Abstract
Objectives
We evaluated a community-based intervention to promote safe motherhood, focusing on knowledge and behaviors that may prevent maternal mortality and birth complications. The intervention aimed to increase women’s birth preparedness, knowledge of birth danger signs, use of antenatal care (ANC) services, and delivery at a health facility.
Methods
Volunteers from a remote rural community in Northern Eritrea were trained to lead participatory educational sessions on safe motherhood with women and men. The evaluation used a quasi-experimental design (non-equivalent group pretest-posttest) including cross-sectional surveys with postpartum women (pretest N=466, posttest N=378) in the intervention area and in a similar remote rural comparison area.
Results
Women’s knowledge of birth danger signs increased significantly in the intervention area, but not in the comparison area. There was a significant increase in the proportion of women who had the recommended four or more ANC visits during pregnancy in the intervention area (from 18% to 80%, p<.001); while this proportion did not change significantly in the comparison area (from 53% to 47%, p=0.194). There was a greater increase in delivery in a health facility in the intervention area.
Conclusions
Participatory sessions led by community volunteers can increase safe motherhood knowledge and encourage use of essential maternity services.
Keywords: Pregnancy, Maternal Health Services, Africa, Obstetric Labor Complications, Rural Health
INTRODUCTION
Despite dramatic advances in maternity care for women in high and middle income countries, women in developing countries remain at increased risk for preventable birth complications and have high rates of maternal and neonatal mortality.1 Although it is essential to improve referral and transport systems, upgrade health facilities, and increase the number of skilled birth attendants in developing countries, these improvements take considerable economic resources and time to implement. If low-cost, community-based programs can contribute to the prevention of maternal mortality and serious birth complications, they may serve as important adjuncts to larger human resource and infrastructure improvements.
Community-based interventions that encourage use of health facilities for antenatal care (ANC) and delivery, preparations for the birth, and prompt recognition and reaction to danger signs of complications during pregnancy and childbirth have the potential to prevent maternal mortality and birth complications.2 However, with a few notable exceptions,3, 4 rarely have such community interventions been evaluated using experimental or quasi-experimental designs, controlling for other factors that may influence outcomes. Consequently it has been difficult to identify and disseminate successful programs.
Eritrea is located in the northern half of sub-Saharan Africa where early marriage and pregnancy are coupled with poor access to cesarean section. This area has a high maternal mortality ratio (estimated at 430 per 100,000 live births in 2005).5 As of 2006, the national Ministry of Health workforce included only 14 obstetrician/gynecologists and 1184 nurses for a population of 3.37 million, with the lowest coverage in remote rural areas of the country.6 Given the limited resources for comprehensive emergency obstetric care, prevention is a priority.
We examined the effects of a participatory community-based intervention for safe motherhood, developed through a partnership of the Eritrean Ministry of Health, the United Nations Population Fund (UNFPA) Campaign to End Fistula, and the Stanford Eritrean Women’s Health Project. Using pre- and post-intervention assessments, we compared awareness of birth danger signs, birth preparedness, and use of antenatal care and delivery services in an intervention area and a comparison area.
METHODS
The Setting
The intervention area was a district in the Semenawi Keih Bahri (Northern Red Sea) Zone and the comparison area was a district located in the neighboring Anseba Zone. Although both areas are located in Northern Eritrea, they are over 100 kilometers distant from one another and due to lack of transportation and poor roads, contact between the residents of the two areas was unlikely. The areas were similar in healthcare access, having only small primary health care facilities. In both areas the nearest health facility equipped to provide cesarean section was located 2–3 hours away by car on rough roads and transportation was very difficult to arrange. Table 1 presents the characteristics of the two study areas from assessments conducted prior to initiation of the study.
Table 1.
Characteristics of the Study Areas at Initial Assessment in 2005
| Characteristic | Intervention Area | Comparison Area |
|---|---|---|
| Zone | Northern Red Sea | Anseba |
| Number of villages in area (kebabi) | 4 | 6 |
| Estimated catchment population of health facility | 20,665 | 20,722 |
| Numbers and types of health facilities in the area | 1 Health Center in village | 1 Health Center in one village, 1 smaller Health Station in another village |
| Number and types of trained health care providers | 2 nurses and 1 health assistant (associate nurse) | 2 nurses and 2 health assistants (Health Center) and 2 health assistants (Health Station) |
| Location and distance to nearest hospital that can perform cesarean section | Keren Hospital, 3 hours by car (There is a Community Hospital in the nearest town (1 hour by car), but not able to perform c-sections.) | Keren Hospital, 2.25 hours by car |
| Modes of emergency transport | Health Center has one ambulance (not operational at the time of initial assessment), lorry, camel, donkey, walking | Health Center shares one ambulance with Health Station (often no fuel available), public bus to Keren once a day, lorry, camel, donkey, walking |
The Intervention
The focus of the intervention was the training of community members as Maternal Health Volunteers who would then lead participatory educational sessions on safe motherhood topics with women and men in the community. During a community meeting where results from the baseline survey (described later in this article) were presented and discussed, Maternal Health Volunteers were selected using the following criteria: 1) respected persons in the community, 2) permanent residents, 3) literate (preferred but not a requirement), 4) motivated to teach others about safe motherhood, and 5) willing and able to work on a volunteer basis.
