Abstract
Context
Neuromuscular deficits are common in people with chronic ankle instability (CAI). Corticomotor pathways are very influential in the production of voluntary muscle function, yet these pathways have not been evaluated in people with CAI.
Objective
To determine if corticomotor excitability of the fibularis longus (FL) differs between individuals with unilateral CAI and matched control participants without CAI.
Design
Case-control study.
Setting
Laboratory.
Patients or Other Participants
Ten people with CAI (4 men, 6 women; age = 21.2 ± 1.23 years, height = 175.13 ± 9.7 cm, mass = 77.1 ± 13.58 kg) and 10 people without CAI (4 men, 6 women; age = 21.2 ± 2.3 years; height = 172.34 ± 8.86 cm, mass = 73.4 ± 7.15 kg) volunteered for this study.
Main Outcome Measure(s)
Transcranial magnetic stimulation was performed over the motor cortex on neurons corresponding with the FL. All testing was performed with the participant in a seated position with a slightly flexed knee joint and the ankle secured in 10° of plantar flexion. The resting motor threshold (RMT), which was expressed as a percentage of 2 T, was considered the lowest amount of magnetic energy that would induce an FL motor evoked potential equal to or greater than 20 μV, as measured with surface electromyography, on 7 consecutive stimuli. In addition, the Functional Ankle Disability Index (FADI) and FADI Sport were used to assess self-reported function.
Results
Higher RMTs were found in the injured and uninjured FL of the CAI group (60.8% ± 8.4% and 59.1% ± 8.99%, respectively) than the healthy group (52.8% ± 8.56% and 52% ± 7.0%, respectively; F1,18 = 4.92, P = .04). No leg × group interactions (F1,18 = 0.1, P = .76) or between-legs differences (F1,18 = 0.74, P = .40) were found. A moderate negative correlation was found between RMT and FADI (r = −0.4, P = .04) and FADI Sport (r = −0.44, P = .03), suggesting that higher RMT is related to lower self-reported function.
Conclusions
Higher bilateral RMTs may indicate deficits in FL corticomotor excitability in people with CAI. In addition, a moderate correlation between RMT and FADI suggests that cortical excitability deficits may be influential in altering function.
Key Words: motor cortex, neuromuscular activity, muscles, transcranial magnetic stimulation
Key Points
Bilateral fibularis longus resting motor threshold was higher in participants with chronic ankle instability (CAI) than in participants without CAI.
Increased resting motor threshold might indicate deficits in fibularis longus corticomotor excitability in people with CAI.
Resting motor threshold and self-reported function were moderately correlated, suggesting deficits in corticomotor excitability might influence function.
Ankle sprains are the most common injury in physically active people and account for approximately 23%1 and 15%2 of all injuries in high school and collegiate athletics, respectively. In addition, 628 000 ankle sprains are treated annually in emergency facilities within the United States, representing approximately 20% of all injuries treated with emergency care.3 Further evidence indicates two-thirds of all ankle injuries are left untreated by health care professionals, suggesting that the true incidence of ankle injury in the United States is greater than initial estimates.3 After an initial sprain, some individuals have sequelae injuries4 and report a lack of stability around the ankle that decreases overall function.5 The rate of recurrent ankle injury might be as high as 28.3%6 and might be due to a condition termed chronic ankle instability (CAI). The knowledge regarding the CAI phenomenon is evolving, and most often it is described as a residual clinical problem in which patients exhibit repetitive lateral ankle instability resulting in multiple ankle sprains.7,8 Current theory suggests that CAI comprises factors related to mechanical instability, perceived instability, and recurrent sprain. Hertel7 comprehensively described many factors that likely contribute to CAI. Specifically, neuromuscular adaptations of the lower extremity after an acute ankle sprain have been thought to be major factors contributing to the CAI and its inherent disability.7
Neuromuscular alterations, such as diminished reflex excitability of stabilizing muscles,9,10 might contribute to the clinical impairments that affect gait,11–14 balance,15,16 and perceived function5,17 and may be risk factors for developing osteoarthritis of the ankle.18 Whereas the origin of this neuromuscular dysfunction is not completely understood, researchers have hypothesized that mechanisms within the central nervous system might modulate motor control in people with CAI.9,10,19,20 Unfortunately, only limited information is available about neural motor alterations in people with CAI. Most information regarding these neural alterations has been associated with spinal reflex differences in ankle-stabilizing muscles after acute lateral ankle sprains21 and in individuals with CAI.9 Recently, researchers22 have demonstrated neuromuscular alterations exist in the proximal quadriceps musculature of patients with CAI, which might indicate the involvement of multiple neural centers. Whereas spinal reflexive mechanisms have demonstrated differences after ankle injury,10 motor alterations arising from the motor cortex have not been studied in this population. A better understanding of the neurologic origins of the clinical impairments that patients with CAI have is imperative to developing successful intervention strategies.
Corticomotor excitability commonly is assessed using transcranial magnetic stimulation (TMS), which evokes a stimulus over the motor cortex and allows for evaluation of descending corticospinal motor pathways in the corresponding musculature.23,24 Corticomotor evaluation allows for the evaluation of the excitability of the motor cortex in the brain and of descending spinal tracts that influence the production of voluntary human movement. Investigators have found that the corticomotor excitability of leg muscles is sensitive to changes in posture control25 and is involved with anticipatory postural reactions.26 Whereas postural control deficits are common in people with ankle injury,27 we do not know if corticomotor excitability is altered in people with ankle instability or if corticomotor excitability of leg muscles affects self-reported function.
Therefore, the purpose of our study was to determine if corticomotor excitability of the fibularis longus (FL) differs between individuals with unilateral CAI and matched control participants without CAI. To our knowledge, we are the first to investigate corticomotor excitability in patients with CAI; therefore, we evaluated the FL because it has been found to exhibit reflexive dysfunction in similar patients9 and its function might be important for resisting inversion of the ankle. We also investigated how corticomotor excitability of the FL relates to self-reported function in individuals with and without CAI. We hypothesized that FL excitability would be lower in the injured ankle than the uninjured ankle in people with CAI and would be lower in both ankles of people with CAI than in the ankles of healthy matched control participants. We also hypothesized that decreased corticomotor excitability would be related to decreased self-reported function.
METHODS
This case-control study involved 2 groups of individuals: those with unilateral CAI and matched control participants without CAI. Corticomotor excitability was tested bilaterally in both groups using resting motor thresholds (RMTs) of the FL muscle, and self-reported function was assessed with the Functional Ankle Disability Index (FADI) and FADI Sport.17 The control group was assigned an “injured” limb for matching purposes, and the order of leg tested was randomized in both groups. The same investigator (B.G.P.) conducted outcome measures in all participants.
Participants
Twenty-three people initially volunteered for this study. Three potential participants were excluded because bilateral measurable motor evoked potentials could not be elicited (1 with CAI, 2 without CAI); therefore, 20 participants were included in the final data analysis. Demographic data are provided in the Table. Participants had no neurologic or muscular disease; history of brain or cranial surgeries, migraines, or concussion in the 6 months before the study; or history of knee injury or surgery. Participants with CAI had a history of at least 2 unilateral ankle sprains and decreased self-reported function (FADI <90%, FADI Sport <80%).17 No participant with CAI had sprained his or her ankle in the 6 weeks before testing. In addition, no participant reported symptoms of instability for the uninjured ankle in the CAI group or for either ankle in the control group (FADI >95%, FADI Sport >85%). Healthy control participants without CAI were matched to participants with CAI based on sex, age, height, and mass. To limit the potential bias of limb dominance (dominant, nondominant), we matched the injured ankle in the healthy group to that of the CAI counterpart based on side dominance instead of merely matching by side (right and left limb). For example, if a participant with CAI had an injured nondominant leg, the nondominant leg of the corresponding healthy matched participant would be assigned as the injured limb regardless of the side (right, left) on which the injury had occurred. We defined the dominant limb as the limb with which participants reported they preferred to kick a ball. All participants provided written informed consent, and the study was approved by the Institutional Review Board of the University of Toledo.
Table.
