Abstract
Context
Individuals with and without functional ankle instability have been tested for deficits in lower limb proprioception with varied results.
Objective
To determine whether a new protocol for testing participants' joint position sense during stepping is reliable and can detect differences between participants with unstable and stable ankles.
Design
Descriptive laboratory study.
Setting
University clinical laboratory.
Patients or Other Participants
Sample of convenience involving 21 young adult university students and staff. Ankle stability was categorized by score on the Cumberland Ankle Instability Tool; 13 had functional ankle instability, 8 had healthy ankles.
Intervention(s)
Test-retest of ankle joint position sense when stepping onto and across the Active Movement Extent Discrimination Apparatus twice, separated by an interim test, standing still on the apparatus and moving only 1 ankle into inversion.
Main Outcome Measure(s)
Difference in scores between groups with stable and unstable ankles and between test repeats.
Results
Participants with unstable ankles were worse at differentiating between inversion angles underfoot in both testing protocols. On repeated testing with the stepping protocol, performance of the group with unstable ankles was improved (Cohen d = 1.06, P = .006), whereas scores in the stable ankle group did not change in the second test (Cohen d = 0.04, P = .899). Despite this improvement, the unstable group remained worse at differentiating inversion angles on the stepping retest (Cohen d = 0.99, P = .020).
Conclusions
The deficits on proprioceptive tests shown by individuals with functional ankle instability improved with repeated exposure to the test situation. The learning effect may be the result of systematic exposure to ankle-angle variation that led to movement-specific learning or increased confidence when stepping across the apparatus.
Key Words: proprioception, repeated measures, Cumberland Ankle Instability Tool
Key Points
Joint position sense scores were better on the Active Movement Extent Discrimination Apparatus using the step protocol than the standing protocol.
The functional ankle instability group scored worse than the healthy group on every protocol.
Test-retest scores for the step protocol were consistent in those with stable ankles but improved in those with unstable ankles. However, the latter group performed worse on the retest than did the former group.
The ankle is one of the most frequently injured body regions in sport. Injury proportions vary by body part among different sports and demographic groups, but ankle injuries have been reported to account for 24% to 54% of total injuries.1,2 Up to 70% of individuals with a history of ankle injury report ongoing symptoms of ankle instability or pain,3 of whom 40% report “giving way” as their main problem, resulting in functional ankle instability (FAI).
Ankle control is provided by the interaction among the active restraint from muscles,4 passive stability of noncontractile soft tissues,5 and bony geometry6 with the mediating effects of the sensorimotor system.7 The sensorimotor system incorporates sensory reception and central neurologic processing to generate preactive and reactive motor output in order to maintain healthy joint positioning during activity.8 Studies of the different forms of sensorimotor deficits that contribute to symptoms of FAI have revealed significant differences between groups with stable and unstable ankles. These include deficits in balance,9 strength,10 muscle response time to inversion perturbation,11 motoneuron pool excitability,12 and time to stabilization after landing.13
Proprioception is an integral factor in the protection and performance of ankle control.14 It is the sensory15 component of sensorimotor control8 and has been defined as afferent information arising from sensory receptors, directed at maintaining overall body posture, segmental posture, active and passive movement, and resistance to movement.8 It is further separated into 3 submodalities of sensation: joint position sense (JPS; awareness of joint angle and limb position), kinesthesia (awareness of movement), and force sense (awareness of force applied or resistance encountered).8 Deficits in JPS,13 kinesthesia,16 and force sense17 have been found in study participants with FAI.
However, not all studies of people who suffer recurrent ankle sprains have found associated deficits in ankle proprioception.18–20 These contrasting findings with current laboratory tests suggest the need for assessments that are more ecologically valid, or more comparable with functional activity, to determine deficits that affect ankle movement control at the level of routine performance and function. To date, the majority of tests carried out to evaluate proprioception involve isolating movement to the joint that is being examined and are often conducted in sitting or non–weight-bearing positions.21 Different positions and levels of weight bearing of the lower limb joints during testing result in different levels of proprioceptive acuity.21,22
For optimum ecological validity, ankle function assessments should aim to reproduce movement speeds, joint ranges of movement, and muscle forces similar to those experienced during functional activity.23 The Active Movement Extent Discrimination Apparatus (AMEDA) was developed with this intention.24 Participants are tested standing, bearing full weight, and with movements through the midrange of active ankle inversion involving the supporting musculature. Previous authors using this apparatus to test JPS have demonstrated measurable differences between insole interventions and clinically different participant groups. For example, AMEDA scores were significantly different between participants with injured and healthy ankles, although no difference was found between the injured and uninjured ankles of the same participants.24 As measured by the AMEDA, JPS can be improved by training on a wobble board.25
In our current study, we sought to further increase the ecological validity of testing ankle JPS and to evaluate the role of JPS in FAI. Our purpose was twofold: first, to test a new method of using the AMEDA by enabling participants to step onto the footplate rather than standing stationary on it; second, to assess the difference between participants with stable or functionally unstable ankles when tested with this new method (AMEDA-step) and with the original method (AMEDA-stand). The new method incorporates the benefits of the original AMEDA, such as normal leg alignment for gait, full weight bearing during testing, and incorporation of active movement to involve leg muscles. However, the new test offers improved validity because of its similarity to functional activity from incorporating movements of the participant that are associated with gait and unilateral weight bearing.
We hypothesized that the AMEDA-step protocol would produce higher JPS scores than those obtained with the original AMEDA-stand because of the increased sources of proprioceptive input. We also proposed that the AMEDA-step would demonstrate good reliability, with no difference between the test and retest scores. A final hypothesis was that the AMEDA-step protocol would differentiate between participants with stable and unstable ankles, as measured by the Cumberland Ankle Instability Tool (CAIT).26
METHODS
Design
Participants completed 3 test series on the AMEDA: AMEDA-step, AMEDA-stand, and then a repeat of the AMEDA-step. To evaluate the new protocol using the AMEDA-step, we used a cross-sectional design with 2 repeated measures for a test-retest comparison within participants and a between-groups comparison of participants with stable or unstable ankles as determined by CAIT score. The AMEDA-stand was used as a test of external validity by comparing the new protocol with the original test method.
Participants
Volunteers were sought as a sample of convenience from within the students and staff at a university. Approval for the study was obtained from the Committee for Ethics in Human Research at the university. Before the study, all participants were provided with details of the testing and data confidentiality of the study, and all gave informed consent.
No requirements existed for specific sport activity levels among participants, nor were specific age levels excluded. However, individuals with a current ankle injury were not included because FAI is by definition a chronic condition.26 Participants had no ankle injury within the past 6 months and had returned to full activity from any injury before that date. They also had to be able to step across the AMEDA at its steepest inversion angle (14.52° below the horizontal) without difficulty. All participants were in normal good health, with no injury or illness that kept them from their normal pattern of recreation and exercise. The dominant leg was determined by the preferred kicking foot.
Participants provided demographic information and a history of their sports background (all sports or fitness activity types pursued within the last 2 years). The number of sports played regularly by each participant within the last 2 years was recorded as an absolute value. Level of ankle challenge within the participant's chosen sports was classified into 3 levels: level 1 was defined as casual exercise, such as walking, with no intent to measure any increase in strength or endurance; level 2 was defined as fitness exercise, such as gym training, including classes led by an instructor, with no opponent; level 3 was defined as agility and competitive sports, such as field and court sports, with high-speed directional changes determined by the response to an opponent.
A total of 21 people volunteered to participate. The demographic and sports participation details for the groups with stable and unstable ankles and the whole sample are shown in Table 1.
Table 1.
Participants' Characteristics
| Characteristic |
Group |
Total |
|
| Stable Ankles |
Unstable Ankles |
||
| Participants, No. | 8 | 13 | 21 |
| Males:females, No. | 2:6 | 5:8 | 7:14 |
| Age, y (mean ± SD) | 23.77 ± 5.23 | 25.75 ± 9.72 | 24.52 ± 7.17 |
| Height, m (mean ± SD) | 1.72 ± 0.13 | 1.73 ± 0.14 | 1.73 ± 0.13 |
| Weight, kg (mean ± SD) | 68.38 ± 10.03 | 71.85 ± 14.57 | 70.52 ± 12.57 |
| Cumberland Ankle Instability Tool score (mean ± SD) | 29.50 ± 0.76 | 21.31 ± 3.55 | 24.43 ± 4.94 |
| Previous ankle injuries, No. | 0.25 ± 0.71 | 1.62 ± 1.61 | 1.10 ± 1.48 |
| Time since most recent sprain, mo | 12a | 45.90 ± 41.80 | 42.82 ± 40.95 |
| Sports played, No. | 3.50 ± 2.39 | 3.08 ± 1.50 | 3.24 ± 1.84 |
| Highest sport levelb | 2.50 ± 0.76 | 2.46 ± 0.78 | 2.48 ± 0.75 |
One participant was in this category, so no SD could be calculated.
Level 1 = casual exercise, such as walking, with no intent to measure any increase in strength or endurance; level 2 = fitness exercise, such as gym training, including classes led by an instructor, with no opponent; level 3 = agility and competitive sports, such as field and court sports, with high-speed directional changes determined by responses to an opponent.
Procedures
Data Collection Sequence
Participants attended a single testing session. At the start of the session, they provided their informed consent signature, demographic information, and sports history and completed the CAIT questionnaire.
Participants then completed 3 tests on the AMEDA, using their dominant leg on the footplate. The first test used the stepping protocol on the AMEDA. To avoid immediately repeating the same protocol, the second test used the stationary standing protocol on the AMEDA. The third test was a repeat of the stepping protocol. The overall measurement session took approximately 45 minutes per participant, with a recovery of 5 minutes between tests. The test sequence was the same for all participants; any other order would have required the participant to perform the 2 AMEDA-step tests consecutively.
Functional Ankle Stability
Each participant completed the CAIT (Table 1). The CAIT was developed to enable classification of FAI and has shown good reliability and validity in differentiating people with healthy ankles from those with FAI.26
The CAIT consists of 9 questions relating to ankle stability, pain, and recovery from rolling incidents. The scores for all 9 questions are added, giving an overall score for ankle stability on a scale from zero to 30 points, with lower scores representing more instability. A criterion score of 27 or less is recommended to separate those with FAI from those with stable ankles.26
The AMEDA-Stand
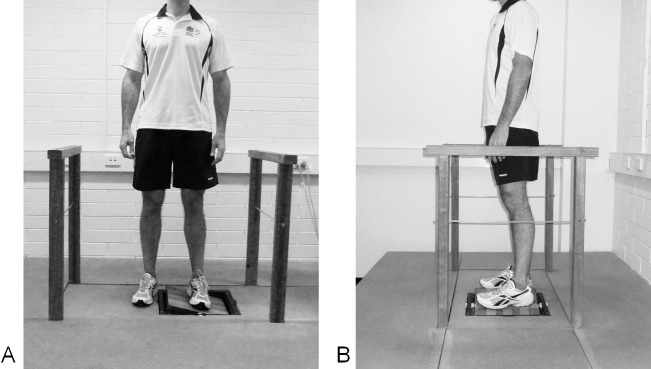
The AMEDA apparatus was developed for use in testing ankle JPS while standing24 (Figure 1). Participants stand on a square footplate, which can be tilted along its central axis by actively moving their foot. The platform enables participants to be positioned such that the plate tips into plantar flexion, dorsiflexion, inversion, or eversion, depending on the direction they face across or along the footplate. In our study, participants were positioned with their foot along the axis, with the footplate free to drop to the lateral side of the testing leg to produce an inversion movement. The apparatus was set at 5 angles of lateral tilt27 (10.49°, 11.84°, 12.55°, 13.27°, and 14.52°28), which were taught to the participant as stops 1 to 5, respectively.
Figure 1.
Front and side views of the Active Movement Extent Discrimination Apparatus during the standing protocol.
Each complete AMEDA-stand test involves a standardized warm-up, in which the participant is shown all 5 stop positions corresponding to the different ankle inversion depths, in sequence from 1 to 5, given 3 times consecutively. Participants are then presented with a test series involving 50 repetitions, with a change of angle on each repetition randomized to 1 of the 5 test angles.27 Between active inversion movements, they are asked to return the footplate to flat and hold it for a standardized interval, while the next stop angle is set. Ten repetitions of each inversion angle position are used, pseudorandomized27 to avoid giving more than 2 consecutive repetitions of any angle.
The protocol measures the participant's ability to differentiate between the angles. The participant tells the researcher which of the 5 stops he or she thinks is set for each footplate inversion. On completion, discrimination between each pair of adjacent angles is calculated using the signal detection data-analysis method described by Maher and Adams.29 The final, overall discrimination score is the average of the scores for the 4 pairwise tests. A score of 0.50 is equivalent to chance, and 1.00 is a perfect score.
Stepping Across the AMEDA
The AMEDA-step was used to test the participant's ability to distinguish between angles of inversion tilt as he or she actively stepped across the apparatus (Figure 2). This change to the AMEDA-stand test incorporates more movement from other joints of the limb, which have been shown to be important contributors to ankle proprioception,30 and allows greater feedback from the vestibular and visual systems, as is normal in functional activity.8
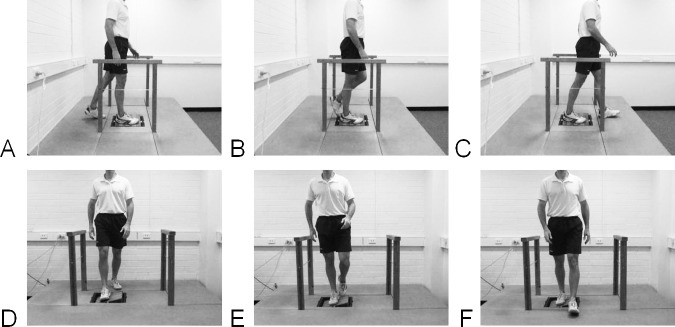
Figure 2.
Side and front views of the Active Movement Extent Discrimination Apparatus during the walking protocol. A–C, Side view. D–F, Front view. Footplate is at position 1.
The participant stood stationary on a platform facing the footplate. The footplate was weighted on its lateral edge, to hold it in the inversion position before foot contact. After the footplate was positioned at the required angle, the participant stepped onto the footplate with the test foot and completed a full step across it onto the other foot. To repeat the measurement, a return platform was added to the apparatus, enabling the participant to walk back around to the starting point. The footplate angle was reset during this time.
