a Cronbach alpha value of 0.74 indicating good inter-item correlation (Table 1). The two items that were removed from the scale were not consistent with the apparent face validity and inter-item correlation of the scale, and were thus removed.
Table 1.
Health risk perception scale survey items by frequency of response.
| Statement/Question | Mean | Std. Deviation |
|---|---|---|
| The environment is a major concern for Canadians.a | 4.00 | 1.03 |
| The environment should be a major concern for Canadians.a | 4.39 | 0.72 |
| Environmental impacts on health are a major concern for Canadians.a | 3.93 | 1.10 |
| Environmental impacts on health should be a major concern for Canadians.a | 4.37 | 0.70 |
| How worried are you that the environment can impact your health?b | 3.99 | 1.24 |
| How worried are you that the environment can impact the health of your family?b | 4.16 | 1.14 |
| There are risks where I livea,* | 3.03 | 1.49 |
| My community is becoming a healthier place to livea,* | 2.95 | 1.17 |
Scale ranged from (1) “Strongly Disagree” to (5) “Strongly Agree.”
Scale ranged from (1) “Not Worried at All” to (5) “Very Worried.”
Items removed from the scale due to poor inter-item reliability
Questions about food allergies specifically were designed to assess respondents’ perception of the prevalence of food allergy, general knowledge, as well as related symptoms, triggers, and risks. Indicators of self-rated concern about food allergies, and recall of food allergy-related information received in the past six months were also collected.
Previous knowledge and past experiences are known mediating factors for what one considers risky, and expects from new risks (Zinn 2008). Among others, Sjöberg (1996) has argued for attitudes toward risk as an important explanatory factor for risk perceptions. The central thesis is that attitudes toward risks, both personal and general, will guide perceptions of specific risks. The survey measured level of agreement with seven statements measuring five worldviews thought to be important for risk perception (fatalism, hierarchy, individualism, egalitarianism, and technological enthusiasm) used previously in a study of Canadians’ health risk perceptions (Health Canada 1993). Worldviews (Dake 1991; Wildavsky and Douglas 1982) are one example of general risk attitudes, developed as individuals take stock of the environments in which they live (Slovic 2000), and form an orienting disposition toward risk.
Following the methodology employed by Krewski and colleagues (1995, 2006a,b) respondents were also asked to rate the degree of health risk posed to the Canadian public for 27 hazards. These hazard ratings were measured on a 5-point Likert scale ranging from “No risk at all” to “High risk.” Items cover a range of hazards including technological (e.g., nuclear power), social (e.g., crime and violence), environmental (e.g., air quality), and lifestyle-related (e.g., stress). Most items were retained from previous work (Krewski et al. 2006a,b) while others with particular topical interest, including food allergies, anaphylaxis, and lead in paint were added. Hazard ratings for risks were recoded to represent high risk (i.e., “High” and “Moderate”), versus low risk (i.e., “Slight,” “Almost No,” and “No”). Respondents with no opinion were collapsed into the low risk category.
Demographic characteristics were collected at the end of the survey. It is important to note that there were a number of individuals (n = 1210) for whom an income value had to be generated using a hot-decking imputation. This approach imputes a randomly selected value for household income from a donor case from within the sample based on age, education, household composition (e.g., lone adult family), and province of residence. This “approximate Bayesian bootstrap” approach has been used successfully by the United States Census Bureau (Allison 2002) and others (Law et al. 2005).
Weighted logistic regression was used to explore the determinants of food allergy risk perception. The sample was weighted on the variables age and sex (five-year categories) to the structure of the 2006 Canadian population (Statistics Canada 2009). Probability weights were appended to the sample for each respondent, and used to weight the regression analysis. Z-statistics and likelihood ratio tests were used to test the significance of each variable to the overall fit of the model, and insignificant variables were removed. This model was verified using backward stepwise model selection. Interaction terms based on all possible pairs of variables were added to the main effects model one at a time. Overall model fit was assessed using the rho-squared statistic and the Hosmer-Lemeshow goodness-of-fit test. All analyses were carried out using R v. 2.13.0.
RESULTS
Sample Characteristics
Compared to the structure of the 2006 Canadian population, the SCAAALAR sample had a higher proportion of females (65.1%), older respondents, and Canadian-born respondents (85.6%) (Table 2). It is also clear that respondents with lower levels of socioeconomic status (SES), as measured by education and household income, were underrepresented. For example, 9.3% of the sample had less than secondary school as their highest level of education, compared to 23.8% of the Canadian population. Respondents from Quebec (39.3%) made up a greater proportion of the sample relative to the national population (24.3%).
Table 2.
SCAAALAR sample characteristics (n = 3462) compared to the 2006 Canadian population.
| Respondents (%) | Canada (%)a | |
|---|---|---|
| Gender | ||
| Male | 34.9 | 48.3 |
| Female | 65.1 | 51.7 |
| Age (mean = 51.6, std. deviation = 15.1) | ||
| 18–29 | 8.4 | 19.8 |
| 30–39 | 14.7 | 17.1 |
| 40–49 | 20.5 | 21.2 |
| 50–59 | 25.2 | 18.0 |
| 60–69 | 18.8 | 11.4 |
| 70+ | 12.3 | 12.5 |
| Education | ||
| Less than secondary school | 9.3 | 23.8 |
| Secondary school/some college or university | 30.2 | 42.7 |
| College or university | 47.6 | 28.9 |
| Master's/Ph.D./professional degree | 12.9 | 4.6 |
| Immigrant status | ||
| Born in Canada | 85.6 | 80.0 |
| Immigrant | 14.4 | 20.0 |
| Marital status | ||
| Married | 57.2 | 47.9 |
| Separated/divorced | 9.4 | 11.0 |
| Widowed | 5.9 | 6.2 |
| Living with a partner/never married | 27.6 | 34.9 |
| Household income | ||
| Less than $20,000 | 4.6 | 6.9 |
| $20,000–$849,999 | 24.1 | 27.9 |
| $50,000–$99,999 | 43.1 | 39.9 |
| More than $100,000 | 28.1 | 25.3 |
| Region of residence | ||
| British columbia | 10.3 | 13.3 |
| Prairie (Alberta, Saskatchewan, Manitoba) | 12.0 | 16.7 |
| Ontario | 32.9 | 38.3 |
| Quebec | 39.3 | 24.3 |
| Atlantic (Nova Scotia, New Brunswick, Newfoundland, Prince Edward Island) | 5.4 | 7.4 |
Source: Statistics Canada (2009).
Twenty percent of survey respondents (n = 688) reported having at least one food allergy in the household. Of these, 131 reported having allergic children in the household, and 112 reported having multiple allergic individuals. More than 50% of the sample reported being at least indirectly affected by food allergies (688 directly [19.9%], 1061 indirectly [30.7%]). Of respondents, 44% recalled hearing or receiving some information about food allergies in the previous six months, and 1433 (41.4%) reported being more concerned about the risks associated with food allergy compared to others. In terms of knowledge about food allergies, almost all respondents (95%) knew that even a tiny amount of allergen could cause a reaction, and 42% thought that reactions to allergens were easily treatable. Respondents’ estimates of the percentage of Canadians with food allergies ranged from 0% to 100%, with a mean value of 30.6% (median 25.0%), indicating an inflated perception of prevalence compared to current systematic estimates (Ben-Shoshan et al. 2010).
Of 5638 total open-ended responses to “What are the greatest concerns facing Canadians today?,” environmental concerns (e.g., climate change, air/water pollution, garbage/waste) were overwhelmingly represented, comprising 27% of the total response sample. This was followed by economic issues related to the 2008/09 economic downturn (10%), and issues associated with overweight and obesity (e.g., diet, physical activity) (8% of all mentions). Issues related to allergy and asthma were the seventh most frequently mentioned problem (3.5%), behind health care (6.9%), energy costs (4.0%), and cost of living (3.7%). Due to the potential role of the environment in the etiology of food allergies, respondents were asked questions about the impact of the environment on their health. Worry and concern about environmental impacts on health were consistently expressed by the majority of respondents. For example, 40.9% of respondents were very worried about environmental impact on their health while 41.0% where somewhat worried.
To illustrate how the general population perceives the risks of food allergy and anaphylaxis relative to other environmental health risks in Canada, shown in Figure 1 are the perceived levels of risk for the 27 environmental hazards. The top five risks were obesity (92.3% rated as high), cigarettes (91.4%), stress (90.9%), chemical pollution (88.7%), and smog and air quality (85.0%). The lowest three risks were laser eye surgery (22.1%), alternative health products (28.1%), and vaccines (31.7%). Food allergies and anaphylaxis risk were rated approximately in the middle range of the hazards, rated highly by 69.6% and 60.1%, respectively, among hazards such as: bacteria in foods, nuclear waste, flu epidemics, and genetically modified organisms.
Figure 1.
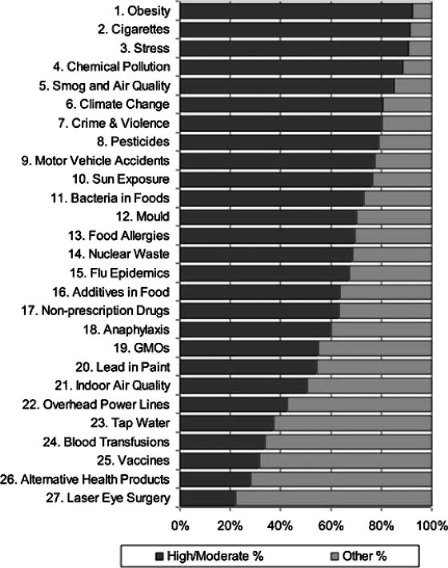
Perceived level of risk to the Canadian public for 27 health hazards.
Regression Results
Weighted logistic regression analysis was conducted to characterize the perception of risk around food allergy. Coefficients are presented here as odds ratios (ORs) with 95% confidence intervals (CIs). With the exception of the risk perception scale, odds ratios for each variable can be interpreted as the odds of a respondent to rate the risk of food allergy as high, relative to the reference category of the variable, while controlling for all other variables in the model. The regression model (Table 3) achieved a rho-square of 0.15 with 67.9% of cases correctly classified, based on a cutoff calculated as the mean fitted value.
Table 3.
