Abstract
Despite the known benefits of a healthy lifestyle, many individuals find it hard to maintain such a lifestyle in our modern world, which facilitates sedentary behavior and overeating. As a consequence, the prevalence of type 2 diabetes mellitus is predicted to increase dramatically over the coming years. Will developments in treatments be able to counteract the resulting impact on morbidity and mortality? The various lines of research can be grouped into three main categories: technological, biological, and pharmacological. Technological solutions are focused on the delivery of insulin and glucagon via an artificial pancreas, and components of the system are already in use, suggesting this option may well be available within the next 10 years. Of the biological solutions, pancreas transplants seem unlikely to be used widely, and islet cell transplants have also been hampered by a lack of appropriate donor tissue and graft survival after transplant. However, significant progress has been made in these areas, and additional research suggests manipulating other cell types to replace beta cells may be a viable option in the longer term. The last category, pharmacological research, appears the most promising for significantly reducing the burden of type 2 diabetes mellitus. In recent years, research has concentrated on reducing blood glucose, and the increasing pace of research has been reflected in a growing number of antidiabetic agents. In the past few years, studies of the complementary approach of protecting cells from the damaging effects of high blood glucose have also been reported, as has research into the control of energy intake and energy expenditure. Evidence from studies of dietary restriction and bariatric surgery suggests it may be possible to reset metabolism to effectively cure diabetes, and research into pharmacological agents that could selectively restore energy balance is currently the most exciting prospect for future treatments for people with type 2 diabetes mellitus.
Keywords: hypoglycemic agents, obesity, prevalence, translational medical research, type 2 diabetes mellitus
Introduction
Before the availability of insulin in the 1920s, hailed not only as the cure for diabetes but also as one of the greatest advances in the treatment of any disease, a person diagnosed with diabetes would have faced death within a few years. Today, diabetes is not the devastating diagnosis it would have been 100 years ago; in fact, it is now a common misconception among the public that diabetes is not a serious disease. In reality, the impact of diabetes is so significant that it is affecting overall life expectancy: in the United States (US), life expectancy is falling for the first time since statistics were collected, due to obesity and diabetes [Olshansky et al. 2005], and estimates of diabetes prevalence over the coming years suggest many of us reading this article will develop diabetes during our lives [Whiting et al. 2011]. The predictions of the increased prevalence of diabetes are rarely accompanied by predictions of improvements in the treatment of diabetes; however, given the impact of diabetes, it has been the focus of intensive research, resulting in major advances in our understanding of diabetes as well as in treatment options. As the centenary of the discovery of insulin approaches, it seems timely to consider how treatment options may look in the 2020s, and the likelihood that the elusive cure for diabetes could be found by that time.
Technological solutions
The majority of cases of diabetes are type 2 diabetes mellitus (T2DM), and the predicted rise in diabetes prevalence is expected to be driven by increases in the number of T2DM cases. However, it is likely that significant advances in therapy for T2DM will result from the research in type 1 diabetes mellitus (T1DM), as they are both essentially disorders of glucose management (Box 1).
Box 1. Pathophysiology of type 1 and type 2 diabetes mellitus.
Type 1 (T1DM) and type 2 diabetes mellitus (T2DM) are both characterized by abnormally high levels of glucose in the bloodstream and until the 1930s, when ‘insulin-sensitive’ and ‘insulin-insensitive’ diabetes were differentiated, all patients with diabetes were thought to have a shortage of insulin production [Saltiel, 2000].
Since then the pathophysiology of the two diseases has been researched extensively, and T1DM is relatively well understood. In short, the patient’s immune system attacks and destroys beta cells in the islets of the pancreas, resulting in insulin deficiency. The factors behind the immune response are still uncertain, but are thought to be both genetic and environmental [van Belle et al. 2011].
Even today, the pathophysiology of T2DM is less well understood. At diagnosis, most patients have insulin resistance: the pancreas is producing insulin, but the body cannot use it effectively. Initially, the pancreas compensates by producing more insulin, and patients have larger beta-cell mass. At some point, typically several years after diagnosis, insulin production will decrease, with a corresponding drop in beta-cell mass, and many people with T2DM eventually need to take insulin. Although the underlying cause is unknown, it is thought that liver, fat, and muscle cells all play a role, in addition to the pancreatic beta cells [Saltiel, 2000].
In T1DM, the complete lack of endogenous insulin has focused research on ever-more sophisticated ways to deliver insulin, with the eventual goal of developing an ‘artificial pancreas’. The elements are already available: a sensor to detect blood glucose readings, a computer to calculate insulin requirements, and a pump to automatically deliver insulin. The feasibility of bringing these elements together has already been demonstrated in clinical trials, with sensor-augmented pump therapy, integrating a sensor and a pump, shown to improve glycemic control compared with a regimen of multiple insulin injections per day [Bergenstal et al. 2010; Hermanides et al. 2011]. A true artificial pancreas would also deliver glucagon to raise blood glucose and prevent severe hypoglycemia, a concept that has already been shown to be feasible [El-Khatib et al. 2010].
