Abstract
Research on the predictors of response to cognitive-behavioral treatments for PTSD has often produced inconsistent or ambiguous results. We argue this is in part due to the use of statistical techniques that explore relationships among the entire sample of participants rather than homogeneous subgroups. Using two large randomized controlled trials of Cognitive Processing Therapy (CPT), CPT components, and Prolonged Exposure, we employed growth mixture modeling to identify distinct trajectories of treatment response and to determine the predictors of those trajectories. We determined that the participants' trajectories could be best represented by two latent classes, which we subsequently labeled responders (87% of the sample) and non-responders (13% of the sample). Notably, there was not a separate class for partial responders. Assignment to the non-responder class was associated with receiving the written accounts (WA) component of CPT, a pre-treatment diagnosis of major depression (MDD), and more pre-treatment hyperarousal symptoms. Thus, it appears that some individuals do not benefit from merely writing about their trauma and processing it with the therapist; they may also need to engage in cognitive restructuring to successfully ameliorate their symptoms. Additionally, those who meet criteria for MDD or have high levels of hyperarousal at the onset of treatment might require additional treatment or support.
Keywords: posttraumatic stress disorder, treatment outcomes, cognitive behavior therapy, trajectories
Cognitive processing therapy (CPT) and prolonged exposure (PE) are among the two most commonly employed empirically supported cognitive-behavioral treatments for posttraumatic stress disorder (PTSD; Foa, Keane, Friedman & Cohen, 2009). Their effectiveness for sexual and non-sexual assault survivors is well established (e.g., Chard, 2005; Foa et al, 1999; Foa, Rothbaum, Riggs, & Murdock, 1991; Foa et al., 2005; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Resick & Schnicke, 1992). Yet, there is no consensus on which treatment is superior or recommended for certain types of clinical presentations.
CPT (Resick & Schnicke, 1993) focuses on challenging beliefs and assumptions related to the trauma, oneself, and the world. In the first phase, clients are educated about the symptoms of PTSD, the treatment model, the identification of their beliefs about the trauma and its impact, and the connection between thoughts and feelings. In the second phase of the full CPT protocol, clients write narratives of the traumatic event to allow for the natural expression of emotion. A cognitive-only version of the therapy (CPT-C) can be conducted without the written accounts. In the last phase of treatment, clients continue to challenge faulty cognitions to generate healthier, and more accurate, beliefs about the event(s), the self, others, and the world using a series of worksheets. The proposed mechanism of change involves altering cognitions related to the trauma. In contrast, PE (Foa, Hearst, Dancu, Hembree, & Jaycox, 1994) is predominantly an exposure therapy that includes repeated behavioral and imaginal exposures to the trauma and related trauma reminders. After learning about the symptoms of PTSD and receiving training in controlled breathing for management of anxiety symptoms, clients generate a hierarchy for in vivo exposures to feared situations. Imaginal exposures to the traumatic memory are also completed daily, with the goal of extinguishing the fear network related to the traumatic memories.
The one side-by-side comparison of PE and CPT yielded few significant differences (Resick et al., 2002). Although CPT had a greater impact on two aspects of guilt and on end-state functioning, they were equally successful in targeting PTSD and depression. Recent meta-analyses of the legitimate psychotherapies for PTSD (e.g., Benish, Imel, & Wampold, 2008; Bradley, Greene, Russ, Dutra, & Westen, 2005) underscore their comparability. Consequently, there is a state of clinical equipoise; both CPT and PE are used interchangeably with no specific guidelines about when to choose one over the other. Even the results for CPT and its two subcomponents (CPT-C and written accounts [WA]) were similar at six months after treatment (Resick et al, 2008).
However, to date, the evaluations of the impact of PE and CPT (and its subcomponents) have assumed that the variation in treatment response can be modeled as continuously distributed around a single set of change parameters. Other studies simply split participants into two groups based on pre-treatment and post-treatment assessments only (e.g., Ehlers et al., 1998; Tarrier et al., 1999). There is little recognition of the possibility that there might be several qualitatively distinct trajectories of treatment response (Taylor et al., 2001). There might be groups of individuals who recover quickly, recover and relapse, partially recover, or do not respond. Collapsing these disparate groups might lead researchers to overlook important patterns or draw inaccurate conclusions.
Prior studies of the predictors of treatment response have similar drawbacks, which may partially account for the inconsistent results (see van Minnen, Arntz, & Keijsers, 2002 for a review). Different groups of individuals might have separate sets of predictors. For example, those who recover quickly might have relatively low levels of anger, whereas those who partially recover might have relatively high levels of anger. Furthermore, the predictors that are identified in these omnibus analyses might merely represent the characteristics of the most severe cases when treatments are very successful. If most people recover, the greatest amount of change will be associated with the highest level of symptoms at the initial assessment. An alternative analytic approach would be to identify the predictors that distinguish distinct groups of individuals having similar courses.
To this end, we employed growth mixture modeling (GMM) to identify distinct trajectories of treatment response and to test whether pre-treatment markers differentially predict assignment to those trajectories. GMM is a relatively new statistical procedure that tests for the presence of subgroups of individuals with similar response patterns and allows individual variability around each one (Nagin, 2005). Change parameters are not assumed to be normally distributed. Thus, it offers an important alternative over conventional growth curve modeling (which assumes that change parameters are normally distributed) and latent class growth analysis (which does not account for within-class variability).
