Abstract
Over 65,000 primary brain tumors are diagnosed annually in the US alone. Malignant gliomas represent more than one-third of such cases. Despite advances in neuroimaging, surgical techniques, radiotherapy and chemotherapy, the survival rate of this disease remains poor. The introduction of agents which disrupt the function of vascular endothelial growth factor (VEGF) and its receptors to glioma therapy has resulted in an unusually high percentage of patients experiencing radiographic responses. Bevacizumab, approved by the Food and Drug Administration for the treatment of recurrent glioblastoma in 2009, has changed the field of neuro-oncology. The drug has been utilized as a single agent and in combination with the classic cytotoxic agents typically applied in this setting. Numerous studies have reported high response rates and encouraging extensions of time-to-progression. The optimal schedule and combination of bevacizumab with alternative drugs has not been identified. The current study presents the results of a retrospective analysis of the combination therapy utilizing bevacizumab with the alkylating agent carboplatin in patients with recurrent malignant glioma.
Keywords: malignant glioma, carboplatin, anti-VEGF therapy
Introduction
The treatment of malignant glioma is associated with a high failure rate. The majority of patients progress following initial therapy. The current standard of care for newly diagnosed glioblastoma includes maximal safe surgical resection followed by radiotherapy with concomitant and adjuvant chemotherapy (temozolomide) (1). Despite this approach, the median survival rate is estimated to be 14.6 months and only approximately 25% of patients are alive at 2 years from diagnosis. At the time of progression, salvage therapies offer extremely modest efficacy. The majority of salvage therapies are associated with low response rates and a marginal benefit on progression-free and overall survival (OS) rates. Numerous agents have been tried in this setting, offering low response rates ranging from 5 to 20% and median OS between 5 and 7.5 months (2–5).
The introduction of bevacizumab, a humanized monoclonal antibody against vascular endothelial growth factor (VEGF), to the therapy of recurrent glioblastoma (GBM) resulted in a significant improvement in response rates. By removing available circulating VEGF (frequently overexpressed by malignant gliomas), bevacizumab inhibits the proliferation of endothelial cells and the formation of new blood vessels (6), frequently resulting in remarkable radiographic responses. Stark-Vance, who pioneered the use of this antibody in glioma, paved the way for larger studies utilizing bevacizumab in combination with irinotecan in GBM (7). A phase II study led by Vredenburgh confirmed the initial encouraging findings and reported an overall response rate of 57% in patients with recurrent GBM treated with bevacizumab in combination with irinotecan. Of these patients, 46% were progression-free at 6 months (8,9). Single-agent bevacizumab has also been utilized in several prospective studies for recurrent GBM. Reported progression-free survival (PFS) was between 4 and 4.2 months. Between 29 and 42% of patients were free from progression at 6 months and the reported median OS was between 7.8 and 9.2 months (10,11).
Combination therapies utilizing an anti-VEGF platform studied in a prospective fashion include bevacizumab with the following agents: irinotecan (9,10), etoposide (12), erlotinib (13), temzolomide (14), carboplatin plus irinotecan (15) and carboplatin plus etoposide (16). The majority of combinations offered similar benefits but toxicity was generally more pronounced when cytotoxic regimens were added to anti-VEGF therapy. Only one small retrospective study used carboplatin alone in combination with bevacizumab in patients with recurrent malignant glioma (17). A total of 9 patients were treated with this combination (5 with WHO grade III glioma and 4 with WHO grade IV glioma). The PFS rate at 6 months was 40% for grade III and 50% for grade IV patients. Due to the extremely small number of subjects in this retrospective study, it is difficult to draw conclusions concerning the efficacy of this regimen.
Carboplatin, a platinum analog, has been used in therapy for a variety of types of cancer, including ovarian, bladder, head and neck, endometrial, small- and non-small cell lung and germ cell tumors. The drug covalently binds to DNA preferentially at the N-7 position of guanine and is not cell-cycle specific. Following intravenous administration, carboplatin is widely distributed throughout the body and crosses the blood-brain barrier, which makes it particularly attractive for glioma therapy. Carboplatin dosing is based on the target area under the curve (AUC) and, typically, doses between AUC of 4 and 7 mg/ml/min are prescribed. The major toxicity of carboplatin is myelosuppression. Carboplatin monotherapy has been shown to be modestly effective in therapy of recurrent malignant glioma (5,18). The results of combination therapies utilizing carboplatin for this indication have also been encouraging (16,19).
As previously mentioned, only one small retrospective case series evaluated the combination of carboplatin with bevacizumab in recurrent malignant glioma. We present the largest retrospective series of patients treated with this combination at one institution to date.
Materials and methods
We performed a retrospective chart review of patients treated at the University of Washington Medical Center between 2008 and 2010. The local Institutional Review Board approved the study. Patients eligible for the inclusion in the study cohort had to have WHO grade III or IV glioma that progressed following initial or prior therapy. Information was gathered, including patients' demographics, tumor type and grade, prior treatments, number of progressions, Karnofsky Performance Status (KPS), treatment schedule, number of doses of the treatment drugs, time-to-progression, OS rate and toxicity.
All patients selected for the study were treated with a combination of bevacizumab and carboplatin. Bevacizumab (Avastin®; Genetech, South San Francisco, CA, USA) was administered at a dose of 10 mg/kg every 14 days and carboplatin was dosed using AUC of 4–6 mg/ml/min, depending on the patient's prior treatment history and bone marrow reserves. One cycle consisted of 2 doses of carboplatin (every 28 days) and 3 doses of bevacizumab (every 14 days) and lasted 6 weeks. Radiographic assessment included review of MRI scans of all patients at multiple time points. T1-weighted post-contrast and T2-fluid attenuated inversion recovery (FLAIR) images were used for analysis. Responses were determined using modified McDonald/RANO criteria. Steroid dosing was recorded for all patients and taken into account during response assessment.
Results
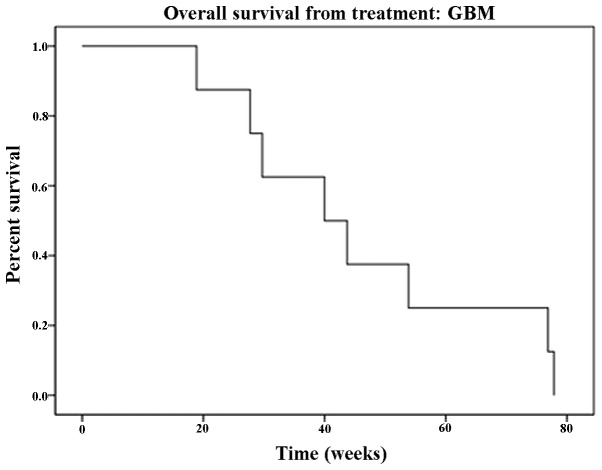
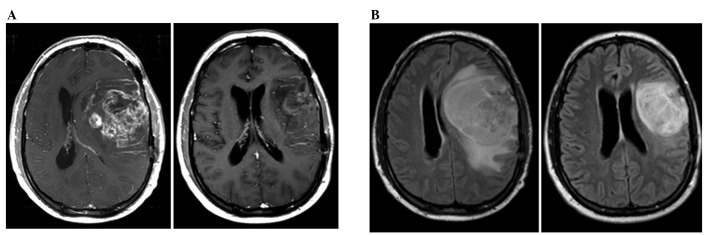
Of the 19 eligible patients, 58% were male and 42% were female. The median age at diagnosis was 53 years. Median KPS at the time of therapy initiation was 80. At the time of disease progression, the median KPS was 60. At initial diagnosis, 14 patients had GBM, two anaplastic oligodendroglioma (AO), one oligoastrocytoma (OA) and two were classified as high-grade glioma (HGG) at the time of recurrence. A total of 13 patients were treated at the time of the first progression and six at the time of the second