Several technological challenges need to be overcome to produce a clinically useful artificial pancreas. First, currently available continuous glucose monitors measure glucose levels in interstitial fluid rather than directly in the blood, resulting in a time lag before changes are measured. As a consequence, accuracy is not sufficiently reliable, with reported error rates of between 12% and 17%. Accuracy is likely to be lowest when blood glucose levels are low; hence, continuous glucose monitoring of interstitial fluid is currently recommended only as an adjunct to standard blood glucose monitoring [Weinzimer and Tamborlane, 2008]. Insulin pump technology is more advanced; nevertheless, today’s pumps deliver insulin subcutaneously, and the delay while insulin is absorbed into the bloodstream limits the ability of software to regulate blood glucose accurately [Renard, 2008]. Catheter complications have prevented intravenous delivery of insulin, and surgically implanted pumps are expensive. It is clear that none of these technological challenges are trivial, but given the pace of developments in technology, we can expect more practical options for patients within the next 10 years. For example, so-called ‘smart tattoo’ biosensors are capable of detecting glucose levels continuously using a simple infrared detector and providing results in real time. These biosensors, which are based on single-walled carbon nanotubes wrapped in glucose-sensitive polymers that fluoresce in the presence of glucose, are currently being researched in animal models [Barone and Strano, 2009].
Biological solutions
Even as technological solutions advance closer and closer to an artificial pancreas, it is unlikely that technology could ever regulate insulin as precisely as beta cells in a healthy pancreas. Research therefore continues into replacing damaged beta cells with functioning cells, or replacing the entire pancreas [Claiborn and Stoffers, 2008; Sachdeva and Stoffers, 2009]. As with the artificial pancreas, most research to date has been conducted in T1DM, but the results will ultimately translate into therapies for T2DM.
Pancreas transplants have been performed since the late 1980s, with more than 30,000 pancreas transplants recorded in the past 25 years [Gruessner, 2011]. In principle, pancreas transplants offer the promise of excellent outcomes for patients with diabetes. Indeed, stricter donor criteria, as well as improvements in surgical techniques and immunosuppression, have led to improved success rates, with the majority of patients no longer needing insulin therapy after the transplant [Gruessner, 2011]. In practice, the vast majority of pancreas transplants are done in patients who have end-stage renal disease and also need a kidney transplant; this is partly due to the shortage of donor organs, but also because the risks of the necessary post-transplant immunosuppressant therapy usually outweigh the health risks of diabetes itself.
A less invasive option that has already been shown to be viable, at least for some patients, is replacing pancreatic beta cells via islet cell transplants [Truong and Shapiro, 2006]. Isolating these cells from a donor pancreas and infusing them into the patient’s portal vein has been researched since the 1960s, and a successful protocol using islets from multiple donors, improved cell culture techniques, and reduced toxicity was optimized during the 1990s at the University of Alberta in Edmonton, Canada. Using the Edmonton protocol, initial studies reported success; however, over time transplanted islets lose function and patients still require immunosuppressive drugs, which are known to increase the risk of infections and the incidence of malignancy, as well as being toxic to the islet cells themselves [Alejandro et al. 2008; Shapiro et al. 2000].
The treatment is still considered experimental and is only available to patients with very poor glycemic control and severe hypoglycemic events but, given the benefits of a successful therapy, there is significant drive to overcome the challenges of limited availability of donor tissue and graft survival after transplant. As well as optimizing the yield of islets from donor pancreata, basic science research into cell differentiation has identified possible alternative sources of beta cells, including differentiating stem cells and reprogramming somatic cells [Baiu et al. 2011; Kelly et al. 2011]. Various strategies are also being researched to improve graft survival after transplantation, by developing immunosuppression regimens that are less toxic to islets and inducing revascularization/reinnervation of the islets [Plesner and Verchere, 2011].
In the longer term, other biological solutions using nonislet cells from the patient themselves are possible options, such as transdifferentiation (mediated by growth factor treatments or gene transfer) of nonislet pancreatic cells or liver cells [Claiborn and Stoffers, 2008; Kojima et al. 2003], and regenerating beta cells and/or expanding beta-cell mass using mediators of beta-cell differentiation and maintenance of adult beta cells [Sachdeva and Stoffers, 2009].
Pharmacological solutions
For patients with T1DM, who make no insulin, the only pharmacologic option is replacement insulin. Astonishing progress has been made since replacement insulin first became available, when insulin batches were of variable quality and large, twice-daily injections were needed. Today, it is hard to imagine how difficult it must have been to manage T1DM without disposable needles or patients self-testing glucose. The possibilities for improvement in pharmacological care for these patients should not be underestimated, although most likely they will be essentially improvements in the convenience of insulin delivery.
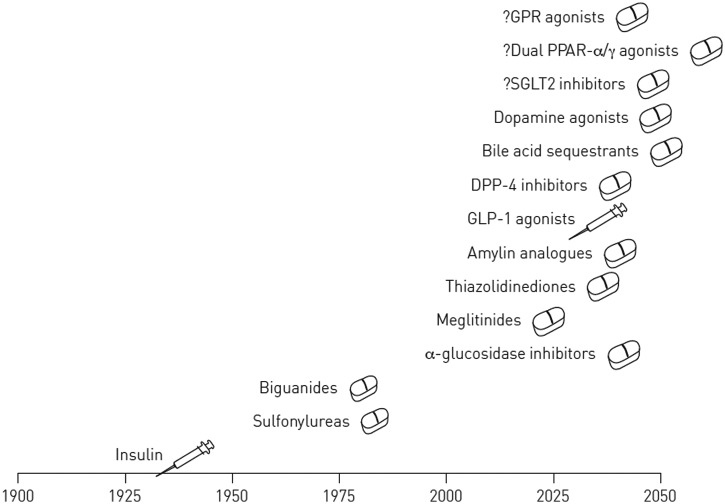
In patients with T2DM, a range of pharmacologic treatments have been developed, and continue to be developed (Figure 1). For many years, treatment was dominated by two drug classes, sulfonylureas and biguanides. These two drug classes demonstrate not only the advances in clinical research, but also the role that luck, both good and bad, plays in the progress of treatment. Sulfonylureas were discovered serendipitously in France during the Second World War after hypoglycemia was induced in soldiers in whom the drug was being tested as an antimicrobial agent for typhoid fever [Vaisrub, 1972]. In the US, sulfonylureas first became available in 1955 and for many years were the first-line option for treating T2DM. These drugs were no miracle cure: as is well known, the first-generation sulfonylureas were associated with a high risk of hypoglycemia; the second-generation sulfonylureas, which are still used today, were introduced in 1984.