Logistic regression results: perceived food allergy risk.
| Explanatory Variables | Adjusted Odds Ratio | 95% Confidence Interval | Signif.a |
|---|---|---|---|
| Sociodemographics | |||
| Female (ref.) | 1.00 | — | — |
| Male | 0.59 | (0.50, 0.69) | *** |
| Age: 18–29 (ref.) | 1.00 | — | — |
| Age: 30–39 | N/S | — | — |
| Age: 40–49 | N/S | — | — |
| Age: 50–59 | 1.39 | (1.11, 1.74) | ** |
| Age: 60–69 | 1.43 | (1.09, 1.89) | * |
| Age: 70–79 | 1.60 | (1.15, 2.23) | ** |
| Household: >1 adult, no minor(s) (ref.) | 1.00 | — | — |
| Household: >1 adult and minor(s) | 1.26 | (1.04, 1.53) | * |
| Household: lone adult and minor(s) | 1.99 | (1.17, 3.51) | * |
| Immigrant status: Canadian born (ref.) | 1.00 | — | — |
| Immigrant status: less than 10 years | 2.51 | (1.48, 4.47) | ** |
| Immigrant status: 10 or more years | 0.80 | (0.62, 1.04) | ** |
| Household income: less than $20,000 (ref.) | 1.00 | — | — |
| Household income: $20,000–59,999 | 0.67 | (0.42, 1.04) | ** |
| Household income: $60,000–99,999 | 0.61 | (0.38, 0.96) | * |
| Household income: $100,000+ | 0.62 | (0.38, 0.97) | * |
| Risk profile | |||
| Risk perception scale | 1.07 | (1.05, 1.09) | *** |
| There are risks where I live: agree | 1.21 | (1.02, 1.43) | * |
| A risk-free country is a possible goal: agree | 1.45 | (1.21, 1.73) | ** |
| Worldview: fatalist | 1.27 | (1.05, 1.55) | * |
| Worldview: egalitarian | 1.44 | (1.21, 1.72) | *** |
| Knowledge/experience with food allergy | |||
| Education completed: high school (ref.) | 1.00 | — | — |
| Education completed: college/univ. | N/S | — | — |
| Education completed: Masters/PhD/Prof. | 0.62 | (0.49, 0.79) | ** |
| Allergies in household: none (ref.) | 1.00 | — | — |
| Allergies in household: one | N/S | — | — |
| Allergies in household: multiple | 2.77 | (1.56, 5.27) | *** |
| Recalled reading/hearing information about food allergies in the past 6 months | 1.69 | (1.37, 2.09) | *** |
| Compared to other people, more concerned about food allergies | 2.42 | (2.02, 2.92) | *** |
| Food allergies are easily treatable: disagree Region | 1.44 | (1.21, 1.72) | *** |
| Ontario (ref.) | 1.00 | — | — |
| Prairies | N/S | — | — |
| British Colombia | N/S | — | — |
| Atlantic | 1.54 | (1.06, 2.28) | * |
| QuebecInteraction terms | 2.07 | (1.63, 2.63) | *** |
| Quebec*Food allergy information | 0.63 | (0.45, 0.89) | ** |
| Model fit Rho-square: 0.15 67.9% correctly classified (cutoff = 0.72) | |||
Significance: ***p < .001 = ‘; **p < .01; *p < .05.
Sociodemographics
Males were about half as likely to rate the risks of food allergy (OR: 0.59, 95%CI: [0.50–0.69]) as high. Older adults consistently rated the risks as higher than respondents aged 18–29 (reference category), though those aged 30–39 and 40–49 were not significantly different. Immigration status of the respondents displayed an interesting relationship with risk perception. In particular, immigrants who had lived in Canada for less than 10 years were more likely than non-immigrants to rate the risks of food allergy as high (OR: 2.51, 95% CI: [1.48, 4.47]). This relationship was then inverted for immigrants whom had lived in Canada for at least 10 years (OR: 0.80, 95% CI: [0.62, 1.04]). Indicators of household composition suggested that respondents from homes with more residents rated the risks of food allergy higher, with a particularly strong effect for households with children less than 18 years of age (minors). This relationship was stronger still for single-adult homes with at least one minor (OR: 1.99, 95% CI: [1.17, 3.51]). Total household income from the previous tax year (2008) was also significant. Compared to respondents with household incomes of less than $20,000, those from households with higher incomes were consistently less likely to rate food allergies as high risks to the Canadian public.
Risk profile
A number of variables related to health risk perception emerged as important in the model. The health risk perception scale was highly significant, and odds ratios indicate that for each increase by one in the scale, the likelihood that a respondent would rate the risks of food allergy as high increased by 7.1%. Respondents who agreed that there were health risks where they lived were more likely to rate the risks of food allergy as high (OR: 1.21, 95% CI: [1.02, 1.43]), as were respondents who believed that a risk-free country was a possible goal (OR: 1.45, 95% CI: [1.21, 1.73]). Respondents who agreed with statements measuring fatalism were more likely to rate the risks as high (OR: 1.27, 95% CI: [1.05, 1.55]). This effect was similar for those who agreed with statements measuring egalitarian worldviews (OR: 1.44, 95% CI: [1.21, 1.72]).
Knowledge/experience with food allergy
In terms of the variables measuring experience with, and knowledge about food allergies and the related risks, respondents with the highest levels of education (Master's degree, Ph.D., professional degree) were significantly less likely to rate the risks of food allergy (OR: 0.62, 95% CI: [0.49, 0.79]) as high. Direct experience with food allergy (respondents from allergic households) was a significant predictor, but only for respondents who reported multiple allergies in the home (OR: 2.77, 95% CI: [1.56, 5.27]). Respondents who reported receiving some information about food allergies in the past six months were more likely than those who did not to rate the risks as high (OR: 1.69, 95% CI: [1.37, 2.09]); as were those who reported being more concerned about the risks associated with food allergies (OR: 2.42, 95% CI: [2.02, 2.92]).
Finally, those who disagreed that food allergies were easily treatable perceived the risks of food allergy (OR: 1.44, 95% CI: [1.21, 1.72]) as high risks to the Canadian public.