Given the novelty of our analytic approach and the exploratory nature of our study, our hypotheses were circumscribed. We predicted three trajectories: a non-responder trajectory, a partial responder trajectory, and a responder trajectory. This prediction was based on the variation in outcomes that have been observed among participants in PTSD treatment studies (e.g., Foa et al., 2005) and the results of two studies on the patterns of treatment response to cognitive-behavioral therapy (e.g., Elliot et al., 2005; Taylor et al., 2001). In the first study, Taylor et al. (2001) used dynamic cluster analysis to identify two distinct groups of participants in CBT treatment for PTSD from motor vehicle accidents: responders and partial responders. In the second study, Elliot et al. (2005) employed GMM to find three response patterns for Vietnam veterans in CBT treatment for PTSD: two with moderate improvement (at different rates) and one with no improvement.
Because CBT treatments require emotional processing of the traumatic event and cognitive processing of new, corrective information (Foa & Kozak, 1986; Foa, Steketee, & Rothbaum, 1989; Resick & Schnicke, 1992), we also predicted that participants with more numbing or depression (indicating rigid beliefs about the self and the world; e.g., Beck, 1976; Gan, Zhang, Wang, Wang, & Shen, 2006) at pre-treatment would have an increased odds of being assigned to the non-responder and partial responder trajectories compared to participants with lower levels of the symptoms. These participants would likely find it more difficult to fully process the traumatic event or alter their maladaptive beliefs. Indeed, both numbing and depression were significantly higher among partial responders as compared to responders in Taylor et al.'s (2001) study. Although Elliot et al. (2005) found that higher depressive symptoms were associated with greater improvements in PTSD symptomatology, they posited that their results could reflect a regression to the mean.
We also modeled several predictors that were either significant in previous treatment outcome research (e.g., anger, guilt; Elliot et al., 2005; Rizvi, Vogt, & Resick, 2009; Taylor et al., 2001) or were specifically related to the characteristics of the sample. For example, we thought that it was important to examine the influence of childhood physical and sexual abuse. Adults with histories of childhood abuse tend to have more emotion regulation and interpersonal difficulties (see Cloitre et al., 2010), which could lead to increased reluctance to engage in treatment and decreased effectiveness. In total, we examined 17 predictor variables. Rizvi et al. (2009) used one of the samples included in this study and five of the predictors but conducted different analyses. Due to the large number of predictors, we took a multi-step approach to model building (see Dickstein, Suvak, Litz, & Adler, 2010). First, conceptually similar predictors were grouped together and tested in separate conditional models (named form of treatment, demographics, posttraumatic symptoms, psychiatric disorders, affective states, and abuse history). Then, significant predictors from these exploratory analyses were combined into a final conditional model. Because predictors need to be significant in two models (i.e., the exploratory conditional models and the final conditional model), this approach allows for the identification of the most robust predictors from a relatively large set.
Method
Participants and Procedure
Participants were female victims of interpersonal violence drawn from two large randomized controlled trials of cognitive-behavioral therapy for PTSD (Resick et al., 2008; Resick et al., 2002). Study 1 compared CPT, PE, and a wait-list condition in an intent-to-treat (ITT) sample of 171 female survivors of sexual assault (Resick et al., 2002). Following a 6-week waiting period, participants in the wait-list condition were randomized into either the CPT or PE conditions. Study 2 consisted of a dismantling study of CPT in which the full protocol was compared to its constituent components, CPT-C and WA (Resick et al., 2008). In CPT-C, the two trauma account sessions are removed, and there is an increased emphasis on Socratic questioning with the worksheets from CPT. Conversely, in WA, the trauma account sessions are the predominant focus of the 12 hours of treatment. There are two introductory one-hour sessions in the first week, followed by five weekly two-hour sessions that begin with a homework review and status check. Then, participants write their trauma narrative for one hour with the therapist out of the room. In the last 45 minutes, the client reads the narrative out loud to the therapist and processes the associated emotions with him/her. Unlike CPT and CPT-C, WA contains no cognitive therapy component. The therapist could provide educational information, focus on areas that needed elaboration, ask about thoughts and emotions, make reflective statements, and assign the client to continue to write and read back the account every day between sessions.
An ITT sample of 150 women who had experienced physical and/or sexual assault was randomized into one of the three conditions. The original studies' aims, design, and primary outcomes are detailed in previous publications (Resick et al., 2002, 2008). The two studies were conducted consecutively, with continuous recruitment from the same location. Therefore, there were many salient similarities across the samples, including nearly identical inclusion criteria, as well as similar study design, protocol, therapist training, recruitment methods, participant characteristics, and measurements.
To be included in Study 1, participants must have endorsed at least one discrete incident of completed rape (oral, anal, or vaginal) in childhood or adulthood. For Study 2, participants must have experienced either sexual or physical assault in childhood or adulthood. In both studies, participants were eligible if they had experienced multiple episodes of physical and/or sexual assault or any other lifetime traumatic events. Additionally, participants in both studies were at least 3 months posttrauma, met criteria for PTSD at the time of the initial assessment, and were stable on any psychiatric medications. Women with substance dependence were included in both studies if/when they had been abstinent for 6 months. Those with substance abuse were permitted to participate in the study if they agreed to desist in usage during the period of treatment. Exclusion criteria for both studies were identical, and included current psychosis, suicidal intent, current dependence on drugs or alcohol, and illiteracy. In addition, participants could not be in a currently abusive relationship or a situation where they were being stalked. An earlier study using the combined dataset found no differences in demographic variables (including income, education, and marital status) between the samples in each study (Lester, Resick, Young-Xu, & Artz, 2010).
