Abstract
Introduction
While biomedical innovations have made it possible to prevent the vertical transmission of HIV from mother to child, poor retention along the prevention of mother-to-child transmission (PMTCT) cascade continues to limit the impact of programmes, especially in low-resourced settings. In many of the regions with the highest burden of HIV and the greatest number of new paediatric cases, the uptake of facility-based care by pregnant women remains low. In such settings, the continuum of care for pregnant women and other women of reproductive age necessarily relies on the community. There is no recent review capturing effective, promising practices that are community-based and/or employ community-oriented groups to improve outcomes for the prevention of vertical transmission. This review summarizes those studies demonstrating that community-based and community-oriented interventions significantly influence retention and related outcomes along the PMTCT cascade.
Methods
Literature on retention within prevention of vertical transmission programmes available on PubMed, Psych Info and MEDLINE was searched and manuscripts reporting on key prevention of vertical transmission outcomes were identified. Short-listed studies that captured significant PMTCT outcome improvements resulting from community-based interventions or facility-based employment of community cohorts (e.g. lay counsellors, community volunteers, etc.) were selected for review.
Results
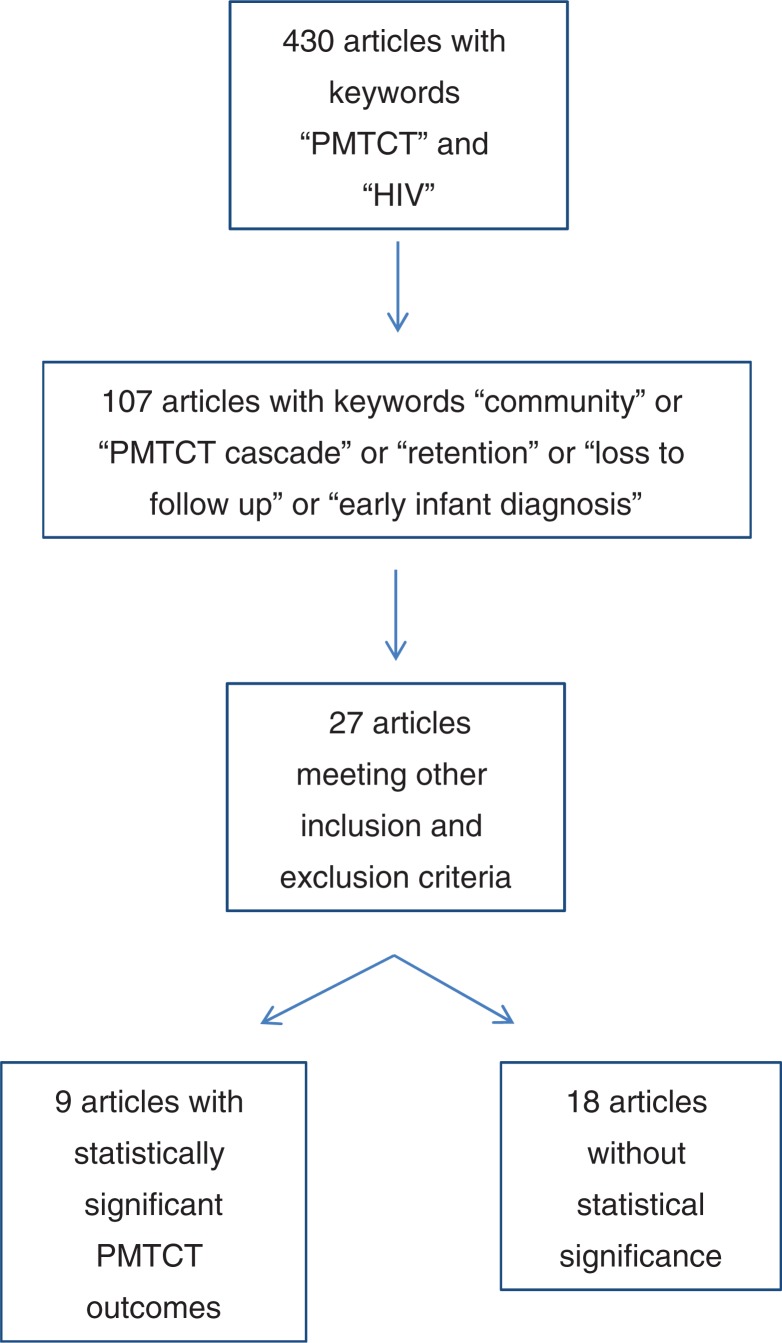
The initial search (using terms “HIV” and “PMTCT”) yielded 430 articles. These results were further narrowed using terminology relevant to community prevention of vertical transmission strategies addressing retention: “community,” “PMTCT cascade,” “retention,” “loss to follow up” and “early infant diagnosis.” Nine of these reported statistically significant improvements in key prevention of vertical transmission outcomes while meeting other review criteria. Short-listed articles reflect diverse study designs and a variety of effective interventions. Two interventions occurred exclusively in the community and four effectively employed community groups within facilities. The remaining three integrated community- and facility-based components. The outcomes of the included studies focus on knowledge (n=3) and retention along the PMTCT cascade (n=6).
Conclusions
This review captures an array of promising community-based and community-oriented interventions that demonstratively improve key prevention of vertical transmission outcomes. Though the strategies captured here show that such interventions work, the limited number of rigorous studies identified make it clear that expansion of community approaches and complementary reporting and related research are sorely needed.
Keywords: HIV, PMTCT cascade, vertical transmission, loss to follow-up, retention, community oriented, community-based
Introduction
While biomedical innovations and proven public health strategies have made it possible to almost completely prevent the vertical transmission of HIV from a mother to her child, approximately 2.5 million children under 15 are currently living with HIV, and about 1000 children newly acquire the virus on a daily basis [1,2]. The transmission of the virus from HIV-positive women to their babies can occur during pregnancy, at the time of delivery or through breastfeeding. Without intervention, vertical transmission occurs in up to 4 of every 10 deliveries among HIV-positive women [1]. Without treatment, approximately half of the children who have acquired HIV die before two years of age, and very few survive their school years [1].
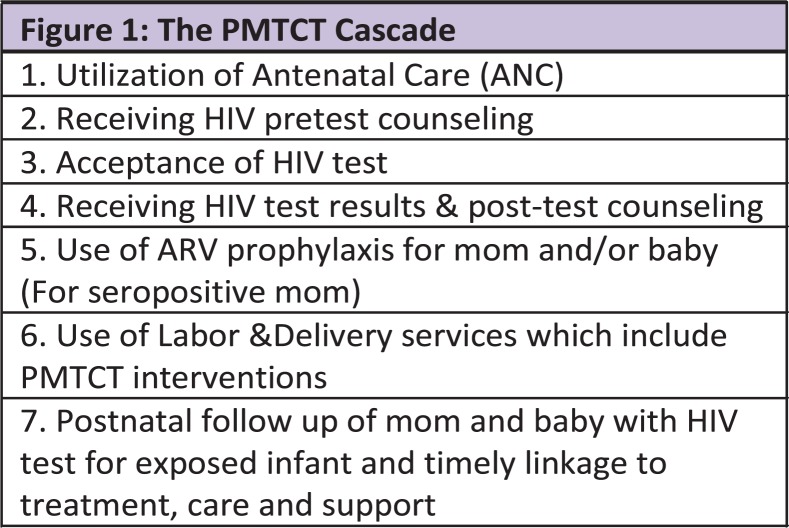
Preventing HIV amongst infants and young children involves a four pronged approach: primary prevention of HIV among women of reproductive age using health service delivery points and community structures; providing support and counselling to women living with HIV to empower them to make informed decisions about their reproductive life; ensuring that pregnant women living with HIV are tested and have access to treatment that will promote their health and prevent vertical transmission of HIV to their babies; and integrating HIV care, treatment and support for women living with HIV and their families [3]. The effectiveness of prevention of mother-to-child transmission (PMTCT) in low-resource settings is limited by poor retention along the continuum of care, often called the “PMTCT cascade” (Figure 1) [4]. This cascade refers to a stepwise process that a pregnant woman must navigate to prevent vertical transmission and ensure that, if her infant acquires HIV, the child receives appropriate HIV care and treatment. While antenatal care (ANC) serves as an entry point to identify HIV-positive pregnant women, dropout rates during the subsequent steps of the cascade can result in a failure to get needed treatment to mothers and prevent their infants from acquiring HIV [5].
Figure 1.
Outlines the steps of the prevention of mother-to-child transmission of HIV (PMTCT) cascade.
Cumulative losses in sub-Saharan Africa's prevention of vertical transmission programmes are very high. Many mothers deliver without ever attending ANC or having the opportunity for HIV testing. Up to 28% who enroll in ANC are lost prior to delivery, while 8 of every 10 are lost at six months postpartum [6–11]. This loss to follow-up (LTFU) occurs at many steps along the cascade, including when pregnant women do not return for test results between ANC and delivery; when pregnant women return for results and test positive but do not begin prophylaxis to prevent vertical transmission; and when the infant is not brought in for diagnosis and care postdelivery [12,13]. When postnatal care is sought, it is often only after infants living with HIV become severely ill. Appropriate access of healthcare is often limited by inadequate understanding of key elements of HIV and prevention of vertical transmission among expectant mothers as well as insufficient sensitization of health caregivers or providers of all levels.
In sub-Saharan Africa, where only 40% of pregnant women deliver in facilities and only 53% of women living with HIV receive any facility-based prevention of vertical transmission services [14,15], the continuum of care for pregnant women and other women of reproductive age necessarily relies on the community. Several factors influencing a woman's ability to successfully navigate the PMTCT cascade (i.e. social support, stigma, disclosure of status, partner support, etc.) cannot be adequately addressed by clinicians in healthcare settings alone and are arguably better addressed by personnel well-positioned to intervene at a community level [5,16]. In addition, transport between community and facility often imposes an immense and unaffordable expense (of both time and money) on pregnant mothers and other caregivers, making it difficult for mothers to continue using facility-based prevention of vertical transmission services. Access to healthcare services is further compounded by stigma, which makes it especially difficult for women to seek and receive the care they need for themselves and their babies. Often women face the added burden of travelling to areas where they will not be recognized so that they may anonymously use prevention of vertical transmission services.
Because many programmes that aim to prevent vertical transmission have historically relied on facilities, related interventions still primarily target facility-based care and focus on professional, medical staff such as doctors, nurses and clinical officers. As a result, the vast majority of published manuscripts reporting on successful prevention interventions describe facility-based interventions. There is no recent review capturing those effective, promising practices that are community-based or employ community-oriented groups to improve prevention of vertical transmission outcomes. This review identifies and summarizes those studies that report on effective interventions occurring in communities and/or employing community groups, with a particular focus on those achieving statistically significant improvements in retention and related outcomes along the PMTCT cascade.
Methods
Literature on strategies to improve retention of and services to mothers and babies within prevention of vertical transmission programmes available on PubMed, Psych Info and MEDLINE, dated between January 1990 and July 2011, were searched. McLeroy et al.'s typographies for the term “community-based” were used to set the inclusion criteria [17]. Interventions occurring in the community and demonstrating significant results were included. Given the limited number of published studies that captured significant prevention of vertical transmission outcome improvements but did not include facility-based components, interventions located in a facility that effectively engaged cohorts of lay community members (e.g. lay counsellors, community volunteers, etc.) as agents of change were also included. Studies within this latter category are referred to as “community-oriented” as opposed to “community-based.” All study designs except for review articles were eligible for inclusion. The review excluded manuscripts if they described prevention of vertical transmission interventions that were housed in a facility and did not employ a community cohort (e.g. lay counsellors, community volunteers). Though many screened articles discussed community-based and community-oriented prevention of vertical transmission activities and reported on related outcomes, studies without statistically significant findings were also excluded.
Studies were initially identified using the search terms “PMTCT” and “HIV.” These studies were narrowed using the following terminology relevant to community PMTCT strategies addressing retention: “community,” “PMTCT cascade,” “retention,” “loss to follow up” and “early infant diagnosis.” The studies identified by these specific terms were shortlisted and subsequently narrowed by two independent reviewers using the above criteria in order to minimize article selection bias. To help ensure the comprehensiveness of the final lists, bibliographies of the short-listed manuscripts were screened for additional, qualifying studies.
Results
The initial search (using terms HIV and PMTCT) yielded 430 articles. Using the above criteria, 27 articles were isolated from this group (Figure 2). Nine of the twenty-seven studies reported statistically significant improvements in PMTCT outcomes, with two occurring exclusively in the community and four effectively employing community groups within facilities. Of the nine studies, three had both community and facility components. Table 1 provides a summary of these nine studies meeting the above criteria, including study design, statistical significance of findings and study limitations. The remaining 18 of the 27 included applicable community-level data and/or made specific, community-focussed recommendations, but did not report statistically significant results.
Figure 2.
Schematic representation of the literature search and yield for articles discussing community strategies to address loss to follow-up along the PMTCT cascade. PMTCT, prevention of mother-to-child transmission of HIV.
Table 1.
Interventions with community component improving PMTCT outcomes
| Citation | Study design/model | Community component | Outcomes | Study limitations | |||
|---|---|---|---|---|---|---|---|
| Futterman et al. [18], South Africa | Pilot study of Mamekhaya programme, which combines mothers2mothers peer mentoring programme with culturally adapted CBI incorporating educational and psychosocial support | Pregnant women attending two maternities invited to participate. Intervention site: women received support from mentor mother and attended eight sessions of Mamekhaya CBI | Indicator | Control (n=31) | Intervention (n=41) | Significance | Relatively small sample size |
| Knowledge about HIV | Using 14-point scale at six months postdelivery: score went from 7.9 to 9.4 | Using 14-point scale at six months postdelivery: score went from 9.0 to 13.9 | p=0.001 | ||||
| Orne-Gliemann et al. [19], Zimbabwe | KAP survey in November 2002 and again in July 2004 to evaluate influence of prevention of vertical transmission advocacy and mobilization campaign on awareness and knowledge levels within community. Prevention of vertical transmission services introduced in mid-2001 in Buhera district but w/o community sensitization | Peer educators conducted core community mobilization activities. Influential community members consulted to assess their knowledge and inform them of as well as recruit them to share information on available PMTCT services | Indicator | KAP2002 | KAP2004 | Significance | Low and erroneous knowledge of importance of breastfeeding |
| Women had heard about MTCT | 73.1% | 92.3% | p=0.001 | ||||
| Proportion of women aware of the possibility to prevent vertical transmission of HIV | 48% | 82.8% | p=0.001 | ||||
| Awareness of risk of vertical transmission of HIV through breastfeeding | 22.5% | 59.5% | p=0.001 | ||||
| Systematic use of condoms at each sexual intercourse | 4.1% | 24.4% | p=0.001 | ||||
| Balogun and Odeyemi [20], Nigeria | Assessing knowledge and practices of 108 registered TBAs in Lagos. Cross-sectional survey | TBAs assist most deliveries in Nigeria. The assessment looked at how TBA knowledge affected the care they provided to their clients | Indicator | “Poor” level of knowledge | “Good” level of knowledge | Significance | No follow-up of mothers postreferral (did they make it to the site, etc.) |
| Counselling of clients exposed to HIV | 28 out of 63 (44.4%) | 6 out of 9 (66.7%) | p=0.042 | ||||
| Referral of clients for HIV testing | 41 out of 63 (65.1%) | 82 out of 108 (75.9%) | p=0.005 | ||||
| Teasdale and Besser [13], South Africa | Cross-sectional study: Independent evaluation of M2M conducted by Population Council's Horizons Programme in 2005 to 2006; KwaZulu-Natal, South Africa | M2M programme is designed to enhance prevention of vertical transmission services in facilities through mentor mothers who educate and support pregnant women and new mothers LWHIV | Indicator | No M2M | M2M | Significance | |
| Take NVP for prevention of vertical transmission | 83% | 93% | p<0.01 | ||||
| Give infants NVP for prevention of vertical transmission | 78% | 88% | p<0.05 | ||||
| Torpey et al. [21], Zambia | Zambia Prevention, Care, and Treatment Partnership project designed to build capacity in the healthcare system to allow for scale up of HIV services. In this phase, interventions were introduced to 38 prevention of vertical transmission sites and data collected monthly from July 2005 to September 2008 | Healthcare workers (HCWs) and lay providers conduct rapid HIV testing. Community motivators and lay counsellors trained to support and provide prevention of vertical transmission services. Traditional and religious leader engagement for community sensitization and to increase partner involvement | Indicator | Baseline | End of year 1 | Significance | |
| Pregnant women tested and receiving results | 4630 (45%) | 6758 (90%) | p<0.01 | ||||
| Seropositive pregnant women receiving complete course of ARV prophylaxis | 258 of 890 that tested positive (29%) | 701 of 1057 that tested positive (66%) | p<0.01 | ||||
| Faraquhar et al. [22], Kenya | Determining effect of partner involvement and couple's counselling on uptake of prevention of vertical transmission interventions | Partners were involved in counselling as key community members with potential to support follow-up and continuation | Strength of association | Advocates for no breastfeeding (reports this as a positive outcome). Does not address social stigma barriers that those who did not return with their partners may have faced | |||
| Strength of association: women whose partners came to clinic for voluntary counselling and testing approximately three times more likely to return for follow-up and report taking maternal or infant dose of NVP (OR = 3.4; 95% CI 1.3 to 9; p=0.009) | |||||||
| Chandisarewa et al. [24], Zimbabwe | Pilot study of provider initiated routine HIV counselling and testing | Community counsellor trained in routine HIV testing policy from June 2005 to November 2005. Key outcomes from first six months of routine testing compared with prior six month “opt-in” period | Indicator | Opt in | Opt out | Significance | No significance for sdNVP uptake by mother/infant pairs though number in opt out group is greater than number in opt in group |
| Women tested for HIV | 3058 out of 4872 (65.1%) | 4547 out of 4551 (99.9%) | p<0.001 | ||||
| Positive women posttest counselled and collecting results | 487 of 513 (95%) | 908 of 926 (98%) | p<0.001 | ||||
| # HIV positive women identified at ANC | 513 out of 3058 (16.8%) | 926 out of 4527 (20.4%) | p<0.001 | ||||
| Mother infant pair seen at six-week visit | 49 of 186 delivering at ANC (26.3%) | 105 of 256 delivering at ANC (41%) | p=0.002 | ||||
| Mother/infant pair receiving sdNVP | 185 (36%) | 256 (28%) | – | ||||
| Bekker et al. [25], South Africa | Prospective study comparing mortality, viral suppression and programme retention in three consecutive years of community-based ART clinic in Guguletu township | Community-based counsellor provided programme support. Counsellors provide ongoing counselling, psychosocial and support to continue full regimen of treatment, treatment readiness groups information sessions twice a week and home visits | Indicator | 2002/2003 | 2004/2005 | Significance | Captures statistical significance for all women of reproductive age but inadequately powered to demonstrate significance among pregnant women starting ART between year one and year three. Study does not specify which groups were LTFU though it discusses low rates of LTFU: 78 clients (7%) died, 33 (3%) LTFU |
| Women living with HIV starting ART | 114 | 479 | p=0.002 | ||||
| Kurewa et al. [6], Zimbabwe | Five-year follow-up of mother-child pairs in prevention of vertical transmission programme | Support groups, health education, trained counsellors from community responsible for follow-up after missed appointments | Indicator | HIV negative women | HIV positive women | Significance | Monitoring can be attributed to research institution. No comparison group (e.g. women living with HIV who did not receive the additional health education support) |
| LTFU in first year | 76 (13.4%) | 34 (7.3%) | p=0.012 | ||||
ANC, antenatal care; ART, antiretroviral therapy; CBI, cognitive behavioural intervention; KAP, knowledge attitude practice; LTFU, loss to follow-up; NVP, nevirapine; M2M, mothers2mothers; MTCT Plus, mother-to-child-transmission plus initiative; PMTCT, prevention of mother-to-child transmission of HIV; sdNVP, single dose nevirapine; TBAs, traditional birth attendants.
Of the nine articles meeting the criteria for this review, three focus on the outcome of knowledge on HIV and prevention of vertical transmission specifically [18–20]. These studies focus on “peer mentors” (as defined by the Mothers2Mothers (M2M) programme) [18], peer educators [19] and traditional birth attendants (TBAs) [20]. The intervention in these studies focuses on the dissemination of information about prevention of vertical transmission and demonstrates an improvement in mothers' knowledge of HIV [18], increased awareness of transmission risks, increased condom use at each sexual intercourse [19] and a greater appreciation for the importance of HIV testing [20].
The first of the three studies with knowledge-related outcomes was conducted by the Mamekhaya project in South Africa and provided cognitive behaviour interventions along with support to mothers living with HIV using the M2M model [18]. The pilot evaluation by Futterman et al. compared two clinics, one where the Mamekhaya intervention was applied and one where existing prevention of vertical transmission services were offered. M2M mentors were trained in support and cognitive behaviour interventions and conducted sessions with mothers living with HIV, with a curriculum including supportive mentorship, coping with stigma, avoiding negative emotions, infant feeding practices, partner disclosure, safe sex practices, family planning and pre- and postdelivery care for their infants. The pilot study revealed that the involvement of mentor mothers in education and support for HIV-positive women was associated with a higher HIV knowledge score six months postdelivery, with the intervention group scoring 3.3 points higher than the control group on a 14-point scale (p<0.001).
The second study reflected a key component of Zimbabwe's national initiative for prevention of vertical transmission, which incorporates education, advocacy and community mobilization campaigns. Orne-Gliemann et al. reported on a two-phase PMTCT advocacy and community mobilization programme in Buhera district [19], where the strategy included recruiting influential community members to sensitize others about prevention of vertical transmission followed by community mobilization by peer educators in discussion with community stakeholders. Surveys were given to women attending 10 health centres in the south Buhera district at baseline in 2002 and then again two years later. Results showed that women's awareness of the risk of vertical transmission from breastfeeding increased from 28.9% in 2002 to 55.3% in 2004 (OR, 4.1; CI, 2.9 to 5.9; p=0.001), while women's awareness that vertical transmission is preventable increased from 48.0% in 2002 to 82.8% in 2004 (OR, 4.9; CI, 3.3 to 7.3; p=0.001).
The third study that included knowledge as an outcome is a cross-sectional survey that demonstrated the relationship of prevention of vertical transmission knowledge and practice amongst TBAs in Nigeria [20]. Balogun and Odeyemi reported that, when 108 TBAs in Lagos were interviewed using a pretested questionnaire, TBA's prevention of vertical transmission knowledge levels, though low overall, correlated strongly with appropriate counselling and prevention of vertical transmission referrals, with 100% of those with “good” prevention of vertical transmission knowledge referring pregnant women to health facilities for HIV testing compared to 65.1% with “poor” knowledge. Using a Fisher exact test, the authors report a positive correlation between TBA knowledge levels and practice (p=0.042 and p=0.005 for counselling and referral, respectively).
The remaining six studies captured by this review reported on outcomes related to various steps along the PMTCT cascade (see Figure 1). In one cross-sectional study by Teasdale and Besser, the involvement of mentor mothers in the M2M programme in South Africa was associated with improved maternal uptake of treatment and higher rates of prophylaxis for infants. Specifically, facilities employing mothers from surrounding communities to provide education and support for HIV-positive pregnant women achieved significantly improved rates of maternal (93% vs. 83%; p<0.01) and infant (88% vs. 78%; p<0.05) nevirapine coverage compared to non-supported sites [13].
In another, Zambia-based study by Torpey et al., community engagement and sensitization by healthcare workers, lay counsellors and religious leaders focussed on partner involvement in the prevention of vertical transmission, with community leaders using community forums to specifically encourage males to attend ANC. The package of facility- and community-based interventions, of which male involvement and community mobilization was a significant component, resulted in a doubling of pregnant women being testing for HIV and receiving results (45% up to 90%; p<0.01). The intervention also led to a higher proportion of women completing ARV prophylaxis (29% at baseline up to 66% at one year; p<0.01) [21].
The next article focussed on other key community members – the partners of pregnant women. This Kenya-based study by Faraquhar et al. demonstrated a significant increase in prophylaxis to prevent vertical transmission as a result of partner engagement in either individual or couples counselling. A reported 2836 women enrolled in the study with 2231 returning to the clinic for a second study visit. Eighty-nine percent of this group of women reported inviting their partner to return with them for voluntary counselling and testing; 308 of these women's partners accompanied them to the clinic at their next counselling session and were also tested. Eighty-three percent of women whose partners attended couples counselling returned to access nevirapine, compared to 71% whose partners came for individual counselling and 56% of women whose partners did not come for voluntary counselling and testing (p=0.02) [22]. Eighty-eight percent of women whose partners attended couples counselling reported continuing their use of maternal nevirapine compared to 67% whose partners counselled individually and 45% whose partners did not participate in voluntary counselling and testing (p=0.006). Women whose partners came to clinic for testing and counselling also reported administering infant dose of nevirapine with higher frequency (OR, 3.4; 95% CI, 1.3 to 9; p=0.009) [22].
Kurewa et al. [6] reported on a five-year study in Zimbabwe that set up support groups in addition to employing trained counsellors from the same communities as the mothers receiving services. Mothers who missed appointments for prevention of vertical transmission received supportive visits from these counsellors at their homes, leading to LTFU rates of 7.3% among mothers living with HIV in the programme, compared to 13.4% among HIV negative mothers (p=0.012) [13]. The authors emphasize the significance of addressing a mother's needs through complete follow-up and care regardless of mother's HIV status. They attribute higher retention rates and higher rates of nevirapine uptake (in comparison to other studies) to the additional health education provided and the prolonged observation and follow-up of clients [23].
Chandisarewa et al. reported on a study in Zimbabwe that captured a significant effect of opt-out testing in a site supported by routine lay counsellor-led pretest counselling. In the study, “PMTCT counsellors” held 15-minute group education sessions with nearly 9500 pregnant women over a 12-month period, using a structured flip chart to guide discussion. The session focussed on HIV transmission, PMTCT prophylaxis and the importance of routine HIV testing for all pregnant women. In the context of such support, the shift from opt-in to opt-out testing at the clinic led to a substantial increase in the number of women tested (p<0.001), the number of women receiving test results (p<0.001), the number of women living with HIV identified in ANC (p<0.001) and the number of mother-infant pairs reporting for six-week postpartum follow-up (p<0.001) [24].
In a South African study reported by Bekker et al., the use of community-based counsellors and support groups was positively associated with initiation of women on treatment as well as a decrease in LTFU [25]. The number of women living with HIV who initiated antiretroviral therapy (ART) rose from 114 to 479 over the course of three years (p=0.002), capturing a strongly significant uptake in treatment services among women in a treatment programme with a dedicated community component. During the implementation of the programme, community-based “therapeutic counsellors” living in or near the selected community reinforced the continued use of services and addressed psychosocial issues, while holding treatment-readiness group information sessions twice weekly in a local community setting. The number of pregnancies occurring amongst the participants during the study period was not reported. However the cohort, largely composed of women of reproductive age, elegantly captured the impact of increasing counseling support on women's uptake of treatment services. In addition to increased uptake of services by women in particular, the second and third years of the study captured a higher median CD4 count (p<0.001), a lower mean viral load (p<0.001) and a lower proportion of AIDS diagnoses (p<0.001) among those on treatment.
As noted in the Methods section, in addition to the nine articles documenting statistically significant improvements in important prevention of vertical transmission-related outcomes, this review identified several papers without statistically significant outcomes that describe a variety of prevention of vertical transmission interventions involving community-level groups of caregivers and/or support units. These articles, which are not discussed in detail here, reported several community-level challenges (e.g. barriers to partner engagement [26,27], attitudes towards community care providers, stigma [4,16,28]) and included a variety of community units (e.g. community health workers [29], peer counsellors [30], volunteers [31–33], TBAs [34], traditional chiefs and religious leaders [35] and social workers [36]). Though these articles capture a broad spectrum of community agents and outcomes, the findings do not meet statistical significance.
Discussion
In many of the regions with the highest burden of HIV and the greatest number of new vertical transmissions, the uptake of facility-based care by pregnant women remains low, as does retention in such care. In these same areas, many of which have facility-based PMTCT uptake of well under 50% of women living with HIV, community engagement is also limited [14]. Programmes that do not extend beyond facilities and fail to engage lay staff will not be able to achieve the level of prevention of vertical transmission coverage required to approach zero new transmissions of HIV to children [14,15]. In addition, the women most at risk of acquiring HIV and most in need of treatment may be the least able to access services.
Community-based solutions are essential to ensuring women and their children have access to the full cascade of prevention of vertical transmission interventions. As literature on community-based prevention of vertical transmission strategies is limited, this review also includes what we call “community-oriented” prevention of vertical transmission strategies, where community-level units well-positioned to improve prevention of vertical transmission outcomes conduct activities that are housed in facilities. By including both of these categories of interventions, this review summarizes the limited, collective literature describing which community-based and community-oriented efforts have demonstrated statistically significant improvements in prevention of vertical transmission outcomes such as the retention of HIV positive pregnant women and their infants in care; HIV positive pregnant women continuing their treatment; mothers giving their HIV exposed infants prophylaxis and, ultimately, survival of both mother and child. Though this collective literature is unfortunately scarce, as summarized in the Results section above and in Table 1, activities captured here improve knowledge of prevention of vertical transmission, increase uptake of testing and prevention services and promote better rates of disclosure and retention.
The community groups involved in the achievement of these outcomes are diverse and include community health workers, peer counsellors, volunteers, TBAs, mentor mothers, traditional chiefs and religious leaders. However, unlike more specialized healthcare providers, these personnel are often readily available where the need is greatest and can be efficiently and effectively trained and recruited to implement prevention of vertical transmission interventions. Importantly, as studies included in the review show, these community groups can effectively engage mother-infant pairs and partners both at facilities and within the community at large. In fact, many of the study outcomes summarized in this review were achieved by integrating both community-based and facility-based community-oriented strategies [13,18,21,37].
Though this summary represents a careful search for published community-based and community-oriented prevention of vertical transmission strategies with significant improvements in outcomes, there are limitations to this review. One such limitation relates to the continuing evolution of strategies to prevent vertical transmission. Most notably, where a number of the included studies discussed single-dose nevirapine coverage as an outcome, it is now recognized that such prophylaxis is far inferior to multidrug prophylaxis, especially highly active ART. It is possible that the uptake of multidrug regimens and the implementation of other more progressive components of the latest international normative guidance on prevention of vertical transmission are more difficult to achieve than the outcomes captured in studies included here. Secondly, given the small evidence base supporting community-based and community-oriented prevention of vertical transmission strategies and our omission of a broad spectrum of more descriptive articles, the groups, outcomes and study methodologies among the articles included are admittedly varied. In short, the depth and breadth of this review is clearly limited by the shortage of robust literature on this topic. However, this is also one of the review's more important take-home messages.
Conclusions
The studies included here cover several proven, community-based and community-oriented strategies that improve retention along the PMTCT cascade and other key prevention of vertical transmission-related outcomes. These strategies make it clear that community interventions can and do work. However, this review clearly demonstrates that community-level activities as well as those conducted by community-oriented health caregivers reaching out from facilities continue to receive less attention than interventions by professional providers based in healthcare facilities. As a result, key community-level and community-oriented strategies for optimal prevention of vertical transmission uptake and retention remain inadequately discussed and understood, resulting in lost opportunities to protect mothers and babies from acquiring HIV. Rigorous measurement and evaluation of ongoing interventions with community components are essential, as is the subsequent sharing of promising practices through peer-reviewed literature. Such rigor will do much to ensure that community-based prevention of vertical transmission interventions live up to their promise in the years ahead.
Acknowledgments
The views and opinions expressed in the article are solely those of the authors and do not necessarily reflect those of the US Agency for International Development nor those of the US Government.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
BRP, GB and YM conceived the review. YM undertook research and screened articles relevant to production of the manuscript and drafted the manuscript. BRP and GB helped to conceive the study, undertook research relevant to production of the manuscript and drafted the manuscript in addition to editing and revising all parts. All authors read and approved the final manuscript.
Abbreviations
ANC, antenatal care; ART, antiretroviral therapy; CBI, cognitive behavioural intervention; KAP, knowledge attitude practice; LTFU, loss to follow-up; NVP, nevirapine; M2M, mothers2mothers; MTCT Plus, mother-to-child-transmission plus initiative; PMTCT, prevention of mother-to-child transmission of HIV; sdNVP, single dose nevirapine; TBAs, traditional birth attendants.