progression. In total, 90 doses of carboplatin and 172 doses of bevacizumab were administered. The mean time-to-progression was 19 weeks (95% CI, 15.3–22.6) for the GBM cohort (median, 22 weeks) and 21.9 weeks (95% CI, 18.2–25.6) for the entire cohort (median, 22.2 weeks). Survival curves are depicted in Fig. 1. The median OS rate for GBM patients was 40 weeks (mean, 46.07 weeks; 95% CI, 30.7–61.3; Fig. 2). The calculated median OS from the time of initial diagnosis was 111 weeks (95% CI, 68.8–153.1) for GBM patients. At 6 months 40% of GBM patients were progression-free and 8 were alive at the time of data analysis; for the 7 deceased patients, the median survival was 43.7 weeks. Hematological toxicity was observed in 8 (42%) patients. More than half of the patients (58%) experienced grade I or II toxicity. Of the patients who experienced hematological toxicity, three patients (37.5%) experienced grade III neutropenia, four (50%) grade III lymphopenia and one (12.5%) grade III thrombocytopenia. Grade IV hematological toxicity was not observed. One patient (5.2%) suffered from brain hemorrhage and one patient developed meningoencephalitis following herpes zoster infection. At the time of evaluation, the response rate was 52.6% [complete response (CR) plus partial response (PR); n=10]. Of the patients, 21% (n=4) had stable disease (SD) and in 26.3% (n=5) the response could not be fully assessed due to inadequate scans, missing data or lack of measurable disease at the start of therapy (Table I). Progressive disease was not observed prior to completion of the first cycle of therapy. A response following 1 cycle of therapy was achieved by 66% of responding patients, 25% following 2 cycles and 8.3% following 3 cycles. The majority of patients who failed this therapy experienced confined, ipsilateral radiographic progression on T1 post-gadolinium and FLAIR images. A summary of the data is shown in Table I and an example of a radiographic response is shown in Fig. 3.
Figure 1.
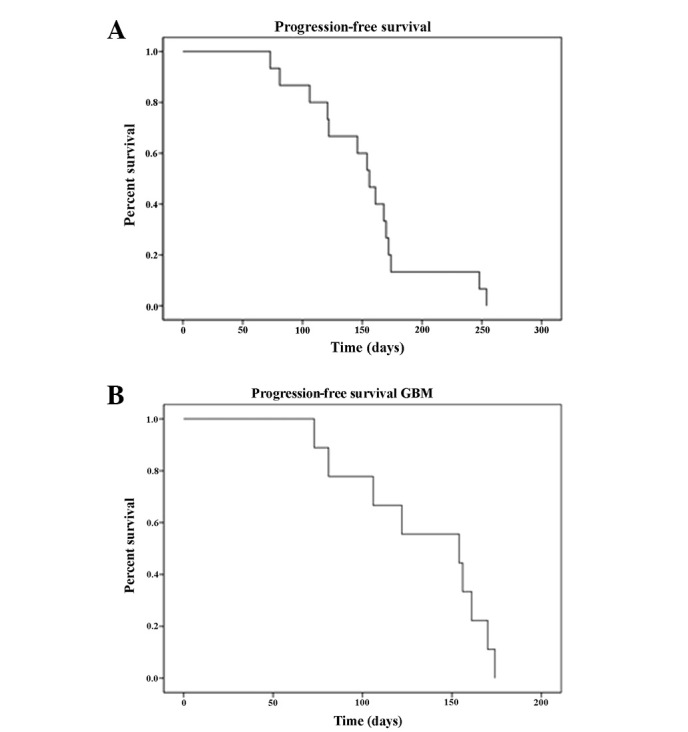
Kaplan-Meier analysis of PFS (A) for all patients in the study and (B) for GBM patients only. PFS, progression-free survival; GBM, glioblastoma.
Figure 2.
Kaplan-Meier analysis of OS for GBM patients in the study. Note median OS of 40 weeks. OS, overall survival. GBM, glioblastoma.
Table I.
Summary of selected characteristics of patients enrolled in this study.
| Subject number | Gender | Age at diagnosis (years) | Tumor type | KPS at initiation of therapy | No. of doses (carboplatin/bevacizumab) | Response |
|---|---|---|---|---|---|---|
| 1 | M | 41 | GBM | 80 | 10/20 | PR |
| 2 | F | 60 | GBM | 70 | 5/9 | PR |
| 3 | M | 47 | GBM | 100 | 3/7 | SD |
| 4 | M | 61 | GBM | 80 | 5/11 | CR |
| 5 | M | 27 | GBM | 70 | 4/11 | Possible PD |
| 6 | M | 67 | GBM | 60 | 2/3 | SD |
| 7 | F | 35 | HGG | 70 | 4/7 | Possible SD |
| 8 | M | 53 | GBM | 90 | 7/15 | PR |
| 9 | F | 22 | GBM | 90 | 8/15 | SD |
| 10 | F | 61 | GBM | 50 | 1/10 | Possible CR |
| 11 | M | 47 | GBM | 60 | 4/8 | PR |
| 12 | M | 64 | GBM | 80 | 5/6 | Possible SD |
| 13 | M | 74 | GBM | 70 | 3/1 | PR |
| 14 | F | 63 | AO | 80 | 7/14 | PR |
| 15 | M | 39 | OA | 70 | 5/10 | CR |
| 16 | F | 38 | HGG | 90 | 3/13 | Possible SD |
| 17 | F | 23 | AO | 80 | 5/12 | CR |
| 18 | F | 55 | GBM | 90 | 5/15 | PR |
| 19 | M | 58 | GBM | 50 | 5/UNK | SD |
M, male; F, female; GBM, glioblastoma; HGG, high-grade glioma; AO, anaplastic oligodendroglioma; OA, oligoastrocytoma; KPS, Karnofsky Performance Status; PR, partial response; CR, complete response; PD, progressive disease; SD, stable disease; UNK, unknown.
Figure 3.
Example of a radiographic response to the combination of bevacizumab and carboplatin following one cycle of therapy in a patient with recurrent GBM (subject number 1). (A) T1 post-gadolinium images and (B) FLAIR images are shown prior to (left) and following (right) therapy. Note the significant reduction of the mass effect indicating rapid onset of anti-edema effects of bevacizumab. Radiographic response was correlated with the marked improvement of the patient's neurological symptoms (aphasia and hemiparesis). FLAIR, fluid attenuated inversion recovery. GBM, glioblastoma.
Discussion
According to the studies published to date, there is no strong evidence suggesting that the addition of cytotoxic therapy to anti-VEGF agents translates into improved efficacy (20,21), although the vascular normalization theory offers an attractive mechanism supporting a combination approach utilizing an anti-VEGF agent with a traditional cytotoxic agent. The current retrospective series is the largest reported to date utilizing the combination of carboplatin with bevacizumab. The choice of agents for the treatment of recurrent malignant glioma at our institution was dictated by the available evidence, properties and pharmacokinetics of the agents and toxicity profile. It was revealed that carboplatin paired with bevacizumab offers a high response rate (52.6% in the present study) that compares favorably with the results of other published studies. The median OS for GBM patients in our study was 10 months and 40% of these patients were progression-free at 6 months. These results also compare favorably with published prospective data. While direct comparisons are not possible due to differences in study designs, numbers of patients, treatment regimens and tumor histologies, the reviewed data indicate that carboplatin with bevacizumab offers moderate activity, comparable or possibly superior to single-agent anti-VEGF therapies (Table II). To confirm this hypothesis, a prospective randomized study of this combination is required. Notably, the results of a recently published phase II study combining carboplatin with irinotecan and bevacizumab did not confirm the superiority of that particular combined approach over the single-agent bevacizumab (15).
Table II.
Summary of selected studies using bevacizumab alone or in combination with other chemotherapeutics for recurrent high-grade glioma.
| Regimen | No. patients | Median PFS (months) | Median OS (months) | Study design | Author (ref.) |
|---|---|---|---|---|---|
| Bev + carbo | 19 (all subjects) | 5.5 (all subjects) | 10 (GBM) | Retrospective | Present study |
| 14 (GBM) | 5.4 (GBM) | ||||
| 5 (HGG) | |||||
| Bev + carbo | 9 (all subjects) | 7.2 (GBM) | Not attained | Retrospective | Thompson et al (17) |
| 4 (GBM) | 4.2 (WHO gr. III) | ||||
| 5 (WHO gr. III) | |||||
| Bev + carbo + VP-16 | 6 (GBM) | 4.7 | 7.4 | Retrospective | Francesconi et al (16) |
| Bev + carbo + CPT-11 | 40 (GBM) | 5.9 | 8.3 | Prospective | Reardon et al (15) |
| Bev | 85 (GBM) | 4.2 | 9.2 | Prospective | Friedman et al (10) |
| Bev | 48 (GBM) | 4.0 | 7.8 | Prospective | Kreisl et al (11) |
PFS, progression-free survival; OS, overall survival. Bev, bevacizumab; carbo, carboplatin; VP-16, etoposide; CPT-11, irinotecan. HGG, high-grade glioma; GBM, glioblastoma.
In addition to the encouraging efficacy of the studied combination, a rapid response to therapy (66% of patients responded following only one cycle of therapy) and tolerable toxicity with no instances of grade IV hematological events was also observed. Patients maintained a good quality of life while receiving therapy. The combination was active at first and second recurrence in bevacizumab-naïve patients. The majority of the radiographic progressions observed were ipsilateral to the initial disease site and did not indicate the conversion of glioma into a more aggressive, diffuse phenotype that is occasionally described post anti-VEGF therapy (22).
In conclusion, acknowledging the limitations of the current study, we consider that the combination of carboplatin and bevacizumab is active and well-tolerated in recurrent HGG patients. Optimization of carboplatin dose intensity and schedule with regard to the administration of anti-VEGF agents (‘vascular normalization window’) may result in improved efficacy in future studies with this combination.
Acknowledgments
This manuscript is dedicated to the late Dr Alexander Spence, a co-author of this work and a dear colleague and friend. We would like to thank Dr Sandra Johnston for providing statistical assistance.
Abbreviations:
- GBM
glioblastoma
- VEGF
vascular endothelial growth factor
- PFS
progression-free survival
- OS
overall survival
- HGG
high-grade glioma
References
- 1.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 2.Fulton D, Urtasun R, Forsyth P. Phase II study of prolonged oral therapy with etoposide (VP16) for patients with recurrent malignant glioma. J Neurooncol. 1996;27:149–155. doi: 10.1007/BF00177478. [DOI] [PubMed] [Google Scholar]
- 3.Friedman HS, Petros WP, Friedman AH, Schaaf LJ, Kerby T, Lawyer J, Parry M, et al. Irinotecan therapy in adults with recurrent or progressive malignant glioma. J Clin Oncol. 1999;17:1516–1525. doi: 10.1200/JCO.1999.17.5.1516. [DOI] [PubMed] [Google Scholar]
- 4.Yung WK, Albright RE, Olson J, Fredericks R, Fink K, Prados MD, Brada M, et al. A phase II study of temozolomide vs. procarbazine in patients with glioblastoma multiforme at first relapse. Br J Cancer. 2000;83:588–593. doi: 10.1054/bjoc.2000.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warnick RE, Prados MD, Mack EE, Chandler KL, Doz F, Rabbitt JE, Malec MK. A phase II study of intravenous carboplatin for the treatment of recurrent gliomas. J Neurooncol. 1994;19:69–74. doi: 10.1007/BF01051050. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, Fei D, Vanderlaan M, Song A. Biological activity of bevacizumab, a humanized anti-VEGF antibody in vitro. Angiogenesis. 2004;7:335–345. doi: 10.1007/s10456-004-8272-2. [DOI] [PubMed] [Google Scholar]
- 7.Stark-Vance V. Bevacizumab and CPT-11 in the treatment of relapsed malignant glioma. Abstracts from the World Federation of Neuro-Oncology Second Quadrennial Meeting and the Sixth Meeting of the European Association for Neuro-Oncology. Neuro-Oncol. 2005;7 abstract 342. [Google Scholar]
- 8.Vredenburgh JJ, Desjardins A, Herndon JE, II, Marcello J, Reardon DA, Quinn JA, Rich JN, et al. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol. 2007;25:4722–4729. doi: 10.1200/JCO.2007.12.2440. [DOI] [PubMed] [Google Scholar]
- 9.Vredenburgh JJ, Desjardins A, Herndon JE, II, Dowell JM, Reardon DA, Quinn JA, Rich JN, et al. Phase II trial of bevacizumab and irinotecan in recurrent malignant glioma. Clin Cancer Res. 2007;13:1253–1259. doi: 10.1158/1078-0432.CCR-06-2309. [DOI] [PubMed] [Google Scholar]
- 10.Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2009;27:4733–4740. doi: 10.1200/JCO.2008.19.8721. [DOI] [PubMed] [Google Scholar]
- 11.Kreisl TN, Kim L, Moore K, Duic P, Royce C, Stroud I, Garren N, et al. Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol. 2009;27:740–745. doi: 10.1200/JCO.2008.16.3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reardon DA, Desjardins A, Vredenburgh JJ, Gururangan S, Sampson JH, Sathornsumetee S, McLendon RE, et al. Metronomic chemotherapy with daily, oral etoposide plus bevacizumab for recurrent malignant glioma: a phase II study. Br J Cancer. 2009;101:1986–1994. doi: 10.1038/sj.bjc.6605412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sathornsumetee S, Desjardins A, Vredenburgh JJ, McLendon RE, Marcello J, Herndon JE, Mathe A, et al. Phase II trial of bevacizumab and erlotinib in patients with recurrent malignant glioma. Neuro Oncol. 2010;12:1300–1310. doi: 10.1093/neuonc/noq099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desjardins A, Reardon DA, Coan A, Marcello J, Herndon JE, II, Bailey L, Peters KB, et al. Bevacizumab and daily temozolomide for recurrent glioblastoma. Cancer. 2012;118:1302–1312. doi: 10.1002/cncr.26381. [DOI] [PubMed] [Google Scholar]
- 15.Reardon DA, Desjardins A, Peters KB, Gururangan S, Sampson JH, McLendon RE, Herndon JE, II, et al. Phase II study of carboplatin, irinotecan and bevacizumab for bevacizumab naïve, recurrent glioblastoma. J Neurooncol. 2012;107:155–164. doi: 10.1007/s11060-011-0722-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Francesconi AB, Dupre S, Matos M, Martin D, Hughes BG, Wyld DK, Lickliter JD. Carboplatin and etoposide combined with bevacizumab for the treatment of recurrent glioblastoma multiforme. J Clin Neurosci. 2010;17:970–974. doi: 10.1016/j.jocn.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Thompson EM, Dosa E, Kraemer DF, Neuwelt EA. Treatment with bevacizumab plus carboplatin for recurrent malignant glioma. Neurosurgery. 2010;67:87–93. doi: 10.1227/01.NEU.0000370918.51053.BC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yung WK, Mechtler L, Gleason MJ. Intravenous carboplatin for recurrent malignant glioma: a phase II study. J Clin Oncol. 1991;9:860–864. doi: 10.1200/JCO.1991.9.5.860. [DOI] [PubMed] [Google Scholar]
- 19.Jeremic B, Grujicic D, Jevremovic S, Stanisavljevic B, Milojevic L, Djuric L, Mijatovic L. Carboplatin and etoposide chemotherapy regimen for recurrent malignant glioma: a phase II study. J Clin Oncol. 1992;10:1074–1077. doi: 10.1200/JCO.1992.10.7.1074. [DOI] [PubMed] [Google Scholar]
- 20.Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 21.Jain RK. Antiangiogenic therapy for cancer: current and emerging concepts. Oncology (Williston Park) 2005;19:7–16. [PubMed] [Google Scholar]
- 22.Norden AD, Young GS, Setayesh K, Muzikansky A, Klufas R, Ross GL, Ciampa AS, et al. Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology. 2008;70:779–787. doi: 10.1212/01.wnl.0000304121.57857.38. [DOI] [PubMed] [Google Scholar]