Both studies were similar in length of active treatment (approximately 6 weeks) and total hours of therapy time (12–13 hours). However, there were slight differences in assessment procedures. The first follow-up for Study 1 occurred 3 months after treatment, and the first follow-up for Study 2 occurred 6 months after treatment. Due to variations in standard practices at the time the studies were conducted, the studies also differed with regard to the handling of participants who terminated from the study early. Individuals in Study 1 did not continue to be assessed after early study termination (i.e., if they dropped out of the study before the post-treatment assessment), whereas those in Study 2 did.
Thirty-six percent of the sample completed all nine assessments that were administered from baseline to the first follow-up. Fifty-two percent completed at least eight assessments, and 61% completed at least seven assessments. The final sample had a mean age of 33.60 (SD = 11.28) and an average of 14.10 (SD = 2.57) years of education. Sixty-five percent were Caucasian and 31% were African American. Forty-eight percent were single, 22% were either married or cohabiting, and 30% were separated, divorced, or widowed. The average number of years since the index (worst) assault was 11.04 (SD = 12.26). In addition to the index event, 17% had been in a natural disaster, 42% had had a serious accident in which they were seriously injured or felt that their life was seriously threatened, 11% had been exposed to dangerous chemicals or radiation, 27% had experienced other situations of serious injury or fear, 41% had witnessed someone seriously injured or killed, and 32% had seen dead bodies outside of a hospital or funeral home setting during their lifetime.
Measures
PTSD Symptom Scale (PSS)/Postraumatic Diagnostic Scale (PDS)
PTSD symptoms were assessed using the PSS (Foa, Riggs, Dancu, & Rothbaum, 1993) from Study 1, and its modified version, the PDS (Foa, 1995) from Study 2. These measures have been combined in previous treatment studies (e.g., Lester, et al., 2010). Although the wording is slightly different between the measures, each contains 17 items that correspond to the DSM-IV symptoms of PTSD and the scales are nearly identical. Participants indicate the frequency/severity of each symptom in the past week on a scale from 0 = not at all or only one time to 3 = 5 or more times per week/almost always. A total score was obtained by summing the scores of the 17 symptom items. For Study 1, the average total score at pre-treatment was 29.30 (SD = 8.75). For Study 2, the average total score at pre-treatment was 29.01 (SD = 9.53). The PSS and PDS have demonstrated high reliability and validity, and high diagnostic agreement with other clinical diagnostic measures of trauma related psychopathology (Foa, Cashman, Jaycox, & Perry, 1997). In the current study, alpha coefficients were .83 and .86, respectively. Both the PSS and the PDS were administered at baseline, weekly during treatment, and at the posttreatment follow-up assessments. Researchers have recommended clinical cutoff scores of 17 for clinical samples (Griffin, Uhlmansiek, Resick, & Mechanic, 2004).
Demographics
Demographic characteristics were assessed using questionnaires from the Standardized Trauma Interview, adapted from Resick, Jordan, Girelli, Hutter, and Marhoeder-Dvorak's (1988) treatment study. This structured interview covered topics including demographic information, information about the index assault, within-crime reactions, trauma history, social support, and treatment history. Only the demographics (i.e., age, race, education, and marital status) were included in these analyses.
Clinician Administered PTSD Scale (CAPS)
The CAPS (Blake et al., 1990, 1995) is a structured clinical interview that assesses PTSD symptoms. For each symptom, a clinician rates two dimensions—frequency and intensity—on a scale ranging from 0 (never) to 4 (daily) and 0 (none) to 4 (extreme), respectively. CAPS diagnosis and total scores have demonstrated reliability and validity (Weathers, Keane, & Davidson, 2001). Although the CAPS was administered at baseline, post-treatment, and follow-ups, we decided to rely more heavily on the aforementioned self-report measures of PTSD (i.e., the PSS/PDS) because they were administered throughout treatment and there was a greater correspondence in the timing of the administrations between the two studies. However, we did use the baseline CAPS scores to assess symptom levels prior to treatment (M = 72.90, SD = 18.88). We organized the ratings according to the PTSD symptom clusters as defined by the DSM-IV (American Psychiatric Association, 1994) with one exception: the avoidance cluster was split into effortful avoidance (2 symptoms) and emotional numbing (3 symptoms). Alpha coefficients were .80, .61, .75, and .69 for the re-experiencing cluster, effortful avoidance cluster, emotional numbing cluster, and hyperarousal cluster, respectively. Inter-rater reliability on both frequency and intensity ratings exceeded .92 for each symptom cluster.
Structured Clinical Interview for DSM-IV Axis I Disorder-Patient Edition (SCID-I)
The SCID-I (First, Spitzer, Gibbon, & Williams, 1996) is a semi-structured interview designed to assess DSM-IV Axis I disorders. In both Study 1 and Study 2, the interview was conducted at pretreatment to detect the presence of a major depressive disorder, a panic disorder, and several substance dependence disorders. The SCID has generally yielded moderate reliability coefficients. A random sample of tapes selected for diagnostic reliability yielded kappa values ranging from .80 – 1.00 for the aforementioned disorders. Forty-five percent of the total sample reported symptoms consistent with a major depressive disorder and 15% reported symptoms consistent with panic disorder. Because of the exclusionary criteria (i.e., no substance dependence in the 6 months before treatment), only four participants reported symptoms consistent with a diagnosis of substance dependence in the past year. That is, there were four participants in the sample who met criteria for substance dependence in the year before treatment, but not in the 6 months before treatment.
State Trait Anger Expression Inventory (STAXI)
Pre-treatment levels of anger were measured with the 10 state items from the STAXI (Spielberger & Sydeman, 1994), which have response options from 1 = not at all to 5 = very much so. The STAXI scales have demonstrated good internal consistency and good convergent validity with other measures of anger-hostility (Spielberger, Jacobs, Crane, & Russell, 1983). For the current study, the alpha coefficient was .94 and total scores range from 10 to 40.
Trauma Related Guilt Inventory (TRGI)
The TRGI (Kubany et al., 1996) is a 32-item questionnaire that assesses guilt cognitions (22 items) in addition to a number of subscales. Items are scored on a 5-point scale ranging from 1 (never/not at all true) to 5 (always/extremely true). Construct, criterion-related, and discriminant validity have been established with samples of Vietnam veterans and battered women. In the sample, the alpha coefficient for the guilt cognitions scale was .92.
Assessing Environments III (AE-III)
Childhood physical abuse victimization was measured using the Physical Punishment Scale of the AE-III (Berger, Knutson, Mehm, & Perkins, 1988). The AE-III examines the experience of punishment during childhood (before age 16) with 12 true or false items ranging from mild (e.g., spanked) to physically damaging (e.g., severely beaten). A total score is computed by summing the positively endorsed items, with a higher score reflecting more physical abuse experiences. The AE-III has demonstrated reliability and validity (Berger, et al., 1988; Feindler, Rathus, & Silver, 2003). In the current study, alpha was .79.
Sexual Abuse Exposure Questionnaire (SAEQ)
Childhood sexual abuse was assessed with the SAEQ (Rowan, Foy, Rodriquez, & Ryan, 1994), a retrospective self-report measure. This study used the 10-item overall exposure portion of the questionnaire in which respondents indicate whether they experienced each of 10 sexual abuse events before the age of 16. An overall exposure score was calculated by summing affirmative responses. The overall exposure portion of the SAEQ has demonstrated reliability and validity in a treatment seeking sample (= .73–.93), as well as statistically significant relationships with PTSD diagnoses and symptom severity. Our alpha coefficient was .83.
Data Analysis
Our primary method of data analysis was growth mixture modeling (GMM), a group-based latent growth modeling approach capable of identifying qualitatively distinct growth trajectories within a given sample (see Jung and Wickrama, 2008). GMM consists of two stages: unconditional and conditional model analyses. Unconditional GMM is used to determine the number of latent classes best fitting the data and conditional GMM is used to test predictors of latent class membership. All GMM analyses were conducted using Mplus version 6.0 (Muthén & Muthén, 2010).
To determine the optimal number of latent classes, we compared the goodness of fit statistics for several unconditional latent class model solutions. Statistics included: (a) the Bayesian Information Criterion (BIC); (b) the Akaike Information Criterion (AIC); (c) the Lo-Mendell-Rubin Likelihood Ratio Test (LMR-LRT); (d) Entropy; and (e) the average latent class probabilities of group membership. Optimal fit is indicated for the solution with the lowest BIC and AIC, a statistically significant LMR-LRT, and an Entropy value and average latent class probabilities approaching 1.00 (Jung and Wickrama, 2008; Nagin & Odgers, 2010). First, we conducted the unconditional models using the data from Study 1. Then, we tried to cross-validate the findings with data from Study 2.
Following selection of a solution for the unconditional model, seven conditional models were tested. The first model, form of treatment, included three binary predictors (received PE, received CPT-C, and received WA), representing the four treatment groups. Because we were interested in comparing CPT to PE and CPT to its subcomponents, CPT was selected as the reference category. The second model, demographics, included four predictors: age, race (minority vs. white), years of education, and marital status (single vs. partnered). The third model, posttraumatic symptoms, included the four pre-treatment scores for the CAPS symptom clusters: re-experiencing, effortful avoidance, numbing, and hyperarousal. These scores provided an assessment of PTSD symptoms that was independent from the outcome measure. The fourth model, psychiatric disorders, included two dichotomous predictors, both assessed at pre-treatment: diagnosis of major depressive disorder and diagnosis of panic disorder. The variables for the other disorders (i.e., the substance dependence disorders) were not included in the model because of low levels of endorsement. The fifth model, affective states, included two predictors: the STAXI state anger subscale and the TRGI guilt cognitions scale. Both were assessed at pre-treatment. The sixth regression model, abuse history, included severity of childhood physical abuse (the AE-III) and severity of childhood sexual abuse (the SAEQ). Significant predictors from these analyses were then combined into a final conditional model. To control for differences in the two studies, we also included a dummy variable coding study (Study 1 = 1, Study 2 = 2) in the final model.
Missing Data
Participants in Study 1 completed a 3-month follow-up assessment and participants in Study 2 completed a 6-month follow-up assessment. Although the different schedules across the two studies created a large amount of missing data at these two time points (69% and 63%, respectively), we did not want to disregard the information. Fortunately, the vast majority of participants were assessed at post-treatment (71%) and at either the 3-month of 6-month follow-up (68%). Additionally, Mplus features full information maximum likelihood (FIML) to account for missing data. This technique does not estimate missing data; rather, it uses all of the available information to arrive at the most likely parameter estimates.
To check for non-ignorable missingness due to dropout (see Muthen, Asparouhov, Hunter, & Leuchter, 2011), we compared average scores for those who dropped out to those who completed the study at each time point. We also used the Diggle-Kenward selection model (Diggle & Kenward, 1994) to model the missing data. Because there were no significant differences between the two groups and the modeling of the missing data did not change the results appreciably in the unconditional analysis, we concluded that the missing at random assumption that underlies FIML was appropriate.