Initially 30 female Maternal Health Volunteers participated in a 10-day course led by a team from the Eritrean Ministry of Health to prepare them to conduct participatory discussion groups with fellow community members, and they received a 5-day refresher training approximately one year later. Topics included use of antenatal care; malaria prevention; birth preparedness; recognition of danger signs during pregnancy, labor, and delivery; the importance of prompt referral when complications occur; prevention and treatment of obstetric fistula; and the importance of using skilled birth attendants.
Based on feedback from the community regarding the importance of reaching men with safe motherhood information and cultural norms for separate male and female social gatherings,7 30 male Maternal Health Volunteers were subsequently selected and trained according to the same protocol. After training, each Maternal Health Volunteer formed one or more groups of 15–25 local women/men and began to hold weekly meetings to discuss safe motherhood topics with these groups, using educational materials developed for this purpose. Pregnant women were especially encouraged to attend the women’s groups, but the groups were open to all interested persons in the community. The Maternal Health Volunteers were unpaid but were given per-diem payments during their initial and refresher trainings. The intervention was low-cost; the total cost to train the 60 Maternal Health Volunteers and maintain the intervention activities over a 2-year period was approximately $40,000.
Although the major focus of the intervention strategy was on the Maternal Health Volunteers and the participation of the community, the intervention also included a 6-day training program on interpersonal communication skills for local maternal and child health care providers (nurses and associate nurses) in the intervention area.
Evaluation design and methods
Evaluation of the intervention was conducted using a quasi-experimental study design (non-equivalent group pretest-posttest) to assess the impact of the community intervention on knowledge, attitudes, and practices related to safe motherhood. A variety of methods were used in the baseline (pretest) and final (posttest) assessments, including cross-sectional surveys of postpartum women; focus groups with men, older women, and community leaders; one-on-one qualitative interviews with traditional birth attendants; observation of discussion groups, health facility assessments, and collection of maternity service statistics.8 There was no ethical review committee in Eritrea at the time of the research, but the Eritrean Ministry of Health approved the study and was fully involved in study implementation. The study received ethical approval from the Stanford University Human Research Protection Program.
Several methods were used to promote ownership of this project by the local community. The local community leaders in the intervention area were consulted and involved from the initial visit for selection of the project site to the final assessment visits. After the selection of the intervention community, community leaders and other groups in the community (married men, elder women, and traditional birth attendants (TBAS) were involved in the baseline focus group discussions and in-depth interviews regarding their knowledge and attitudes about safe motherhood, as well as their suggestions for improving maternal health in their community. Following the analysis and write-up of the baseline data, the survey and focus group findings were presented at a community meeting. At this meeting, the community supported the idea of training Maternal Health Volunteers and was active in their selection. The mid-intervention assessment included meetings with community leaders, which were village leaders and representatives of groups that are active at the community level in Eritrea (such as the National Union of Eritrean Women (NUEW) and the National Union of Eritrean Youth & Students (NUEY&S). At this time, the participants stated their support of the project and promised to carry out specific duties to enhance the effectiveness of the project. Focus group discussions and in-depth interviews with community members were repeated at the time of the final assessment. Throughout the life of the project, efforts were made to implement the community members’ suggestions for improving the project.
This report focuses on the results of the cross-sectional surveys with women who had recently given birth. The target sample size for each community at each time point was set at 250 women in each area. This was based on calculations showing that a sample size of 200 women per community (total sample size 400) would result in a power of over 90% to detect a 15% difference in the proportion of women with knowledge of birth danger signs, with an alpha level of .05.
In March–April 2005, the Ministry of Health study team conducted these cross-sectional household surveys of women in the intervention and comparison areas who had given birth in the past 12 months. The sample in each area was identified using a random walk method9 in each village of the selected districts to visit a random selection of households and identify women who had recently given birth. At baseline, 466 women were interviewed by trained female interviewers in Tigre or Arabic language using a semi-structured questionnaire. At the time of the final assessment in June 2007, another cross-sectional sample of 378 women who had given birth in the past 12 months were identified and interviewed using the same methods. Women were taken through an oral informed consent process in the local language and those participating in the surveys gave their signed informed consent. Refusal rates were less than 5% at each time period.
The questionnaires covered socio-demographic characteristics; obstetric history; use of health services for her most recent pregnancy, birth and postpartum periods; knowledge of danger signs; birth preparations; and knowledge about obstetric fistula prevention and repair. The same questionnaire was used at the baseline and final assessments, with only the addition of questions regarding the Maternal Health Volunteer discussion groups to the final questionnaire for the intervention area.
The primary outcomes examined in this report are 1) knowledge of birth danger signs, 2) birth preparedness, and 3) use of maternity services. Knowledge of birth danger signs was measured using women’s unprompted responses to the question, “Do you know any danger signs for a woman who has begun labor and delivery? If yes, which danger signs do you know?” Danger signs listed on the questionnaires (and their explanations) included premature membrane rupture (the bag of water breaks and the woman has no birth pains), meconium staining (waters are brown, yellow, or green), prolonged labor (strong birth pains last more than a day and a night and baby is not born), obstructed labor (pushing with strong birth pains for more than one hour and baby is not born), hemorrhage (too much bleeding), fits/convulsions, fever, cord prolapse (cord comes down in front of baby), and retained placenta (placenta doesn’t come out by 60 minutes after the baby is born).
Birth preparedness10 was measured by coding women’s unprompted responses to the question, “Did you make any plans or preparations for the delivery and potential complications before your most recent birth? If yes, what type of preparations did you make?” The woman was coded as having made birth preparations if she mentioned one or more of the following types of preparations: (1) identified the nearest health facility where she could go if there were problems, (2) found out how to arrange transportation if necessary to go to a health facility, (3) set aside money to pay for transportation and/or medical care, (4) decided who would go along if she had to go to a health facility, (5) talked with the nearest trained health worker about the upcoming birth, or (6) decided who would assist with the birth.
Key indicators for use of antenatal care included any use of ANC services, timing of the first ANC visit, and total number of ANC visits during pregnancy. The main ANC use indicator used for the analyses was a dichotomous variable grouped as less than 4 ANC visits vs. 4 or more ANC visits (the minimum number recommended by WHO11 and the Eritrean Ministry of Health). The location of the delivery (home vs. health facility) was used as an indicator of skilled birth attendance, since trained health workers do not conduct deliveries outside of the health facility in these areas. In addition women were asked if they (or the infant) experienced any problem during the birth.
Chi-square tests and t-tests were initially used to compare the characteristics of women in the two study areas at baseline and at final assessment. Subsequently, the Breslow-Day Test (used to test homogeneity of odds ratios in different strata)12 and ANOVA were used to compare the amount of change in key indicators from baseline to final assessment in the two areas. As has been used in studies with similar designs,13, 14 for categorical variables a P value < .05 for the Breslow-Day Test Chi-Squared indicated that the odds ratios (ORs) for the two study areas for baseline-to-final change were significantly different from one another. For continuous variables, a P value < .05 for the interaction term for area (intervention vs. comparison) and timing (baseline vs. final) in ANOVA indicated that the change from baseline to final is significantly different for the two areas. In order to further examine the change over time in ANC use in the Maternal Health Volunteer intervention area compared with ANC use change in the comparison area, we conducted a logistic regression with number of ANC visits during pregnancy (grouped as 0–3 vs. the recommended ≥4 visits) as the dependent variable and the following independent variables: timing (baseline vs. final), study area (intervention vs. comparison), woman’s education (none vs. some), lifestyle (sedentary vs. nomadic), husband’s occupation (army vs. other), and the interaction between timing and area.
RESULTS
Socio-demographic characteristics
At both baseline and final assessment, women interviewed in the intervention and comparison communities were similar in terms of age, ethnic group, religion, marital status, number of lifetime pregnancies, number of living children, and the proportion who had been pregnant only once (Table 2). However, the comparison area had a significantly higher proportion of women with some education at the time of final assessment (71% vs. 59%, P=.021). Other significant differences between the two areas at final assessment included the proportion living a nomadic or semi-nomadic lifestyle (14% intervention, 2% comparison) and the proportion with a husband who was a soldier in the Eritrean Army (12% intervention, 49% comparison). Soldiers in the Eritrean-Ethiopian Wars and the Independence Struggle have been given preference in some training and employment opportunities in post-independence Eritrea, meaning that women in the comparison area may have had relatively greater access to some social and economic resources, although they had access to the same types of basic health services for pregnancy and childbirth. Given these differences, we adjusted for women’s education, lifestyle and husband’s occupation in the final analyses.
Table 2.
Socio-Demographic Characteristics of Women Interviewed in Intervention and Comparison Areas, at Baseline and Final Assessments (N=844)
| BASELINE (March–April 2005) | FINAL (June 2007) | |||
|---|---|---|---|---|
| Intervention (n=216) | Comparison (n=250) | Intervention (n=129) | Comparison (n=249) | |
| Continuous Variables | ||||
| Mean age (SD) | 28.3 (6.5) | 27.8 (5.8) | 27.7 (5.9) | 27.6 (6.2) |
| Mean age of husband (SD) | 40.81 (9.7) | 38.6 (9.4) | 43.01 (9.7) | 40.0 (9.6) |
| Mean age at first pregnancy (SD) | 17.9 (2.9) | 19.01 (2.9) | 18.8 (2.9) | 18.5 (2.2) |
| Mean age at first birth (SD) | 19.0 (3.0) | 19.51 (2.8) | 19.8 (3.0) | 19.5 (2.4) |
| Categorical Variables | ||||
| Tigre ethnic group, n (%) | 204 (94.4)2 | 250 (100)1 | 129 (100) | 249 (100) |
| Muslim, n (%) | 216 (100) | 250 (100) | 129 (100) | 249 (100) |
| With some formal education,3 n (%) | 76 (35.5) | 114 (45.6) | 76 (58.9) | 176 (70.7)3 |
| Lifestyle nomadic or semi-nomadic (versus sedentary), n (%) | 25 (11.6)1 | 5 (2.0) | 18 (14.0)1 | 5 (2.0) |
| Currently living with husband, n (%)4 | 215 (100) | 247 (98.8) | 127 (98.4) | 244 (98.0) |
| Husband currently working, n (%) | 156 (72.2) | 224 (90.0)1 | 112 (87.5) | 222 (91.7) |
| Husband who is a soldier, n (%) | 32 (14.9) | 106 (42.6)1 | 15 (11.7) | 121 (49.0)1 |
| Has a job that earns money, n (%)4 | 2 (0.9) | 8 (3.2) | 2 (1.6) | 13 (5.2) |
| First pregnancy, n (%) | 33 (15.3) | 40 (16.0) | 24 (18.6) | 41 (16.7) |
| Three or more living children, n (%) | 151 (69.9) | 156 (62.4) | 81 (62.8) | 145 (59.2) |
P value from chi-square (categorical variables) or t-test (continuous variables) comparing the intervention and comparison areas < .05.
Twelve women from the Rashaida ethnic group were interviewed in the Intervention area at baseline.
Any formal education, including female literacy courses (but not including Koran courses)
Fisher’s Exact Test used to compare the two areas, due to expected value < 5 for 1 or more cells.
Participation in the Intervention
Of the 129 women interviewed during the final assessment in the intervention area, 90% had heard of the Maternal Health Volunteer program and 81% had participated in a Maternal Health Volunteer discussion group. Approximately 25% of those who had heard of the intervention stated that their husband had attended a Maternal Health Volunteer discussion group.
Knowledge of Birth Danger Signs
Despite the similarity of the two study communities on most socio-demographic characteristics, we found that many indicators of knowledge related to safe motherhood were significantly higher in the comparison area at baseline and the differences were large and consistent for most of the variables examined (see Table 3). By the time of the final assessment, knowledge of several birth danger signs was significantly improved in the intervention area, but there was no significant change in the comparison area.
Table 3.
Changes in Knowledge of Birth Danger Signs and Birth Preparedness (N=844)
| Women spontaneously mentioning the indicator, n (%)
|
|||||||
|---|---|---|---|---|---|---|---|
| Intervention Area | Comparison Area | P value from Breslow-Day Test of Homogeneity of Odds Ratios1 | |||||
|
| |||||||
| Baseline (n=216) | Final (n=129) | Odds Ratio for Final vs Baseline (95% CI) | Baseline (n=250) | Final (n=249) | Odds Ratio for Final vs Baseline (95% CI) | ||
| Birth Danger Sign Indicators | |||||||
|
| |||||||
| Prolonged or obstructed labor | 36 (16.7) | 38 (29.5) | 2.09 (1.24–3.52)2 | 77 (30.8) | 77 (31.0) | 1.01 (0.69–1.48) | P=.027 |
| Hemorrhage | 41 (19.0) | 56 (43.4) | 3.27 (2.01–5.33)2 | 95 (38.0) | 92 (37.1) | 0.96 (0.67–1.38) | P<.001 |
| Fever | 25 (11.6) | 39 (30.2) | 3.31 (1.89–5.80)2 | 47 (18.8) | 64 (25.8) | 1.50 (0.98–2.30) | P=.027 |
| Retained placenta | 8 (3.7) | 9 (7.0) | 1.95 (0.73–5.19) | 32 (12.8) | 34 (13.7) | 1.08 (0.64–1.82) | P=.294 |
| Cord prolapse | 8 (3.7) | 12 (9.3) | 2.67 (1.06–6.71)2 | 20 (8.0) | 9 (3.6) | 0.43 (0.19–0.97) 2 | P=.003 |
| Meconium staining | 0 (0) | 1 (0.8) | non– significant3 | 5 (2.0) | 3 (1.2) | 0.60 (0.14–2.54) | P=.138 |
| Convulsions | 22 (10.2) | 5 (3.9) | 0.35 (0.13–0.96) 2 | 17 (6.8) | 12 (4.8) | 0.70 (0.33–1.49) | P=.289 |
| Any birth danger sign | 91 (42.1) | 79 (61.2) | 2.17 (1.39–3.39) 2 | 164 (65.9) | 138 (55.6) | 0.65 (0.45–0.93)2 | P<.001 |
|
| |||||||
| Birth Preparedness Indicators | |||||||
|
| |||||||
| Identified nearest health facility | 30 (13.9) | 65 (50.4) | 6.30 (3.75–10.56) 2 | 25 (10.0) | 111 (44.8) | 7.26 (4.48–11.77) 2 | P=.693 |
| Arranged transportation | 12 (5.6) | 22 (17.1) | 3.50 (1.67–7.34) 2 | 18 (7.2) | 29 (11.7) | 1.70 (0.92–3.15) | P=.141 |
| Set aside money | 8 (3.7) | 21 (16.3) | 5.06 (2.17–11.79) 2 | 9 (3.6) | 26 (10.5) | 3.12 (1.43–6.81) 2 | P=.411 |
| Talked with a trained HW | 2 (0.9) | 11 (8.5) | 9.98 (2.17–45.76) 2 | 21 (8.4) | 31 (12.5) | 1.55 (0.86–2.78) | P=.015 |
| Made any birth preparations | 86 (39.8) | 110 (85.3) | 8.75 (5.01–15.29) 2 | 66 (26.5) | 190 (76.6) | 9.08 (6.05–13.64) 2 | P=.916 |
The Breslow-Day Test was used to test the homogeneity of Odds Ratios (ORs) in different strata of the data (i.e., to compare the OR for change over time in the intervention area with the OR for change over time in the comparison area).
P value of the OR from univariate logistic regression comparing baseline and final for the area is < .05, indicating a significant change in the indicator over time within the area.
Fisher’s Exact Test used to compare baseline and final, due to expected value < 5 for 1 or more cells.
Birth Preparedness
As shown in the bottom panel of Table 3, the percentages of women who reported making any of the specified birth preparations increased greatly in both areas over the study period (from 39.8% to 85.3% in the intervention area and from 26.5% to 76.6% in the comparison area). In particular, there were large increases in the proportion of women who said that prior to the birth they identified the nearest health facility they could go to if there was a problem in both areas (from 13.9% to 50.4% in the intervention area and from 10% to 44.8% in the comparison area).
Use of Antenatal Care
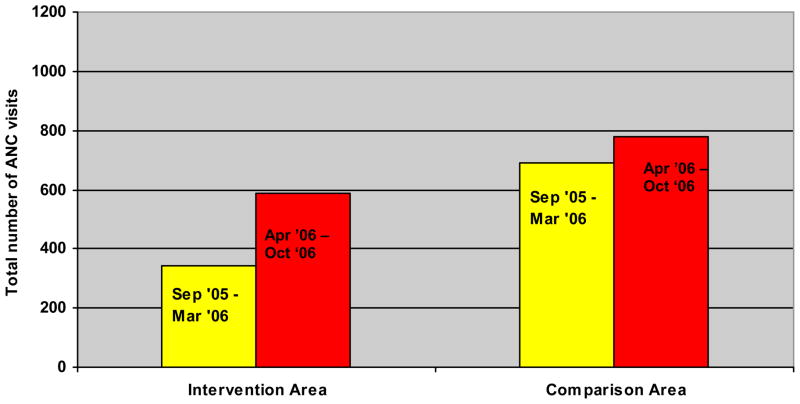
There were significant improvements in reported use of antenatal care over the study period in the intervention area, but not in the comparison area (Table 4). The significant increases in ANC indicators over time in the intervention area persisted after statistically controlling for women’s education, husband’s occupation, and sedentary vs. nomadic lifestyle (data not shown). For those who did use ANC services, the mean number of visits during the recent pregnancy increased from 2.9 to 5.4 (P< .001) in the intervention area, while the mean remained stable at 3.7 visits in the comparison area. As shown in Figure 1, service statistics from the health center in the intervention area also showed a large increase in use of ANC services, from 344 total ANC visits (including both first and return visits) in the 9 months pre-intervention to 586 visits in the 9-month period after the intervention began (increase of 242 visits). In the comparison area there was a smaller increase in total visits, from 689 ANC visits in the 9 months pre-intervention to 778 visits in the following 9-month period (increase of 89 visits).
Table 4.
Changes in Use of Facility-Based Maternity Services (N=844)
| Indicator | Intervention Area | Comparison Area | P value from Breslow-Day Test of Homogeneity of Odds Ratios1 | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Baseline (n=216) | Final (n=129) | Odds Ratio for Final vs Baseline (95% CI) | Baseline (n=250) | Final (n=249) | Odds Ratio for Final vs Baseline (95% CI) | ||
| Four or more ANC visits, n (%) | 40 (18.5) | 101 (79.5) | 17.09 (9.85–29.66) 2 | 133 (53.2) | 117 (47.4) | 0.79 (0.56–1.13) | P<.001 |
| Initial ANC visit in the 1st trimester,3 n (%) | 12 (7.4) | 36 (28.6) | 6.72 (3.34–13.52) 2 | 20 (8.5) | 20 (8.8) | 1.01 (0.53–1.93) | P=.001 |
| Any use of ANC, n (%) | 161 (74.9) | 128 (99.2) | 42.93 (5.86–314.57) 2, 4 | 235 (94.0) | 226 (91.5) | 0.69 (0.34–1.37) | P<.001 |
| Delivery at a health facility,5 n (%) | 7 (3.2) | 58 (46.8) | 26.24 (11.42–60.27) 2 | 9 (3.6) | 31 (15.2) | 4.80 (2.23–10.34) 2 | P=.003 |
The Breslow-Day Test was used to test the homogeneity of Odds Ratios (ORs) in different strata of the data (i.e., to compare the OR for change over time in the intervention area with the OR for change over time in the comparison area).
P value of the OR from univariate logistic regression comparing baseline and final for the area is < .05, indicating a significant change in the indicator over time within the area.
Among those who had at least one ANC visit (N=749).
Due to approaching the ceiling for this variable at the time of the final assessment (128/129 women), the OR is large with a very wide confidence interval.
Intervention area, n=340 (216 baseline and 124 final), Comparison area, n=454 (250 baseline and 204 final) for this variable, due to missing data.
Figure 1.
Total numbers of ANC visits at Health Centers in the Intervention and Comparison Areas from Service Statistics
Pre-Intervention Period, Sept.05–March 06 (yellow); Post-Intervention period, April–Oct 2006 (red)
Table 5 presents the results of the multivariate logistic regression examining the change over time in ANC use in the intervention area compared with change in ANC use in the comparison area; adjusting for pre versus post intervention time, study area, woman’s education, lifestyle, husband’s occupation, and the interaction between timing and area. The interaction between timing and area was highly significant (P<.001) after controlling for these factors. This significant interaction term means that the relationship between pre versus post intervention time and the outcome was very different in two study areas; in this case reflecting the fact that ANC use improved significantly over time in the intervention area, while there was no significant change in this indicator over time in the comparison area. Education and lifestyle also remained significant in this model, with women who had some formal education and women living sedentary lifestyles having significantly higher odds of having had 4 or more ANC visits.
Table 5.
Multivariate logistic regression of predictors of having ≥ 4 Antenatal Care (ANC) visits, N=833
| Odds Ratios for ≥ 4 ANC Visits after Adjustment for Covariates | 95% Confidence Intervals for Adjusted Odds Ratios | |
|---|---|---|
| Women’s education | ||
| No formal education r | 1.00 | |
| Some formal education | 1.562 | 1.13 – 2.14 |
| Lifestyle | ||
| Nomadic or semi-nomadic r | 1.00 | |
| Sedentary | 2.211 | 1.06 – 4.60 |
| Husband’s occupation | ||
| Other r | 1.00 | |
| Eritrean army | 0.98 | 0.70 – 1.37 |
| Study area | ||
| Comparison r | 1.00 | |
| Intervention | 0.223 | 0.14 – 0.33 |
| Timing | ||
| Baseline r | 1.00 | |
| Final | 0.723 | 0.50 – 1.03 |
| Study area x timing | ||
| Interaction | 23.732 | 12.09 – 46.56 |
reference group
p value < .05
p value < .01
These overall coefficients are difficult to interpret due to the important interaction between study area and timing, with effects operating in different directions in the two study areas.23
Use of Health Facility Delivery Services
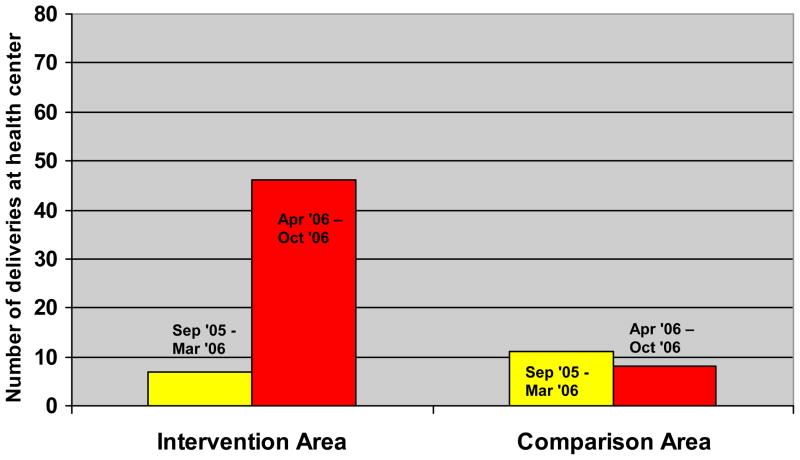
The proportion of women who reported delivering in a health facility increased from 3% (n = 7/216) to 47% (n = 58/124) in the intervention area, and from 4% (n = 9/250) to 15% (n = 31/204) in the comparison area (Breslow-Day Test=9.113, P= .003). As shown in Figure 2, service statistics from the health center in the intervention area also showed an increase in use of facility-based delivery services, from only 7 health facility deliveries in the 9 months pre-intervention to 46 health facility deliveries in the 9-month period after the intervention began. In the comparison area, the number of health facility deliveries actually decreased from 11 during the first 9-month period to 8 during the following 9 months.
Figure 2.
Numbers of Health Center Deliveries in the Intervention and Control Areas from Service Statistics
Pre-Intervention period, Sept.05–March 06 (yellow); Post-Intervention Period, April–Oct 2006 (red)
Birth Complications
There was a significant decrease in the proportion of women who reported that they or the infant experienced a problem during their recent birth in the intervention area (from 34% to 13%, p<.001), while the proportion did not change significantly in the comparison area (from 11% to 8%, p=.224). However the difference in the odds ratios for the two areas did not reach statistical significance (Breslow-Day Test=3.47, P= .062).
DISCUSSION
In this controlled study, we found that a low-cost, community-based intervention was associated with significant improvements in safe motherhood knowledge and use of essential maternity services. The intervention affected not only safe motherhood knowledge and attitudes, but also actual use of health services that are known to prevent maternal mortality and birth complications.
The intervention had significant positive effects on safe motherhood knowledge, but there were also improvements in the comparison area during this time period. These improvements may be due to other safe motherhood campaigns of the Eritrean Ministry of Health and/or the increased educational level of women. Female literacy courses appear to have greatly contributed to women’s education in both areas during the time period, with around 41% of all participants having attended such a course at final assessment, compared with 27% at baseline. However, the gains in awareness of birth danger signs were generally greater in the intervention area than in the comparison area. Nonetheless, increases to women’s safe motherhood knowledge are not likely to be sufficient on their own to prevent infant and maternal morbidity and mortality, especially in settings where there are significant financial, logistical, and social barriers to seeking skilled maternity care.15
Between 2005 and 2007, the proportion of women surveyed who reported that they made safe motherhood preparations before their recent birth increased greatly in both the intervention and the control areas. Again, the campaigns of the Eritrean Ministry of Health and increased educational levels can be cited as potential reasons behind this positive trend. However, the Maternal Health Volunteer intervention had a significant effect on use of ANC services at the final assessment when compared to the baseline assessment; illustrated by more use of any ANC, more total visits during pregnancy, and first visits earlier in pregnancy. These indicators did not improve in the comparison area. Greater improvement in the intervention area was also observed in health facility service statistics and remained significant after statistically controlling for other potential explanatory factors, including the woman’s education, lifestyle, and husband’s occupation. In addition, it appears that the intervention resulted in a greater proportion of women delivering in health facilities with a skilled attendant and fewer women reporting maternal and/or infant problems during the birth. Although women surveyed may have obtained maternity care at other health facilities, the service statistics presented give another indication of trends in maternity service use in the two areas.
Thus, it appears that this community intervention successfully increased safe motherhood behaviors that are known to prevent maternal mortality and birth complications. Women in the intervention area gained knowledge about birth danger signs, increased their birth preparedness, increased their use of ANC services (thus giving ANC providers more opportunities to inform women about danger signs, increase birth preparedness, and encourage delivery with a skilled attendant, as well as identify risk factors), and increased their use of skilled attendants for delivery.
Although not specifically tested in this study, the effectiveness of this program may be due to the use of participatory community-based methods. Since the 1970s, there has been increasing international recognition that communities can make deep and lasting contributions to their own health and well-being, and participatory community programs have been shown to result in significant improvements in maternal and newborn health in diverse settings around the world.4, 16, 17 The benefits of empowering communities to address their own health problems include: community contribution of resources that are not present within the formal health care system, facilitating information transfer to those who are hardest to reach, articulating community needs to government officials, and creating culturally appropriate strategies to address health problems.18 Community participation and developing the capacity of women, their families, and communities to better care for themselves has been identified as a key strategy by the World Health Organization Making Pregnancy Safer Department.19
Some limitations of the evaluation research methods should be recognized. As is the case in many real-world operations research studies,20 and due to time and resource constraints, it was not feasible to randomly assign individuals or a large number of communities to the intervention and comparison arms of the study. With respect to the matching of characteristics and demographics between the intervention and comparison areas, the differences in the proportions of women with some education (71% in the comparison area vs. 59% in the intervention area) and the proportions with husbands in the Eritrean army (49% in the comparison area vs. 11% in the intervention area) may have meant that women in the comparison area had better access to information and resources than did women in the intervention area. Given this situation, it is impressive that the intervention area reached or surpassed the level of the comparison area on key maternal health indicators following the intervention. However, the lower baseline levels in the intervention area suggests that there was more room for significant improvement in that setting, whereas the comparison area had less room for improvement on some of the indicators studied. It has been noted that the effects of some health interventions are likely to be larger when baseline levels of the desired outcome are low.21 However several important safe motherhood indicators, including initial ANC visit during the first trimester of pregnancy and skilled delivery attendance, were also at very low levels at baseline in the comparison area (8% and 4%, respectively) and did not show the same magnitude of improvement that we observed in the intervention area.
Another limitation was the lower sample size attained in the intervention area at the time of the final assessment, despite the inclusion of the same villages and use of the same sampling methods. The data collection team reported that there were fewer women who had recently given birth in the intervention community—possibly due to recent drought conditions and reduced fertility. Limitations inherent in the study design included the fact that a sample of women who gave birth in the last 12 months does not include those women who died during childbirth (survivor bias), and the fact that the survey data is based on self-reports—women may have reported behaviors that they thought would please the interviewer. However, the service statistics on ANC and delivery service use in the two areas also support the greater improvements in the intervention area.
An important strength of this study is the use of a quasi-experimental study design that included a comparison area and pre- and post-intervention assessments to identify temporal trends. Significant change was apparent in a relatively short time, and it is possible that the effects will be even greater as the intervention continues in the Northern Red Sea Zone. Based on the results of this evaluation, similar Maternal Health Volunteer interventions were initiated by the Ministry of Health in nine other health districts in Eritrea.22 While there is an urgent need for improvements in access to emergency obstetric care and the quality of maternity services, such community efforts can significantly contribute to improved maternal health and prevention of maternal and infant mortality and morbidity in remote settings.
Acknowledgments
First, we would like to thank the women, health workers, Maternal Health Volunteers, and other community members who gave their time and shared their experiences with us during this intervention study. We also acknowledge the hard work of the data collection teams who conducted the survey, focus groups, and one-on-one interviews in the two study areas. The field work for this study; including data collection, coding, data entry, and data cleaning; was conducted by the Health Promotion Unit of the Eritrean Ministry of Health. We especially acknowledge the work of Beshir Salih, Mussie Tessema, Amanuel Kifle, Senait Mesfin, and Fatima Hassan for their assistance in gathering, managing, and analyzing the data. We thank Suellen Miller, Sara Brubaker, Beth Cohen, Carinne Meyer, Sun Yu, and Amy Markowitz of UCSF for their helpful comments on the manuscript. We also appreciate helpful feedback throughout the duration of the study from Berhane Ghebretinsae (Director General of the MOH), Berhana Haile (Head of the Reproductive Health Unit of the MOH), Berhane Debru (Head of Clinical Services in the MOH) and Charlotte Gardener, Dirk Jena, and Elsa Mengasteab of the UNFPA Eritrea Office. We acknowledge the financial and logistical support of the Eritrea Office of the United Nations Population Fund (UNFPA) and the Eritrean Ministry of Health (MOH) in carrying out this project. Janet Molzan Turan’s work on this article was also supported, in part, by grant # K01MH081777 from the U.S. National Institute of Mental Health (NIMH).