Participant Demographics and Main Outcome Measures (Mean ± SD)
| Characteristic |
Chronic Ankle Instability Group (n = 10) |
Healthy Matched Control Group (n = 10) |
| Sex | ||
| Male | 4 | 4 |
| Female | 6 | 6 |
| Age, y | 21.2 ± 1.23 | 21.2 ± 2.3 |
| Height, cm | 175.13 ± 9.7 | 172.34 ± 8.86 |
| Mass, kg | 77.1 ± 13.58 | 73.4 ± 7.15 |
| Functional Ankle Disability Index (maximum = 100.0) | ||
| Injured | 81.4 ± 7.2a,b | 99.9 ± .32 |
| Uninjured | 96.9 ± 2.15a | 99.9 ± .32 |
| Functional Ankle Disability Index Sport (maximum = 100.0) | ||
| Injured | 65.5 ± 7.5a,b | 100.0 ± .00 |
| Uninjured | 94.6 ± 7.53a | 100.0 ± .00 |
| Resting motor threshold, % of 2 T | ||
| Injured | 60.8 ± 8.4c | 52.8 ± 8.56 |
| Uninjured | 59.1 ± 8.99c | 52 ± 7.0 |
Indicates different from healthy matched control group (P ≤ .001).
Indicates lower than uninjured limb of chronic ankle instability group (P < .001).
Indicates different from healthy matched control group (P = .04).
Experimental Procedures
Participants were positioned on a dynamometer seat (Biodex System II Pro; Biodex Medical Systems, Shirley, NY) with their hips flexed to 85°, knees flexed to approximately 10°, and testing ankles plantar flexed to 10°. Although force was not being measured, the dynamometer provided a means of maintaining constant patient positioning. The calcaneus was secured in a rubber heel cup mounted on a flat platform (Figure). The superolateral leg inferior to the knee joint was shaved, debrided, and cleaned with alcohol before application of the electromyography (EMG) electrodes. Disposable, 10-mm, pregelled Ag/AgCl electrodes (BIOPAC Systems, Inc, Goleta, CA) were applied, and the signal was amplified with a gain of 1000 (EMG100C; BIOPAC Systems, Inc) before being converted digitally with a 16-bit data-acquisition system (MP150; BIOPAC Systems, Inc). The EMG signal was collected at 2 kHz with a common-mode rejection ratio of 110 dB, a noise voltage of 0.2 μV, and an input impedance of 1 MΩ. Two EMG electrodes were adhered 1.75 cm apart on the greatest bulk of the FL, approximately 2 to 3 cm inferior to the fibular head (Figure).28,29 The reference electrode was positioned on the medial malleolus of the nondominant leg. AcqKnowledge software (version 3.7.3; BIOPAC Systems, Inc) was used to visualize the EMG and force signal.
Figure.
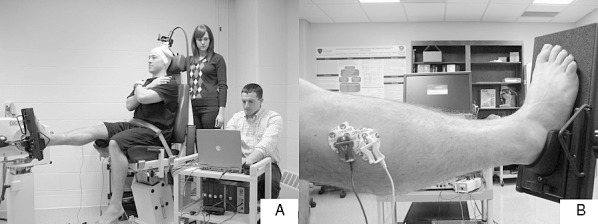
Experimental setup. A, Transcranial magnetic stimulation was performed bilaterally with a double-cone coil secured over the appropriate area on the motor cortex with the participant at rest. One investigator applied the stimulation, and another investigator recorded the peak-to-peak amplitudes of the motor evoked potentials. B, The foot was secured in a head cup during testing.
Transcranial Magnetic Stimulation
Before testing, participants donned a Lycra swim cap (Sprint Aquatics; Rothhammer International Inc, San Luis Obispo, CA) and earplugs (Aearo Co, Indianapolis, IN) to muffle the sound of the TMS. Two landmark lines were drawn on the swim cap: 1 sagittally separating hemispheres and 1 intersecting the sagittal line coronally at the external auditory meatus.30 The MagStim (model 200; MagStim Company, Ltd, Wales, United Kingdom) was used to deliver a single magnetic pulse with a possible strength of 2 T; the double-cone coil configuration allowed for a maximum of only 70% of the stimulation (1.4 T). A double-cone coil was moved anterior to posterior over the vertex of the skull while the investigator applied a magnetic stimulus of a constant intensity until the largest peak-to-peak motor evoked potential in the contralateral FL was found. This point was denoted on the swim cap with a felt-tipped marker and used as the point for stimulation during RMT testing.31 The double-cone coil was secured to the dynamometer with an articulating arm (196AB-2; Manfrotto Lino, Manfrotto, Italy).
During testing, participants were instructed to focus on an X marked on the wall in front of the dynamometer. For both legs, FL RMTs were found by using a protocol previously recommended for lower extremity corticomotor excitability testing.32 The magnetic stimulation was decreased by 5% until no motor evoked potential could be elicited. Next, the percentage of magnetic stimulation was increased by 1% until 7 consecutive stimuli32 produced a measureable motor evoked potential (>20 μV).33 The RMT was expressed as a percentage of 2 T.
Statistical Analyses
Separate independent t tests were performed to determine if differences in demographics (age, height, mass, FADI, FADI Sport) existed between groups. Paired-samples t tests were used to evaluate differences in FADI and FADI Sport between the limbs of the same participants in the CAI group. A 2 × 2 repeated-measures analysis of variance was used to determine if differences existed in RMT between groups (CAI, control) and ankles (injured, uninjured). In addition, we used separate 1-tailed Pearson product moment correlations to determine the relationships between RMT and FADI and between RMT and FADI Sport for the injured ankle of the CAI group and the matched ankle of the control group. We classified correlation coefficients of 0 to 0.4 as weak, 0.41 to 0.7 as moderate, and 0.71 to 1.0 as strong.34 The α level was set a priori at .05. All statistical analyses were performed using SPSS (version 17.0 for Windows; IBM Corporation, Somers, NY).
RESULTS
We found no differences between groups for age (t18 < 0.001, P > .99), mass (t18 = 0.67, P = .50), and height (t18 = 0.76, P = .46). The FADI (t18 = −8.1, P < .001) and FADI Sport (t18 = −3.99, P = .001) scores for the injured ankles were lower in the CAI group than in the control group. The FADI (t18 = −1.1, P < .001) and FADI Sport (t18 = 9.39, P < .001) scores for the uninjured ankles were lower in the CAI group than in the control group (Table). The FADI (t9 = −6.83, P < .001) and FADI Sport (t9 = −9.88, P < .001) scores were lower for the injured limb than for the uninjured limb in the CAI group but not in the control group (Table). No between-legs differences were found for FADI and FADI Sport scores in the control group; inferential statistics could not be performed for this comparison because means and measures of variability were identical between legs (Table).
The CAI group had a higher RMT than the control group bilaterally (F1,18 = 4.92, P = .04, 1 − β = .56) (Table). We did not find a difference between legs (F1,18 = 0.74, P = .40, 1 − β = .13) or a leg × group interaction (F1,18 = 0.1, P = .76, 1 − β = .06).
We found negative moderate correlations between FADI and FL RMT (r = −0.4, r2 = 0.16, P = .04) and between FADI Sport and RMT (r = −0.44, r2 = 0.19, P = .03) in the injured ankles of all participants, indicating that decreased function was correlated with increased RMT.
DISCUSSION
To our knowledge, we are the first to evaluate corticomotor excitability in the FL of the ankles in individuals with CAI. Our findings are important because alterations in descending corticospinal excitability may affect clinical decision making for specific interventions. Whereas little research is available on RMT in the FL, we demonstrated RMTs similar to those in previous experiments in which investigators used comparable methods in the lower extremity musculature of the quadriceps.32 Our findings, which demonstrated altered descending corticospinal pathways in CAI, may suggest the need to incorporate interventions that target descending corticospinal pathways, such as TMS35,36 and biofeedback,37 and might better address altered neural pathways originating at the motor cortex.
Increased bilateral RMTs in the FL muscle of those with CAI indicate decreased descending corticomotor excitability of ankle-stabilizing muscles. Transcranial magnetic stimulation is a relatively noninvasive method that can be used to evaluate corticomotor excitability of different muscles. Magnetic energy penetrates the skull and excites areas in the motor cortex, triggering a descending neural response that travels to a corresponding muscle and causes a measurable contraction.23 These increased RMTs suggest that a greater exogenous magnetic stimulus is needed to excite cortical neurons that correspond with muscles within the periphery. The assumption is that if these cortical neurons require increased TMS to be excited, patients with CAI may encounter more difficulty generating motor commands to the FL muscle. We do not know how an alteration in FL corticomotor excitability will affect function. In a recent systematic review, Hiller et al38 demonstrated that selected neuromuscular impairments and functional responses, such as ankle muscle strength and muscular response to a perturbation, are not grossly different between people with and without CAI. However, more sophisticated tasks incorporating postural control and gait have shown that people with CAI display deficits, suggesting that more complicated tasks may be more affected by altered RMT.38
The FL may be vital for ankle stabilization because it eccentrically controls ankle inversion and may play some role in preventing ankle sprains. Of interest, we observed an altered RMT of the FL bilaterally in the participants with CAI, yet they reported only unilateral symptoms of CAI. Whereas uninjured FADI scores were lower in the CAI group than the control group (Table), means for the uninjured FADI (96.9%) and FADI Sport (94.6%) in the CAI group were much higher than the inclusion criteria. Therefore, the uninjured ankle of the CAI group could be considered functionally asymptomatic but still demonstrated decreased corticomotor excitability. Investigators have reported bilateral deficits in movement patterns21,30 and force production39 about the knee in participants with CAI, but those researchers only quantified self-reported functional deficits in the injured ankles of the participants and theorized that bilateral alterations to reorganization in the central nervous system may help to explain the findings. However, they could not examine specific motor pathways as we have in this study. Unfortunately, as was the case for those other researchers, the retrospective study design that we used did not allow us to determine if the decreased bilateral corticomotor excitability occurs after unilateral CAI or if the decreased excitability is a predisposing factor that may lead to chronic ankle sprains. Researchers should strive to determine if this phenomenon is present in individuals who eventually have an initial acute ankle sprain or if this relationship develops after initial ankle sprain and is an important contributor to CAI and subsequent, repeated ankle conditions. In addition, further analysis is needed to determine the effect of CAI on corticomotor excitability of other stabilizing muscles, such as the anterior tibialis and soleus.
We also evaluated the relationship between the self-reported function and FL corticomotor excitability in the injured ankles of participants in both the CAI and control groups. Moderate negative correlations were found between corticomotor excitability of the FL and self-reported function. Further examination of the correlations suggested that RMT of the FL explains 16% (r2 = 0.16) of the variance in the FADI and 19% (r2 = 0.19) of the variance in the FADI Sport. Whereas 16% and 19% may seem small, the FL is only one muscle responsible for ankle stabilization. Corticomotor dysfunction possibly exists in other muscles surrounding the ankle, which may share responsibility in self-reported ankle instability. In addition, this 16% specifically relates to neuromuscular dysfunction generated by corticomotor mechanisms, which may not necessarily reflect other spinal reflex influences reported to be different in patients with CAI.9,10
Deficits in spinal reflex excitability have been reported in the musculature surrounding the ankle in those with CAI and have been attributed to arthrogenic muscle inhibition.9 This spinal reflexive muscle dysfunction may alter neuromuscular control that is vital for maintenance of postural control15,16,27 and gait,11,12 which are affected in people with CAI. We can speculate that the inability to voluntarily and reflexively excite stabilizing muscles around the ankle may contribute to neuromuscular dysfunction that perpetuates CAI in this population. Researchers have suggested that spinal reflexive deficits40 and corticomotor alterations32,41 occur in the quadriceps after knee injury or effusion, indicating that a possible combination of corticomotor and spinal reflexive deficits may contribute to neuromuscular dysfunction after lower extremity joint injuries. Further support has been noted in studies in which the authors have reported an altered motor pattern in the knees of individuals with CAI before landing,19,20,42 suggesting a potentially different feed-forward pattern may be associated with this condition. Feed-forward motor control relies on the initiation of preemptive strategies that create anticipatory movements. This differs from feedback strategies that rely on real-time sensory information to make moment-to-moment alterations in neuromuscular activation.43 Wikstrom et al13 showed that both feed-forward and feedback neural mechanisms play a role in the gross neuromuscular alterations in patients with CAI, yet further research is needed to determine which of these strategies would best be manipulated to improve function in patients with CAI.
Understanding the effect of joint injuries on specific neural pathways may be vital in the development of therapeutic interventions that can target neural mechanisms causing neuromuscular dysfunction. Many recent therapeutic advances have targeted spinal reflex inhibition44–46 in the quadriceps after knee joint injury, yet modalities that specifically influence corticomotor pathways are less advanced at this time.35,36 In addition, few researchers have assessed the effects of therapeutic interventions targeting muscle inhibition around the ankle.47 Our finding that corticomotor excitability of the FL is diminished in those with CAI may support the need for clinicians to consider targeting the motor cortex with effective interventions. Transcranial magnetic stimulation has been used to enhance neuromuscular function in the quadriceps after knee injury,35,36 but the efficacy of this intervention has not been assessed in muscles surrounding the ankle. An alternate approach may be the use of biofeedback during strength training,48 which has been used to enhance muscle strength by attempting to involve increased cortical control.
Our study had limitations. Whereas RMT is a common and central33 outcome measure to assess corticomotor excitability, a plethora of outcome measures can be evaluated via TMS. Livingston and Ingersoll31 assessed the magnitude and latency of motor evoked potentials and have evaluated the physiologic reaction of the motor evoked potential amplitudes in reaction to increasing the magnitude of the stimulus. Using a battery of outcome measures in future studies may provide more unique information that can increase our understanding about corticomotor excitability after joint injury. Furthermore, this data collection occurred during rest in a somewhat static condition. With future testing, researchers may assess corticomotor excitability during an active muscle contraction or during movement, which may reveal more about cortical muscle control during functional activity. Whereas corticomotor excitability of the FL does explain 16% of the variance associated with self-reported function, the self-reported function of other muscles, such as the tibialis anterior and surae, should be evaluated to understand the collective contribution of corticomotor excitability in various lower extremity muscles that stabilize the ankle. Researchers also may assess the relationship between cortical and spinal reflex control of muscles during movement after joint injury to determine the most influential neural pathways for therapeutic intervention.
The number of magnetic stimuli evoked in each participant varied depending on the ease of locating the optimal stimulating position and the specific nature of determining individual RMTs. Whereas we used previously published methods to minimize the amount of stimuli to locate the RMT in a systematic process,32 the repeated TMS possibly affected the thresholds of cortical neurons. Researchers have used TMS to alter neuromuscular outcomes,35,36 but many of them used higher magnetic outputs and active muscle contractions. Therefore, the potential effect that the testing measure may have had on evaluating RMT remains unknown, yet the current methods seem to be underpowered to produce a therapeutic effect.
CONCLUSIONS
We provided a unique assessment of corticomotor pathways that may be involved in altering neuromuscular function of stabilizing muscles in people with CAI. Specifically, our data indicated increased bilateral FL RMT in patients with CAI. The presence of increased RMT may be of specific interest to clinicians because this measure seems to have a moderate relationship with self-reported function.
REFERENCES
- 1.Nelson AJ, Collins CL, Yard EE, Fields SK, Comstock RD. Ankle injuries among United States high school sports athletes, 2005–2006. J Athl Train. 2007;42(3):381–387. [PMC free article] [PubMed] [Google Scholar]
- 2.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 3.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 4.Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–380. [PMC free article] [PubMed] [Google Scholar]
- 5.Carcia CR, Martin RL, Drouin JM. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swenson DM, Yard EE, Fields SK, Comstock RD. Patterns of recurrent injuries among US high school athletes, 2005–2008. Am J Sports Med. 2009;37(8):1586–1593. doi: 10.1177/0363546509332500. [DOI] [PubMed] [Google Scholar]
- 7.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 8.Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. J Athl Train. 2011;46(2):133–141. doi: 10.4085/1062-6050-46.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McVey ED, Palmieri RM, Docherty CL, Zinder SM, Ingersoll CD. Arthrogenic muscle inhibition in the leg muscles of subjects exhibiting functional ankle instability. Foot Ankle Int. 2005;26(12):1055–1061. doi: 10.1177/107110070502601210. [DOI] [PubMed] [Google Scholar]
- 10.Sefton J, Hicks-Little C, Hubbard T et al. Segmental spinal reflex adaptations associated with chronic ankle instability. Arch Phys Med Rehabil. 2008;89(10):1991–1995. doi: 10.1016/j.apmr.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Drewes LK, McKeon PO, Paolini G et al. Altered ankle kinematics and shank-rear-foot coupling in those with chronic ankle instability. J Sport Rehabil. 2009;18(3):375–388. doi: 10.1123/jsr.18.3.375. [DOI] [PubMed] [Google Scholar]
- 12.Drewes LK, McKeon PO, Kerrigan DC, Hertel J. Dorsiflexion deficit during jogging with chronic ankle instability. J Sci Med Sport. 2009;12(6):685–687. doi: 10.1016/j.jsams.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Wikstrom EA, Bishop MD, Inamdar AD, Hass CJ. Gait termination control strategies are altered in chronic ankle instability subjects. Med Sci Sports Exerc. 2010;42(1):197–205. doi: 10.1249/MSS.0b013e3181ad1e2f. [DOI] [PubMed] [Google Scholar]
- 14.Hass CJ, Bishop MD, Doidge D, Wikstrom EA. Chronic ankle instability alters central organization of movement. Am J Sports Med. 2010;38(4):829–834. doi: 10.1177/0363546509351562. [DOI] [PubMed] [Google Scholar]
- 15.Wikstrom EA, Fournier KA, McKeon PO. Postural control differs between those with and without chronic ankle instability. Gait Posture. 2010;32(1):82–86. doi: 10.1016/j.gaitpost.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 16.Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25(1):33–39. doi: 10.1016/j.gaitpost.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 18.Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61(3):354–361. [PubMed] [Google Scholar]
- 19.Caulfield BM, Garrett M. Functional instability of the ankle: differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int J Sports Med. 2002;23(1):64–68. doi: 10.1055/s-2002-19272. [DOI] [PubMed] [Google Scholar]
- 20.Gribble P, Robinson R. Differences in spatiotemporal landing variables during a dynamic stability task in subjects with CAI. Scand J Med Sci Sports. 2010;20(1):e63–e71. doi: 10.1111/j.1600-0838.2009.00899.x. [DOI] [PubMed] [Google Scholar]
- 21.Klykken LW, Pietrosimone BG, Kim KM, Ingersoll CD, Hertel J. Motor-neuron pool excitability of the lower leg muscles after acute lateral ankle sprain. J Athl Train. 2011;46(3):263–269. doi: 10.4085/1062-6050-46.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sedory EJ, McVey ED, Cross KM, Ingersoll CD, Hertel J. Arthrogenic muscle response of the quadriceps and hamstrings with chronic ankle instability. J Athl Train. 2007;42(3):355–360. [PMC free article] [PubMed] [Google Scholar]
- 23.Hallett M. Transcranial magnetic stimulation and the human brain. Nature. 2000;406(6792):147–150. doi: 10.1038/35018000. [DOI] [PubMed] [Google Scholar]
- 24.Rossini PM, Rossi S. Transcranial magnetic stimulation: diagnostic, therapeutic, and research potential. Neurology. 2007;68(7):484–488. doi: 10.1212/01.wnl.0000250268.13789.b2. [DOI] [PubMed] [Google Scholar]
- 25.Solopova IA, Kazennikov OV, Deniskina NB, Levik YS, Ivanenko YP. Postural instability enhances motor responses to transcranial magnetic stimulation in humans. Neurosci Lett. 2003;337(1):25–28. doi: 10.1016/s0304-3940(02)01297-1. [DOI] [PubMed] [Google Scholar]
- 26.Petersen TH, Rosenberg K, Petersen NC, Nielsen JB. Cortical involvement in anticipatory postural reactions in man. Exp Brain Res. 2009;193(2):161–171. doi: 10.1007/s00221-008-1603-6. [DOI] [PubMed] [Google Scholar]
- 27.Wikstrom EA, Naik S, Lodha N, Cauraugh JH. Bilateral balance impairments after lateral ankle trauma: a systematic review and meta-analysis. Gait Posture. 2010;31(4):407–414. doi: 10.1016/j.gaitpost.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Palmieri RM, Ingersoll CD, Hoffman MA et al. Arthrogenic muscle response to a simulated ankle joint effusion. Br J Sports Med. 2004;38(1):26–30. doi: 10.1136/bjsm.2002.001677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delagi E, Perotto A, Iazzetti J, Morrison D. Anatomic Guide for the Electromyographer: The Limbs. 2nd ed. Springfield, IL: Charles C Thomas Publishers; 1981. [Google Scholar]
- 30.Norte GE, Pietrosimone BG, Hart JM, Hertel J, Ingersoll CD. Relationship between transcranial magnetic stimulation and percutaneous electrical stimulation in determining the quadriceps central activation ratio. Am J Phys Med Rehabil. 2010;89(12):986–996. doi: 10.1097/PHM.0b013e3181f1c00e. [DOI] [PubMed] [Google Scholar]