References
- 1.UNAIDS. Geneva: UNAIDS; 2010. Report on the Global AIDS Epidemic 2010. [Google Scholar]
- 2.Mofensen L. Prevention in neglected subpopulations: prevention of mother-to-child transmission of HIV infection. Clin Infect Dis. 2010;50(3):S130–48. doi: 10.1086/651484. [DOI] [PubMed] [Google Scholar]
- 3.UNICEF. New York: UNICEF; 2010. Preventing Mother-to-Child Transmission (PMTCT) of HIV factsheets on the status of national PMTCT responses in the most affected countries. [Google Scholar]
- 4.Towle M, Lende DH. Community approaches to preventing mother-to-child HIV transmission: perspectives from rural Lesotho. Afr J AIDS Res. 2008;7(2):219–28. doi: 10.2989/AJAR.2008.7.2.7.524. [DOI] [PubMed] [Google Scholar]
- 5.Theuring S, Mbezi P, Luvanda H, Jordan-Harder B, Kunz A, Harms G. Male involvement in PMTCT services in Mbeya region, Tanzania. AIDS Behav. 2009;13:S92–102. doi: 10.1007/s10461-009-9543-0. [DOI] [PubMed] [Google Scholar]
- 6.Kurewa EN, Kandawasvika GQ, Mhlanga F, Munjoma M, Mapingure MP, Chandiwana P, et al. Realities and challenges of a five year follow up of mother and child pairs on a PMTCT program in Zimbabwe. Open AIDS J. 2011;5:5–58. doi: 10.2174/1874613601105010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moth IA, Ayayo AB, Kaseje DO. Assessment of utilization of PMTCT services at Nyanza Provincial Hospital, Kenya. Sahara J. 2005;2(2):244–50. doi: 10.1080/17290376.2005.9724847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Painter Tm, Diaby KL, Matia DM, Lin LS, Sibailly TS, Kouassims MK, et al. Sociodemographic factors associated with participation by HIV-1-positive pregnant women in an intervention to prevent mother-to-child transmission of HIV in Cote d'Ivoire. Int J STD AIDS. 2005;16(3):237–42. doi: 10.1258/0956462053420158. [DOI] [PubMed] [Google Scholar]
- 9.Jones SA, Sherman GG, Varga CA. Exploring socio-economic conditions and poor follow-up rates of HIV-exposed infants in Johannesburg, South Africa. AIDS Care. 2005;17(4):466–70. doi: 10.1080/09540120412331319723. [DOI] [PubMed] [Google Scholar]
- 10.Stringer EM, Sinkala M, Stringer JS, Mzyece E, Makuka I, Goldenberg RL, et al. Prevention of mother-to-child transmission of HIV in Africa: successes and challenges in scaling-up a nevirapine-based program in Lusaka, Zambia. AIDS. 2003;17(9):1377–82. doi: 10.1097/01.aids.0000060395.18106.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stringer JS, Sinkala M, Goldenberg R, Vermund S, Acosta E. Monitoring nevirapine-based program for prevention of mother-to-child transmission of HIV-1. Lancet. 2003;362(9384):667. doi: 10.1016/S0140-6736(03)14172-4. [DOI] [PubMed] [Google Scholar]
- 12.Stringer EM, Chi BH, Chintu N, Creek TL, Ekouevi DK, Coetzee D, et al. Monitoring effectiveness of programs to prevent mother-to-child HIV transmission in lower-income countries. Bull World Health Organ. 2008;86:57–62. doi: 10.2471/BLT.07.043117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teasdale CA, Besser MJ. Enhancing PMTCT programs through psychosocial support and empowerment of women: the Mothers2Mothers model of care. S Afr J HIV Med. 2008;Summer:60–4. [Google Scholar]
- 14.UNICEF. New York: UNICEF; 2009. The State of the world's children 2009, maternal and newborn health: where we stand. [Google Scholar]
- 15.World Health Organization, Joint United Nations Program on HIV/AIDS and United Nations Children's Fund. Geneva: WHO; 2010. Towards universal access – scaling up priority HIV/AIDS interventions in the health sector: progress Report 2010. [Google Scholar]
- 16.O'Gorman DA, Nyirenda LJ, Theobald SJ. Prevention of mother-to-child transmission of HIV infection: views and perceptions about swallowing nevirapine in rural Lilongwe, Malawi. BMC Public Health. 2010;10:354. doi: 10.1186/1471-2458-10-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLeroy KR, Norton BL, Kegler MC, Burdine JN, Sumaya CV. Community-based interventions. Am J Public Health. 2003;93(4):529–33. doi: 10.2105/ajph.93.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Futterman D, Shea J, Besser M, Stafford S, Desmond K, Comulada WS, et al. Mamekhaya: a pilot study combining a cognitive-behavioral intervention and mentor mothers with PMTCT services in South Africa. AIDS Care. 2010;22(9):1093–100. doi: 10.1080/09540121003600352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orne-Gliemann J, Mukotekwa T, Perez F, Miller A, Sakarovitch C, Glenshaw M, et al. Improved knowledge and practices among end-users of mother-to-child transmission of HIV prevention services in rural Zimbabwe. Trop Med Int Health. 2006;11(3):341–9. doi: 10.1111/j.1365-3156.2006.01563.x. [DOI] [PubMed] [Google Scholar]
- 20.Balogun M, Odeyemi K. Knowledge and practice of prevention of mother-to-child transmission of HIV among traditional birth attendants in Lagos State, Nigeria. Pan Afr Med J. 2010;5:7. [PMC free article] [PubMed] [Google Scholar]
