Abstract
Introduction
Efforts to prevent vertical transmission of HIV have gained momentum globally since the launch of the “Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive”, reflecting the growing consensus that we now have low-cost, efficacious interventions that promise to end vertical transmission of HIV. Uganda is one of the 22 focus countries in the global plan and one of the 10 countries with the highest need for prevention of vertical transmission globally. In the context of current shortfalls in the prevention of vertical HIV transmission, this paper presents the results of the Networks project, a community mobilisation model implemented by the International HIV/AIDS Alliance in Uganda, and draws out the theoretical foundations and promising community mobilization practices relevant to prevention of vertical transmission.
Methods
A retrospective review of the Network project's activities, documentation and evaluation was performed.
Results
The Networks project, through community mobilisation and greater involvement of people living with HIV, reached an estimated 1.3 million people with at least one health service. By clustering 750 groups of people living with HIV into larger coalitions, the project supported existing groups to amalgamate their collective strengths and skills in outreach, referral and literacy activities; and improved reach and coverage of HIV services through strengthened linkages with healthcare facilities. Our analysis of the Networks model shows that it could contribute to the prevention of vertical transmission of HIV as a replicable and sustainable community mobilisation approach. In particular, the Networks model increased the uptake of decentralized interventions for preventing vertical transmission through community referrals; promoted male involvement through peer sensitisation; and linked communities to advocacy channels for advancing maternal health and prevention of vertical HIV transmission.
Conclusions
By placing persons living with HIV at the centre, the Networks model offers a mechanism for strengthening community and male involvement in preventing vertical transmission of HIV. The role of communities and networks of people living with HIV in planning, service delivery and monitoring of national targets for prevention of vertical transmission should be further strengthened through greater community engagement in service delivery and advocacy and through the regular sharing of data between communities and health facilities.
Keywords: community mobilization, Uganda, Africa, vertical transmission, people living with HIV, Networks model, male involvement
Introduction
Consensus is emerging on the imperative to optimize biomedical interventions to prevent vertical transmission of HIV, focusing on and beyond drug regimens and diagnostics. This shift demands a rapid expansion of access to HIV services through strengthened, decentralized and integrated health systems; adopting more cost-effective, equitable and community-centred delivery of services; and addressing behavioural and structural barriers to effective HIV prevention, treatment and care [1–3].
In particular, the call for more effective strategies to prevent vertical transmission of HIV stems from the recognition that one in seven people who acquire HIV globally do so perinatally, accounting for almost 400,000 new cases of children acquiring HIV annually. Vertical transmission accounts for 90% of all HIV cases among children [3]. It is not surprising therefore that prevention of vertical transmission of HIV forms a core programmatic area in the investment framework to halt the HIV epidemic proposed by Schwartländer et al. [4].
In June 2011, the “Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive” was launched with a commitment to reduce new cases of HIV among children by 90% and to halve AIDS-related maternal deaths by 2015. The plan focuses on the 22 countries with the highest numbers of pregnant women living with HIV globally [3].
Uganda, one of the 22 focus countries in the global plan, has a generalized HIV epidemic, with an estimated HIV prevalence of 6.5%, antenatal HIV prevalence of 7.5% and HIV incidence of 1% among women of reproductive age (15 to 49 years) [5–8]. Within this generalized epidemic are pockets of particularly high HIV prevalence – for instance, of up to 28% in fishing communities – in which young sexually active women are bearing children [9]. Consequently, vertical transmission continues to be a major driver of the HIV epidemic in Uganda, accounting for 18% of incident HIV infections. In 2008, an estimated 82,000 HIV-positive women needed interventions to prevent vertical transmission and 22,000 newborns acquired HIV in Uganda [3,5,7,10].
The national AIDS programme has made progress in decentralizing services to prevent vertical transmission in Uganda. By June 2009, interventions to prevent vertical transmission were being provided in all districts and had been decentralized to 314 health centres at the sub-county level and 148 health centres at the parish level. At this time, 947 health facilities were offering services to prevent vertical transmission, representing 87% of hospitals, 93.2% of health centres at the county or parliamentary constituency level, 73.2% of sub-county health centres and 12.4% of parish health centres [11].
Despite this progress, serious challenges continue to undermine prevention of vertical HIV transmission in Uganda. In a 2006 demographic and health survey, 94% of women were found to utilize antenatal care (ANC) services at least once during pregnancy, but only 42% delivered at a health facility [8]. Access and utilization of ANC services by poor rural women, who often deliver outside of health facilities [12], was particularly low at 37% [8]. By 2009, 64% of all pregnant women were being tested for HIV but only 53% of those who tested HIV-positive and only 28% of HIV-exposed infants were receiving antiretroviral prophylaxis [10].
Studies conducted in predominantly rural settings in Wakiso, Mbarara and Kabarole districts in Uganda between 2008 and 2010 suggest that tackling vertical transmission of HIV requires addressing a combination of individual, community and societal barriers. These range from failure to disclose HIV status and lack of money for food and transport at the individual level [13,14] to HIV-related stigma, poor support from male partners and negative community reactions to exclusive breastfeeding at the community and societal level [12,13,15,16]. This is in addition to health systems-related barriers such as long distances and poor linkages between community and facility-based services, as well as sub-optimal provider-patient interactions [13,14] that exacerbate stigma and discrimination.