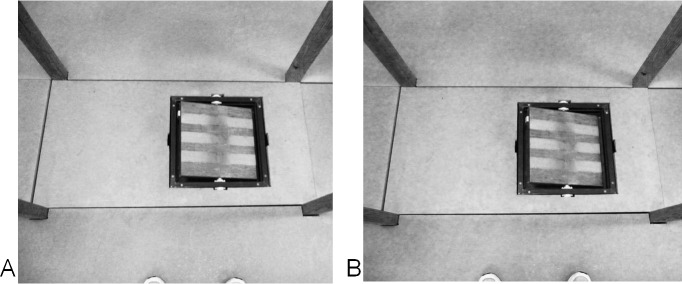
Because partially or wholly obscuring vision can change biomechanics and result in searching with the landing foot,31 participants were permitted normal use of vision throughout the trials. They were asked to look and target their step and then to raise their focus of vision and look forward horizontally as they stepped across the footplate, in order to walk with a normal, head-up posture. To reduce visual cues, the surfaces of the AMEDA were painted a homogeneous matte color (Figure 3), so that the step across the footplate was as normal as possible, to maintain ecological validity.
Figure 3.
Participant's view of the Active Movement Extent Discrimination Apparatus footplate when set at A, position 1, and B, position 5.
The same angles, number of trials, data-processing methods, and reporting protocol as those in the standing protocol were used with the AMEDA-step protocol.
Data Analysis
Data analysis was performed using SPSS (version 17; IBM Corporation, Somers, NY). A P value of .05 or less was chosen a priori to determine statistical significance.
To test our hypothesis that the AMEDA-step protocol would produce higher scores for JPS than those obtained with the AMEDA-stand, we conducted a paired-samples t test between each of the AMEDA-step tests and the AMEDA-stand test for the FAI and healthy groups. To examine whether the AMEDA-step protocol would be able to differentiate between participants with FAI and stable ankles, we conducted a 2-way analysis of variance. The outcomes of interest were the difference in the mean AMEDA-step scores between those with FAI and stable ankles and the change in the mean AMEDA-step scores within each group between the first and second tests. Having determined the pattern of significant changes between groups and test repetitions in the analysis of variance, we performed a number of t tests to evaluate the statistical significance of the simple differences at each level of testing. The Cohen d was calculated to determine effect sizes between all compared scores.32
To assess the reliability of the AMEDA-step protocol, we calculated the intraclass correlation coefficient (ICC [2,1]) between the first and second AMEDA-step tests.
RESULTS
In the stable ankle group, both the first and second AMEDA-step scores were higher than the AMEDA-stand score (Table 2). The effect size (Cohen d) for the difference between the first AMEDA-step test and the AMEDA-stand test was 1.77 (95% confidence interval [CI] = 0.69, 2.45, t = 3.39, P = .006), which constitutes a very large effect.32 The difference between the second AMEDA-step test and the AMEDA-stand test had an effect size of 1.24 (95% CI = 0.21, 2.28, t = 2.27, P = .029), which also indicates a large effect. In the FAI group, the difference between the first AMEDA-step test and the AMEDA-stand test did not reach statistical significance (effect size = 0.29, 95% CI = −0.39, 0.93, t = 0.74, P = .267). The difference between the second AMEDA-step test and the AMEDA-stand test had an effect size of 1.38 (95% CI = 0.89, 1.86, t = 5.03, P < .001), indicating a very large difference.
Table 2.
Ankle Inversion Joint Position Sense Discrimination Scores on the Active Movement Extent Discrimination Apparatus (AMEDA)
| AMEDA-Step, Test 1 |
AMEDA-Stand |
AMEDA-Step, Test 2 |
AMEDA-Step Difference (95% Confidence Interval) |
|
| Area under the curve (mean ± SD) | ||||
| Stable ankles | 0.761 ± 0.029 | 0.711 ± 0.028 | 0.762 ± 0.04 | 0.001 (−0.021, 0.024) |
| Unstable ankles | 0.688 ± 0.042 | 0.677 ± 0.037 | 0.727 ± 0.03 | 0.038 (0.013, 0.063) |
| Group difference (95% confidence interval) | ||||
| 0.073 (0.038, 0.108) | 0.034 (0.002, 0.066) | 0.035 (0.002, 0.069) | 0.037 (0.003, 0.072) | |
Ankle stability had an influence on AMEDA-step test-retest reliability, resulting in an interaction between our second and third hypotheses. The AMEDA-step data were analyzed using a 2 (ankle group: FAI, healthy) × 2 (test: AMEDA-step 1, 2) analysis of variance (Table 2).
A significant between-groups effect of ankle stability on AMEDA-step score was noted (F1,19 = 14.518, P = .001, ηp2 = 0.433). When the scores of both tests were considered together, the FAI participants scored lower on inversion JPS than did those with stable ankles. For each of the 3 AMEDA tests, the FAI and stable ankle groups differed, with the FAI group consistently demonstrating less JPS. In the first AMEDA-step test, the effect size (Cohen d) for this difference was 1.96 (95% CI = 1.24, 2.67, t = 4.34, 1-tailed P <.001), a very large effect. In the intervening AMEDA-stand test, the effect size was 1.00 (95% CI = 0.28, 1.72, t = 2.24, 1-tailed P = .014), again showing a large effect. In the second AMEDA-step test, the effect size was 0.89 (95% CI = 0.10, 1.68, t = 2.21, 1-tailed P = .034), also a large effect.
Repetition of the AMEDA-step test had a significant effect on scores (F1,19 = 5.784, P =.027, ηp2 = 0.233), with the combined groups of participants scoring higher on the second test. An interaction between ankle stability group and AMEDA-step test repeat was demonstrated (F1,19 = 5.078, P = .036, ηp2 = 0.211). Repetition of the test led to a significantly greater increase in AMEDA-step score for the FAI group than for the healthy group, indicating an increase in JPS (Figure 4). For the stable ankle group, the AMEDA-step score showed almost no change between the first and second tests. Thus, the gain in score on the second trial of the AMEDA-step was almost entirely due to the higher score within the FAI group alone. The effect sizes (Cohen d) for the change in mean scores on retesting across the AMEDA-step were 0.99 (95% CI = 0.46, 1.51, t = 3.35, P = .003) for the FAI group (which constitutes a large effect) and 0.03 (95% CI = −0.41, 0.47, t = 0.13, P = .450) for the healthy group.
Figure 4.
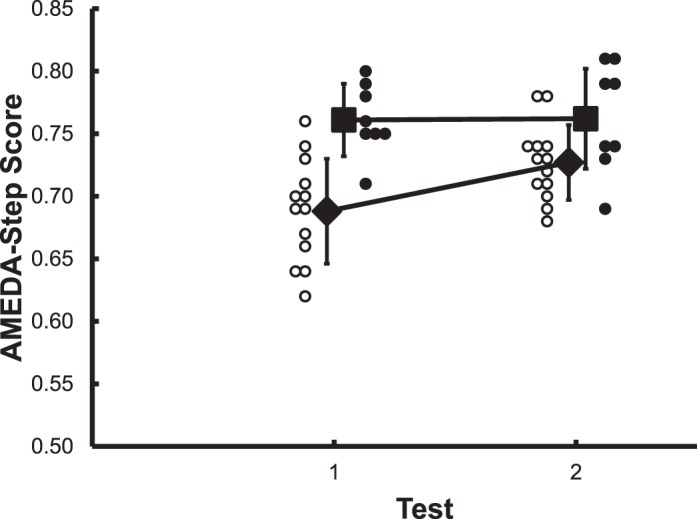
Effect of ankle stability on test-retest scores for the Active Movement Extent Discrimination Apparatus (AMEDA)–walking protocol. ▪ = Group mean score for stable ankles, ♦ = group mean score for unstable ankles, • = individual scores for stable ankles, ○ = individual scores for unstable ankles. Error bars represent SDs.
Using the 2 AMEDA-step test scores for the stable ankle group to evaluate test-retest reliability, the resulting ICC indicated a consistent pattern of scoring (ICC = 0.83, mean difference = 0.0013, SEM = 0.01, P = .012, 95% CI = 0.23, 0.97).
DISCUSSION
Overall Findings
Our hypothesis that the AMEDA-step would produce higher JPS scores, representing greater JPS acuity, than the AMEDA-stand was confirmed in the group with stable ankles. This was demonstrated in both comparisons between the AMEDA-stand and each of the AMEDA-step tests, with large effect sizes for the differences between test conditions. However, in the FAI group, the difference in scores between the first test of the AMEDA-step and the AMEDA-stand was small, likely because of the initial low score on the AMEDA-step test. In their second AMEDA-step test, FAI participants scored higher than on the AMEDA-stand test.
On the test-retest of the AMEDA-step, the large increase in JPS score within the FAI group indicates improved capacity to discriminate midrange inversion angles and thus an overall learning effect for test repetition. The mechanism for this improvement in sensory discrimination requires further study but may reflect a lack of confidence when stepping on the angled plate in the first test. The learning differential between the FAI and healthy groups on retesting is of clinical interest and was examined with regard to our other hypothesis, that the AMEDA can differentiate between ankle stability groups. It suggests a difference in stability of proprioceptive skill or in confidence between the groups, rather than an inconsistency within the test protocol. This difference in learning effect with repeated testing in the FAI group has not been demonstrated previously and warrants consideration when investigating and rehabilitating ankle injuries. It would suggest that adequate familiarization with testing procedures needs to be established before scores are interpreted. This factor should either be controlled as a confounding variable or included as a variable of interest when studying longitudinal changes in JPS.
As further support for the hypothesis that the AMEDA would demonstrate differences between groups, both the AMEDA-step and -stand protocols revealed differences in JPS between ankle stability groups within each of the 3 tests. The healthy group performed better than the FAI group in differentiating the foot-inversion angle, whether they were standing on or stepping across the AMEDA. This deficit in the unstable group is similar to the results of other tests of ankle function17,33 and is further support for previous findings that individuals with FAI have deficits in active JPS.13
The difference between stability groups for AMEDA-step to AMEDA-stand was greater on the first trial of AMEDA-step. A learning effect enabled the FAI group to reduce the gap in performance relative to the healthy group. Despite this gain in JPS score on the second test, the FAI group remained at a lower JPS score than did the stable ankle group. Individuals with FAI produce different gait patterns and use different control strategies than those with healthy ankles,34–36 and it may be that this altered control is influenced by the sensory deficits exhibited during the AMEDA-step test.
Because the largest difference between groups occurred at the first exposure to the test, the amount of prior experience with a test requires careful consideration in research design. The learning effect in the more disadvantaged group may hide clinically significant differences between populations if too much practice on a test is permitted or if the first exposure to a JPS test is influenced by participant uncertainty. The same standardized warm-up was used for each AMEDA test repetition; it appears to have been adequate to allow stability of testing in the healthy group but has revealed performance variations in the FAI group. Further investigation is required to determine whether people with unstable ankles maintain the improvement after the testing session and whether this same improvement is demonstrated between repeated tests with longer interim rest periods.
In this study, the AMEDA-step displayed testing reliability in a healthy population and differences in testing between participants with different levels of ankle function. Further study is needed using this apparatus and protocol to determine whether a difference in proprioception skill exists between sides in participants with more subtle FAI or at a higher functional status than has previously been detectable.24,37
The improved performance within a testing session of 45 minutes' duration suggests that the change was not due to recovery of any physical damage in the receptor tissues in the lower limb. In the absence of any treatment intervention, no physiologic basis for tissue healing or recovery within this time frame has been reported for the ankle. This learning effect can be considered implicit learning,38 resulting from repeated exposure to a task without external feedback. Implicit learning occurs most efficiently when the demands of the task are varied.39 The varied nature of the 3 randomized trials of the AMEDA protocol may have further enhanced this effect. The nature of implicit learning is robust enough to be retained between repeated trials of a complex series of differentiation choices.40 Further study is required to evaluate this format of sensorimotor challenge and establish whether it can play a role in enhancing rehabilitation programs.
Altered neuromuscular processing has also been associated with differences in positioning of the foot and ankle during gait35 and may contribute to episodes of inversion sprain.41 These risks are inherent in every poorly controlled footstep. Hence, the effect of minor changes in proprioception that may contribute to this neuromuscular control deficit is amplified by the thousands of footsteps occurring per day. The large JPS gains made by the FAI group are of particular relevance when considered in light of the number of repetitions of movement and loading experienced by the lower limb during normal activity. Minor changes in obstacle clearance can have a significant effect on risk of injury.42 Because small errors in the perceived angle of the foot and ankle may change the height of the leading foot in clearing an obstacle,43 small JPS deficits may increase the risk of tripping.
If the improvement shown in our study is assisted by gains in confidence with repetition, it may be that rehabilitation programs can be designed to overcome functional changes in mobility patterns by directly exposing those with unstable ankles to workloads and tasks involving proprioceptive challenges. Patients with chronic pain can improve their function and build confidence to overcome fear and avoidance of pain by exposure in vivo to workloads that they normally avoid.44 This sort of exposure may result in more normal movement patterns and hence produce immediate changes in proprioceptive accuracy. If the improvement arises from reactivation of inhibited or dysfunctional psychomotor processes, perhaps the recovery process in patients can be facilitated by exposure to proprioceptive tasks.
Clinical Relevance
The difference between individuals with FAI and healthy ankles at the first experience with a test and subsequent differences in learning effects may be significant indicators of functional ankle stability status. Individuals with FAI have the potential to rehabilitate this deficit through systematic exposure to activities with proprioceptive demands, particularly when those tasks involve clear increments of change rather than continuous variations in angle. This learning effect should be considered when evaluating the outcomes of treatment or ankle training.
Limitations
The test-retest reliability of AMEDA-step protocol is demonstrated by the consistent scores between tests in the healthy group, supporting the hypothesis. Individuals who reported no ankle instability performed at a high level at their first introduction to the AMEDA-step test and remained consistent at this level. As a consequence, the ICC between retest scores in this group is high. The large systematic increase in AMEDA-step scores on retesting for the FAI group makes these scores inappropriate for obtaining a reliability measure.45 Thus, further testing is needed to evaluate AMEDA-step reliability with an adapted FAI group.
The participants in this study were permitted free use of vision in preparing for each step across the AMEDA, although they were asked to maintain their focus on the horizon as they crossed the footplate. We felt this was in keeping with the aim of producing an ecologically valid testing protocol, because vision is typically available during normal activity to inform spatial awareness. However, the participants kept their heads up and did not see the footplate during the AMEDA-stand test, so it is likely that vision contributed to the increased accuracy exhibited by all participants during this test. Further study is needed to clarify the contribution of vision to this test regime, by differentiating focal from peripheral vision and occluding vision of the footplate. It is also important to note that the learning effect was constrained to the FAI group, despite the fact that both groups experienced the same visual conditions, suggesting that the healthy group was already performing at its highest level from the outset.
A longer approach to the footplate might result in different performance levels because of different neuromuscular control patterns and different stress levels on anatomical tissues. However, a longer approach would also require increased use of visual cues when nearing the footplate.
CONCLUSIONS
Participants produced a better JPS score when tested using the AMEDA-step protocol than in stationary standing. Those with stable ankles had consistent test-retest scores on the AMEDA-step, whereas those with unstable ankles demonstrated a learning effect. Despite this latter improvement, the FAI group performed worse on the second test than did the healthy group. All the AMEDA protocols demonstrated that FAI participants did not score as well as those with stable ankles. The AMEDA-step test was the more sensitive test (participants scored higher than on the AMEDA-stand) and also revealed a significantly different learning effect between the stable and unstable ankle groups. The healthy group showed no change on retesting with the AMEDA-step, whereas the FAI group demonstrated improvement.
REFERENCES
- 1.Cumps E, Verhagen E, Meeusen R. Prospective epidemiological study of basketball injuries during one competitive season: ankle sprains and overuse knee injuries. J Sports Sci Med. 2007;6(2):204–211. [PMC free article] [PubMed] [Google Scholar]
- 2.Bahr R, Bahr IA. Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports. 1997;7(3):166–171. doi: 10.1111/j.1600-0838.1997.tb00134.x. [DOI] [PubMed] [Google Scholar]
- 3.Braun BL. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch Fam Med. 1999;8(2):143–148. doi: 10.1001/archfami.8.2.143. [DOI] [PubMed] [Google Scholar]
- 4.Arnold BL, Linens SW, de la Motte SJ, Ross SE. Concentric evertor strength differences and functional ankle instability: a meta-analysis. J Athl Train. 2009;44(6):653–662. doi: 10.4085/1062-6050-44.6.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hubbard TJ. Ligament laxity following inversion injury with and without chronic ankle instability. Foot Ankle Int. 2008;29(3):305–311. doi: 10.3113/FAI.2008.0305. [DOI] [PubMed] [Google Scholar]
- 6.Magerkurth O, Frigg A, Hintermann B, Dick W, Valderrabano V. Frontal and lateral characteristics of the osseous configuration in chronic ankle instability. Br J Sports Med. 2010;44(8):568–572. doi: 10.1136/bjsm.2008.048462. [DOI] [PubMed] [Google Scholar]
- 7.Hass CJ, Bishop MD, Doidge D, Wikstrom EA. Chronic ankle instability alters central organization of movement. Am J Sports Med. 2010;38(4):829–834. doi: 10.1177/0363546509351562. [DOI] [PubMed] [Google Scholar]
- 8.Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71–79. [PMC free article] [PubMed] [Google Scholar]
- 9.Arnold BL, de la Motte SJ, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41(5):1048–1062. doi: 10.1249/MSS.0b013e318192d044. [DOI] [PubMed] [Google Scholar]
- 10.Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J Athl Train. 2002;37(4):487–493. [PMC free article] [PubMed] [Google Scholar]
- 11.Konradsen L, Ravn JB. Ankle instability caused by prolonged peroneal reaction time. Acta Orthop Scand. 1990;61(5):388–390. doi: 10.3109/17453679008993546. [DOI] [PubMed] [Google Scholar]
- 12.McVey ED, Palmieri RM, Docherty CL, Zinder SM, Ingersoll CD. Arthrogenic muscle inhibition in the leg muscles of subjects exhibiting functional ankle instability. Foot Ankle Int. 2005;26(12):1055–1061. doi: 10.1177/107110070502601210. [DOI] [PubMed] [Google Scholar]
- 13.Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2009;13(1):2–12. doi: 10.1016/j.jsams.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37(1):80–84. [PMC free article] [PubMed] [Google Scholar]
- 15.Sherrington CS. The Integrative Action of the Nervous System. New Haven, CT: Yale University Press; 1906. [Google Scholar]
- 16.Forkin DM, Koczur C, Battle R, Newton RA. Evaluation of kinesthetic deficits indicative of balance control in gymnasts with unilateral chronic ankle sprains. J Orthop Sports Phys Ther. 1996;23(4):245–250. doi: 10.2519/jospt.1996.23.4.245. [DOI] [PubMed] [Google Scholar]
- 17.Docherty CL, Arnold BL. Force sense deficits in functionally unstable ankles. J Orthop Res. 2008;26(11):1489–1493. doi: 10.1002/jor.20682. [DOI] [PubMed] [Google Scholar]
- 18.Brown C, Ross S, Mynark R, Guskiewicz K. Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J Sport Rehabil. 2004;13(2):122–134. [Google Scholar]
- 19.de Noronha M, Refshauge KM, Kilbreath SL, Crosbie J. Loss of proprioception or motor control is not related to functional ankle instability: an observational study. Aust J Physiother. 2007;53(3):193–198. doi: 10.1016/s0004-9514(07)70027-2. [DOI] [PubMed] [Google Scholar]
- 20.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Refshauge KM, Fitzpatrick RC. Perception of movement at the human ankle: effects of leg position. J Physiol. 1995;488(pt 1):243–248. doi: 10.1113/jphysiol.1995.sp020962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hsu LJ, Lin SI, Li SW, Tsai IJ, Liao CF. Effect of weight bearing on ankle joint position sense. J Biomech. 2006;39(suppl 1):S484. [Google Scholar]
- 23.Riemann BL, Myers JB, Lephart SM. Sensorimotor system measurement techniques. J Athl Train. 2002;37(1):85–98. [PMC free article] [PubMed] [Google Scholar]
- 24.Waddington G, Adams R. Discrimination of active plantarflexion and inversion movements after ankle injury. Aust J Physiother. 1999;45(1):7–13. doi: 10.1016/s0004-9514(14)60335-4. [DOI] [PubMed] [Google Scholar]
- 25.Waddington G, Adams R, Jones A. Wobble board (ankle disc) training effects on the discrimination of inversion movements. Aust J Physiother. 1999;45(2):95–101. doi: 10.1016/s0004-9514(14)60341-x. [DOI] [PubMed] [Google Scholar]
- 26.Hiller C, Refshauge K, Bundy A, Herbert R, Kilbreath S. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 27.Waddington G, Adams R. Ability to discriminate movements at the ankle and knee is joint specific. Percept Mot Skills. 1999;89(3 pt 1):1037–1041. doi: 10.2466/pms.1999.89.3.1037. [DOI] [PubMed] [Google Scholar]
- 28.Waddington G, Seward H, Wrigley T, Lacey N, Adams R. Comparing wobble board and jump-landing training effects on knee and ankle movement discrimination. J Sci Med Sport. 2000;3(4):449–459. doi: 10.1016/s1440-2440(00)80010-9. [DOI] [PubMed] [Google Scholar]
- 29.Maher CG, Adams RD. Stiffness judgments are affected by visual occlusion. J Manipulative Physiol Ther. 1996;19(4):250–256. [PubMed] [Google Scholar]
- 30.Bloem BR, Allum JH, Carpenter MG, Honeggar F. Is lower leg proprioception essential for triggering human automatic postural responses? Exp Brain Res. 2000;130(3):375–391. doi: 10.1007/s002219900259. [DOI] [PubMed] [Google Scholar]
- 31.Buckley JG, MacLellan MJ, Tucker MW, Scally AJ, Bennett SJ. Visual guidance of landing behaviour when stepping down to a new level. Exp Brain Res. 2008;184(2):223–232. doi: 10.1007/s00221-007-1096-8. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 33.Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25(1):33–39. doi: 10.1016/j.gaitpost.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 34.Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34(12):1970–1976. doi: 10.1177/0363546506290989. [DOI] [PubMed] [Google Scholar]
- 35.Drewes LK, McKeon PO, Paolini G et al. Altered ankle kinematics and shank-rear-foot coupling in those with chronic ankle instability. J Sport Rehabil. 2009;18(3):375–388. doi: 10.1123/jsr.18.3.375. [DOI] [PubMed] [Google Scholar]
- 36.Wikstrom EA, Bishop MD, Inamdar AD, Hass CJ. Gait termination control strategies are altered in chronic ankle instability subjects. Med Sci Sports Exerc. 2010;42(1):197–205. doi: 10.1249/MSS.0b013e3181ad1e2f. [DOI] [PubMed] [Google Scholar]
- 37.Lim EC, Tan MH. Side-to-side difference in joint position sense and kinesthesia in unilateral functional ankle instability. Foot Ankle Int. 2009;30(10):1011–1017. doi: 10.3113/FAI.2009.1011. [DOI] [PubMed] [Google Scholar]
- 38.Steenbergen B, van der Kamp J, Verneau M, Jongbloed-Pereboom M, Masters RS. Implicit and explicit learning: applications from basic research to sports for individuals with impaired movement dynamics. Disabil Rehabil. 2010;32(18):1509–1516. doi: 10.3109/09638288.2010.497035. [DOI] [PubMed] [Google Scholar]
- 39.Wulf G, Schmidt R. Variability of practice and implicit motor learning. J Exp Psychol Learn Mem Cogn. 1997;23(4):987–1006. [Google Scholar]
- 40.Jackson RC, Farrow D. Implicit perceptual training: how, when, and why? Hum Mov Sci. 2005;24(3):308–325. doi: 10.1016/j.humov.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 41.Willems T, Witvrouw E, Delbaere K, De Cock A, De Clercq D. Relationship between gait biomechanics and inversion sprains: a prospective study of risk factors. Gait Posture. 2005;21(4):379–387. doi: 10.1016/j.gaitpost.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 42.Chen HC, Ashton-Miller JA, Alexander NB, Schultz AB. Stepping over obstacles: gait patterns of healthy young and old adults. J Gerontol. 1991;46(6):M196–M203. doi: 10.1093/geronj/46.6.m196. [DOI] [PubMed] [Google Scholar]
- 43.Waddington G, Adams R. Football boot insoles and sensitivity to extent of ankle inversion movement. Br J Sports Med. 2003;37(2):170–174. doi: 10.1136/bjsm.37.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21(1):9–17. doi: 10.1097/00002508-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Bland JM, Altman DG. A note on the use of the intraclass correlation coefficient in the evaluation of agreement between two methods of measurement. Comput Biol Med. 1990;20(5):337–340. doi: 10.1016/0010-4825(90)90013-f. [DOI] [PubMed] [Google Scholar]