Figure 1.
US Food and Drug Administration approval of pharmacological options for type 2 diabetes mellitus.
Like sulfonylureas, drugs of the biguanide class were observed to have antihyperglycemic properties before their mechanism of action was understood. In fact, the class had been studied in the 1920s but, perhaps because of the excitement over insulin, was largely ignored and it was not until the 1950s that phenformin, buformin, and metformin were researched in clinical trials. Unfortunately, the only biguanide marketed in the US, phenformin, was associated with lactic acidosis, leading not only to withdrawal of phenformin but, understandably, to mistrust of other medications in the same class [Witters, 2001]. It was not until the 1990s, when the large United Kingdom Prospective Diabetes Study (UKPDS) showed the benefits of metformin, especially in terms of weight-neutrality, that it became available and more widely used in the US [United Kingdom Prospective Diabetes Study Group, 1995]. More recently, metformin has been associated with reduced risk of cancer in observational studies, although this potential additional benefit needs to be confirmed in long-term randomized controlled trials [Noto et al. 2012].
The last 20 years have seen an astonishing pace in research into the molecular pathology of diabetes. Our improved understanding of diabetes has facilitated the development of drug classes that target specific metabolic pathways such as the thiazolidinediones, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, and sodium–glucose cotransporter type 2 (SGLT2) inhibitors (Figure 1) [Tahrani et al. 2011]. In the next 10 years, based on current research, we can expect more purposely targeted drugs for T2DM, and better combinations of drugs with simpler treatment regimens [Fakhrudin et al. 2010].
Beyond the drugs already in the pipeline, where might research take us? Can we begin to think about therapies that would cure or even prevent T2DM?
For some time, researchers have known that the brain plays an important role in eating behavior and satiety, and ‘gut–brain’ connections may be the next therapeutic targets, with newer drugs targeting the central nervous system [Pagotto, 2009]. With the currently available GLP-1 receptor agonists, for example, the brain is likely to mediate at least some of the important effects, such as improved satiety and weight loss, regulation of gastric emptying, and possibly suppression of glucose [De Silva et al. 2011; Knauf et al. 2008]. Indeed, the relatively new use of the centrally acting therapy, quick-release bromocriptine, illustrates the potential of the brain as a treatment target for T2DM. Bromocriptine, a D2 dopamine receptor agonist, has been available for many years as a treatment for acromegaly and hyperprolactinemia, and was approved by the US Food and Drug Administration in May 2009 as a treatment for T2DM [Gaziano et al. 2010]. Similar to when metformin was first used, the mechanism by which bromocriptine improves glycemic control is as-yet unknown, although it is clear that improvements in glycemic control are seen without increases in insulin concentration [Cincotta et al. 1999; Vero Science, 2010]. Investigators believe the drug acts at a central target in the hypothalamus and may affect circadian rhythms to favor improvements in metabolism. This concept was apparently suggested by the metabolism of migrating birds that develop seasonal insulin resistance before migrating, and then return to a lean state after migration [Scranton and Cincotta, 2010].
Bromocriptine is likely to be used in only a minority of patients due to its fairly modest glucose-lowering effects, although it could spark new avenues of research for diabetes treatments, as is always the case when new drug classes are identified. Intriguingly, the theory of seasonal insulin resistance in migrating birds is consistent with studies of insulin resistance in hibernating animals, suggesting the brain is involved via regulation of dopamine and prolactin, and plays a role in accumulation of fat and development of insulin resistance in winter [Martin, 2008]. Humans have no seasonal variations in dopamine, but this neurotransmitter may still play a role in insulin resistance, with people who develop diabetes essentially trapped in a constant state of ‘winter’, characterized by chronic insulin resistance and fat accumulation. Because there is no seasonal food shortage, there is no loss of adipocytes, and the body never returns to ‘summer’ [Martin, 2008]. This pathway, which bromocriptine appears to reset, could open up entirely new approaches to preventing or even curing T2DM.
Could an imposed food shortage help reset metabolism? Studies of bariatric surgery (gastric bypass, sleeve gastrectomy, biliopancreatic diversion or duodenal switch procedure) in obese patients with T2DM seem to suggest that it does, with patients receiving bariatric surgery significantly more likely to eliminate the need for antidiabetic therapies compared with patients receiving only medical therapy for T2DM [Mingrone et al. 2012; Schauer et al. 2012; Sovik et al. 2011]. These surgical procedures improve diabetes not only by causing weight loss, but also by affecting hormones such as GLP-1 and ghrelin, which help signal satiety and hunger, respectively, to the human brain [Peterli et al. 2012]. Increasing satiety signals and reducing hunger signals to the brain can help patients tolerate extreme caloric restrictions.
Dietary restriction is known to increase lifespan in rodents, and can delay or prevent diseases such as cancer, heart disease, and diabetes; however, studies in nonhuman primates have reported conflicting findings, indicating the effects of dietary restriction are likely to be complex [Mattison et al. 2012]. Such studies are hard to replicate in people, but trials showing a severely restricted diet can improve beta-cell function and insulin sensitivity in patients with a relatively short duration of T2DM suggest that humans, like hibernating mammals, have the capacity for recovering from insulin resistance [Lim et al. 2011]. The problem, the study investigators believe, is that few people could maintain such a limited calorie intake, and any successful nonsurgical solution may therefore rely on drugs mimicking the effects of dietary restriction. Given the current and predicted prevalence of obesity, there is already intensive research into agents that decrease appetite or increase satiety. The endocannabinoid system is known to have a role in the regulation of appetite, but cannabinoid receptor antagonists such as rimonabant have been associated with unacceptable side effects [Eckel et al. 2011], although more selective agonists may be an avenue targeted in the future. To date, other therapies developed for the treatment of obesity have also been plagued by safety issues, but there are now several promising molecules in the early stages of development [Eckel et al. 2011].
Among the currently available therapies for T2DM, various classes also promote weight loss. For example, the subcutaneous agent pramlintide is associated with reduced food intake and body weight in obese people with and without diabetes, although it is associated with only modest hemoglobin A1c (HbA1c) reductions and the amount of weight loss induced is also relatively small [Lee et al. 2012]. Pramlintide is a synthetic form of amylin, which is secreted after meals and signals short-term satiety, and may therefore be more useful in combination with other agents. Therapies combining pramlintide with long-term signaling molecules are in the early stages of development, along with other therapies targeting appetite [Powell et al. 2011].
Metformin is also associated with weight loss, although the amount of weight shed is insufficient to meet FDA criteria for a weight loss drug (at least 5% of body weight). Guidelines now recommend physicians consider metformin for preventing or delaying diabetes in individuals with elevated glucose measurements and a body mass index >35 kg/m2 [American Diabetes Association, 2012]. Intriguingly, research has shown that metformin-induced alterations mimic many of the same transcriptional changes in the liver that occur with dietary restriction [Dhahbi et al. 2005]. The effects of metformin are still incompletely understood, but activation of AMP-activated protein kinase (AMPK) appears to play a central role [Zhou et al. 2001]. AMPK is a sensor of energy shortage within cells, acting as a metabolic switch (Box 2). The role of AMPK, and possible activators, are being intensively investigated and, at present, this route appears the most exciting line of enquiry into a possible cure for T2DM.
Box 2. AMP-activated protein kinase: master switch in metabolism.
We often think of glucose as the fuel for cells, but glucose is just one of the fuels used to produce the actual energy source in every cell: adenosine triphosphate (ATP). The energy balance within individual cells is maintained by the enzyme AMP-activated protein kinase (AMPK), which is activated when the ratio of ATP to adenosine monophosphate (AMP) falls [Viollet et al. 2009]. Because AMPK is the ‘master switch’ of energy intake and energy expenditure, this enzyme is a theoretical key target for therapeutic intervention in patients with T2DM. If it is possible to activate AMPK, the resulting signaling pathways could be manipulated to restore energy balance, making people more fit and less likely to develop insulin resistance, without the need to decrease energy intake or lose weight [Gruzman et al. 2009].
Investigations of AMPK activators are already confirming some of these theoretical effects. For example, giving an oral AMPK agonist AICAR to sedentary mice was shown to improve treadmill performance [Narkar et al. 2008]. The polyphenol resveratrol, an AMPK modulator present in red wine, appears to protect mice against diet-induced obesity and insulin resistance [Lagouge et al. 2006], and has also been shown to mimic the effects of calorie restriction in people with obesity [Timmers et al. 2011]. These studies are at early stages, although a phase II/III trial of the effect of resveratrol on inflammatory mediators and insulin resistance in patients with T2DM or obesity is underway [ClinicalTrials.gov identifier: NCT01158417].
The current antidiabetes drug metformin reportedly increases AMPK activity; however, the mechanism of action is incompletely understood and metformin may also act via AMPK-independent pathways [Foretz et al. 2010; Fryer et al. 2002]. The antihyperglycemic effect of metformin was discovered by chance, but the subsequent discovery that this drug activates AMPK raises the intriguing possibility of developing drugs to extend the benefits of metformin with fewer side effects. This is certainly possible: although AMPK is found in all cells, different complexes localize to the liver, adipocytes, or skeletal muscles, and a drug targeting these complexes with high specificity could selectively restore energy balance without harming other tissues [Gruzman et al. 2009].
Prevention of diabetes-related complications
Using the World Health Organization cut-offs for diagnosing diabetes may seem rather arbitrary to patients and we often need to explain that an HbA1c level of 6.5% was chosen because people with blood glucose over this level are at much higher risk of diabetic retinopathy. In clinical practice today, patients rarely die from the immediate effects of high blood sugar; instead, we screen for and treat diabetes primarily to prevent complications. It is clear that good control of glucose levels is associated with reduced risk of complications [Diabetes Control and Complications Trial Research Group, 1993; United Kingdom Prospective Diabetes Study Group, 1998], but what exactly is it about high glucose that causes complications? Could identifying and targeting those pathways bring the residual rate of complications down to that seen in people without diabetes?
Microvascular complications such as neuropathy, retinopathy, and nephropathy are highly correlated with glucose levels. Various pathways leading to the damage that high glucose levels cause have been proposed, including osmotic stress from sorbitol accumulation [Lorenzi, 2007]; oxidative damage to cells, with free radical production and reactive oxygen species formation [Ceriello and Motz, 2004]; and toxicity from advanced glycation end-products (AGE). As proof of principle, animal studies have shown that inhibition of AGE accumulation might represent an effective strategy to reduce the rate of diabetes progression and/or prevent diabetes-related complications [Schmidt and Stern, 2000; Watson et al. 2011].
Macrovascular complications of T2DM, such as myocardial infarction and ischemic stroke, may not just be related to hyperglycemia; inflammation mediated by macrophages appears to contribute to, or even be responsible for, insulin resistance [Olefsky and Glass, 2010]. Atherosclerosis is also thought to result from chronic inflammation leading to injury to the arterial wall [Ross, 1999]. Anti-inflammatory drugs could therefore provide a direct method to reduce the risk of macrovascular complications. In fact, aspirin, one of the oldest anti-inflammatory medications, is recommended in certain groups of patients with diabetes, but use is limited by the high risk of bleeding [American Diabetes Association, 2012]. Development of compounds to inhibit mediators of inflammation, such as tumor necrosis factor (TNF)-α and interleukin (IL)-6, as well as other cytokines from fat and immune cells, could reduce inflammation-associated insulin resistance if the proteins could be selected to act in a highly tissue-specific manner without affecting other functions of the immune system [Olefsky and Glass, 2010]. Research in this field is still in the early stages. A trial of etanercept (a TNF-α blocker) failed to improve insulin sensitivity in patients with the metabolic syndrome [Bernstein et al. 2006]. However, the IL-1 receptor antagonist drug used to treat rheumatoid arthritis, anakinra, improved beta-cell function in patients with T2DM [Larsen et al. 2007, 2009], suggesting anti-inflammatory compounds may be part of the future treatment of diabetes.
How might treatment evolve?
The current standard of care for T2DM consists of screening for elevated HbA1c levels or, in some cases, fasting plasma glucose, with diagnosis followed by management with lifestyle modifications and metformin except where contraindicated [American Diabetes Association, 2012]. For patients who do not achieve HbA1c targets, antidiabetes medications are added to metformin; subsequently, patients are monitored and further oral antidiabetes drugs or insulin are added if needed.
Clearly, the care of patients with T2DM is currently suboptimal, largely because our healthcare system has traditionally been based on an acute-care model. In contrast, chronic disease management emphasizes a team approach, medication management and patient adherence, prevention of complications, lifestyle modifications as well as coordination of care among subspecialists. Guidelines for the prevention of T2DM emphasize moving beyond the healthcare system towards integration with other areas, such as government and the media [Lindstrom et al. 2010; Paulweber et al. 2010]. There is already evidence that intervention at the public health level could significantly impact rates of T2DM [Elbel et al. 2012; Schwartz et al. 2012]. In the future, coordination of care using case managers, technology that helps patients between medical visits, such as mobile health and telemedicine, and restructuring care using patient-centered medical homes and accountable care organizations may be better suited for T2DM management [Quinn et al. 2011].
How might treatment options look in the year 2025? We can certainly expect that genetic testing will be used to determine whether the patient will develop diabetes and, if so, which of the predisposing genes are involved. Genetic testing is already used to diagnose subtypes of maturity-onset diabetes of the young (MODY), for which six different subtypes resulting from mutations in different genes have been identified. Diagnosing the exact subtype can help the physician select the most appropriate treatment, as well as screening family members who may benefit from support with lifestyle changes [Gardner and Tai, 2012]. In the future, analogous genetic tests for T1DM and T2DM will enable us to offer the patient the appropriate solution, either genetic therapy to ‘repair’ the defective gene or pharmacotherapy to compensate for it. Because there will likely be 50 or more drugs to choose from, the choice of pharmacotherapy will be personalized based on the patient’s genetic profile, which will also indicate predisposition to complications such as kidney disease or retinopathy that can then be treated with a ‘complication-prevention’ drug. An artificial pancreas will be an option for severe cases, or in patients who cannot tolerate other options.
Conclusion
To allow us to cope with periods of famine and feast, humans are adapted to make the most of the energy available to them. What ensured our survival then has become our weakness now, and all predictions indicate the prevalence of T2DM will get worse before it improves. Modern lifestyles allow continual access to food and encourage sedentary behavior, leading to a progressive cycle of overeating and weight gain. Despite efforts at education, lifestyles will likely become yet more sedentary over the next 20 years, facilitated by advances in technology. For example, concepts for controlling the world around us with only our thoughts would have been science fiction 20 years ago, but are now actively researched [Hochberg et al. 2006]. There seems little doubt that, without interventions, the prevalence of T2DM will increase.
For those who prefer simplistic views, it is easy to blame individuals for having diabetes. Indeed, despite the clear benefits of a healthy lifestyle, changes in long-term behavior and lifestyle are rare. However, as we understand more about our biology, we can appreciate that our environment naturally puts us all at high risk of diabetes. Nowhere is this seen more clearly than in populations that have been exposed to sudden changes in lifestyles as a result of urbanization, such as the Pima Indians in the US, who have far higher rates of T2DM than Pima Indian populations in Mexico [Esparza-Romero et al. 2010].
Is it realistic to ask people to change their lifestyles? The advances in therapy over the past 50 years have provided a remarkable array of options so that treatment can be tailored for each patient, but, even with expert teams of dieticians and diabetes educators, most patients need drug therapy, probably multiple-drug therapy, to achieve recommended HbA1c targets. However, in spite of achieving HbA1c targets, they still retain a residual risk for complications compared with people without diabetes. In the future, we may accept that drugs are needed to allow us to lead modern lifestyles without increasing our risk of diabetes. The scientific community should be applauded for taking the pragmatic approach of searching for interventions that could help individuals, probably the majority, who are unable to maintain healthy lifestyles in the long term. Because our lifestyle means that diabetes will become a normal aspect of life, the research ongoing today is vital to provide tools to counteract the diabetes epidemic.
Acknowledgments
Medical writing assistance, supported financially by Boehringer Ingelheim, was provided by Geraldine Thompson of Envision Scientific Solutions during the preparation of this review. Boehringer Ingelheim was given the opportunity to check the data used in the manuscript for factual accuracy only. The author was fully responsible for all content and editorial decisions, was involved at all stages of manuscript development, and has approved the final version of the review that reflects the authors’ interpretation and conclusions.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare no conflicts of interest in preparing this article.
References
- Alejandro R., Barton F., Hering B., Wease S. (2008) 2008 update from the Collaborative Islet Transplant Registry. Transplantation 86: 1783–1788 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association (2012) Standards of medical care in diabetes–2012. Diabetes Care 35(Suppl. 1): S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baiu D., Merriam F., Odorico J. (2011) Potential pathways to restore beta-cell mass: pluripotent stem cells, reprogramming, and endogenous regeneration. Curr Diab Rep 11: 392–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barone P., Strano M. (2009) Single walled carbon nanotubes as reporters for the optical detection of glucose. J Diabetes Sci Technol 3: 242–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergenstal R., Tamborlane W., Ahmann A., Buse J., Dailey G., Davis S., et al. (2010) Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med 363: 311–320 [DOI] [PubMed] [Google Scholar]
- Bernstein L., Berry J., Kim S., Canavan B., Grinspoon S. (2006) Effects of etanercept in patients with the metabolic syndrome. Arch Intern Med 166: 902–908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceriello A., Motz E. (2004) Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol 24: 816–823 [DOI] [PubMed] [Google Scholar]
- Cincotta A., Meier A., Cincotta M., Jr. (1999) Bromocriptine improves glycaemic control and serum lipid profile in obese Type 2 diabetic subjects: a new approach in the treatment of diabetes. Expert Opin Investig Drugs 8: 1683–1707 [DOI] [PubMed] [Google Scholar]
- Claiborn K., Stoffers D. (2008) Toward a cell-based cure for diabetes: advances in production and transplant of beta cells. Mt Sinai J Med 75: 362–371 [DOI] [PubMed] [Google Scholar]
- De Silva A., Salem V., Long C., Makwana A., Newbould R., Rabiner E., et al. (2011) The gut hormones PYY3-36 and GLP-17-36 amide reduce food intake and modulate brain activity in appetite centers in humans. Cell Metab 14: 700–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhahbi J., Mote P., Fahy G., Spindler S. (2005) Identification of potential caloric restriction mimetics by microarray profiling. Physiol Genomics 23: 343–350 [DOI] [PubMed] [Google Scholar]
- Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329: 977–986 [DOI] [PubMed] [Google Scholar]
- Eckel R., Kahn S., Ferrannini E., Goldfine A., Nathan D., Schwartz M., et al. (2011) Obesity and type 2 diabetes: what can be unified and what needs to be individualized? Diabetes Care 34: 1424–1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Khatib F., Russell S., Nathan D., Sutherlin R., Damiano E. (2010) A bihormonal closed-loop artificial pancreas for type 1 diabetes. Sci Transl Med 2(27): 27ra27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbel B., Cantor J., Mijanovich T. (2012) Potential effect of the New York City policy regarding sugared beverages. N Engl J Med 367: 680–681 [DOI] [PubMed] [Google Scholar]
- Esparza-Romero J., Valencia M., Martinez M., Ravussin E., Schulz L., Bennett P. (2010) Differences in insulin resistance in Mexican and U.S. Pima Indians with normal glucose tolerance. J Clin Endocrinol Metab 95: E358–E362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakhrudin N., Ladurner A., Atanasov A., Heiss E., Baumgartner L., Markt P., et al. (2010) Computer-aided discovery, validation, and mechanistic characterization of novel neolignan activators of peroxisome proliferator-activated receptor gamma. Mol Pharmacol 77: 559–566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foretz M., Hebrard S., Leclerc J., Zarrinpashneh E., Soty M., Mithieux G., et al. (2010) Metformin inhibits hepatic gluconeogenesis in mice independently of the LKB1/AMPK pathway via a decrease in hepatic energy state. J Clin Invest 120: 2355–2369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryer L., Parbu-Patel A., Carling D. (2002) The anti-diabetic drugs rosiglitazone and metformin stimulate AMP-activated protein kinase through distinct signaling pathways. J Biol Chem 277: 25226–25232 [DOI] [PubMed] [Google Scholar]
- Gardner D., Tai E. (2012) Clinical features and treatment of maturity onset diabetes of the young (MODY). Diabetes Metab Syndr Obes 5: 101–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaziano J., Cincotta A., O’Connor C., Ezrokhi M., Rutty D., Ma Z., et al. (2010) Randomized clinical trial of quick-release bromocriptine among patients with type 2 diabetes on overall safety and cardiovascular outcomes. Diabetes Care 33: 1503–1508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruessner A. (2011) 2011 update on pancreas transplantation: comprehensive trend analysis of 25,000 cases followed up over the course of twenty-four years at the International Pancreas Transplant Registry (IPTR). Rev Diabet Stud 8: 6–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruzman A., Babai G., Sasson S. (2009) Adenosine monophosphate-activated protein kinase (AMPK) as a new target for antidiabetic drugs: a review on metabolic, pharmacological and chemical considerations. Rev Diabet Stud 6: 13–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermanides J., Norgaard K., Bruttomesso D., Mathieu C., Frid A., Dayan C., et al. (2011) Sensor-augmented pump therapy lowers HbA(1c) in suboptimally controlled Type 1 diabetes; a randomized controlled trial. Diabet Med 28: 1158–1167 [DOI] [PubMed] [Google Scholar]
- Hochberg L., Serruya M., Friehs G., Mukand J., Saleh M., Caplan A., et al. (2006) Neuronal ensemble control of prosthetic devices by a human with tetraplegia. Nature 442: 164–171 [DOI] [PubMed] [Google Scholar]
- Kelly C., Flatt C., McClenaghan N. (2011) Stem cell-based approaches for the treatment of diabetes. Stem Cells Int 2011: 424986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knauf C., Cani P., Kim D., Iglesias M., Chabo C., Waget A., et al. (2008) Role of central nervous system glucagon-like peptide-1 receptors in enteric glucose sensing. Diabetes 57: 2603–2612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kojima H., Fujimiya M., Matsumura K., Younan P., Imaeda H., Maeda M., et al. (2003) NeuroD-betacellulin gene therapy induces islet neogenesis in the liver and reverses diabetes in mice. Nat Med 9: 596–603 [DOI] [PubMed] [Google Scholar]
- Lagouge M., Argmann C., Gerhart-Hines Z., Meziane H., Lerin C., Daussin F., et al. (2006) Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell 127: 1109–1122 [DOI] [PubMed] [Google Scholar]
- Larsen C., Faulenbach M., Vaag A., Ehses J., Donath M., Mandrup-Poulsen T. (2009) Sustained effects of interleukin-1 receptor antagonist treatment in type 2 diabetes. Diabetes Care 32: 1663–1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen C., Faulenbach M., Vaag A., Volund A., Ehses J., Seifert B., et al. (2007) Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N Engl J Med 356: 1517–1526 [DOI] [PubMed] [Google Scholar]
- Lee N., Norris S., Thakurta S. (2012) Efficacy and harms of the hypoglycemic agent pramlintide in diabetes mellitus. Ann Fam Med 8: 542–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim E., Hollingsworth K., Aribisala B., Chen M., Mathers J., Taylor R. (2011) Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54: 2506–2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom J., Neumann A., Sheppard K., Gilis-Januszewska A., Greaves C., Handke U., et al. (2010) Take action to prevent diabetes - the IMAGE toolkit for the prevention of type 2 diabetes in Europe. Horm Metab Res 42(Suppl. 1): S37–S55 [DOI] [PubMed] [Google Scholar]
- Lorenzi M. (2007) The polyol pathway as a mechanism for diabetic retinopathy: attractive, elusive, and resilient. Exp Diabetes Res 2007: 61038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin S. (2008) Mammalian hibernation: a naturally reversible model for insulin resistance in man? Diab Vasc Dis Res 5: 76–81 [DOI] [PubMed] [Google Scholar]
- Mattison J., Roth G., Beasley T., Tilmont E., Handy A.M., Herbert R.L., et al. (2012) Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature 489: 318–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mingrone G., Panunzi S., De Gaetano A., Guidone C., Iaconelli A., Leccesi L., et al. (2012) Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med 366: 1577–1585 [DOI] [PubMed] [Google Scholar]
- Narkar V., Downes M., Yu R., Embler E., Wang Y., Banayo E., et al. (2008) AMPK and PPARdelta agonists are exercise mimetics. Cell 134: 405–415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noto H., Goto A., Tsujimoto T., Noda M. (2012) Cancer risk in diabetic patients treated with metformin: a systematic review and meta-analysis. PLoS One 7: e33411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olefsky J., Glass C. (2010) Macrophages, inflammation, and insulin resistance. Annu Rev Physiol 72: 219–246 [DOI] [PubMed] [Google Scholar]
- Olshansky S., Passaro D., Hershow R., Layden J., Carnes B., Brody J., et al. (2005) A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 352: 1138–1145 [DOI] [PubMed] [Google Scholar]
- Pagotto U. (2009) Where does insulin resistance start? The brain. Diabetes Care 32(Suppl. 2): S174–S177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulweber B., Valensi P., Lindstrom J., Lalic N., Greaves C., McKee M., et al. (2010) A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res 42(Suppl. 1): S3–S36 [DOI] [PubMed] [Google Scholar]
- Peterli R., Steinert R., Woelnerhanssen B., Peters T., Christoffel-Courtin C., Gass M., et al. (2012) Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, prospective trial. Obes Surg 22: 740–748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plesner A., Verchere C. (2011) Advances and challenges in islet transplantation: islet procurement rates and lessons learned from suboptimal islet transplantation. J Transplant 2011: 979527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell A., Apovian C., Aronne L. (2011) New drug targets for the treatment of obesity. Clin Pharmacol Ther 90: 40–51 [DOI] [PubMed] [Google Scholar]
- Quinn C., Shardell M., Terrin M., Barr E., Ballew S., Gruber-Baldini A. (2011) Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care 34: 1934–1942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renard E. (2008) Insulin delivery route for the artificial pancreas: subcutaneous, intraperitoneal, or intravenous? Pros and cons. J Diabetes Sci Technol 2: 735–738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross R. (1999) Atherosclerosis – an inflammatory disease. N Engl J Med 340: 115–126 [DOI] [PubMed] [Google Scholar]
- Sachdeva M., Stoffers D. (2009) Minireview: Meeting the demand for insulin: molecular mechanisms of adaptive postnatal beta-cell mass expansion. Mol Endocrinol 23: 747–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saltiel A. (2000) Series introduction: the molecular and physiological basis of insulin resistance: emerging implications for metabolic and cardiovascular diseases. J Clin Invest 106: 163–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer P., Kashyap S., Wolski K., Brethauer S., Kirwan J., Pothier C., et al. (2012) Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 366: 1567–1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt A., Stern D. (2000) RAGE: a new target for the prevention and treatment of the vascular and inflammatory complications of diabetes. Trends Endocrinol Metab 11: 368–375 [DOI] [PubMed] [Google Scholar]
- Schwartz J., Riis J., Elbel B., Ariely D. (2012) Inviting consumers to downsize fast-food portions significantly reduces calorie consumption. Health Aff (Millwood) 31: 399–407 [DOI] [PubMed] [Google Scholar]
- Scranton R., Cincotta A. (2010) Bromocriptine – unique formulation of a dopamine agonist for the treatment of type 2 diabetes. Expert Opin Pharmacother 11: 269–279 [DOI] [PubMed] [Google Scholar]
- Shapiro A., Lakey J., Ryan E., Korbutt G., Toth E., Warnock G., et al. (2000) Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med 343: 230–238 [DOI] [PubMed] [Google Scholar]
- Sovik T., Aasheim E., Taha O., Engstrom M., Fagerland M., Bjorkman S., et al. (2011) Weight loss, cardiovascular risk factors, and quality of life after gastric bypass and duodenal switch: a randomized trial. Ann Intern Med 155: 281–291 [DOI] [PubMed] [Google Scholar]
- Tahrani A., Bailey C., Del Prato S., Barnett A. (2011) Management of type 2 diabetes: new and future developments in treatment. Lancet 378: 182–197 [DOI] [PubMed] [Google Scholar]
- Timmers S., Konings E., Bilet L., Houtkooper R., van de, Weijer T., Goossens G., et al. (2011) Calorie restriction-like effects of 30 days of resveratrol supplementation on energy metabolism and metabolic profile in obese humans. Cell Metab 14: 612–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong W., Shapiro A. (2006) Progress in islet transplantation in patients with type 1 diabetes mellitus. Treat Endocrinol 5: 147–158 [DOI] [PubMed] [Google Scholar]
- United Kingdom Prospective Diabetes Study Group (1995) United Kingdom Prospective Diabetes Study (UKPDS) 13: Relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years. BMJ 310: 83–88 [PMC free article] [PubMed] [Google Scholar]
- United Kingdom Prospective Diabetes Study Group (1998) Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352: 854–865 [PubMed] [Google Scholar]
- Vaisrub S. (1972) Serendipitous sulphonylureas. JAMA 219: 1335 [DOI] [PubMed] [Google Scholar]
- van Belle T., Coppieters K., von Herrath M. (2011) Type 1 diabetes: etiology, immunology, and therapeutic strategies. Physiol Rev 91: 79–118 [DOI] [PubMed] [Google Scholar]
- Vero Science (2010) CYCLOSET® (bromocriptine mesylate) Tablets, oral. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020866s002lbl.pdf
- Viollet B., Lantier L., Devin-Leclerc J., Hebrard S., Amouyal C., Mounier R., et al. (2009) Targeting the AMPK pathway for the treatment of Type 2 diabetes. Front Biosci 14: 3380–3400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson A., Soro-Paavonen A., Sheehy K., Li J., Calkin A., Koitka A., et al. (2011) Delayed intervention with AGE inhibitors attenuates the progression of diabetes-accelerated atherosclerosis in diabetic apolipoprotein E knockout mice. Diabetologia 54: 681–689 [DOI] [PubMed] [Google Scholar]
- Weinzimer S., Tamborlane W. (2008) Sensor-augmented pump therapy in type 1 diabetes. Curr Opin Endocrinol Diabetes Obes 15: 118–122 [DOI] [PubMed] [Google Scholar]
- Whiting D., Guariguata L., Weil C., Shaw J. (2011) IDF Diabetes Atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94: 311–321 [DOI] [PubMed] [Google Scholar]
- Witters L. (2001) The blooming of the French lilac. J Clin Invest 108: 1105–1107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou G., Myers R., Li Y., Chen Y., Shen X., Fenyk-Melody J., et al. (2001) Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 108: 1167-1174 [DOI] [PMC free article] [PubMed] [Google Scholar]