Results
Unconditional Models
First, we used Study 1 data to examine unconditional models ranging in size from 1 to 4 latent classes.1 Based on the goodness of fit statistics (Table 1) and established criteria (see Jung and Wickrama, 2008; Nagin & Odgers, 2010), we deemed the 2-class solution to have the best fit. This solution had BIC and AIC values that were relatively low in comparison to those of the other latent classes, a high Entropy value, and a significant LMR-LRT. The 3- and 4-class solutions had lower sample-size adjusted BIC and AIC values; however, reductions in these values were marginal and the LMR-LRT was non-significant, indicating that the more complex models (i.e., the models with more latent classes) did not provide a significant improvement in model fit.
Table 1.
Goodness of Fit Statistics for Unconditional Model Solutions
| Model | BIC | Sample Size Adjusted BIC | AIC | Entropy | LMR-LRT |
|---|---|---|---|---|---|
| Study 1 | |||||
| 1 Class | 6,836 | 6,791 | 6,792 | - | - |
| 2 Class | 6,823 | 6,763 | 6,764 | 0.92 | 36.75 (p = 0.009) |
| 3 Class | 6,827 | 6,751 | 6,753 | 0.79 | 20.18 (p = 0.171) |
| 4 Class | 6,834 | 6,742 | 6,744 | 0.79 | 15.91 (p = 0.673) |
|
| |||||
| Study 2 | |||||
| 1 Class | 6,917 | 6,872 | 6,875 | - | - |
| 2 Class | 6,901 | 6,841 | 6,843 | 0.79 | 39.57 (p = 0.042) |
| 3 Class | 6,904 | 6,828 | 6,831 | 0.75 | 21.33 (p = 0.097) |
| 4 Class | 6,917 | 6,825 | 6,830 | 0.70 | 16.72 (p = 0.482) |
Note. BIC = Bayesian Information Criterion. AIC = Akaike Information Criterion. LMR-LRT = Lo-Mendell-Rubin Likelihood Ratio Test.
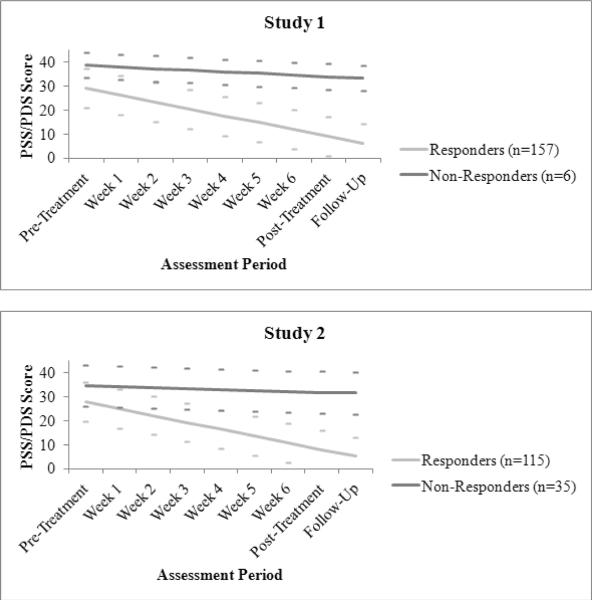
Then, we tried to cross-validate the results with Study 2 data. Again, we deemed the 2-class solution to have the best fit. This solution had the highest Entropy value, a significant LMR-LRT, and sample-size adjusted BIC and AIC values that were only marginally higher than the corresponding values in the more complex models. Furthermore, the growth parameter estimates for the 2-class solution were consistent across studies (see Figure 1). In both datasets, the 2-class solution contained a non-responder group (i.e., persistent, high levels of PTSD symptoms over time) and a responder group (i.e., decreasing symptoms over time). Across the two studies, 13% (n = 41) of participants were assigned to the non-responder group and 87% (n = 272) of participants were assigned to the responder group.
Figure 1.
Trajectories of response to PTSD treatment among assault victims: the two-class unconditional model solutions. The dashed lines represent the trajectories of each class at one standard deviation above and below the predicted values.
Finally, we combined the two samples to provide more power for the conditional analyses. The intercept growth parameter for the non-responder group indicated that group members began trauma-focused treatment with high levels of PTSD symptoms (B = 35.19, SE B = 1.33, 95% CI = 32.58, 37.80, p < .001), and the linear change parameter indicated that this group did not report a significant change in PTSD symptoms over time (B = −0.23, SE B = 0.28, 95% CI = −0.78, 0.32, p = .41). The variance of the parameter estimates for the intercept and slope were 70.55 (SE = 21.96, 95% CI = 27.51, 113.59, p = .001) and 0.84 (SE = 0.54, 95% CI = −0.22, 1.90, p = .123), respectively. The intercept growth parameter for the responder group indicated that group members began treatment with high levels of PTSD symptoms (B = 28.71, SE B = 0.57, 95% CI = 27.59, 29.83, p < .001), and the linear change parameter indicated that this group reported a significant change in PTSD symptoms over time (B = −2.87, SE B = 0.12, 95% CI = −3.11, −2.63, p < .001). The variance of the parameter estimates for the intercept and slope were 52.99 (SE = 5.56, 95% CI = 42.10, 63.89, p < .001) and 1.20 (SE = 0.19, 95% CI = 0.83, 1.58, p < .001), respectively. The average posterior probabilities along the diagonal for the 2-class solution approached 1.00 (Table2), indicating that participants assigned to the two groups were assigned correctly. That is, there were few borderline cases “falling between” the latent classes. The average posterior probabilities along the diagonal for the 3- and 4-class solutions were noticeably smaller.
Table 2.
Average Posterior Probabilities for Most Likely Latent Class Membership (Row) by Latent Class (Column)
| Assigned Group | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| 2-Class Solution | ||||
| 1 | 0.953 | 0.047 | ||
| 2 | 0.049 | 0.951 | ||
|
| ||||
| 3-Class Solution | ||||
| 1 | 0.845 | 0.070 | 0.085 | |
| 2 | 0.116 | 0.792 | 0.092 | |
| 3 | 0.093 | 0.033 | 0.874 | |
|
| ||||
| 4-Class Solution | ||||
| 1 | 0.710 | 0.190 | 0.044 | 0.056 |
| 2 | 0.189 | 0.752 | 0.003 | 0.057 |
| 3 | 0.031 | 0.001 | 0.944 | 0.025 |
| 4 | 0.109 | 0.099 | 0.078 | 0.714 |
Note. Posterior probabilities for the combined dataset are shown.
Predictors of Latent Class Assignment
Among the 17 predictors, four were found to significantly relate to latent class assignment (i.e., responder or non-responder trajectory): received CPT-C, received WA, MDD diagnosis, and total hyperarousal symptoms. Participants who received CPT-C and WA were more likely to be assigned to the non-responder trajectory (compared to individuals who received CPT) as were individuals who had an MDD diagnosis and greater hyperarousal symptoms (see Table 3 for percentages and means). The other variables (received PE, age, race, years of education, marital status, re-experiencing symptoms, effortful avoidance symptoms, numbing symptoms, diagnosis of panic disorder, state anger, guilt cognitions, the AE-III, and the SAEQ) were unrelated to class assignment.
Table 3.
Percentages and Means of Latent Class Predictors in Final Conditional Model
| Variable | Value | Response Group n (%)/ M (SD) | Non-Response Group n (%)/ M (SD) | Test Statistic (df) |
|---|---|---|---|---|
| Dichotomous Variables | ||||
| Received PEa | 78 (94.0) | 5 (06.0) | χ2 = .05 (1) | |
| Received CPT-Ca | 38 (80.9) | 9 (19.1) | χ2 = 5.92 (1)* | |
| Received WAa | 32 (64.0) | 18 (36.0) | χ2 = 24.69 (1)*** | |
| Diagnosis of MDD | Yes | 109 (78.4) | 30 (21.6) | χ2 = 15.33 (1)*** |
| No | 160 (93.6) | 11 (06.4) | ||
|
| ||||
| Continuous Variables | ||||
| Hyperarousal Symptoms | 23.10 (6.64) | 27.00 (6.25) | t = 3.53 (310)*** | |
Note. PE = Prolonged Exposure; CPT-C = Cognitive Therapy only; WA = Written Accounts; MDD = Major Depressive Disorder; BDI-II = Beck Depression Inventory-II.
Participants who received CPT were the reference group for these variables. More than 93% of the participants who received CPT were assigned to the responder group.
p < .05.
p < .001.
When the four predictors (along with the study variable and received PE2) were entered into the final conditional model, received WA, hyperarousal symptoms, and MDD diagnosis retained statistical significance (p = .017, p = .011, and p = .043, respectively). Received CPT-C was no longer significant. Odds ratios and 95% confidence intervals generated from this model are presented in Table 4. The odds of being in the non-responder group were over 4 times greater for patients who received WA compared to those who received CPT, controlling for other predictors in the model. Additionally, the odds of being in the non-responder group were over 3 times greater for patients diagnosed with MDD compared to those not diagnosed with MDD, controlling for the other predictors in the model.
Table 4.
Odds Ratios from Final Conditional Model
| Variable | Odds Ratioa | 95% CI |
|---|---|---|
| Received PE | 1.88 | [0.26, 13.51] |
| Received CPT-C | 1.70 | [0.33, 8.77] |
| Received WA | 4.81* | [1.33, 17.24] |
| Diagnosis of MDD | 3.52* | [1.04, 11.90] |
| Hyperarousal Symptoms | 2.81* | [1.26, 6.25] |
| Study | 3.04 | [0.28, 33.33] |
Note. PE = Prolonged Exposure; CPT-C = Cognitive Therapy only; WA = Written Accounts; MDD = Major Depressive Disorder; BDI-II = Beck Depression Inventory-II.
Odds ratios were generated using the responder group as the reference group.
p < .05.
Discussion
Our analyses revealed two distinct trajectories (a responder trajectory and a non-responder trajectory) for assault survivors engaged in trauma-focused therapy, the targeted population in the initial testing of the therapies. Most individuals (87%) were assigned to the responder trajectory. Average symptom levels in this trajectory were below clinical cutoffs by the end of the study, indicating a positive response to treatment. Nevertheless, 41 individuals (13%) were assigned to the non-responder trajectory. Symptom levels in this trajectory were substantially above the clinical cutoff at all time points. Contrary to expectations, there was no distinct trajectory for partial responders. However, given the variability in the slope of the responder group, the partial responders might represent the lower end of this group. Therefore, the notion of a partial responders group might still be relevant.
Besides determining the number of trajectories (i.e., latent classes) best fitting our data, another objective of our study was to examine whether treatment condition differentially predicted latent class assignment. Although we did not find a significant difference between prolonged exposure (PE) and cognitive processing therapy (CPT), there was a large difference between the latter and the written account component of CPT (WA). Participants who received WA were far more likely to be assigned to the non-responder trajectory compared to CPT as the reference group. Initially, we also found that those who received the cognitive component of CPT (CPT-C) were more likely to be assigned to the non-responder course; however, this relationship failed to retain significance in the final model. Because studies show that CPT, PE, CPT-C, and WA produce similar changes in PTSD symptoms (Resick et al., 2002; Resick et al., 2008), it appears that the average participant can benefit from any of the four treatments. However, individuals with more risk factors (e.g., an MDD diagnosis, high levels of hyperarousal) might require the more comprehensive treatments (i.e., CPT and PE) due to their multifaceted approach. Additionally, there may be other factors that affect treatment success or efficiency. For instance, in an examination of level of dissociation from the dismantling study, Resick, Suvak, Johnides, Mitchell, and Iverson (in press) found that those participants with high levels of dissociation did best with the full CPT protocol while those with low levels of dissociation responded better to CPT-C.
Consistent with Taylor et al. (2001), the presence of a MDD diagnosis was also a significant predictor of class assignment. Thirty of the 41 individuals assigned to the non-responder trajectory had a clinical diagnosis of major depression at pre-treatment. It is likely that individuals with an MDD diagnosis are more at risk for poor treatment response due to the entrenched nature of their maladaptive beliefs and other depressive symptoms (low energy, poor sleep, etc). However, because the large majority of those with MDD fell into the responder group (78.4%), more research is needed to determine in what way depression is a risk factor for poor treatment response. For example, those women who had MDD prior to their index trauma or those who had been depressed longer might be more refractory.
The third and final significant predictor of class assignment was hyperarousal symptom severity. Because CBT requires emotional processing of the traumatic event to uncover maladaptive beliefs (Resick & Schnicke, 1992), we had expected that participants who had difficulty accessing their emotions (because they were numb) would have a slower recovery. However, symptoms related to heightened levels of arousal appear to be the greater impediment to successful treatment. It may be that these symptoms are distracting or incompatible with corrective information about safety. Results suggest that some patients may need help in regulating hyperarousal symptoms before beginning therapy or may need a few more sessions to respond to treatment. To our knowledge, Taylor et al. (2001) was the only other study that examined the relative role of the individual PTSD symptom clusters on response to CBT. The fact that they found that numbing better differentiated the two groups than hyperarousal might be due to the differences in the traumas that were studied. It is likely that the hyperarousal symptoms of motor vehicle survivors are more circumscribed than the hyperarousal symptoms of female interpersonal assault victims.
Limitations and Future Directions
Because of the exploratory nature of our study, we included a large number of predictor variables in the conditional analyses, thereby increasing the chance of making a Type I error. Although we could have employed a Bonferroni correction to reduce this possibility, we decided to maintain the conventional alpha level of .05 to ensure that we identified all of the potential predictors of response. In other words, we chose to limit the chance of making a Type II error rather than a Type I error. We felt that this was appropriate given the novel and exploratory nature of our study.
In addition, it was beyond the scope of the paper to test interaction effects, such as whether one of the treatments had a greater impact on participants with MDD or participants with a relatively high level of hyperarousal symptoms. As the proliferation of CPT and PE increase, it will be important to gauge the relative effectiveness of the treatments for subgroups of participants. It was also beyond the scope of the paper to examine predictors of treatment response within trajectories. Because it is possible that a predictor could be significant for one class but not another, this type of analysis could identify determinants of treatment response that are overlooked using conventional growth curve procedures.
Future research should employ larger treatment samples to more fully explore the spectrum of response trajectories, the relative efficacies of the various treatments, and the relationships among the predictors. We believe that GMM is especially useful for comparisons of efficacy given its ability to distinguish subgroups of responders. Future research should also consider using GMM with other treatment samples to test the generalizability of our results. Because our sample is limited to female sexual and physical assault survivors, it is quite possible that different trajectories or predictors would be identified for other types of traumas or other populations. For example, Elliot et al. (2005) found two partial response trajectories and a non-response trajectory for Vietnam veterans engaged in treatment.
Despite the limitations, we believe that our analysis makes a significant contribution to the treatment literature. To our knowledge, only two other studies have examined latent classes of PTSD treatment response (for Vietnam veterans; Elliott et al., 2005; for survivors of road-traffic collisions; Taylor et al., 2001). By conducting this analysis, we were able to identify two distinct groups of individuals: responders and non-responders. Investigators and therapists should be aware of this dichotomy. Those who are likely to be non-responders could be identified early by an extremely slow or non-existent decrease in symptoms. We also discovered that WA was ineffective for some participants. Apparently, writing a trauma narrative and processing the emotions is not always enough to promote significant symptom relief. Having a therapist who will encourage and teach clients to reappraise dysfunctional beliefs may also be critical. This finding has practical implications because variants of the WA intervention (e.g., written emotional disclosure; see Sloan, Marx, & Greenberg, 2011) are being delivered currently. Additionally, the finding highlights the utility of the GMM methodology for comparisons of treatments because WA appeared to be highly effective for the average participant in the original dismantling study (Resick et al., 2008). Finally, our study represents an initial step toward identifying individuals at pre-treatment who would require additional sessions, more intense psychological care, or alternative treatments.
Highlights
-
>
We employed growth mixture modeling to examine trajectories of treatment response.
-
>
We determined that the trajectories could be best represented by two latent classes.
-
>
Notably, there was not a separate class for partial responders.
-
>
Assignment to the non-responder class was associated with MDD and hyperarousal.
-
>
The effect of treatment condition was also explored.
Acknowledgments
This research was supported by Grant 1-R01-MH51509 and Grant 2-R01-MH51509, awarded by the National Institute of Mental Health to Patricia A. Resick. We thank the therapists, assessors, and research assistants who worked on this project, and the participants who were willing to receive therapy in a research context.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Initially, we tested unconditional models with an intercept, slope, and quadratic term. However, we were forced to drop the quadratic term due to convergence problems and improper solutions. Nevertheless, we determined that the removal of this term had a negligible impact on the results.
We included this predictor in the final model so that the interpretation of the other dummy-coded variables for treatment condition would not change.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. International Univeristies Press; New York: 1976. [Google Scholar]
- Benish SG, Imel ZE, Wampold BE. The relative efficacy of bona fide psychotherapies for treating post-traumatic stress disorder: A meta-analysis of direct comparisons. Clinical Psychology Review. 2008;28:746–758. doi: 10.1016/j.cpr.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Berger AM, Knutson JF, Mehm JG, Perkins KA. The self-report of punitive childhood experiences of young adults and adolescents. Child Abuse and Neglect. 1988;12:251–262. doi: 10.1016/0145-2134(88)90033-6. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;18:187–188. [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Chard MM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73(5):965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, Petkova E. Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry. 2010;167:915–924. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- Dickstein BD, Suvak M, Litz BT, Adler AB. Heterogeneity in the Course of Posttraumatic Stress disorder: Trajectories of Symptomatology. Journal of Traumatic Stress. 2010;23:331–339. doi: 10.1002/jts.20523. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM, Dunmore E, Jaycox L, Meadows E, Foa EB. Predicting response to exposure treatment in PTSD: The role of mental defeat and alientation. Journal of Traumatic Stress. 1998;11(3):457–471. doi: 10.1023/A:1024448511504. [DOI] [PubMed] [Google Scholar]
- Elliott P, Biddle D, Hawthorne G, Forbes D, Creamer M. Patterns of Treatment Response in Chronic Posttraumatic Stress Disorder: An Application of Latent Growth Mixture Modeling. Journal of Traumatic Stress. 2005;18(4):303–311. doi: 10.1002/jts.20041. [DOI] [PubMed] [Google Scholar]
- Feindler EL, Rathus JH, Silver LB. Assessment of family violence: A handbook for researchers and practitioners. American Psychological Association; Washington, DC: 2003. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders: Research Version-Patient Edition. New York State Psychiatric Institute, Biometrics Research Department; New York: 1996. [Google Scholar]
- Foa EB. Posttraumatic Stress Diagnostic Scale (manual) National Computer Systems; Minneapolis, MN: 1995. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Stress Diagnostic Scale. Psychological Assessment. 1997;9(4):445–451. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Stress GP. A comparison of exposure therapy, stress innoculation training, and the combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67(2):194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. 2nd ed. Guilford Press; New York: 2009. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Foa EB, Riggs D, S., Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59(5):715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualization of post-traumatic stress disorder. Behavior Therapy. 1989;20:155–176. [Google Scholar]
- Foa EB, Tolin Comparison of the PTSD Symptom Scale-Interview Version and the Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 2000;13(2):181–191. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- Gan Y, Zhang Y, Wang X, Wang S, Shen X. The coping flexibility of neurasthenia and depressive patients. Personality and Individual Differences. 2006;40:859–871. [Google Scholar]
- Griffin MG, Uhlmansiek MH, Resick PA, Mechanic MB. Comparison of the Posttraumatic Stress Disorder Scale versus the Clinician-Administered Posttraumatic Stress Disorder Scale in domestic violence survivors. Journal of Traumatic Stress. 2004;17(6):497–503. doi: 10.1007/s10960-004-5798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2:302–317. [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory (TRGI) Psychological Assessment. 1996;8:428–444. [Google Scholar]
- Lester K, Resick PA, Young-Xu Y, Artz C. Impact of race on early treatment termination and outcomes in posttraumatic stress disorder treatment. Journal of Consulting and Clinical Psychology. 2010;78(4):480–489. doi: 10.1037/a0019551. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. 6th ed. Muthén & Muthén; Los Angeles, CA: 2010. [Google Scholar]
- Nagin DS. Group-Based Modeling of Development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoeder-Dvorak S. A comparative outcome study of behavioral group therapy for sexual assault victims. Behavior Therapy. 1988;19(3):385–401. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic Posttraumatic Stress Disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70(4):867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Resick PA, Suvak MK, Johnides BD, Mitchell KS, Iverson KM. The impact of dissociation on PTSD treatment with Cognitive Processing Therapy. Depression and Anxiety. doi: 10.1002/da.21938. in press. [DOI] [PubMed] [Google Scholar]
- Resick PA, Uhlmansiek MO, Clum GA, Galovski TE, Scher CD, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76(2):243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Vogt DS, Resick PA. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy. 2009;47:737–743. doi: 10.1016/j.brat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan AB, Foy DW, Rodriguez N, Ryan S. Posttraumatic stress disorder in a clinical sample of adults sexually abused as children. Child Abuse and Neglect. 1994;18:51–61. doi: 10.1016/0145-2134(94)90095-7. [DOI] [PubMed] [Google Scholar]
- Sloan DM, Marx BP, Greenberg EM. A test of written emotional disclosure as an intervention for posttraumatic stress disorder. Behaviour Research and Therapy. 2011;49:299–304. doi: 10.1016/j.brat.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Sydeman SJ. State-Trait Anxiety Inventory and State-Trait Anger Expression Inventory. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcome assessment. Erlbaum; Hillsdale, NJ: 1994. pp. 292–231. [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, Barrowclough C. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67(1):13–18. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- Taylor S, Fedoroff I, C., Koch WJ, Thordarson DS, Fecteau G, Nicki RM. Posttraumatic stress disorder arising after road traffic collisions: Patterns of response to cognitive-behavior therapy. Journal of Consulting and Clinical Psychology. 2001;69(3):541–551. [PubMed] [Google Scholar]
- van Minnen A, Arntz A, Keijsers GPJ. Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behavior Research and Therapy. 2002;40:439–457. doi: 10.1016/s0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. The Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]