The Uganda Networks project
The Networks project was funded by USAID and implemented by the International HIV/AIDS Alliance between 2006 and 2009. It aimed to increase access to a comprehensive continuum of HIV services by transforming groups of people living with HIV from passive service recipients to active service providers and facilitators [17,18]. Project activities focussed on supporting 750 existing groups of people living with HIV to organize themselves into a network of 120 larger, sub-national clusters. This amalgamated the collective strengths and skills held by these networked groups in outreach and education activities and improved the reach and coverage of HIV and health services through referrals and strengthened linkages with healthcare providers, [17,19].
Implementation of the project began with the development of operational and monitoring systems from the grass-roots (parish) level to the sub-national level. This involved mobilising groups of people living with HIV to form larger networks and building the capacity of the networks through training, mentorship and the provision of small grants. These groups and selected “network support agents” (NSAs) then facilitated the implementation of a community-based education, referral and linkage system [17,19]. By the end of 2008, 750 groups of people living with HIV had been mobilized and 120 county networks had been established in 40 districts, with a membership of over 40,000.1
A key feature of the Networks project was the training of 1302 people to serve as NSAs. These community members were seconded to work alongside healthcare providers in 643 facilities [17,18]. NSAs were selected, trained and supervised based on criteria and a training curriculum designed to promote the involvement of people living with HIV, including men [14] (Table 1).
Table 1.
Selection criteria, supervision and training curriculum of the NSAs
| 1. Selection criteria for NSAs | |
| Gender | NSAs were selected as male-female pairs |
| Locality | Selected from any of the 40 districts covered by the project |
| HIV status | HIV-positive (self-declared) |
| ART status | On antiretroviral therapy for at least one year |
| 2. Training and supervision | |
| Training | Three weeks’ training on nutrition, HIV, tuberculosis, home-based care, pretest and adherence counselling, confidentiality, family planning, HIV-related gender-based violence, disclosure and discordance and safer infant feeding practice |
| Supervision | Supervised by health workers (nurses) in 643 designated facilities |
| 3. Remuneration and compensation | |
| Compensation | Reimbursement of expenses such as transport costs |
Abbreviations: ART, antiretroviral therapy; NSAs, network support agents.
NSAs supported people living with HIV and their families by making referrals, providing pretest and adherence counselling during home visits, tackling stigma through education and increasing client access to HIV and general health services. NSAs would, for example, physically accompany clients to health facilities and work alongside providers at designated facilities to assist with client orientation, pretest counselling and registration [17,18].
Through partnerships with external stakeholders,2 the Networks project facilitated 55 clusters of networked groups to engage in income generation, music and drama training and home care for vulnerable children. These clusters served as service delivery points for people living with HIV, facilitated focussed interventions for people affected by HIV and enabled the engagement of people living with HIV as coproviders of services. The Alliance provided organizational strengthening and technical support to these networked groups to improve their leadership, organizational management, HIV-literacy and referral skills [17,19].
Aims and objectives of this paper
The aim of this paper is to examine the contribution of the Networks model to the prevention of vertical transmission of HIV. Specifically, we explore the theoretical foundations of the model, describe its results and identify and discuss promising practices relevant to prevention of vertical transmission of HIV.
Methods
We employed a combination of retrospective reviews of the Networks’ activities and project documentation to develop a conceptual model for community mobilisation aimed at strengthening the translation of practice to policy [20].
Ethical issues
No new data were collected for this analysis. Secondary analysis of data was performed and triangulated with findings from an evaluation of the project [18] and a qualitative study of Ugandan networks of people living with HIV performed by Hodgson et al. [19] in accordance with ethical approval from the Uganda Virus Research Institute and the Uganda National Council for Science and Technology. No personally identifiable data were contained in the data analyzed in this study.
Results
Description of the model
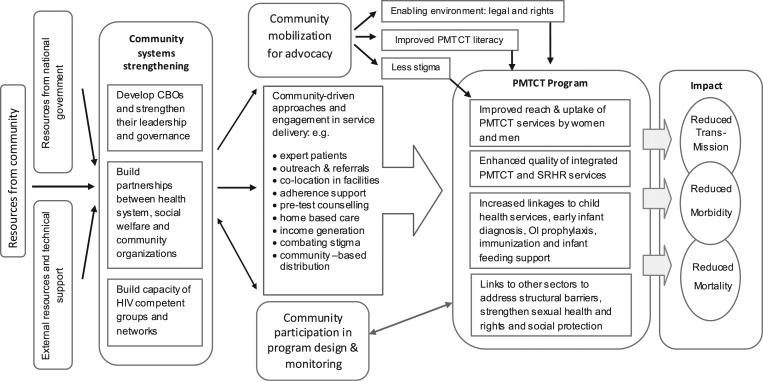
The Networks model pooled community, government and external resources to strengthen community systems to deliver and increase the reach, quality and linkages of HIV services. Inherent to this community mobilization process was an organizational capacity-building element, which supported groups of people living with HIV to function more effectively. This included training on organizational development and management, increasing their HIV literacy and fostering partnerships with other stakeholders.2 Groups of people living with HIV were provided with financial assistance (through mini-grants), equipment (such as motorbikes) and technical support (such as training), which transformed them into “AIDS-competent” groups, enabling them to “generate a sustainable local response to HIV” [21] (p.1662),22 (p.1557)] and collectively deliver services to their members. Groups of people living with HIV acted as service delivery points and linked their members with health facilities through NSAs. Of particular relevance to prevention of vertical HIV transmission was the NSAs’ outreach, onward referrals and accompaniment of clients to health facilities. These activities led to better uptake of services and linkages with other health services [17] (Figure 1).
Figure 1.
Conceptual framework of community mobilisation as applied to PMTCT programme area. It creates an enabling environment for community engagement in HIV service delivery through community systems strengthening, which in turn enables communities to engage in the planning, design and delivery of services to prevent vertical HIV transmission. This leads to improved reach, male involvement and linkages between prevention of vertical HIV transmission and other services, as well as to the desired long-term impacts of reduced HIV transmission, morbidity and mortality.
Theoretical foundations underlying the model
The Networks model has two fundamental foundations: community mobilisation and greater involvement of people living with HIV (GIPA).
Community engagement and mobilization
Judged by the established criteria of longevity, acceptance and continuum of community involvement [23,24], the project was founded on community engagement and encompassed varying degrees of community mobilisation, participation and empowerment. As in other models [21,22], community members, in this case NSAs, were mobilized to take up the role of service coproviders, transforming the paradigm of HIV service delivery from “for the community” to “by the community” [25] (p.i3)]. The model is based on the premise that community engagement and mobilisation creates community structural elements in ways that ultimately increase acceptance, ownership, capacity and sustainability. By recruiting local community members as NSAs, the project tapped community expertise and knowledge and strengthened linkages between facilities and the community. These linkages continued beyond the life of the project funding.
Greater involvement of people living with HIV and AIDS
While community engagement as coproviders of HIV services plays a significant role in the model, ownership of the model was equally strengthened by the fact that all NSAs were people living with HIV (Table 1). Their participation in the planning and implementation of the project enabled them to contribute while overcoming barriers to GIPA such as HIV stigma [19,26]. For instance, one NSA, quoted in Hodgson et al. [19(p.3)], asserts:
Disclosing my status, and going for training as an NSA has affected my life greatly. People are friendlier, and want me to counsel them. My life is now comfortable.
Impact on preventing vertical transmission of HIV
By the end of the implementation period, the Networks project had achieved a number of outcomes related to prevention of vertical transmission of HIV.
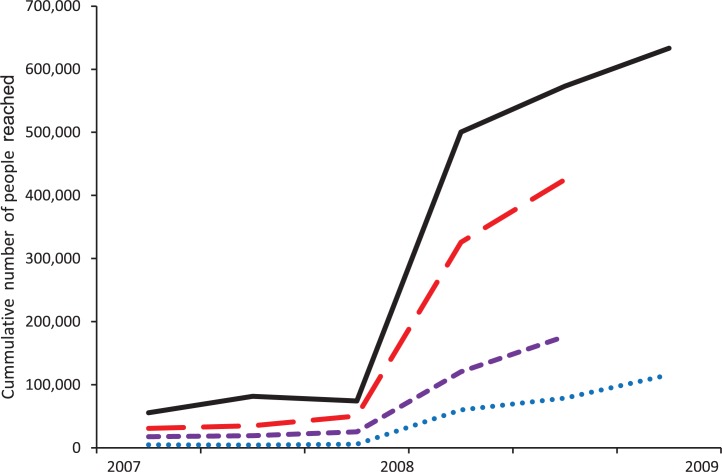
Increased uptake of decentralized services to prevent vertical transmission of HIV
Results of the evaluation showed that the project contributed to the realization of national targets relating to vertical HIV transmission, particularly in the mid-eastern districts, where the number of pregnant women provided with services to prevent vertical transmission of HIV increased from a baseline of 1264 at the start of the project in 2008 to 15,892 in 2009 [17]. These services included identifying pregnant women in the community, encouraging them to go for testing, accompanying them to get test results while observing confidentiality, reminding them of ANC appointments and providing antiretroviral adherence support. By creating a cadre of lay workers at the community level to deliver services, the model substantially strengthened the ability of community systems to reach rural and marginalized communities and increase service uptake (Figure 2).
Figure 2.
Cumulative services and referrals provided by groups of people living with HIV and NSAs between 2007 and 2009. The project reached 1.3 million people with at least one health service, including HIV education and awareness prevention (continuous black); antiretroviral literacy and education (long red dashes); antiretroviral adherence counselling and support (short purple dashes) and referrals for health facility and community-based services (blue dotted). Abbreviation: NSAs, network support agents.
Promoted a family-centred approach to preventing vertical transmission of HIV
The Networks project reached an estimated 1.3 million people with at least one health service (Figure 2).
NSAs reached households with pregnant mothers through home visits and used these visits as an entry point to assess the overall health needs of their children and male partners. As a result, 19,832 children were referred for additional services including nutrition, education and health. For instance, 2200 vulnerable children were registered for direct support including support for school fees. In addition, NSAs provided direct adherence support for antiretroviral and tuberculosis (TB) treatment and provided home-based and palliative care to approximately 70,000 people living with HIV. Finally, NSAs counselled male partners of pregnant women on the importance of antenatal clinic attendance and prevention of vertical HIV transmission [17] (Table 2).
Table 2.
Services provided to different household and community members
| Population | Services provided |
|---|---|
| Men and women | HIV pretest counselling |
| HIV education and literacy | |
| Referral for HIV testing | |
| Referral for antiretroviral therapy | |
| Adherence support for antiretroviral and TB drugs | |
| Counselling and referral for family planning | |
| Home-based and palliative care | |
| Pregnant women | Identification of pregnant women |
| HIV pretest counselling | |
| ANC appointment reminders | |
| ART adherence support for HIV-positive pregnant women | |
| Male partners of pregnant women | Peer sensitization on ANC and prevention of vertical transmission |
| HIV pretest counselling | |
| Referral for HIV testing | |
| Children | Screening and referrals for nutrition support |
| Direct support with school fees for vulnerable children |
Abbreviations: ANC, antenatal care; ART, antiretroviral therapy; TB, tuberculosis.
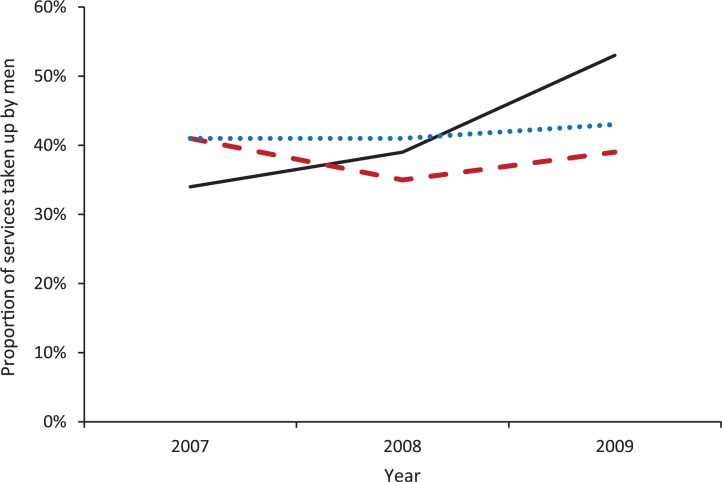
Promoted male involvement
Peer sensitisation was employed as a means of getting men to convince other men to take up services. The gender-balanced approach of selecting paired male and female NSAs increased male involvement in supporting improved outcomes for women and children and facilitated men's uptake of relevant services in the cascade of services required to prevent vertical transmission of HIV (Figure 3).
Figure 3.
Proportion of HIV pretest counselling (continuous black), referral for HIV testing (long red dashes) and referral for antiretroviral therapy (blue dotted) taken up by men.
Bridged the divide between the community and the health system
Observational studies in a variety of settings have documented barriers to uptake of HIV services occasioned by a lack of trust and confidence in healthcare workers, which results in poor interactions between clients and service providers [13]. In such contexts, lay and community health workers are seen as “a bridge between patients/community and the health system” [27] (p.185)], fostering the interactions, understanding and articulation of their communities’ needs. Hence, by virtue of their proximity to the community:
They [NSAs] managed to convince the communities that HIV/AIDS is real and the people believe them, in a way they never believed the health workers. They [NSAs] … helped to bridge the gap between the health care system and the community; people are more comfortable coming to the clinics since they know they will be finding their peers at the facility who will show them around. [18 (p.5)].
Linked communities to district- and national-level advocacy for preventing vertical transmission of HIV
Through a follow-on project funded by the Department for International Development (DFID), groups of people living with HIV and NSAs continued to advocate for better access to maternal and other services to prevent vertical transmission of HIV [28]. The initiative involved gathering data on the availability of and access to maternal and child health services for preventing vertical transmission. These data served as the basis for advocacy around maternal health and prevention of vertical transmission of HIV in district and national consultative forums known as partnership platforms. The partnership platform is a coalition of organizations promoting access to maternal, neonatal and child health services for preventing vertical transmission of HIV [28]. The appeal for NSAs and people living with HIV to engage in advocacy emanates from, among other factors, their emerging role as “expert patients” [29] (p.21)] and their first-hand experience as users of HIV and health services. These forums have created an interface between national decision-makers and women living with HIV and their male partners and have initiated discussions about improving maternal and child health through strengthened health systems.
Discussion
Networks of people living with HIV are recognized as a key resource for enhancing support to those affected by HIV, ameliorating stigma [30] and exemplifying the GIPA principle [18,31] while at the same time empowering people living with HIV to act as service providers in their own right at the community level [19]. Our study highlights a number of promising practices from Ugandan networks of people living with HIV relevant to prevention of vertical transmission of HIV, particularly regarding community mobilisation for service delivery, community-led advocacy and male involvement.
Community mobilisation and involvement in service delivery
Prevention of vertical transmission of HIV is no longer solely dependent on the efficacy of antiretroviral regimens, but equally important, the reach and coverage of the “hard to reach” populations with existing interventions. As decentralization of interventions to prevent vertical transmission of HIV to the community level becomes increasingly necessary in order to reach marginalized women and their partners [32], innovative and participatory community mobilisation approaches are indispensable.
Evidence from South Africa, India and Zimbabwe suggests that while most models of community mobilisation achieve relatively good success in building the capacity of rural and marginalized communities to deliver HIV care, they often differ markedly in their ability to create enabling environments for effective community responses. This includes their ability to identify and tackle preexisting community dynamics that facilitate or hinder HIV prevention, treatment and care [21,22]. At least in part, the collective ability of models with high representation from stigmatized groups such as sex workers and other people affected by HIV to confront stigma and acquire support from external partners appears to be a distinct strength [18,22].
In particular, networks of people living with HIV can mitigate some of the societal and economic barriers to prevention of vertical transmission of HIV in Uganda such as negative social attitudes towards exclusive breastfeeding [16], sub-optimal disclosure, probably resulting from a high level of HIV stigma and the cost of travelling long distances to health facilities [13,14]. This emanates from the ability of these networks to promote the participation of their members in provision of HIV services openly at the community level and, in doing so, to challenge stigma and promote disclosure [18,19]. Networks of people living with HIV offer particular strengths in outreach by creating a “network of support services in the community” [33] (p.S20)]. As Bärnighausen et al. [34] argue, optimal decentralization requires provision of HIV services within community premises.
High rates of loss to follow-up often result from incremental losses along the cascade of interventions for preventing vertical transmission of HIV, from antenatal attendance, prenatal HIV testing and antiretroviral therapy (ART) uptake and delivery in health facilities to infant testing, prophylaxis and feeding [35]. In Uganda, this has particular relevance as the absence of active tracking and referral mechanisms for pregnant mothers often leads to low facility-based delivery rates and low coverage of interventions to prevent vertical transmission of HIV [8,10,12]. Our study suggests that networks of people living with HIV can mitigate some of these challenges through active community-level identification, counselling and support to pregnant women to access health facilities through appointment reminders and accompaniment.
Community advocacy for increased access to services
Mobilising communities to demand, plan, deliver and evaluate efforts to prevent vertical transmission of HIV, as envisioned in the treatment 2.0 framework [1], requires strengthening community systems and social accountability tools to ensure that the coverage and quality of HIV services meets community expectations. Our study suggests that gathering community-level data could potentially strengthen monitoring of national targets for maternal health and prevention of vertical transmission of HIV, particularly targets related to quality, budgetary allocations, coverage and equitable access.
Male involvement through a family-centred approach
Male involvement – which has a positive influence on the uptake of interventions to prevent vertical transmission of HIV [36,37] – should be encouraged through peer sensitization and other innovative approaches that surmount the inability of women to convince their partners to participate in preventing vertical transmission [38], while mitigating the risks of HIV-related intimate-partner violence and abandonment [39]. In the Networks model, male participation was increased through the selection of gender-balanced NSA pairs, which facilitated men-to-men peer education and referrals in a setting where male participation in preventing vertical transmission of HIV has been low [40]. In addition, the model supported vulnerable women to access support and mitigate negative consequences related to HIV diagnosis and disclosure. This was primarily accomplished through NSAs, who were trained on the importance of male involvement and the impact of gender on HIV prevention. The training focussed on the risk of intimate-partner violence associated with HIV testing, disclosure and discordance, as well as the impact of a violent environment on women's ability to negotiate safer sexual practices; access antenatal care; continue taking antiretroviral treatment; and utilize safer infant feeding options.
Sustainability
Our analysis suggests that the integration of grant-making processes transformed the Networks model from a closed-ended into an almost self-perpetuating project, while at the same time building the capacity of groups of people living with HIV to manage finances. As highlighted by Hodgson et al. [19], networks provide people living with HIV with opportunities to take up specific roles in the community including income generation. For example, 58 groups of people living with HIV applied for and received grants for income-generating activities, which were used to support prevention outreach in schools and care for vulnerable children [17,19]. Being recipients and facilitators of health services strengthened the sense of ownership of the project among people living with HIV and bolstered their visibility, legitimacy and recognition [19]. This motivated groups of people living with HIV to continue providing some services even after the funding ended, which is particularly relevant in the current context of increased task-shifting and community engagement in HIV service delivery [1]. Despite these achievements, long-term sustainability based on volunteerism is threatened by high turnover and attrition [41,42]. Integration of community-based initiatives into wider health systems and increased ownership of such initiatives among other community members in addition to people living with HIV is required for greater sustainability.
Replicability
While sustainability remains a concern, the relative success of the Networks project in Uganda has led to the model being replicated within a USAID-funded BRIDGE II project3 in Chiradzulu, Malawi. Implementation of the model in Malawi – which started in July 2010 and is still ongoing – demanded a nuanced understanding of the local context, including decentralization policy, epidemiology, service gaps and barriers to services. For example, the model is being used to fill gaps in the existing referral system by supplementing paper-based referral mechanism with one-on-one referrals. NSAs, termed Community Referral Agents in the Malawi project, are equipped with a comprehensive directory of both statutory and non-statutory HIV services available in each district, which allows them to map and link people living with HIV as well as other community members to services closest to them. This is particularly relevant in settings where long distances to health facilities [13,14] and “unavailability of services at health facilities” (Glory Mkandawire, Chief of Party, BRIDGE II, Malawi, personal communication) can discourage uptake of antenatal and other services to prevent vertical transmission of HIV.
Limitations of this study
Incomplete programme data limited our analysis of cost-effectiveness, uptake of infant prophylaxis and other outcomes related to prevention of vertical transmission. For example, data related to some activities from the fourth quarter of 2008 was missing due to the redesign of the monitoring indicators [17]. In addition, data regarding the uptake of ART by HIV-positive mothers and their HIV-exposed infants, as well as their retention in care was not routinely collected. This suggests weak mechanisms for the sharing of data between the networks and health facilities once mothers were enrolled in ANC and in vertical HIV prevention programs. Similarly, our analysis regarding Networks project costs and cost-effectiveness was limited because unit-cost data were not included in the project design.
Conclusions
Networks of people living with HIV can serve as an effective mechanism for mobilising communities to prevent vertical transmission of HIV. Networks can potentially increase coverage of services; challenge inequities in service delivery; reduce missed opportunities by reaching the poorest and the most marginalized community members whom health systems are unable to reach; and encourage male participation. The Networks model can empower people living with HIV to deliver and advocate for their communities’ needs. Inclusion of livelihood activities may strengthen sustainability.
Refocussing efforts on and beyond diagnostic, therapeutic and clinical aspects of preventing vertical transmission of HIV to address individual behaviours, societal norms and other structural factors that drive vertical transmission of HIV (including stigma, low involvement of men, economic deprivation and inaccessible health systems) is a promising strategy. Investing in the community response by strengthening community systems to extend the healthcare workforce and address community-level service delivery gaps is warranted [1,4].
In particular, social accountability, as well as tools to monitor service availability and delivery, should be strengthened within community-centred models to ensure that community expectations are met regarding the quality and coverage of services to prevent vertical transmission. Regular sharing of data between community groups and health facilities should be encouraged once mothers are enrolled in ANC and in programs to prevent vertical HIV transmission.
Finally, in light of the central role of community mobilisation in prevention of vertical HIV transmission and in other HIV programmatic areas, an evidence-informed articulation of the components and costs of community mobilisation is needed in order to support the inclusion of appropriately costed community efforts within HIV programmes.
Acknowledgements
We are grateful to all participants in the Networks project, including NSAs, other people living with HIV and partners including the Uganda Ministry of Health, Uganda AIDS Commission, Tuberculosis Control Assistance Program, NU-LIFE and the AIDS Support Organization. We thank Beatrice Mutali, Siobhan O'Dowd, Anja Teltschik, Farai Matsika, Kelly Safreed-Harmon and Janet Seeley for comments on earlier drafts of the paper, as well as Glory Mkandawire for information and permission to refer to the Malawi BRIDGE II Project.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KI conceptualized the study and reviewed drafts. DG-M drafted the paper and revised drafts based on comments. FM provided data and comments on the manuscript. All authors read and approved the final manuscript.
Abbreviations
ANC, antenatal care; ART, antiretroviral therapy; NSAs, network support agents; TB, tuberculosis.
Funding sources
The Networks project was funded by USAID under cooperative agreement 617-A-00-06-00008-00.
Notes
1. On average, eight groups of people living with HIV formed a cluster, although the number ranged from as few as six to as many as twenty-three. One lead or liaison group with stronger capacity was identified and its capacity strengthened through training and small grants. Each lead group, in turn, was responsible for building the capacity of the other groups in its cluster. Groups of people living with HIV acted as community service delivery points for a range of HIV services.
2. Partners included the Uganda Ministry of Health and the Uganda AIDS Commission (which allowed NSAs to be co-located in health facilities); NU-LIFE, a technical assistance programme supporting improved health and nutrition outcomes for people living with HIV (which trained NSAs on nutrition); The AIDS Support Organization, a Ugandan HIV services organization (which supported some groups of people living with HIV before implementation of the Networks project); and TB CAP, a USAID-funded programme supporting TB control between 2007 and 2010 (which supported TB case finding among people living with HIV in the Networks project).
3. BRIDGE II is a USAID-funded project led by the Johns Hopkins University Bloomberg School of Public Health Centre for Communication Program, and in which the Alliance is a partner.
References
- 1.WHO. Geneva: WHO; 2011. The treatment 2.0 framework for action: catalysing the next phase of treatment, care and support. [cited 2012 Mar 20]. Available from: http://whqlibdoc.who.int/publications/2011/9789241501934_eng.pdf. [Google Scholar]
- 2.WHO. Geneva: WHO; 2011. Global HIV/AIDS response. Epidemic update and health sector progress towards Universal Access Progress report 2011. [cited 2012 Mar 20]. Available from: http://www.who.int/HIV/pub/progress_report2011/HIV_full_report_2011.pdf. [Google Scholar]
- 3.UNAIDS. Geneva: UNAIDS; 2011. Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive 2011–2015. [cited 2011 Nov 12]. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20110609_JC2137_Global-Plan-Elimination-HIV-Children_en.pdf. [Google Scholar]
- 4.Schwartländer B, Stover J, Hallett T, Atun R, Avila C, Gouws E, et al. Investment Framework Study Group. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377(9782):2031–41. doi: 10.1016/S0140-6736(11)60702-2. [DOI] [PubMed] [Google Scholar]
- 5.UNAIDS. Geneva: UNAIDS; 2010. Report on the global AIDS epidemic 2010. http://www.unaids.org/documents/20101123_GlobalReport_em.pdf. [Google Scholar]
- 6.Musinguzi J, Kirungi W, Opio A, Montana L, Mishra V, Madraa E, et al. Comparison of HIV prevalence estimates from sentinel surveillance and a national population-based survey in Uganda, 2005–2006. J Acquir Immune Defic Syndr. 2009;51(1):78–84. doi: 10.1097/QAI.0b013e3181990713. [DOI] [PubMed] [Google Scholar]
- 7.Kampala, Uganda: Ministry of Health/Macro International; 2006. MOH/ORC. Uganda HIV/AIDS sero-behavioral survey 2004–2005. [Google Scholar]
- 8.Uganda Bureau of Statistics. Kampala: Uganda Bureau of Statistics; 2006. Demographic and health Survey. Preliminary report. [Google Scholar]
- 9.Asiki G, Mpendo J, Abaasa A, Agaba C, Nanvubya A, Nielsen L, et al. HIV and syphilis prevalence and associated risk factors among fishing communities of Lake Victoria, Uganda. Sex Transm Infect. 2011;87(6):511–5. doi: 10.1136/sti.2010.046805. [DOI] [PubMed] [Google Scholar]
- 10.WHO. Geneva: WHO; 2010. PMTCT strategic vision. [cited 2011 Dec 12]. Available from: http://www.who.int/HIV/pub/mtct/strategic_vision.pdf. [Google Scholar]
- 11.Uganda AIDS Commission. Status of HIV & AIDS prevention, care and treatment in Uganda. 2011. [cited 2012 Mar 20]. Available from: http://www.aidsuganda.org/documents/StatusoftheNationalHIVinUganda.pdf.
- 12.Bajunirwe F, Muzoora M. Barriers to the implementation of programs for the prevention of mother-to-child transmission of HIV: a cross-sectional survey in rural and urban Uganda. AIDS Res Ther. 2005;2:10. doi: 10.1186/1742-6405-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duff P, Kipp W, Wild TC, Rubaale T, Okech-Ojony J. Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda. J Int AIDS Soc. 2010;13:37. doi: 10.1186/1758-2652-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mbonye AK, Hansen KS, Wamono F, Magnussen P. Barriers to prevention of mother-to-child transmission of HIV services in Uganda. J Biosoc Sci. 2010;42(2):271–83. doi: 10.1017/S002193200999040X. [DOI] [PubMed] [Google Scholar]
- 15.Dahl V, Mellhammar L, Bajunirwe F, Björkman P. Acceptance of HIV testing among women attending antenatal care in south-western Uganda: risk factors and reasons for test refusal. AIDS Care. 2008;20:746–52. doi: 10.1080/09540120701693990. [DOI] [PubMed] [Google Scholar]
- 16.Matovu A, Kirunda B, Rugamba-Kabagambe G, Tumwesigye NM, Nuwaha F. Factors influencing adherence to exclusive breast feeding among HIV positive mothers in Kabarole district, Uganda. East Afr Med J. 2008;85(4):162–70. doi: 10.4314/eamj.v85i4.9640. [DOI] [PubMed] [Google Scholar]
- 17.International HIV AIDS Alliance. Hove: International HIV AIDS Alliance; 2009. Expanding the role of people living with HIV/AIDS in Uganda: the Networks Project 2006–2009. [cited 2011 Nov 12]. Available from: http://www.aidsalliance.org/includes/Publication/Networks_project_Uganda.pdf. [Google Scholar]
- 18.Kim YM, Kalibala S, Neema S, Lukwago J, Weiss DC. Meaningful involvement of people living with HIV/AIDS in Uganda through linkages between network groups and health facilities: an evaluation study. Psychol Health Med. 2012;17(2):213–22. doi: 10.1080/13548506.2011.592844. [DOI] [PubMed] [Google Scholar]
- 19.Hodgson I, Nakiyemba A, Seeley J, Bitira D, Gitau-Mburu D. Only connect – the role of PLHIV group networks in increasing the effectiveness of Ugandan HIV services. AIDS Care. 2012 doi: 10.1080/09540121.2012.656568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parkhurst J, Weller I, Kemp J. Getting research into policy, or out of practice, in HIV? Lancet. 2010;375(9724):1414–5. doi: 10.1016/S0140-6736(10)60585-5. [DOI] [PubMed] [Google Scholar]
- 21.Nhamo M, Campbell C, Gregson S. Obstacles to local-level AIDS competence in rural Zimbabwe: putting HIV prevention in context. AIDS Care. 2010;22(Suppl 2):1662–9. doi: 10.1080/09540121.2010.521544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell C, Cornish F. Towards a “fourth generation” of approaches to HIV/AIDS management: creating contexts for effective community mobilisation. AIDS Care. 2010;22(Suppl 2):1569–79. doi: 10.1080/09540121.2010.525812. [DOI] [PubMed] [Google Scholar]
- 23.Nakibinge S, Maher D, Katende J, Kamali A, Grosskurth H, Seeley J. Community engagement in health research: two decades of experience from a research project on HIV in rural Uganda. Trop Med Int Health. 2009;14(2):190–5. doi: 10.1111/j.1365-3156.2008.02207.x. [DOI] [PubMed] [Google Scholar]
- 24.Person B, Cotton D. A model of community mobilization for the prevention of HIV in women and infants. Prevention of HIV in Women and Infants Demonstration Projects. Public Health Rep. 1996;111(Suppl 1):89–98. [PMC free article] [PubMed] [Google Scholar]
- 25.Sarkar S. Community engagement in HIV prevention in Asia: going from ‘for the community’ to ‘by the community’ – must we wait for more evidence? Sex Transm Infect. 2010;86(1):2–3. doi: 10.1136/sti.2009.039289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Travers R, Wilson MG, Flicker S, Guta A, Bereket T, McKay C, et al. The greater involvement of people living with AIDS principle: theory versus practice in Ontario's HIV/AIDS community-based research sector. AIDS Care. 2008;20(6):615–24. doi: 10.1080/09540120701661690. [DOI] [PubMed] [Google Scholar]
- 27.Schneider H, Hlophe H, Van Rensburg D. Community health workers and the response to HIV/AIDS in South Africa: tensions and prospects. Health Policy Plan. 2008;23(3):179–87. doi: 10.1093/heapol/czn006. [DOI] [PubMed] [Google Scholar]
- 28.International HIV AIDS Alliance and Pamoja Consulting. Hove: International HIV AIDS Alliance; 2011. HIV related maternal mortality programme. End of program evaluation report. Kenya Country Report. [Google Scholar]
- 29.Kielmann K, Cataldo F. Tracking the rise of the “expert patient” in evolving paradigms of HIV care. AIDS Care. 2010;22(Suppl 1):21–8. doi: 10.1080/09540121003721000. [DOI] [PubMed] [Google Scholar]
- 30.Odhiambo D, Gatua E. Strengthening PLHIV networks for policy, advocacy and stigma reduction. Proceedings of the 17th International AIDS Conference; 2008. Aug 3–8, xico City. Abstract THAE0202. [Google Scholar]
- 31.UNAIDS. The greater involvement of people living with HIV. Geneva: UNAIDS; 2007. (GIPA): policy brief. [Google Scholar]
- 32.Perez F, Mukotekwa T, Miller A, Orne-Gliemann J, Glenshaw M, Chitsike I, et al. Implementing a rural programme of prevention of mother-to-child transmission of HIV in Zimbabwe: first 18 months of experience. Trop Med Int Health. 2004;9(7):774–83. doi: 10.1111/j.1365-3156.2004.01264.x. [DOI] [PubMed] [Google Scholar]
- 33.Rajabiun S, Mallinson RK, McCoy K, Coleman S, Drainoni ML, Rebholz C, et al. “Getting me back on track”: the role of outreach interventions in engaging and retaining people living with HIV/AIDS in medical care. AIDS Patient Care STDS. 2007;21(Suppl 1):S20–9. doi: 10.1089/apc.2007.9990. [DOI] [PubMed] [Google Scholar]
- 34.Bärnighausen T, Bloom DE, Humair S. Human resources for treating HIV/AIDS: needs, capacities and gaps. AIDS Patient Care STDS. 2007;21(11):799–812. doi: 10.1089/apc.2007.0193. [DOI] [PubMed] [Google Scholar]
- 35.UNICEF. New York: UNICEF; 2011. State of the World's Children. Statistical tables. [cited 2012 Mar 20]. Available from: http://www.unicef.org/sowc2011/pdfs/SOWC-2011-Statistical-tables_12082010.pdf. [Google Scholar]
- 36.Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37:1620–6. doi: 10.1097/00126334-200412150-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farquhar C, Mbori-Ngacha DA, Bosire RK, Nduati RW, Kreiss JK, John GC. Partner notification by HIV-1 seropositive pregnant women: association with infant feeding decisions. AIDS. 2001;15:815–7. doi: 10.1097/00002030-200104130-00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Larsson EC, Thorson A, Pariyo G, Conrad P, Arinaitwe M, Kemigisa M, et al. Opt-out HIV testing during antenatal care: experiences of pregnant women in rural Uganda. Health Policy Plan. 2012;27(1):69–75. doi: 10.1093/heapol/czr009. [DOI] [PubMed] [Google Scholar]
- 39.Auvinen J, Suominen T, Välimäki M. Male participation and prevention of human immunodeficiency virus (HIV) mother-to-child transmission in Africa. Psychol Health Med. 2010;15(3):288–313. doi: 10.1080/13548501003615290. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization Maximizing Positive Synergies Collaborative Group. Samb B, Evans T, Dybul M, Atun R, Moatti JP, Nishtar S. An assessment of interactions between global health initiatives and country health systems. Lancet. 2009;373(9681):2137–69. doi: 10.1016/S0140-6736(09)60919-3. [DOI] [PubMed] [Google Scholar]
- 41.Kironde S, Klaasen S. What motivates lay volunteers in high burden but resource-limited tuberculosis control programmes? Perceptions from the Northern Cape province, South Africa. Int J Tuberc Lung Dis. 2002;6(2):104–10. [PubMed] [Google Scholar]
- 42.Celletti F, Wright A, Palen J, Frehywot S, Markus A, Greenberg A, et al. Can the deployment of community health workers for the delivery of HIV services represent an effective and sustainable response to health workforce shortages? Results of a multicountry study. AIDS. 2010;24(Suppl 1):S45–57. doi: 10.1097/01.aids.0000366082.68321.d6. [DOI] [PubMed] [Google Scholar]