- 31.Livingston SC, Ingersoll CD. Intra-rater reliability of a transcranial magnetic stimulation technique to obtain motor evoked potentials. Int J Neurosci. 2008;118(2):239–256. doi: 10.1080/00207450701668020. [DOI] [PubMed] [Google Scholar]
- 32.Heroux ME, Tremblay F. Corticomotor excitability associated with unilateral knee dysfunction secondary to anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2006;14(9):823–833. doi: 10.1007/s00167-006-0063-4. [DOI] [PubMed] [Google Scholar]
- 33.Mills KR, Nithi KA. Corticomotor threshold to magnetic stimulation: normal values and repeatability. Muscle Nerve. 1997;20(5):570–576. doi: 10.1002/(sici)1097-4598(199705)20:5<570::aid-mus5>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 34.Lomax RG. Lomax RG. Statistical Concepts: A Second Course for Education and Behavioral Sciences. Mahwah, NJ: Lawrence Erlbaum Associates; 1998. Bivariate measures of association; pp. 179–188. In. [Google Scholar]
- 35.Gibbons CE, Pietrosimone BG, Hart JM, Saliba SA, Ingersoll CD. Transcranial magnetic stimulation and volitional quadriceps activation. J Athl Train. 2010;45(6):570–579. doi: 10.4085/1062-6050-45.6.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Urbach D, Berth A, Awiszus F. Effect of transcranial magnetic stimulation on voluntary activation in patients with quadriceps weakness. Muscle Nerve. 2005;32(2):164–169. doi: 10.1002/mus.20353. [DOI] [PubMed] [Google Scholar]
- 37.Lepley AS, Gribble PA, Pietrosimone BG. Effects of electromyographic biofeedback on quadriceps strength: a systematic review. J Strength Cond Res. 2012;26(3):873–882. doi: 10.1519/JSC.0b013e318225ff75. [DOI] [PubMed] [Google Scholar]
- 38.Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011;45(8):660–672. doi: 10.1136/bjsm.2010.077404. [DOI] [PubMed] [Google Scholar]
- 39.Gribble PA, Robinson RH. An examination of ankle, knee, and hip torque production in individuals with chronic ankle instability. J Strength Cond Res. 2009;23(2):395–400. doi: 10.1519/JSC.0b013e31818efbb2. [DOI] [PubMed] [Google Scholar]
- 40.Palmieri RM, Tom JA, Edwards JE et al. Arthrogenic muscle response induced by an experimental knee joint effusion is mediated by pre- and post-synaptic spinal mechanisms. J Electromyogr Kinesiol. 2004;14(6):631–640. doi: 10.1016/j.jelekin.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 41.On A, Uludag B, Taskiran E, Ertekin C. Differential corticomotor control of a muscle adjacent to a painful joint. Neurorehabil Neural Repair. 2004;18(3):127–133. doi: 10.1177/0888439004269030. [DOI] [PubMed] [Google Scholar]
- 42.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–355. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kandel ER, Schwartz JH, Jessell TM. Principles of Neural Science. 3rd ed. Norwalk, CT: Appleton & Lange; 1991. [Google Scholar]
- 44.Hopkins JT, Ingersoll CD, Edwards J, Klootwyk TE. Cryotherapy and transcutaneous electric neuromuscular stimulation decrease arthrogenic muscle inhibition of the vastus medialis after knee joint effusion. J Athl Train. 2002;37(1):25–31. [PMC free article] [PubMed] [Google Scholar]
- 45.Pietrosimone BG, Ingersoll CD. Focal knee joint cooling increases the quadriceps central activation ratio. J Sports Sci. 2009;27(8):873–879. doi: 10.1080/02640410902929374. [DOI] [PubMed] [Google Scholar]
- 46.Pietrosimone BG, Hart JM, Saliba SA, Hertel J, Ingersoll CD. Immediate effects of transcutaneous electrical nerve stimulation and focal knee joint cooling on quadriceps activation. Med Sci Sports Exerc. 2009;41(6):1175–1181. doi: 10.1249/MSS.0b013e3181982557. [DOI] [PubMed] [Google Scholar]
- 47.Hopkins JT, Stencil R. Ankle cryotherapy facilitates soleus function. J Orthop Sports Phys Ther. 2002;32(12):622–627. doi: 10.2519/jospt.2002.32.12.622. [DOI] [PubMed] [Google Scholar]
- 48.Durmus D, Alayli G, Canturk F. Effects of quadriceps electrical stimulation program on clinical parameters in the patients with knee osteoarthritis. Clin Rheumatol. 2007;26(5):674–678. doi: 10.1007/s10067-006-0358-3. [DOI] [PubMed] [Google Scholar]