Regional political environment
Reported province of residence was used to situate each respondent in a particular region of Canada. Living in Atlantic Canada (Nova Scotia, New Brunswick, Newfoundland, or Prince Edward Island) was associated with a higher propensity to rate the risks as high (OR: 1.58, 95% CI: [1.05, 2.28]), as was living in the province of Quebec (OR: 2.07, 95% CI: [1.63, 2.63]). An interaction term between residents from the province of Quebec, and receiving food allergy information in the past 6 months also emerged as important. The relationship suggests that, though not receiving food allergy information had an attenuating effect on perceived risks for respondents living elsewhere, this relationship was not apparent in Quebec, where perception of risk was high regardless of level of access to information.
DISCUSSION
To inform policy around emerging health risks, it is essential to understand how the general population perceives these risks, and to identify the associated determinants of perceptions. The results of this study demonstrate the extent to which the general population views the risks of food allergy as risks to the Canadian population. Extended by simple extrapolation, more than 15 million Canadians (50.6%) would report being either directly or indirectly affected by food allergies, and more than 6 million (18.7%) would report having a food allergic person in the household. Further, the average respondent estimated the prevalence of food allergy in Canada to be 30%. These estimates greatly overestimate the confirmed prevalence estimates determined by alternative methods from the SCAAALAR data, published elsewhere (Ben-Shoshan et al. 2010). This reinforces the fact that there are different understandings of the prevalence, and associated risks, of food allergy between the general public and scientists (Altman and Chiaramonte 1996; Shepherd 2006), a phenomenon that consistently arises in investigations of risk perception (e.g., persistent organic pollutants, heavy metals (Scholz and Siegrist 2010)).
Multivariate analysis revealed that older respondents, women, those with lower levels of education and income, and new immigrants perceived the risks of food allergy higher than younger respondents, men, those with relatively higher levels of education and income, and Canadian-born respondents. The relationship between gender and perceived risk is highly consistent with results reported elsewhere (Flynn et al. 1994; Finucane et al. 2000; Dosman et al. 2001; Krewski et al. 2006a,b). Although the reasons for the gender difference are still unclear, they are thought to result from a combination of biological and social differences (Finucane et al. 2000). In the case of food allergies, for example, increased perceived risk may be partially determined by the socialization of women as primary family nurturers and caregivers (Flynn et al. 1994), thus being more sensitive to an issue that disproportionately affects children.
The influence of age has been hypothesized to reflect familiarity with risk, differential levels of exposure to risk, or sociopolitical opinions related to time period or birth cohort effects (Krewski et al. 2006a,b; Dosman et al. 2001). However, the relationship with risk perception is equivocal, and appears to depend on the risk in question (Riechard and Peterson 1998). Results of this study indicate that respondents in their parental and grand-parental years were more likely to rate the risks of food allergy as high compared to younger respondents. There are two related explanations for this finding. Firstly, heightened perception of risk may be related to a relative lack of familiarity with food allergies in comparison with younger respondents. In the span of only two to three decades, food allergies have gone from rare conditions to significant public health issues. The risks of food allergy, then, are particularly new and unfamiliar risks for many older individuals, and the recency of their emergence may be provoking the higher risk perceptions reported here. Secondly, older adults have consistently been shown in the literature to feel a responsibility to protect children from health risks (Slovic 2000; Sjöberg 1998). Higher perceived risks by older respondents may be reflecting this assumed responsibility, as children are currently experiencing a disproportionate burden of food allergy, and peanut allergy in particular (Ben-Shoshan et al. 2010; Rona et al. 2007).
Income is a well-recognized determinant of mental and physical health; however, the relationship with risk perception has been less thoroughly explored. In this study, respondents from households reporting the lowest levels of household income also reported the highest perceived risks of food allergy. This relationship may be explained by feelings of inequality specific to control over and personal choices about risks and their risk management (Lemyre et al. 2006). However, as alluded to previously in this article, the practice of banning particular allergens (e.g., peanut butter) in public spaces also raises important issues of equity for lower income populations. Higher perceived risks within this population may reflect the difficulties associated with finding affordable substitutes to these proteins that comply with regulations. This issue is one that must be considered as policies are developed to address the emergence and potential increases in food allergy.
Income is also highly positively related to level of educational attainment, and the relationships presented here with respect to education echo those found for income. That is, those with the highest levels of education were least likely to perceive the risks of food allergy as high. This relationship has primarily been theorized as being related to understanding risks, and how they may be controlled (Dosman et al. 2001). This understanding may be especially important in the context of emerging health risks that are often characterized by uncertainty and contention. This is certainly the case for food allergies, around which debates about etiology, diagnosis, and management are ongoing (Schnieder Chafen et al. 2010).
Results revealed a strong relationship between perceived risk and time since immigration. Respondents who had lived in Canada for less than 10 years rated the risks of food allergy much higher than Canadian-born respondents, while those who had been in Canada for more than 10 years rated the risks similarly to Canadian-born respondents. We recognize that this could be explained by a cohort effect related to time since immigration; however, it is interesting to note the parallel with the healthy immigrant effect (Asanin Dean and Wilson 2010; Newbold 2005). That is, when immigrants arrive to a developed host country, they typically exhibit better health than the native born population with respect to self-rated health, and chronic disease. However, over time, and particularly at the ten-year mark, immigrant health tends to decline to levels equal to or even worse than that of the host country (Newbold 2005). Theories argue that this relationship may be a reflection of the acculturation process, which would include increased exposure to issues around food allergies—predominantly conditions of the Western world (Rona et al. 2007; Madsen 2005). Food allergies may represent an especially new risk for the population of recent immigrants; however, given the speculative nature of the parallel with the healthy immigrant effect, further investigation is warranted.
Differences in perceived risks between respondents from different household compositions were observed in this analysis. Respondents from households with minors reported higher perceived risks of food allergies, an effect that was amplified if there was only one adult living in the household. As discussed previously, most policies and regulations around food allergies have been implemented at the school-level in Canada, and thus, households with minors are more frequently exposed to issues around allergy-related policy. Frequent exposure may subsequently influence risk perceptions in this population (Slovic 2000). It is also possible that higher perceived risks stem from the lack of certainty about the etiology of food allergies in the scientific community. Parents, and mothers in particular, cope with competing information about what to eat and avoid during pregnancy, and how and when to introduce certain foods into their child's diet in order to avoid the development of potentially life-threatening food allergies. The popular perception that food allergies are increasing, coupled with the stress of making these presumably important decisions in an atmosphere of uncertainty, may be provoking higher risk perceptions in households with minors.
The health risk perception scale indicating general attitudes toward individual, familial, and societal risk tolerance was strongly related to food allergy risk perception. Previous studies of risk perception have evaluated the influence of belief statements reflecting environmental and social concern (Krewski et al. 2008; Lee et al. 2005). Although the statements used to construct the scale evaluated here differ from those previously used, the results certainly resonate with previous findings. That is, perception of new risks (e.g., food allergy), are positively correlated with indicators of broader concerns about environmental and social risks. Individuals rely on previous knowledge of health risks and experiences with risk in general, to form opinions about isolated emerging risks, with which they may be unfamiliar (Lee et al. 2005).
Worldviews have likewise been found to be correlated significantly with risk perceptions previously (Dake 1991; Wildavsky and Dake 1993). Those who agreed with fatalist and egalitarian worldview statements had higher perceived risks of food allergy. These relationships follow those found by others who have reported, for example, that egalitarians are likely to be adverse to societal or population-level risks (Wildavsky and Dake 1993). Similarly, fatalism has been reported in a previous Canadian study to be positively associated with risk perceptions of food- or bacteria-related hazards (Health Canada 1993). These findings reinforce the notion that perceptions of risk are partially based on threats to individual and societal ways of life (Douglas and Wildavsky 1982). This is indeed the case with respect to this newly emerging health risk that is affecting the lives of those directly affected (e.g., with respect to food choices as well as social and recreational venues considered safe) as well as those indirectly affected (e.g., restrictive policies in schools, air planes and other “public” places).
In terms of direct experience, having multiple food allergies in the household was the only significant predictor of high risk perception. This result was unexpected, due to the lack of effect for those reporting a single allergy in the home. This may be explained by increased familiarity with the risk (Dosman et al. 2001), and/or knowledge about the level of control possible, and may also be dependent on who is allergic (adult versus child). Alternatively, respondents from households with one allergic resident may view the risks of food allergy as an individual problem, rather than a threat to society. It is clear, however, that there is a threshold to the relationship with experience, as respondents from households with multiple allergic individuals were much more likely to rate the risks as high.
Having received or read some information about food allergies in the past six months was an important predictor of perceived risk. We know that in order to inform risk perceptions, the general population relies on the media and informal social relationships, particularly when the hazard is new and unfamiliar (Kasperson et al. 1988; Slovic 2000). Although this study was limited to only one question about food allergy risk information, we know from previous studies of risk that Canadians rely on the mass media for the majority of their risk information (Krewski et al. 1995, 2006a,b). Findings here indicate that the perceived risks of food allergy are being amplified through these outlets in some way. Harrington and colleagues (2011), for example, found that the discussions around food allergies in the media are being increasingly dominated by affected individuals, and advocates, with potential consequences for public understanding of food allergy risk.
Finally, in addressing the third research question posed by this article, regional differences in risk perception were observed in this survey, particularly marked differences were found between the province of Quebec and the rest of Canada. Quebec has a unique political environment, in that there is currently no provincial policy related to food allergies. The efficacy of risk management policies around food allergies is beyond the scope of this article; however, a key indication from these findings is that differential risk perceptions are provoked in differing political environments. The sociopolitical climate has previously been hypothesized as an influence on differences between perceived risks of other environmental health hazards between Quebec and the rest of Canada (Krewski et al. 2006a,b). Further, recent work conducted through the AllerGen NCE network has found different patterns of coping between allergic children and their parents dependent on perceptions of management procedures in school environments (Fenton et al. 2010). These findings point directly to the role of the policy environment as a determinant of perceptions for affected individuals. However, results of this study suggest that the sociopolitical climate may be a modifying factor for the perception of emerging risks in the general population. Further exploration of the nature of this relationship will help to tease out these relationships.
FUTURE RESEARCH AND LIMITATIONS
There are some limitations to this analysis. Firstly, the sampling strategy excluded households having cellular telephone service only (8% of households), and those without telephones (2%) (Statistics Canada 2008), further approximately 7% of all numbers are unpublished, and unavailable to Info-Direct (Chang 2011). This is a potential source for bias, and should be considered when interpreting results reported here. Secondly, approximately 33% of household incomes were not reported in the survey. In order to include these cases in final analyses, these data (n = 1210) were imputed using an approximate Bayesian bootstrap hot-decking approach. This approach has been used extensively by the United States Census Bureau (Allison 2002), and sample characteristics with respect to the distribution of household income were maintained; however, risk of misclassification is possible. Thirdly, while respondents from across Canada were represented by a wide variety of demographic backgrounds in the survey, it is evident that certain populations were underrepresented (e.g., low socioeconomic status). Potential bias was addressed by weighting the sample by age and sex to the 2006 Canadian population. In order to provide a more comprehensive picture of prevalence and risk, an extension of the survey will attempt to reach these populations using different methodologies. Finally, there was a relatively low strength of association for the regression model (rho-squared value = 0.15). However, the goal of this research was to explore the correlates of risk perception associated with this newly emerging health risk (as opposed to predict) and we were successful in uncovering numerous statistically significant effects.
These results also provide guidance for future research. Given that SCAAALAR was a large-scale telephone survey, the resulting sample underrepresented some key sectors of the Canadian population. Although households were selected randomly, particular demographic groups were more likely to respond. As such, the resulting sample was not proportionally representative of households of low socioeconomic status, new Canadians living in the country for less than ten years, or those living in the territories. This highlights a significant gap in knowledge, and an extension of the SCAAALAR survey is currently ongoing to reach population groups underrepresented here. Secondly, this research indicated that food allergy information plays a significant role in the perception of food allergies. While there is much research regarding the communication of food hazard risks through the media in general, to our knowledge, there is only one study regarding the communication of food allergy risks (Harrington et al. 2011). Further investigations are needed to fully understand the role of risk communication as a determinant of food allergy risk perceptions. Finally, further study into the nuances of the relationships identified through this research, including those using qualitative inquiry, will be vital for achieving a comprehensive understanding of the perception of food allergies as emerging health risks.
CONCLUSIONS
The risks of food allergies differ from those of other food-borne hazards such as chemical or biological contamination that can affect whole populations (Madsen et al. 2010). They affect a small proportion of the population (particularly children), and even within that group, may affect individuals with differing severity (Schnieder Chafen et al. 2010). Despite the fundamental differences, food allergies are increasingly permeating our everyday discourses (Nettleton et al. 2009; Shepherd 2006), and our everyday lives through policy change (i.e., food labeling, school policy). Debates over best management practices can be found in the scientific literature (Christakis 2008; Munoz-Furlong 2004) as well as the mass media (Harrington et al. 2011; Pearson 2009). In order to respond appropriately to the (potentially) growing prevalence of food allergies, decision-makers must protect the affected population, while accommodating the general public. Understanding the general population's perception of food allergies takes a step in this direction.
This article has provided support for the apparent high level of public perception of the risks associated with food allergies, providing some validation for their prominence on the public agenda. Using multivariate analyses, this research has also contributed by extending the methodology originated by Krewski and colleagues (1995, 2006a,b), for rating hazards, and has identified key role played by demographic, attitudinal, experiential, and contextual factors. As such, the research has established a strong evidence base for risk management policy around food allergies. For example, food allergy risk communications can be informed by these perceptions. An effective approach would necessarily tailor toward particular segments of the population and people living in particular areas. Secondly, results indicated that policy decisions made in a particular environment may act as a modifying determinant of risk perceptions, particularly if no policy exists. As future regulatory decisions are made to address this important health risk, it will be important for those responsible to be informed by the public's risk perceptions to limit backlash to emerging decisions, and facilitate their integration.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the efforts of two anonymous reviewers for their helpful and constructive comments. This work was funded by AllerGen NCE, Health Canada, and a Social Sciences and Humanities Research Council doctoral fellowship (held by the first author [Daniel W. Harrington], award No. 752-2008-1068).
REFERENCES
- AllerGen. Allergen NCE Inc. 2011. Available from http://www.allergen-nce.ca (accessed May 10, 2011)
- Allison PD. Missing Data. Thousand Oaks, CA, USA: Sage Publications Inc; 2002. [Google Scholar]
- Al-Muhsen S. Clarke AE, Kagan RS. Peanut allergy: An overview. Canadian Med Assoc J. 2003;168(10):1279–85. [PMC free article] [PubMed] [Google Scholar]
- Altman DR, Chiaramonte LT. Public perception of food allergy. J Allergy Clinical Immunol. 1996;97:1247–51. doi: 10.1016/s0091-6749(96)70192-6. [DOI] [PubMed] [Google Scholar]
- Asanin Dean J, Wilson K. My health has improved because I always have everything I need here?: A qualitative exploration of health improvement and decline among immigrants. Social Sci Med. 2010;70(8):1219–28. doi: 10.1016/j.socscimed.2010.01.009. [DOI] [PubMed] [Google Scholar]
- Beck U. Risk Society: Towards a New Modernity. New Delhi, India: Sage; 1992. [Google Scholar]
- Ben-Shoshan M. Kagan RS. Alizadehfar R, et al. Is the prevalence of peanut allergy increasing? A 5-year follow-up study of children in Montreal. J Allergy Clin Immunol. 2009;123(4):783–88. doi: 10.1016/j.jaci.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Ben-Shoshan M. Harrington DW. Sicherer SH, et al. A population-based study on the prevalence of peanut, tree nut, fish, shellfish and sesame allergies in Canada. J Allergy Clin Immunol. 2010;125(6):1327–35. doi: 10.1016/j.jaci.2010.03.015. [DOI] [PubMed] [Google Scholar]
- Bloomfield SF. Stanwell-Smith R. Crevel RWR, et al. Too clean, or not too clean: The Hygiene Hypothesis and home hygiene. Clin Exp Allergy. 2006;36(4):402–25. doi: 10.1111/j.1365-2222.2006.02463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branum AM, Lukacs SL. NCHS Data Brief, No. 10, October 2008. Hyattsville, MD, USA: National Center for Health Statistics; 2008. Food Allergy among U.S. Children: Trends in Prevalence and Hospitalizations. [PubMed] [Google Scholar]
- Chang V. Account supervisor. Toronto: List Brokerage Services, Cornerstone Group of Companies; 2011. May 16, 2011 (Personal Communication) [Google Scholar]
- Christakis NA. This allergies hysteria is just nuts. BMJ. 2008;337:1384. doi: 10.1136/bmj.a2880. [DOI] [PubMed] [Google Scholar]
- Dake K. Orienting dispositions in the perception of risk: An analysis of contemporary worldviews and cultural biases. J Cross-Cultural Psychol. 1991;22:61–82. [Google Scholar]
- Dosman DM. Adamowicz WL, Hrudey SE. Socioeconomic determinants of health-and food safety-related risk perceptions. Risk Anal. 2001;21(2):307–18. doi: 10.1111/0272-4332.212113. [DOI] [PubMed] [Google Scholar]
- Douglas M, Wildavsky A. Risk and Culture: An Essay on the Selection of Technological and Environmental Dangers. Berkeley, CA, USA: University of California Press; 1982. [Google Scholar]
- Fenton N. Elliott SJ. Cicutto L, et al. Illustrating risk: Anaphylaxis through the eyes of the food-allergic child. Risk Anal. 2010;31(1):171–83. doi: 10.1111/j.1539-6924.2010.01488.x. [DOI] [PubMed] [Google Scholar]
- Finucane ML. Slovic P. Mertz CK, et al. Gender, race, and perceived risk: The “white male” effect. Health, Risk & Society. 2000;2(2):159–72. [Google Scholar]
- Flynn J. Slovic P, Mertz CK. Gender, race, and perception of environmental health risks. Risk Anal. 1994;14:1101–8. doi: 10.1111/j.1539-6924.1994.tb00082.x. [DOI] [PubMed] [Google Scholar]
- Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opinion Quart. 2006;70(5):646–75. [Google Scholar]
- Grundy J. Matthews S. Bateman B, et al. Rising prevalence of allergy to peanut in children: Data from 2 sequential cohorts. J Allergy Clin Immunol. 2002;110(5):784–9. doi: 10.1067/mai.2002.128802. [DOI] [PubMed] [Google Scholar]
- Harrington DW. Elliott SJ, Clarke AE. Frames, Claims and Audiences: Construction of Food Allergies in the Canadian Media. Public Understanding of Science; 2011. Published online before print March 1, 2011, doi: 10.1177/0963662510393083. [DOI] [PubMed] [Google Scholar]
- Health Canada. Health-risk Perception in Canada. Ottawa: Ministry of Supply and Services; 1993. Ottawa, ON, Canada. [Google Scholar]
- Health Canada. Food Allergies and Intolerances, 2009. 2009. Available at http://www.hc-sc.gc.ca/fn-an/securit/allerg/index-eng.php (accessed on February 10, 2010)
- Kagan RS. Food allergy: An overview. Environ Health Perspect. 2003;111(2):223–5. doi: 10.1289/ehp.5702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasperson RE. Renn O. Slovic P, et al. The social amplification of risk: A conceptual framework. Risk Anal. 1988;8(2):177–87. [Google Scholar]
- Krewski D. Slovic P. Bartlett S, et al. Health risk perception in Canada I: Rating hazards, sources of information and responsibility for health protection. Hum Ecol Risk Assess. 1995;1(2):117–32. [Google Scholar]
- Krewski D. Lemyre L. Turner MC, et al. Public perception of population health risks in Canada: Health hazards and sources of information. Hum Ecol Risk Assess. 2006a;12:626–44. [Google Scholar]
- Krewski D. Lemyre L. Turner MC, et al. 2008. Public perception of population health risks in Canada: Risk perception beliefs. Health, Risk & Soc. 2006b;10(2):167–79. [Google Scholar]
- Krom MPMM and Mol APJ. Food risks and consumer trust. Avian influenza and the knowing and non-knowing on UK shopping floors. Appetite. 2010;55(3):671–8. doi: 10.1016/j.appet.2010.09.022. [DOI] [PubMed] [Google Scholar]
- Law M. Wilson K. Eyles J, et al. Meeting health need, accessing health care: The role of neighborhood. Health & Place. 2005;11:367–77. doi: 10.1016/j.healthplace.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Lee JEC. Lemyre L. Mercier P, et al. Beyond the hazard: The role of beliefs in health risk perception. Hum Ecol Risk Assess. 2005;11:1111–26. [Google Scholar]
- Lee S. Brown RE. Grant D, et al. Exploring nonresponse bias in a health survey using neighborhood characteristics. Am J Public Health. 2009;99(10):1811–7. doi: 10.2105/AJPH.2008.154161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemyre L. Lee J. Mercier P, et al. The structure of Canadians’ health risk perceptions: Environmental, therapeutic and social health risks. Health, Risk & Society. 2006;8(2):185–95. [Google Scholar]
- Liew WK. Williamson E, Tang ML. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol. 2009;123:434–42. doi: 10.1016/j.jaci.2008.10.049. [DOI] [PubMed] [Google Scholar]
- Madsen C. Prevalence of food allergy: An overview. Proceed Nutrition Soc. 2005;64(4):413–7. doi: 10.1079/pns2005458. [DOI] [PubMed] [Google Scholar]
- Madsen C. Crevel R. Chan C, et al. Food allergy: Stakeholder perspectives on acceptable risk. Regul Toxicol Pharmacol. 2010;57:256–65. doi: 10.1016/j.yrtph.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Mills ENC. Mackie AR. Burney P, et al. The prevalence, cost and basis of food allergy across Europe. Allergy. 2007;62(7):717–22. doi: 10.1111/j.1398-9995.2007.01425.x. [DOI] [PubMed] [Google Scholar]
- Munoz-Furlong A. Food allergy in schools: Concerns for allergists, pediatricians, parents and school staff. Ann Allergy Asthma Immunol. 2004;93(5 Suppl 3):S47–50. doi: 10.1016/s1081-1206(10)61732-2. [DOI] [PubMed] [Google Scholar]
- Nettleton S. Woods B. Burrows R, et al. Food allergy and food intolerance: Towards a sociological agenda. Health. 2009;13(6):647–64. doi: 10.1177/1363459308341433. [DOI] [PubMed] [Google Scholar]
- Newbold KB. Self-rated health within the Canadian immigrant population: Risk and the healthy immigrant effect. Social Sci Med. 2005;60:1359–70. doi: 10.1016/j.socscimed.2004.06.048. [DOI] [PubMed] [Google Scholar]
- Pearson P. It's just nuts! Chatelaine Magazine. 2009. December 2009 Issue.
- Primeau MN. Kagan RS. Joseph L, et al. The psychological burden of peanut allergy as perceived by adults with peanut allergy and the parents of peanut-allergic children. Clin Exp Allergy. 2000;30:1135–43. doi: 10.1046/j.1365-2222.2000.00889.x. [DOI] [PubMed] [Google Scholar]
- Radandt S, Renn O. New emerging risks. In: HJ Bischoff., editor. Risks in Modern Society: Topics in Safety, Risk, Reliability and Quality. Brussels, Belgium: Springer; 2008. pp. 259–283. [Google Scholar]
- Riechard DE, Peterson SJ. Perception of environmental risk related to gender, community socioeconomic setting, age, and locus of control. J Environ Educ. 1998;30(1):11–9. [Google Scholar]
- Rona RJ. Keil T. Summers C, et al. The prevalence of food allergy: A meta-analysis. J Allergy Clin Immunology. 2007;120(3):638–46. doi: 10.1016/j.jaci.2007.05.026. [DOI] [PubMed] [Google Scholar]
- Schnieder Chafen JJ. Newberry SJ. Riedl MA, et al. Diagnosing and managing common food allergies. JAMA. 2010;303(18):1848–56. doi: 10.1001/jama.2010.582. [DOI] [PubMed] [Google Scholar]
- Scholz RW, Siegrist M. Low risks, high public concern? The cases of persistent organic pollutants (POPs), heavy metals and nanotech particles. Hum Ecol Risk Assess. 2010;16:185–98. [Google Scholar]
- Shepherd R. Allergy between the ears? In: LJWJ Gilissen., editor; Wichers HJ, editor; Savelkoul HFJ, et al., editors. Allergy Matters: New approaches to Allergy Prevention and Management, 153–161. Dordrecht, The Netherlands: Springer; 2006. [Google Scholar]
- Sicherer SH. Munoz-Furlong A, Sampson HA. Prevalence of peanut and tree nut allergy in the United States determined by means of a random digit dial telephone survey: A 5-year follow-up study. J Allergy Clin Immunol. 2003;112(6):1203–7. doi: 10.1016/s0091-6749(03)02026-8. [DOI] [PubMed] [Google Scholar]
- Sjöberg L. Worry and risk perception. Risk Anal. 1998;18(1):85–93. doi: 10.1111/j.1539-6924.1998.tb00918.x. [DOI] [PubMed] [Google Scholar]
- Sjöberg L. Factors in risk perception. Risk Anal. 2000;20(1):1–11. [PubMed] [Google Scholar]
- Slovic P. The Perception of Risk. London, UK: Earthscan Publications; 2000. [Google Scholar]
- Statistics Canada. Age and Sex Highlight Tables, 2006 Census. 2009. Available from http://www12.statcan.ca/census-recensement/2006/dp-pd/hlt/97-551/index.cfm?Lang=E (accessed February 10, 2010)
- Statistics Canada. Residential Telephone Service Survey, 2008. 2008. Available from http://www.statcan.gc.ca/daily-quotidien/090615/dq090615c-eng.htm (accessed May 17, 2011)
- Subbaro P. Piush JM, Sears MR. Asthma: epidemiology, etiology and risk factors. Canadian Med Assoc J. 2009;181(9):E181–E190. doi: 10.1503/cmaj.080612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uguz A. Lack G. Pumphrey R, et al. Allergic reactions in the community: A questionnaire survey of members of the anaphylaxis campaign. Clinical and Experimental Allergy: J Brit Soc Allergy Clinical Immunol. 2005;35(6):746–50. doi: 10.1111/j.1365-2222.2005.02257.x. [DOI] [PubMed] [Google Scholar]
- Venter C. Hasan Arshad S. Grundy J, et al. Time trends in the prevalence of peanut allergy: Three cohorts of children from the same geographical location in the UK. Allergy. 2010;65(1):103–8. doi: 10.1111/j.1398-9995.2009.02176.x. [DOI] [PubMed] [Google Scholar]
- Wildavsky A, Dake K. In: Theories of Risk Perception: Who Fears What and Why? EJ Burger., editor. Ann Arbor, MI, USA: University of Michigan Press; 1993. pp. 41–60. Risk. [Google Scholar]