- 21.Torpey K, Kabaso M, Kasonde P, Dirks R, Bweupe M, Thompson C, et al. Increasing the uptake of prevention of mother-to-child transmission of HIV services in a resource-limited setting. BMC Health Serv Res. 2010;10:29. doi: 10.1186/1472-6963-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Faraquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37(5):1620–6. doi: 10.1097/00126334-200412150-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arrive E, Kyabayinze DJ, Marquis B, Tumwesigye N, Kieffer MP, Azondekon A, et al. Cohort profile: the pediatric antiretroviral treatment programs in lower-income countries (KIDS-ART-LINC) collaboration. Int J Epidemiol. 2008;37(3):474–80. doi: 10.1093/ije/dym216. [DOI] [PubMed] [Google Scholar]
- 24.Chandisarewa W, Stranix-Chibanda L, Chirapa E, Miller A, Simoyi M, Mahomva A, et al. Routine offer of antenatal HIV testing (“opt-out” approach) to prevent mother-to-child transmission of HIV in urban Zimbabwe. Bull World Health Organ. 2007;85:843–50. doi: 10.2471/BLT.06.035188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bekker L, Myer L, Orrell C, Lawn S, Wood R. Rapid scale-up of a community-based HIV treatment service: program performance over 3 consecutive years in Guguletu, South Africa. S Afr Med J. 2006;96:315–20. [PubMed] [Google Scholar]
- 26.Reece M, Hollub A, Nangami M, Lane K. Assessing male spousal engagement with prevention of mother-to-child transmission (pMTCT) programs in western Kenya. AIDS Care. 2010;22(6):743–50. doi: 10.1080/09540120903431330. [DOI] [PubMed] [Google Scholar]
- 27.Sarker M, Sanou A, Snow R, Ganame J, Gondos A. Determinants of HIV counseling and testing participation in a prevention of mother-to-child transmission program in rural Burkina Faso. Trop Med Int Health. 2007;12(12):1475–83. doi: 10.1111/j.1365-3156.2007.01956.x. [DOI] [PubMed] [Google Scholar]
- 28.Nassali M, Nakanjako D, Kyabayinze D, Beyeza J, Okoth A, Mutyaba T. Access to HIV/AIDS care for mothers and children in sub-Saharan Africa; adherence to the postnatal PMTCT program. AIDS Care. 2009;21(9):1124–31. doi: 10.1080/09540120802707467. [DOI] [PubMed] [Google Scholar]
- 29.Ivers LC, Jerome J, Cullen KA, Lambert W, Celletti F, Samb B. Task-shifting in HIV care: a case study of nurse-centered community-based care in rural Haiti. PLoS One. 2011;6(5):e19276. doi: 10.1371/journal.pone.0019276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shetty AK, Marangwanda C, Stanix-Chibanda L, Chandisarewa W, Chirapa E, Mahomva A, et al. The feasibility of preventing mother-to-child transmission of HIV using peer counselors in Zimbabwe. AIDS Res Ther. 2008;5:17. doi: 10.1186/1742-6405-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shetty AK, Mhazo M, Moyho S, Lieven A, Mateta P, Katzenstein DA, et al. The feasibility of voluntary counseling and HIV testing for pregnant women using community volunteers in Zimbabwe. Int J STD AIDS. 2005;16:755–9. doi: 10.1258/095646205774763090. [DOI] [PubMed] [Google Scholar]
- 32.Ford N, Reuter H, Bedelu M, Schneider H, Reuter H. Sustainability of long-term treatment in a rural district: the Lusikisiki model of decentralized HIV/AIDS care. S Afr J Med. 2006;26:17–22. [Google Scholar]
- 33.Perez F, Mukotekwa T, Miller A, Orne-Gliemann J, Glenshaw M, Chitsike I, et al. Implementing a rural program of prevention of mother-to-child transmission of HIV in Zimbabwe: first 18 months of experience. Trop Med Int Health. 2004;9(7):774–83. doi: 10.1111/j.1365-3156.2004.01264.x. [DOI] [PubMed] [Google Scholar]
- 34.Wanyu B, Diom E, Mitchell P, Tih PM, Meyer DJ. Birth attendants trained in “prevention of mother-to-child HIV transmission” provide care in rural Cameroon, Africa. J Midwifery Womens Health. 2007;52:334–41. doi: 10.1016/j.jmwh.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 35.Zachariah R, Teck R, Buhendwa L, Labana S, Chinji C, Humblet P, et al. How can the community contribute in the fight against HIV/AIDS and tuberculosis? An example from a rural district in Malawi. Trans R Soc Trop Med Hyg. 2006;100:167–75. doi: 10.1016/j.trstmh.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 36.Thomson KA, Cheti EO, Teid T. Implementation and outcomes of an active defaulter tracing system for HIV, prevention of mother to child transmission of HIV (PMTCT) and TB patients in Kibera, Nairobi, Kenya. Trans R Soc Trop Med Hyg. 2011;105:320–6. doi: 10.1016/j.trstmh.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 37.Myer L, Rabkin M, Abrams EJ, Rosenfield A, El-Sadr WM. Focus on women: linking HIV care and treatment with reproductive health services in the MTCT-Plus initiative. Reprod Health Matters. 2011;13(25):136–46. doi: 10.1016/s0968-8080(05)25185-6. [DOI] [PubMed] [Google Scholar]