Biographies
Janet Molzan Turan, PhD, MPH, is an Assistant Professor in the Department of Obstetrics, Gynecology, and Reproductive Sciences at the University of California, San Francisco, USA.
Mekonnen Tesfagiorghis was a member of the Health Promotion Unit, Eritrean Ministry of Health. He is currently with the National Blood Transfusion Center, Asmara, Eritrea.
Mary Lake Polan, MD, PhD, MPH is a Professor in the Department of Obstetrics and Gynecology, Stanford University, Stanford, CA, USA.
Footnotes
Disclaimers: none
References
- 1.Obaid TA. No woman should die giving life. Lancet. 2007 Oct 13;370(9595):1287–1288. doi: 10.1016/S0140-6736(07)61550-5. [DOI] [PubMed] [Google Scholar]
- 2.Wegner MN, Ruminjo J, Sinclair E, Pesso L, Mehta M. Improving community knowledge of obstetric fistula prevention and treatment. Int J Gynaecol Obstet. 2007 Nov;99( Suppl 1):S108–111. doi: 10.1016/j.ijgo.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 3.Brazier E, Andrzejewski C, Perkins ME, Themmen EM, Knight RJ, Bassane B. Improving poor women’s access to maternity care: Findings from a primary care intervention in Burkina Faso. Soc Sci Med. 2009 Sep;69(5):682–690. doi: 10.1016/j.socscimed.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Manandhar DS, Osrin D, Shrestha BP, et al. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004 Sep 11;364(9438):970–979. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 5.WHO, UNICEF, UNFPA, The World Bank. . Maternal Mortality in 2005. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 6.Ministry of Health [Eritrea] Annual Health Service Activity Report of Year 2006. Asmara, Eritrea: HMIS, R & HRD, Ministry of Health [Eritrea]; 2007. [Google Scholar]
- 7.Gebremedhin TG. Women, Tradition and Development: A Case Study of Eritrea. Asmara, Eritrea: The Red Sea Press, Inc; 2001. [Google Scholar]
- 8.Turan JM Eritrean Ministry of Health, UNFPA. . Final Report on the Pilot Community Mobilization/Education Project for Promotion of Safe Motherhood and Prevention of Obstetric Fistula in Eritrea. Nov, 2007. [Google Scholar]
- 9.Milligan P, Njie A, Bennett S. Comparison of two cluster sampling methods for health surveys in developing countries. Int J Epidemiol. 2004 Jun;33(3):469–476. doi: 10.1093/ije/dyh096. [DOI] [PubMed] [Google Scholar]
- 10.Stanton CK. Methodological issues in the measurement of birth preparedness in support of safe motherhood. Eval Rev. 2004 Jun;28(3):179–200. doi: 10.1177/0193841X03262577. [DOI] [PubMed] [Google Scholar]
- 11.Villar J, Bergsjo P. WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. Geneva, Switzerland: World Health Organization; 2002. WHO/RHR/01.30. [Google Scholar]
- 12.Armitage P, Berry G, Matthews JNS. Statistical Methods in Medical Research. 4. Blackwell Publishers; 2001. [Google Scholar]
- 13.O’Rourke K, Howard-Grabman L, Seoane G. Impact of community organization of women on perinatal outcomes in rural Bolivia. Rev Panam Salud Publica. 1998 Jan;3(1):9–14. doi: 10.1590/s1020-49891998000100002. [DOI] [PubMed] [Google Scholar]
- 14.Feinberg AN, Lowry M, 3rd, Koelsch R. Early newborn discharge: a tale of two hospitals. Clin Pediatr (Phila) 2002 Mar;41(2):99–104. doi: 10.1177/000992280204100205. [DOI] [PubMed] [Google Scholar]
- 15.Family Care International. Testing Approaches for Increasing Skilled Care During Childbirth: Key Findings. New York, NY: Family Care International; Oct, 2007. [Google Scholar]
- 16.CEDPA. Mobilizing Communities for Safe Motherhood. 2003. [Google Scholar]
- 17.JHPEIGO. Mobilizing for Impact, Engaging Guatemalan Communities to Save Mothers. Baltimore, MD: JHPIEGO; 2004. [Google Scholar]
- 18.Howard-Grabman L, Snetro G. How to Mobilize Communities for Health and Social Change: A Field Guide. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs (CCP), Health Communication Partnership; 2003. [Google Scholar]
- 19.World Health Organization. Department of Making Pregnancy Safer, Annual Report 2007. Geneva: World Health Organization; 2008. [Google Scholar]
- 20.Fisher AA, Laing J, Stoeckel J. Guidelines for overcoming design problems in family planning operations research. Stud Fam Plann. 1985 Mar-Apr;16(2):100–105. [PubMed] [Google Scholar]
- 21.Lewin S, Lavis JN, Oxman AD, et al. Supporting the delivery of cost-effective interventions in primary health-care systems in low-income and middle-income countries: an overview of systematic reviews. Lancet. 2008 Sep 13;372(9642):928–939. doi: 10.1016/S0140-6736(08)61403-8. [DOI] [PubMed] [Google Scholar]
- 22.UNFPA. The Campaign to End Fistula: 2007 Annual Report. New York, New York: UNFPA; 2007. [Google Scholar]
- 23.Vittinghoff E, Glidden DV, Shiboski SC, McCulloh CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. New York, NY: Springer; 2005. [Google Scholar]