Abstract
Excess of adiposity is a risk factor for coronary artery disease, but it remains unclear if the distribution of fat is an effect modifier or if the risk is mediate by hypertension, diabetes and dyslipidemia. We investigated the association of central in addition to general obesity with coronary artery disease (CAD). A case-control study was conducted in 376 patients, aged 40 years or more, with chronic coronary disease, undergoing elective coronary angiography. Excess of adiposity was evaluated by the Body Mass Index (BMI), waist circumference, waist-hip ratio, and neck circumference. Cases (n=155) were patients referred for coronary angiography with at least 50% of coronary stenosis in at least one epicardial vessels or their branches, with diameter greater than 2.5 mm. Controls (n=221) were patients referred for coronary angiography without significant coronary disease. Odds ratios and 95%CI for significant coronary stenosis were calculated using multiple logistic regression, controlling for age, sex, years at school, smoking, hypertension, HDL-cholesterol, diabetes mellitus, and an adiposity index. There was a predominance of men and individuals older than 50 years among cases. The waist-hip ratio increased four times the chance of CAD, even after the control for confounding factors, including BMI. Neck circumference above the 90th Percentile doubled the chance of CAD, after adjustment for traditional risk factors. Neck circumference and waist-hip ratio are independent predictors of CAD, even taking into account traditional risk factors for CAD. These findings highlight the need of anthropometric assessment among patients with suspected coronary artery disease.
Keywords: Obesity, central obesity, abdominal obesity, coronary artery disease, coronary angiography
Introduction
Excess of adiposity is in the origin of coronary heart disease (CHD), since it is closely associated to the development of hypertension, dyslipidemia, and diabetes mellitus [1]. The paradoxical protection of obesity for CHD or cardiovascular disease (CVD) has been described [2,3], but it is not fully understood [4]. Beyond other potential explanations, emerged the low discriminating power of body mass index, which is a commonly employed tool for measurement of obesity [5].
Body mass index was not associated with mortality in patients submitted to coronary angiography [6]. On the other hand, central obesity was an independent predictor of vascular mortality [7]. Waist-hip ratio, an indicator of visceral adiposity, is associated with coronary artery disease, regardless of the body mass index [8,9]. Neck circumference is another indicator of visceral obesity that has been more strongly associated with insulin resistance than waist circumference [10]. Its association with extent and severity of coronary disease has not been established to date. The aim of this study was to evaluate the independent association of anthropometric indexes of central and overall obesity with the severity and extension of coronary artery disease measured by quantitative coronary angiography.
Material and methods
This case-control study included 376 men and women, aged 40 years or over, with suspected CHD who were referred for coronary angiography. They were enrolled at the Catheterization Laboratory of the Hospital de Clínicas de Porto Alegre, which is reference for secondary health care and for patients from our hospital. Cases were patients referred for elective coronary angiography for diagnostic purposes, who had significant coronary artery disease defined by the presence of stenosis equal or greater than 50% in a major epicardial coronary artery - left anterior descendent, circumflex or right coronary artery - or their branches with or at least 2.5 mm of diameter. They were referred due to class I to II stable angina or an evidence of ischemia in noninvasive testing. Patients with previous revascularization by percutaneous or surgical interventions, dilated or hypertrophic cardiomyopathy, chronic renal disease, hepatic cirrhosis, previous or current cancer, major pelvic surgery, psychiatric disease were excluded. Control patients were those who did not present significant coronary artery disease at coronary angiography. The study was approved by the Ethics Committee of the Hospital de Clinicas de Porto Alegre, which is accredited by the Office of Human Research Protections as an Institutional Review Board, and all participants signed an informed consent to participate.
Traditional cardiovascular risk factors, socioeconomic, demographic, lifestyle and previous morbidity were assessed using a standardized questionnaire, through interviews conducted by trained research assistants. Blood pressure and anthropometric measurements were assessed on the day of enrollment, prior to the procedure. The studied variables were: age, categorized as 40-59, 60-69 or ≥70 years; smoking, defined by the number of packs of cigarettes smoked per year (0, <20 or ≥20 packs/year) [11]; abusive consumption of alcohol (≥30 among men, and ≥15 g ethanol/day for women) [12], physical activity, determined using the International Physical Activity Questionnaire (IPAQ, short version) [13], and by characterizing sedentary for those whose energetic expenditure was lower than 200 kcal/day.
Standardized blood pressure measurements were obtained using an automatic device (OMRON HEM-705 CP;OMRON, Matsuzaka, Mie, Japan), with the patient in sitting position and the average of three measurements was used in the analysis. Hypertension was defined by systolic blood pressure superior or equal to 140 mmHg, or diastolic blood pressure superior to or equal to 90 mmHg, or use of blood pressure-lowering drugs.
A nutritionist performed the anthropometric assessment with the patient wearing light clothing, without shoes, and the average of three measurements was used in the analysis. Weight and height were measured using a Filizola scale with stadiometer, model 110CH, with a capacity of 150 kg and precision of 100 g and 0.1 cm. Circumferences were measured using an inelastic tape with one millimetre precision. Waist circumference was measured at the midpoint between the inferior costal margin and the upper iliac crest whereas the hip circumference was obtained at the level of the femoral trochanters [14], and the neck circumference was measured below the cricoid cartilage, and afterwards, at the level of the mid cervical spine.
Overall obesity was determined by the body mass index [weight (kg)/height (m)2], categorized as < 25, 25-29 or ≥ 30 kg/m2 [15], and central obesity was characterized by waist-hip ratio (categorized as <0.90, 0.90-0.94 or ≥0.95 for men, and <0.80, 0,80-0,84 or ≥0.85 for women) and waist circumference (<94, 94-101 or ≥102 cm for men and <80, 80-87 or ≥ 88 cm, for women) [15]. In the absence of previously defined cut-off points, the neck circumference was defined by values above the 90th Percentile, separately for men (41.6 cm) and women (37.0 cm). Laboratory measurements were done with the patient fasting for 12 hours and approximately 10 millilitres of blood were collected from the femoral artery through the sheath, immediately after its insertion during the cardiac catheterization, and previously to the heparin administration. Diabetes mellitus was diagnosed by fasting glucose ≥126 mg/dL or use of anti-diabetic agents [16]. Dyslipidemia was diagnosed by total cholesterol ≥200 mg/dL, LDL-cholesterol ≥130 mg/dL, HDL cholesterol <40 mg/dL, for men, and <50 mg/dL, for women, and triglycerides ≥150mg/dL [17] or use of lipid-lowering medication.
Coronary angiography was performed through transfemoral access, according to the Seldinger technique, using Siemens equipment - Axion Artis, by experienced interventional cardiologists. The diagnosis of significant lesion was established by quantitative analysis of major epicardial vessels - left main coronary artery, anterior descending artery, and circumflex and right coronary arteries - also, in vessels which diameter is superior or equal to three millimeters - diagonal branches, obtuse marginals, posterolateral branch and posterior descendent artery. A subsample was evaluated independently by two interventional cardiologists and the control of quality was checked by a third physician. Stenosis was detected, as well as the percentage of stenosis in relation to the diameter, through quantitative analysis. Among the cases with significant coronary artery disease on the angiography, the extent of involvement was determined by the number of vessels, categorized as 0, 1 or 2 to 4.
Sample size calculation and statistical analysis
The study was designed to have a sample size sufficient to detect an odds ratio of at least 1.9 with p α=0.05 and power of 80%, assuming the prevalence of obesity of 30% in the control group and 45% among cases, with a ratio between cases and controls of 1:1.5. Thus, it should be necessary to study 146 cases and 218 controls. The statistical analysis of parameters distribution between cases and controls was tested by the Chi-square test. Associations were analyzed through multiple logistic regression using the Statistical Package for Social Sciences (SPSS, version 17.0, SPSS Inc., Chicago, USA) to calculate the odds ratio (OR) and the 95% confidence interval (95% CI), with statistical significance established by the likelihood ratio test. The magnitude of the association between anthropometric indices and significant coronary disease was determined by calculating the non-adjusted and the adjusted OR for the confounding factors at three levels: (1) age, (2) age, sex and education and (3) level 2 plus variables found in the bivariate analysis as potential confounders, using P value ≤0.2. The adjustment of the multivariate models was analyzed by the multicollinearity between the explanatory variables in each model, tested in the correlation matrix, and the Goodness-of-fit test of Hosmer-Lemeshow.
Results
Among 1005 patients undergoing elective coronary angiography, 155 cases and 221 controls were enrolled. The main reasons for exclusion were: 35.3% of the patients had previous coronary artery angioplasty or by-pass surgery, 5.5% had chronic kidney disease or cirrhosis, 3.4% previous or current cancer, 0.8% had previous hip bone or femur surgery, 0.5% due to mental disorders, 8.3% were unable to perform anthropometry, 7.2% for other reasons, and 0.8% refused to participate.
Cases were predominantly males, older (59.7 ±9.1 vs. 57.3 ±9.5 years; P=0.01), and had higher prevalence of obesity and diabetes than controls (Table 1). Significant coronary artery disease was more frequent among individuals aged 50-59 and 70 years or over. These patients had three times the risk of significant coronary disease than those less than 50 years old. Higher waist-hip ratio was associated with a 3.5 fold increased risk of significant CAD. Other anthropometric indices of obesity were not associated with significant coronary artery disease in the bivariate analysis (Table 1).
Table 1.
Characteristics of patients with and without significant coronary disease [n (%)]
| Cases (n = 155) | Controls (n = 221) | OR (95%CI) | P value | |
|---|---|---|---|---|
| Males | 114 (73.5) | 128 (57.9) | 2.0 (1.3-3.2) | 0.002 |
| Age (years) | 0.004 | |||
| 40-49 | 19 (12.3) | 60 (27.1) | 1.0 | |
| 50-59 | 66 (42.6) | 73 (33.0) | 2.9 (1.5-5.3) | |
| 60-69 | 47 (30.3) | 66 (29.9) | 2.2 (1.2-4.3) | |
| ≥70 | 23 (14.8) | 22 (10.0) | 3.3 (1.5-7.2) | |
| Skin color (non-white) | 58 (37.4) | 75 (33.9) | 1.2 (0.8-1.8) | 0.5 |
| Years at school | 0.12 | |||
| 0-4 | 49 (31.6) | 87 (39.5) | 1.0 | |
| 5-8 | 67 (43.2) | 95 (43.2) | 1.3 (0.8-2.0) | |
| ≥9 | 39 (25.2) | 38 (17.3) | 1.8 (1.0-3.2) | |
| Sedentary | 116 (74.8) | 154 (69.7) | 1.3 (0.8-2.1) | 0.3 |
| Abusive consumption of alcohol | 21 (13.5) | 32 (14.5) | 0.9 (0.5-1.7) | 0.8 |
| Smoking (packs-year) | 0.11 | |||
| 0 | 56 (36.1) | 75 (33.9) | 1.0 | |
| 1-19 | 31 (20.0) | 65 (29.4) | 0.6 (0.4-1.1) | |
| ≥20 | 68 (43.9) | 81 (36.7) | 1.1 (0.7-1.8) | |
| Hypertension | 130 (83.9) | 174 (78.7) | 1.4 (0.8-2.4) | 0.2 |
| Diabetes mellitus | 39 (25.3) | 36 (16.4) | 1.7 (1.04-2.9) | 0.03 |
| Total Cholesterol ≥200 mg/dL | 47 (30.5) | 62 (28.2) | 1.1 (0.7-1.8) | 0.6 |
| LDL-cholesterol ≥130 mg/dL | 35 (23.8) | 52 (24.1) | 1.0 (0.6-1.6) | 0.9 |
| HDL-cholesterol* | 95 (61.7) | 112 (50.9) | 1.6 (1.02-2.4) | 0.04 |
| Triglycerides ≥150 mg/dL | 61 (39.6) | 68 (30.9) | 1.5 (1.0-2.3) | 0.08 |
| Body Mass Index (kg/m2) | 0.3 | |||
| <25.0† | 40 (26.0) | 73 (33.0) | 1.0 | |
| 25.0-29.9 | 80 (51.9) | 105 (47.5) | 1.4 (0.9-2.3) | |
| ≥30.0 | 34 (22.1) | 43 (19.5) | 1.4 (0.8-2.6) | |
| