Abstract
Context
No consensus exists about the influence of compliance with neuromuscular training programs on reduction of the risk of anterior cruciate ligament (ACL) injury.
Objective
To systematically review and synthesize the published literature to determine if compliance with neuromuscular training is associated with reduced incidence of ACL injury in young female athletes.
Data Sources
We searched PubMed, SPORTDiscus, CINAHL, and MEDLINE for articles published from 1995 to 2010 using the key words anterior cruciate ligament prevention, ACL prevention, knee prevention, prospective knee prevention, neuromuscular training, and neuromuscular intervention.
Study Selection
Criteria for inclusion required that (1) the number of ACL injuries was reported, (2) a neuromuscular training program was used, (3) females were included as participants, (4) the study design was prospective and controlled, and (5) compliance data for the neuromuscular training program were provided.
Data Extraction
Extracted data included the number of ACL injuries, total number of participants per group, observation time period, number of participants who completed each session, number of sessions completed by an entire team, and number of total sessions. Attendance was calculated as the number of participants who completed each session converted into a percentage of the total number of participants. Intervention completion was calculated as the number of sessions completed by an entire team converted into a percentage of the total number of training sessions. These data were used to calculate an overall rate of compliance.
Data Synthesis
Six of 205 identified studies were included. Incidence rates of ACL injury were lower in studies with high rates of compliance with neuromuscular training than in studies with low compliance rates (incidence rate ratio = 0.27 [95% confidence interval = 0.07, 0.80]). Tertile analysis indicated rates of ACL injury incidence were lower in studies with high compliance rates than in studies with moderate and low compliance rates (incidence rate ratio = 0.18 [95% confidence interval = 0.02, 0.77]).
Conclusions
A potential inverse dose-response relationship exists between compliance with neuromuscular training and incidence of ACL injury. Attending and completing recommended neuromuscular sessions appears to be an important factor for preventing ACL injuries.
Key Words: knee, injury prevention, exercises
Key Points
Higher rates of compliance with neuromuscular training programs were associated with lower rates of anterior cruciate ligament (ACL) injury incidence among physically active young females.
A potential inverse dose-response relationship exists between compliance with neuromuscular training and the incidence of ACL injury in young female athletes.
Attending and completing prescribed neuromuscular training sessions seem to be integral components of preventing ACL injuries in young female athletes.
The incidence rate of anterior cruciate ligament (ACL) injuries among the general population is calculated to be 1 in 3000, and researchers have estimated that about 100 000 individuals injure their ACLs in the United States annually.1 Approximately 50 000 ACL reconstruction surgeries are performed annually in the United States,2 with conservative estimated average costs reported from $11 500 to 17 000 per case.3,4 In sum, the financial cost resulting from ACL injuries is likely near $3 billion annually.5 In addition to the financial cost, individuals who injure their ACLs experience premature osteoarthritis6,7 and reduced quality of life due to limited knee function.8
It is accepted that noncontact ACL injury rates are higher among females than males.9,10 Several factors have been identified to explain this sex disparity11–13; however, a single factor to predict these sex differences in injury rates has not been identified. Anatomic and hormonal factors, such as ACL circumference, joint laxity, and menstrual phase, have been discussed as increased risk factors for noncontact ACL injuries in females.14–16 However, modifying these particular risk factors is difficult if not impossible. In contrast, evidence indicates that neuromuscular risk factors are modifiable.17
Recently, neuromuscular risk factors, such as knee valgus position,18–20 quadriceps and hamstrings muscular activation,21,22 and trunk controls23 in dynamic motions have been proposed as risk factors for noncontact ACL injuries. To modify those risk factors, neuromuscular training intervention trials have been performed.3,24–33 Since the 1990s, large-scale prospective cohort studies have been performed to determine the effect of neuromuscular interventions targeted to reduce ACL, knee, and other lower extremity injuries. In the 1990s and early 2000s, researchers often used isolated training modalities in their neuromuscular training interventions, such as plyometric exercises or balance exercises or a combination of both.24–27,29 Recent neuromuscular interventions are aimed at decreasing not only ACL injuries but also other lower extremity injuries. This approach is more comprehensive and typically consists of combining different types of exercises, such as plyometrics, strengthening, stretching, and balance training. Examples of more recent comprehensive neuromuscular training programs include the Dynamic Neuromuscular Analysis training,17 Prevent Injury and Enhance Performance program,28,30 11,32 and 11+31 programs. In addition, certain components of these newly developed neuromuscular training programs include sport-specific exercises.29,32,33 Whereas the exercise selected for use in these programs is comprehensive, the program execution varies widely.
The reported mode, length, frequency, and duration of neuromuscular interventions have varied considerably in previous investigations, making it challenging to determine specific dose-response effects of neuromuscular training. In their systematic review of 5 large-scale randomized neuromuscular cohort studies aimed at decreasing noncontact ACL injury, Grindstaff et al34 found a 70% total risk reduction in participants in the intervention group compared with the control group. They concluded that neuromuscular interventions effectively reduce the risk of noncontact ACL injury.
Although they reported that neuromuscular interventions reduced the risk for noncontact ACL injury, Grindstaff et al34 did not examine compliance with the intervention, which is likely an important dimension of neuromuscular training efficacy. Compliance provides an indication of how many athletes completed the assigned intervention, revealing actual effects of neuromuscular training. No previous authors of meta-analysis studies have examined an association between rates of compliance and incidence of ACL injury or potential barriers to prescribed neuromuscular training. Therefore, the purpose of our meta-analysis was to investigate whether compliance of neuromuscular training plays a role in reducing the incidence of ACL injury in young female athletes. We hypothesized that neuromuscular training studies with high rates of compliance would have lower rates of ACL injury incidence in young female athletes.
METHODS
Literature Search
A literature search of the PubMed, SPORTDiscus, CINAHL, and Medline (1995–2010) databases was performed in February 2010. Key words were anterior cruciate ligament prevention, ACL prevention, knee prevention, prospective knee prevention, neuromuscular training, and neuromuscular intervention. Language was limited to English. A total of 195 studies was identified. An additional 10 studies were added as a result of cross-referencing. The following inclusion criteria were applied: (1) number of ACL injuries was reported, (2) a neuromuscular training intervention program was applied, (3) females were included as participants, (4) prospective controlled trial study design was employed, and (5) attendance and compliance information for the neuromuscular training program was collected. Abstracts and unpublished data were excluded.
Quality of Methodology Evaluation Methods
Methodologic quality of the included studies was analyzed using the Physiotherapy Evidence Database (PEDro) scale. This scale is a widely used measurement tool to rate the methodologic quality of a randomized clinical trial with moderate intraclass correlation coefficient values.35,36 Two reviewers (D.S. and J.M.M.) independently examined the methodologic quality of each study using the PEDro scale. Discrepancies between the reviewers were settled by arbitration and consensus.
Level of Evidence Assessment Methods
To evaluate the quality of the current analysis, the Centre of Evidence Based Medicine (CEBM)-Levels of Evidence chart was implemented.37 The CEBM-Level of Evidence assesses the quality of the included studies using a combination of numerical and letter scales, which further facilitates generating a recommendation grade for the current meta-analysis.
Data Extraction
Data regarding the number of ACL injury events, the number of athletes who attended intervention sessions, and the number of completed intervention sessions throughout the season were extracted from included studies. The rate of ACL injury was measured for both the control and intervention groups in each study. If the type of ACL injury was documented as either contact or noncontact, the number of each injury mechanism was documented, but the total number of ACL injuries was used to calculate the rate of ACL injury incidence. When the necessary attendance and completion data were not reported in the published manuscript, we sent an e-mail to the corresponding author listed in the original paper and asked compliance-related questions.
Data Analysis
Operational definitions used for the data analysis are listed in Table 1. An incidence rate ratio (IRR) was used to initially compare the incidence of ACL injury between intervention and control groups. This technique was employed because of its capability of comparing the ratio (control to intervention) of incidence rates in multiple groups. The IRR accounts for ACL injury rates in studies that include groups with different numbers of athletes and different observation timeframes. For the observation time periods, months were used as a unit. Specifically, we analyzed percentages and incidence rates of ACL injury for intervention groups in each study.
Table 1.
Operational Definitions for Data Analysis
| Operational Term |
Definition |
| ACL injury, % | Number of ACL injury events/total number of participants in the intervention or control groups |
| ACL injury incidence rates, athletes-months | Number of ACL events/total number of athletes in a group × observation time periods (months) |
| Attendance rates, % | Number of participants who completed the minimum amount of session criteria in the study/total number of participants in the intervention group |
| Completion rates, % | Number of sessions completed in the study/maximum sessions offered to the intervention group |
| Overall compliance rates, % | Attendance rate × completion rate |
| Incidence rate ratio | A meta-analysis method to compare the odds ratio of incidence rates between control and intervention groups in multiple studies |
Abbreviation: ACL, anterior cruciate ligament.
To compare the effects of high compliance and low compliance with neuromuscular training, we initially calculated a mean overall compliance rate of the selected studies. Based on the mean overall compliance rate (45.3%), studies with compliance rates that were more than the mean overall compliance rate were categorized as high (>45.3%), and those with compliance rates that were less than the mean were categorized as low (<45.3%). We used the IRR with 95% confidence interval (CI) to compare the rates of ACL injury incidence between intervention groups with high and low compliance rates. Subsequently, compliance rate was further separated into groups with high (>66.6%), moderate (33.3%–66.6%), or low (<33.3%) compliance. To compare the incidence rates between these tertile categorizations, IRRs with 95% CIs again were calculated.
RESULTS
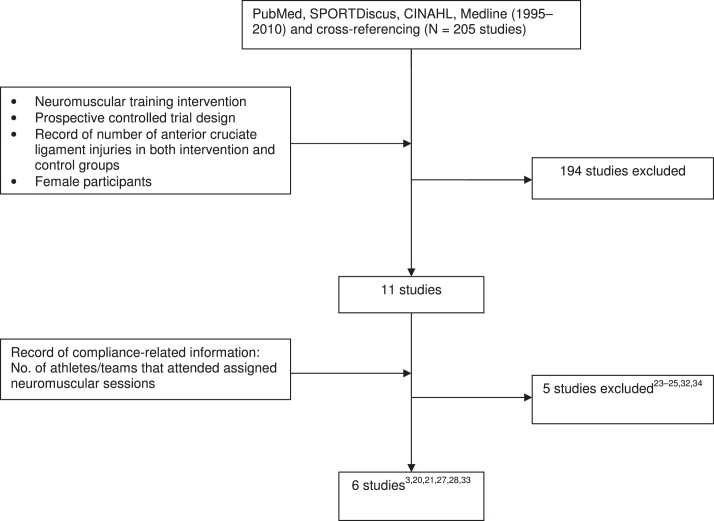
We identified 11 studies with the literature search. Four of the 11 studies included statements about compliance. We sent an e-mail to the corresponding authors of the other 7 studies to obtain the necessary attendance and completion data, but only authors25,32 of 2 of these studies provided sufficient compliance-related information (Figure 1). We excluded the other 5 studies28–30,37,38 from our analysis. Therefore, our final analysis included the 6 studies that met the inclusion criteria of our meta-analysis. Included study characteristics are summarized in Table 2. The mean PEDro scale was 4.7 for the 6 reviewed studies (Table 3). One study32 was rated as 7, whereas 1 study3 was classified as 3 in PEDro scale. The rates of ACL injury, attendance, completion, and overall compliance rates are summarized in Table 4. The attendance rates were reported on either an individual or team basis.
Figure 1.
Flow chart of the literature search.
Table 2.
Summary of Reviewed Studies
| Study Characteristic |
Study |
|||||
| Hewett et al,3 1999 |
Soderman et al,25 2000 |
Heidt et al,39 2000 |
Myklebust et al,26 2003 |
Steffen et al,32 2008 |
Kiani et al,33 2010 |
|
| Study design (CEBM level of evidence) | Prospective cluster cohort (2b) | Prospective randomized cluster cohort (2b)a | Prospective randomized (1b) | Prospective cross-over (2b) | Prospective randomized cluster cohort (1b) | Prospective cluster cohort (2b) |
| Sport | Volleyball, soccer, and basketball | Soccer | Soccer | Handball | Soccer | Soccer |
| Group size (athletes), n | C = 15 teams (463) | C = 6 teams (78) | C = 258 players | C = 60 teams (942) | C = 51 teams (947) | C = 49 teams (729) |
| I = 15 teams (366) | I = 7 teams (62) | I = 42 players | First I = 58 teams (855) | I = 58 teams (1073) | I = 48 teams (777) | |
| Second I = 52 teams (850) | ||||||
| Age, y | 14–18 | C mean = 20.5 ± 5.4 | 14–18 | Overall mean = 21–22 | Overall mean = 15.4 ± 0.8 | C mean = 15.0 (range, 13.0–17.6) |
| I mean = 20.4 ± 4.6 | I mean = 14.7 (range, 12.7–18.6) | |||||
| Intervention provider | Athletic trainers and physical therapists | Physical therapistsc | Athletic trainers | Physical therapists | Norwegian Football Association certified coaches and physical therapists | Physician, physical therapist, and coaches |
| Intervention Type | Stretching, plyometrics, and weight training | Balance with balance boards | Cardiovascular, plyometrics, strength, flexibility, agility, and sport-specific drills | Balance with mats and wobble boards | Core stability, balance, and plyometrics | Core strengthening, and balance |
| Length, min | 60–90 | 10–15 | 75 | 15 | 15 | 20–25 |
| Frequency | 3 d/wk | Each day for 30 d then 3 d/wk for rest of the season | 20 sessions (2 treadmill and 1 plyometric-based session per week) | 3 d/wk for 5–7 wk then 1 d/wk for rest of the season | 15 consecutive sessions then once a week for rest of the season | 2 d/wk for about 2 months then 1 d/wk for rest of the season |
| Duration | 6 wk | 6 mo | 7 wk | 5 mo | 7.5 mo | 9 mo |
| ACL injuries (mechanism), nb | C = 5 (5 noncontact) | C = 1 (no report) | C = 8 (no report) | First year (1998–1999) C = 29 (no report) | C = 5 (2 noncontact) | C = 5 (5 noncontact, 2 combined ACL and MM injury) |
| I = 2 (2 noncontact, 1 combined ACL and MCL injury) | I = 4 (no report, 1 combined ACL and MCL injury) | I = 1 (contact) | Second year (1999–2000) I = 23 (no report) | I = 4 (3 noncontact) | I = 0 | |
| Third year (2000–2001) I = 17 (no report) | ||||||
Abbreviations: ACL, anterior cruciate ligament; C, control; CEMB, Centre of Evidence Based Medicine; I, intervention; MCL, medial collateral ligament; MM, medial meniscus.
Although the study was a randomized controlled design, the follow-up rate was low (51.2%). Therefore, the level of evidence was rated as 2b.
No report indicates the researchers did not provide a description of the mechanism of ACL injury.
Physical therapists instructed the participants in the intervention, but the intervention was performed as a home program.
Table 3.
PEDro Scores of the Reviewed Studies
| PEDro Scalea |
Hewett et al3b |
Soderman et al25 |
Heidt et al39 |
Myklebust et al26b |
Steffen et al32 |
Kiani et al33b |
| 1. Eligibility criteria specified | Not scored | Not scored | Not scored | Not scored | Not scored | Not scored |
| 2. Random allocation of participants | No | Yes | Yes | No | Yes | No |
| 3. Allocation concealed | No | No | No | No | Yes | No |
| 4. Similar groups at baseline | No | Yes | No | No | No | Yes |
| 5. Blinding of participants | No | No | No | No | No | No |
| 6. Blinding of intervention providers | No | No | No | No | No | No |
| 7. Blinding of outcome assessors | No | No | Yes | Yes | Yes | Yes |
| 8. Outcomes obtained from 85% of participants | Yes | No | Yes | Yes | Yes | No |
| 9. Use of intent-to-treat analysis if protocol violated | Yes | No | Yes | Yes | Yes | No |
| 10. Between-groups statistical comparison | Yes | Yes | Yes | Yes | Yes | Yes |
| 11. Point measures and measures of variability | No | Yes | No | Yes | Yes | Yes |
| Total scores | 3 | 4 | 5 | 5 | 7 | 4 |
Abbreviation: PEDro, Physiotherapy Evidence Database.
The PEDro scale is optimized for evaluation of randomized control trials, thus the PEDro assessment score for the nonrandomized control should be interpreted with caution.
Indicates study was not a randomized trial.
Table 4.
Summary of Anterior Cruciate Ligament Injury, Attendance, Completion, and Overall Compliance Rates
| Study Year |
ACL Injury Rate,a % |
Attendance Rate,b % |
Completion Rate,b % |
Overall Compliance Rate,c % |
| Hewett et al,3 1999 | Control = 1.08 | Per individual = 67.8 | 66.6 | 45.2 |
| Intervention = 0.55 | ||||
| Soderman et al,25 2000 | Control = 1.28 | Per individual = 69.7 | 44.9 | 31.3 |
| Intervention = 6.45 | ||||
| Heidt et al,39 2000 | Control = 3.10 | Per individual = 100 | 100 | 100 |
| Intervention = 2.38 | ||||
| Myklebust et al,26 2003 | Control = 3.08 | |||
| First intervention = 2.69 | First intervention per team = 26 | First-year average = 47.1 | First-year average = 12.3 | |
| Second intervention = 2.00 | Second intervention per team = 29 | Second-year average = 47.1 | Second-year average = 13.7 | |
| Steffen et al,32 2008 | Control = 0.59 | Per team = 24.1 | 44.4 | 10.7 |
| Intervention = 0.69 | ||||
| Kiani et al,33 2010 | Control = 0.69 | Per team = 93.8 | 75 | 70.4 |
| Intervention = 0.00 |
Abbreviation: ACL, anterior cruciate ligament.
ACL injury rate = number of ACL injury events/participants in the group (control, intervention).
Indicates attendance and completion rates were extracted or calculated from original literature.
Overall compliance rate = attendance rate × the completion rate.
Reviewed Studies
Hewett et al.3
This research team used a prospective cluster study design and provided 6 weeks of neuromuscular training, which consisted of weight training, plyometrics, and flexibility, to 43 teams from 12 local area high school girls' volleyball, soccer, and basketball teams. Each neuromuscular training session lasted 60 to 90 minutes per session and took place 3 times per week for 6 weeks. The 15 girls' teams that received the intervention (6 weeks of neuromuscular training) comprised 366 athletes: 185 volleyball (50.5%), 97 soccer (26.5%), and 84 basketball (23.0%) players. The incidence of ACL injury was 0 per 1000 hours of athlete-exposure (AE) in volleyball, 0 per 1000 hours of AE in soccer, and 0.12 per 1000 hours of AE in basketball in the intervention group and was 0 per 1000 hours of AE in volleyball, 0.09 per 1000 hours of AE in soccer, and 0.13 per 1000 hours of AE in basketball in the control group. In this study, 67.8% (n = 248 of 366) of the athletes in the intervention group completed a minimum of 4 weeks (completion rate = 66.6%) of the neuromuscular training program sessions. Therefore, the overall compliance rate (0.678 × 0.666 = 0.452) was 45.2% in this study.
Soderman et al.25
In this prospective randomized controlled trial, the authors provided 10 to 15 minutes of balance training with balance boards to the intervention group (n = 121) for 6 months; the control group (n = 100) received no training. Balance training was performed every day for the first month and decreased to 3 days per week after the first month. They reported an incidence of ACL injury of 0.68 per 1000 hours of AE in the intervention group and 0.12 per 1000 hours of AE in the control group. The number of participants in the intervention group declined from 121 to 89 players due to nonathletic or research-related reasons. Ultimately, 69.7% (62 of 89) of participants completed the intervention session for a completion rate of 44.9% (35 minimum sessions, 78 maximum sessions). The attendance rates and completion rates produced an overall compliance rate (0.697 × 0.449 = 0.313) of 31.3%.
Heidt et al.39
This research group employed a 75-minute-long, custom speed and agility program to 42 randomly selected participants for 20 sessions over 7 weeks. Over 4 months, the ACL injury rate in the intervention group was 2.38% and 3.10% in the control group; they did not record exposure data. They reported a 100% rate of attendance and session completion. According to a staff member of the research group, the attendance of the female soccer players who were in the intervention group was monitored by their coaches, leading to a 100% overall compliance rate (1.0 × 1.0 = 1), which potentially could be inaccurate.
Myklebust et al.26
These researchers conducted a 3-year prospective crossover study; the first year was an observational year, whereas the 2 subsequent years were intervention periods. They recruited 1705 female handball players. A 15-minute session of balance exercises with mats and wobble boards was implemented 3 days per week in the initial 5 to 7 weeks and subsequently was reduced to once per week for the remainder of the handball season (approximately 5 months). During the study period, the ACL injury incidence rates were as follows: control group (1998–1999), 0.14 per 1000 hours of AE; intervention group (1999–2000), 0.13 per 1000 hours of AE; and intervention group (2000–2001), 0.09 per 1000 hours of AE. They reported that 26% of the teams in the intervention group fulfilled the criterion: participation in a minimum of 15 neuromuscular training sessions. Based on the frequency and duration of the intervention, the maximum number of neuromuscular training sessions was calculated as 30 to 34 sessions, which generated the session completion rate of 44.1% to 50%. Therefore, the overall compliance rate for the first year (0.26 × 0.441 = 0.115 to 0.26 × 0.50 = 0.13) ranged from 11.5% to 13%. In the second year, the attendance rate increased to 29%. Therefore, in the second year, the overall compliance rate was calculated in the same manner as the first year, which generated an overall compliance rate (0.29 × 0.441 = 0.128 to 0.29 × 0.50 = 0.145) of 12.8% to 14.5%.
Steffen et al.32
Using a cluster-randomized controlled trial (113 teams, 2100 players), this research team prescribed a 15-minute structured warm-up program, which consisted of core stability, balance, plyometrics, and hamstrings strengthening exercises, to 1073 young female soccer players (58 teams) for the first 15 consecutive sessions and once per week for the remaining 7.5 months. They documented an ACL injury incidence rate of 0.06 per 1000 hours of AE in the intervention group and 0.08 per 1000 hours of AE in the control group. The authors reported, “14 out of 58 teams in the intervention completed more than 20 prevention training sessions.” This yielded an attendance rate of 24.1%. The 45 total maximum sessions were calculated based on frequency and duration of the assigned intervention method, which was 15 consecutive sessions, and then reduced to once per week for the last 7.5 months. Based on the maximum number of sessions, the completion rate was calculated to be 44.4% (20 of 45). The combination of the attendance and completion rates yielded a 10.7% overall compliance rate (0.241 × 0.444 = 0.107).
Kiani et al.33
This prospective cluster cohort controlled trial (97 teams, 1506 players) included a 40-minute neuromuscular regimen consisting of a running warm-up, isometric contraction of lower extremity muscle groups, balance exercises with jump components, strengthening of the lower extremities, and core stability in 777 young soccer players (48 teams) 2 days per week for the 2-month preseason and once per week during the 6-month season. They reported ACL injury incidence rates of 0 per 1000 hours of AE in the intervention groups and 0.08 per 1000 hours of AE in the control group. The compliance scale consisted of 4 categories: less than 50%, at least 50%, at least 75%, or 100%. During the preseason, coaches of 3 teams rated compliance as less than 50%, 36 teams reported compliance of at least 75%, and 9 teams reported compliance at 100%. At the end of the season, only 3 teams reported compliance less than 75%. The 93.8% (45/48) attendance rate and the 75% completion rate generated a 70.4% overall compliance rate (0.938 × 0.75 = 0.704).
Data Synthesis
In summary, the overall compliance rates from the reviewed studies ranged from 10.7% to 100%. The mean overall compliance rate of the 6 studies was 45.3%. The reviewed studies initially were categorized into either high or low compliance based on the mean overall compliance rate. The overall compliance rates were higher in 3 studies3,33,39 and lower in 3 studies25,26,32 than the mean overall compliance rate. The results of the IRR meta-analysis indicated lower ACL incidence rates in the studies with high compliance rates than the studies with low compliance rates (IRR = 0.27, 95% CI = 0.07, 0.80; Figure 2).
Figure 2.
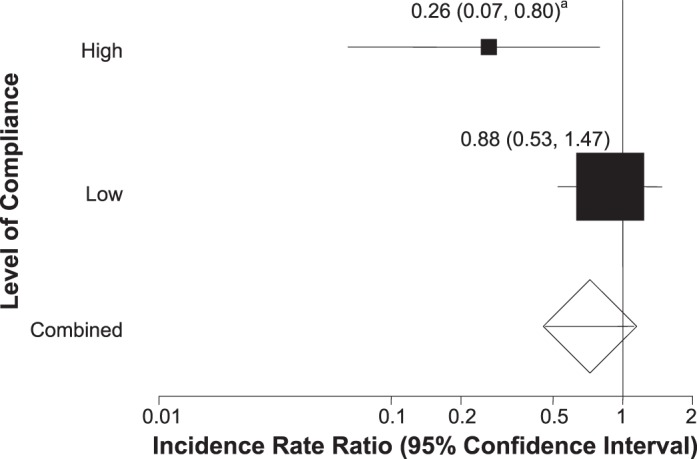
Incidence rate ratio among studies with high and low compliance rates. a Indicates the incidence rate ratios were lower in studies with high compliance rates than low compliance rates (incidence rate ratio = 0.26, 95% confidence intervals = 0.07, 0.80).
The 6 reviewed studies were further classified into one of the following categories based on the generated compliance rates: high (>66.6%), moderate (66.6%–33.3%), and low (<33.3%). Based on this categorization scheme, 2 studies showed high (>66.6%) compliance rates,33,39 and 1 study had moderate (66.6%–33.3%) compliance rates.3 Three studies demonstrated low (<33.3%) compliance rates.25,26,32 The IRR meta-analysis was applied to the 6 studies based on the 3 compliance-rate categories (high, moderate, low). The IRR meta-analysis demonstrated lower ACL incidence rates in the studies with high compliance rates than the studies with moderate and low compliance rates (IRR = 0.18, 95% CI = 0.02, 0.77; Figure 3).
Figure 3.
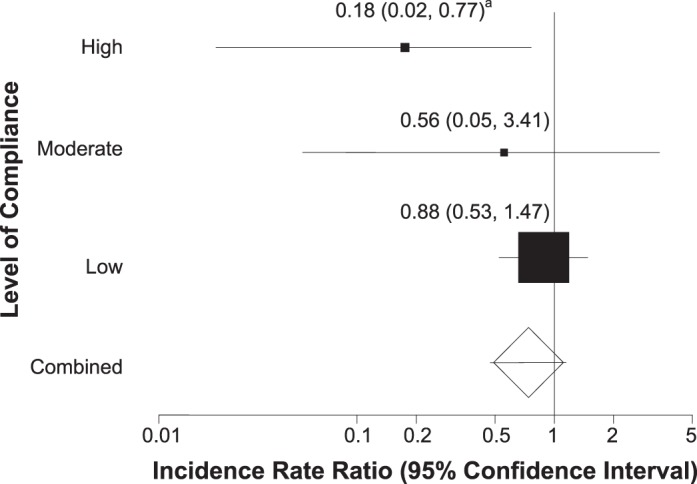
Incidence rate ratio in studies with high, moderate, and low compliance rates. a Indicates the incidence rate ratios were lower in studies with high compliance rates than moderate and low compliance rates (incidence rate ratio = 0.18, 95% confidence interval = 0.02, 0.77).
Evidence Synthesis
The CEBM level of evidence for each study is listed in Table 2. Two of the studies in our analysis were rated as evidence level 1b, whereas 4 studies were rated as evidence level 2b. Based on consistency of the results from the included studies, the strength of recommendation grade for the current evidence is B (consistent level 2 or 3 studies or extrapolations from level 1 studies).
DISCUSSION
The aim of this meta-analysis was to determine if compliance is associated with a reduced incidence of ACL injury in individuals participating in neuromuscular training programs. We hypothesized that neuromuscular training programs with high compliance rates would have lower incidence rates of ACL injury in young female athletes. Our results supported our hypothesis, demonstrating that an inverse relationship might exist between compliance and ACL injury; higher compliance rates signify a greater reduction in the incidence rates of ACL injury. Our findings may be the first to indicate a potential dose-response relationship between neuromuscular training compliance and incidence rates of ACL injury in large-scale prospective cohort studies. We observed a wide variety of overall compliance rates, ranging from 10.7% to 100%. In 4 of the 6 studies, the overall compliance rates were less than 50%.3,25,26,32 In addition, authors of 2 of the 6 studies reported less than 15% compliance, which is quite low.26,32
In the tertile analysis, the 2 studies with high compliance rates33,39 generated an IRR of ACL injury of 0.18 (95% CI = 0.02, 0.77), which was greater than the ratios of the studies with moderate (IRR = 0.56, 95% CI = 0.05, 3.41) and low (IRR = 0.88, 95% CI = 0.53, 1.47) compliance rates. These findings indicated that participants in the studies with moderate compliance rates had a risk of injuring their ACLs that was 3.1 times greater than participants in the studies with high compliance rates. Furthermore, participants in the studies with low compliance rates demonstrated a relative ACL injury risk that was 4.9 times greater than that of participants in the studies with high compliance rates. This information implies how vital it is to maintain a high compliance rate when using neuromuscular training interventions to reduce the incidence of ACL injury. More specifically, our results suggest that the overall compliance rate (attendance × completion) needs to be more than 66% to successfully reduce the risk of ACL injury.
Overall prophylactic effects of neuromuscular training interventions from all 6 reviewed studies resulted in an ACL IRR of 0.74 (95% CI = 0.47, 1.15), which was not different. However, half of the reviewed studies demonstrated low compliance rates, which weighted those studies proportionally heavier relative to the proportions of the studies with high and moderate compliance rates. Potentially, if more studies with high and moderate compliance rates were found and included in this analysis, the weight of studies would have been more evenly distributed throughout the study categories of high, moderate, and low compliance, which might have skewed the IRR results.
Authors of 2 studies33,39 demonstrated overall compliance rates of more than 66%. Kiani et al33 not only incorporated their interventions with their regular practice warm-up but made it similar to the existing warm-up method, which might have helped coaches to accept and understand the program. Although the intervention was 40 minutes long, the overall compliance rate was high (70.4%). They did not observe any ACL injury in the intervention group over the 8-month study. Conversely, 5 ACL injuries were confirmed in the control group, and all had noncontact mechanisms. This suggests that their neuromuscular training type, length, frequency, and duration were valid and effective in their focused population (mean age of the intervention group = 14.7 years) and sport (soccer). Heidt et al39 showed a high overall compliance rate despite not integrating the intervention with the warm-up. Instead, participants commuted to a gymnasium club to perform a custom speed and agility training program as a preseason workout. Selected participants were highly encouraged by their coaches to be involved in all the training sessions, which likely helped lead to the highest overall compliance rate (100%).
On the other hand, half of the studies25,26,32 did not attain at least 33% overall compliance rates. Steffen et al,32 whose study yielded the lowest overall compliance rate (10.7%) of the 6 studies, highlighted low compliance as a limitation and stated that completing only 15 sessions within a 3-month timeframe was not effective to show prophylactic effects for ACL injuries. They commented that a lack of available scheduling for the intervention program due to a short preseason, constant competitions, infrequent practice days, and occasional academic and holiday breaks might have contributed to the low compliance rate. In their study with a low compliance rate (31.3%), Soderman et al25 actually demonstrated higher ACL injury rates in the intervention (6.45%) than control (1.28%) group. The research team gave a balance board to all participants in the intervention group, and the training was explained thoroughly. However, they instructed the participants to perform the balance-board exercise at home instead of including it as a part of practice or team functions. The lack of supervision might have led to low motivation to adhere to the balance-board exercises, which might have led to a low compliance rate. The research team commented that maintaining high motivation for the prescribed intervention was a challenge. In addition, they introduced only single-component neuromuscular training (balance-board exercise) to the participants in the intervention group,25 a protocol that was also seen in another study with a low compliance rate.26 Myklebust et al26 taught a balance exercise using mats and wobble boards to the participants. A lack of variations in exercises might have resulted in boredom with the intervention, especially in young athletes. Reduced interest might lower the athlete's motivation to participate in the intervention, which might be a reason for the low compliance rates.25,26 The restricted time schedules, a lack of supervision, and limited neuromuscular training exercise variations might be major contributing factors to the low overall compliance rate.
Furthermore, the disparity between the high and low overall compliance rates might stem from additional benefits and supports in the studies with high compliance rates. Heidt et al,39 who demonstrated the highest overall compliance rate, used a custom speed and agility training program, which cost $360 for 21 sessions, as an intervention. However, the cost was waived for all participants in the intervention group. In their study, which had the second highest overall compliance rate, Kiani et al33 supplied monthly letters to maintain motivation and adherence to the neuromuscular training. Those incentive-based efforts might have played a key role in maintaining the participants' and coaches' motivations to continue the neuromuscular training, which might have been reflected in the high compliance rate. Conversely, in their study with a low compliance rate, Steffen at al32 stated “reduced motivation among coaches and players” was a limitation and could be a potential contributing factor for the low level of interest in participating in neuromuscular training. This raises the question of how preventive neuromuscular training can be implemented with a degree of high compliance without any incentive or additional supports in real athletic practices. Our analysis suggested that overall compliance rates need to be more than 66% to demonstrate the prophylactic effects of neuromuscular training. Thus, considering strategies to maintain athletes' and coaches' motivation and allocate time to perform a given neuromuscular training on a consistent basis is vital.
Large variances were observed among the neuromuscular training intervention, length, frequency, duration, and methods (Table 2). The intervention session ranged from 10 to 90 minutes in length, and all 3 studies25,26,32 that were categorized as having low compliance rates had relatively short (10 to 15 minutes) session lengths compared with the session lengths of other studies. The duration of the intervention varied from 6 weeks to 8 months. However, the 2 studies3,39 with intervention sessions that lasted more than 60 minutes had relatively shorter durations (6 weeks and 7 weeks), and the interventions were only used for their preseason because, when the season started, time for neuromuscular training was limited. With regard to intervention frequencies, a trend was observed in the studies performed in European countries. The authors of these studies tended to prescribe the intervention more frequently in earlier parts of the season, and the frequency of the intervention tended to decline as the seasons progressed to the more competitive portion (end-of-season tournaments and championships). Those researchers also incorporated interventions as a part of practices, usually with warm-ups.
Along with compliance issues, supervision of the neuromuscular training to ensure proper biomechanical technique should be considered. All investigators had intervention providers, who generally were athletic trainers, physical therapists, or coaches, teach the neuromuscular training to participants in the intervention groups (Table 2). Kiani et al33 had a physician to educate coaches and athletes in the instructional training (Table 2). Authors of 5 of the 6 studies provided instructional videos, written materials, and seminars to give specific biomechanical instructions to the intervention providers. Some investigators included seminars to train the intervention providers, giving theoretical background, practical implementation tips, and information on proper biomechanical techniques of the neuromuscular exercises.26,32 To ensure the abilities and performance of the intervention providers, authors of several studies had research team staff members inspect the instructors at the intervention site. Soderman et al25 instructed the participants to perform neuromuscular training at home instead of a team warm-up. Without supervision but with an emphasis on proper technique, limited or poor physiologic adaptation to the neuromuscular training exercises might result in no decrease in injury risk or possibly an increased rate of injury in intervention participants compared with control participants (Table 2).
Based on this comprehensive review of the literature, moderate to strong evidence exists to support the importance of compliance. Specifically, consistent attendance by involved athletes and commitment to the completion of sessions throughout the intervention period contribute to the effectiveness of the injury-prevention program. We recommend that clinicians make every effort to improve adherence to ACL injury-prevention programs to receive the desired prophylactic effects.
Our study had limitations. Authors of 5 studies28–30,37,38 who did not document sufficient information for attendance and intervention completion were not included in the analysis. The research team contacted the corresponding authors of each study to obtain necessary information for the overall compliance calculation. However, the compliance-related information from 2 studies28,30 was not adequate for our analysis, and authors of 3 studies29,37,38 never responded to our contacts. Inclusion of these studies could have influenced the result of the current analysis.
In 3 studies, researchers measured the attendance rates of each participant,3,25,39 whereas in the other 3 studies, investigators used the team as a unit to record their attendance (Table 4).26,32,33 The different measurement scales might not generate accurate attendance rates, which might influence the accuracy of the overall compliance rate. Measurement on an individual basis provides more reliable data than measurement on a team basis because determining how many athletes on each team in the intervention groups actually participated in the given intervention if attendance was calculated by team function is difficult.
In addition to different measurement scales for the attendance rates, compliance rate scales varied among reviewed studies because each group of researchers used its own protocol. Hewett et al3 used a protocol that required participants to complete more than 66.6% of the neuromuscular training session for inclusion in the data analysis. Soderman et al25 used 45% as the minimum rate of neuromuscular training completion. Differences among the minimum compliance rates for participant inclusion among investigations influenced the percentage of participants included in the data analysis of each study. However, to maintain the balance between the completed sessions and included participants, the overall compliance was calculated as a product of both attendance and completion rates.
Investigators in only 23,33 of the 6 studies documented the mechanism of the ACL injury. In general, neuromuscular training is designed to prevent noncontact ACL injuries. If the reported mechanisms of ACL injuries were contact, comparing the prophylactic effects of each intervention based on the compliance rate may not be valid. The research team contacted the corresponding authors of each study. However, researchers in only 132 of the 425,25,32,39 studies in which the mechanism of the injury was not documented responded with full information; therefore, the IRRs were calculated based on all ACL injuries and not just noncontact ACL injuries.
We focused on compliance. Therefore, our meta-analysis does not reflect the primary effects of neuromuscular training. Contents of the neuromuscular training were diverse and demonstrated wide variety among studies with high and low compliance rates. Because different types of neuromuscular training were prescribed to athletes in different sports and of different ages and because study designs varied, identifying which types of exercises are the most likely to prevent ACL injuries is difficult.
CONCLUSIONS
Among the 6 neuromuscular intervention studies with sufficient compliance information, our meta-analysis demonstrated that higher compliance rates were associated with lower rates of ACL injury incidence in physically active young females. Compared with participants in the studies with high compliance rates (IRR = 0.18, 95% CI = 0.02, 0.77), participants in the studies with moderate compliance rates (IRR = 0.56, 95% CI = 0.05, 3.41) showed a 3.1 times greater risk of sustaining ACL injuries. Moreover, participants in studies with low compliance rates (IRR = 0.88, 95% CI = 0.53, 1.47) demonstrated a 4.9 times greater relative risk of ACL injury than participants in the studies with high compliance rates (IRR = 0.18, 95% CI = 0.02, 0.77). This indicates a potential inverse dose-response relationship between neuromuscular training compliance and ACL injury incidence in young female athletes. The study findings implied that attending and completing the prescribed neuromuscular training sessions are integral components of ACL injury prevention. Incorporation of the neuromuscular training intervention in a warm-up or as a part of regular practices is a reasonable strategy to enhance compliance and ensure proper technique. In addition, finding a strategy to maintain adherence to neuromuscular training may be necessary to enhance compliance among athletes. Those strategies could lead to a more consistent outcome of ACL injury reduction and could promote safe and long-lasting athletic participation in physically active young females.
ACKNOWLEDGMENTS
This study was supported by Grant Nos. R01-AR049735, RO1-AR055563, and R01-AR056259 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases. We thank Timothy L. Uhl, PhD, PT, ATC, FNATA, for his guidance and support throughout this project.
REFERENCES
- 1.Huston LJ, Greenfield ML, Wojtys EM. Anterior cruciate ligament injuries in the female athlete: potential risk factors. Clin Orthop Relat Res. 2000;372:50–63. doi: 10.1097/00003086-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Emerson RJ. Basketball knee injuries and the anterior cruciate ligament. Clin Sports Med. 1993;12(2):317–328. [PubMed] [Google Scholar]
- 3.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 4.Gottlob CA, Baker CL, Jr, Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. [PubMed] [Google Scholar]
- 5.McLean SG, Beaulieu ML. Complex integrative morphological and mechanical contributions to ACL injury risk. Exerc Sport Sci Rev. 2010;38(4):192–200. doi: 10.1097/JES.0b013e3181f450b4. [DOI] [PubMed] [Google Scholar]
- 6.Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21(6):696–702. doi: 10.1016/j.arthro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Louboutin H, Debarge R, Richou J et al. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16(4):239–244. doi: 10.1016/j.knee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 9.Malone TR, Hardaker WT, Garrett WE, Feagin JA, Bassett FH. Relationship of gender to anterior cruciate ligament injuries in intercollegiate basketball players. J South Orthop Assoc. 1993;2(1):36–39. [Google Scholar]
- 10.Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34(2):86–92. [PMC free article] [PubMed] [Google Scholar]
- 11.Moul JL. Differences in selected predictors of anterior cruciate ligament tears between male and female NCAA Division I collegiate basketball players. J Athl Train. 1998;33(2):118–121. [PMC free article] [PubMed] [Google Scholar]
- 12.Goshima K, Kitaoka K, Nakase J, Takahashi R, Tsuchiya H. Clinical evidence of a familial predisposition to anterior cruciate ligament injury. Br J Sports Med. 2011;45(4):350–351. [Google Scholar]
- 13.Hashemi J, Mansouri H, Chandrashekar N, Slauterbeck JR, Hardy DM, Beynnon BD. Age, sex, body anthropometry, and ACL size predict the structural properties of the human anterior cruciate ligament. J Orthop Res. 2011;29(7):993–1001. doi: 10.1002/jor.21245. [DOI] [PubMed] [Google Scholar]
- 14.Dienst M, Schneider G, Altmeyer K et al. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007;127(4):253–260. doi: 10.1007/s00402-006-0177-7. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Zazulak BT, Myer GD. Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. Am J Sports Med. 2007;35(4):659–668. doi: 10.1177/0363546506295699. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhari AM, Zelman EA, Flanigan DC, Kaeding CC, Nagaraja HN. Anterior cruciate ligament-injured subjects have smaller anterior cruciate ligaments than matched controls: a magnetic resonance imaging study. Am J Sports Med. 2009;37(7):1282–1287. doi: 10.1177/0363546509332256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hewett TE, Myer GD, Ford KR, Slauterbeck JR. Dynamic neuromuscular analysis training for preventing anterior cruciate ligament injury in female athletes. Instr Course Lect. 2007;56:397–406. [PubMed] [Google Scholar]
- 18.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417–422. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford KR, Shapiro R, Myer GD, Van Den Bogert AJ, Hewett TE. Longitudinal sex differences during landing in knee abduction in young athletes. Med Sci Sports Exerc. 2010;42(10):1923–1931. doi: 10.1249/MSS.0b013e3181dc99b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR. Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19(1):3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Urabe Y, Kobayashi R, Sumida S et al. Electromyographic analysis of the knee during jump landing in male and female athletes. Knee. 2005;12(2):129–134. doi: 10.1016/j.knee.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 24.Caraffa A, Cerulli G, Projetti M, Aisa G, Rizzo A. Prevention of anterior cruciate ligament injuries in soccer: a prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 25.Soderman K, Werner S, Pietila T, Engstrom B, Alfredson H. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc. 2000;8(6):356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 26.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Wedderkopp N, Kaltoft M, Holm R, Froberg K. Comparison of two intervention programmes in young female players in European handball: with and without ankle disc. Scand J Med Sci Sports. 2003;13(6):371–375. doi: 10.1046/j.1600-0838.2003.00336.x. [DOI] [PubMed] [Google Scholar]
- 28.Mandelbaum BR, Silvers HJ, Watanabe DS et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 29.Petersen W, Braun C, Bock W et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125(9):614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 30.Gilchrist J, Mandelbaum BR, Melancon H et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 31.Soligard T, Myklebust G, Steffen K et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469. doi: 10.1136/bmj.a2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football: a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18(5):605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 33.Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Michaelsson K, Byberg L. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010;170(1):43–49. doi: 10.1001/archinternmed.2009.289. [DOI] [PubMed] [Google Scholar]
- 34.Grindstaff TL, Hammill RR, Tuzson AE, Hertel J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: a numbers-needed-to-treat analysis. J Athl Train. 2006;41(4):450–456. [PMC free article] [PubMed] [Google Scholar]
- 35.Moseley AM, Sherrington C, Elkins MR, Herbert RD, Maher CG. Indexing of randomised controlled trials of physiotherapy interventions: a comparison of AMED, CENTRAL, CINAHL, EMBASE, hooked on evidence, PEDro, PsycINFO and PubMed. Physiotherapy. 2009;95(3):151–156. doi: 10.1016/j.physio.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 36.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 37.Pfeiffer RP, Shea KG, Roberts D, Grandstrand S, Bond L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006;88(8):1769–1774. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 38.Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heidt RS, Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]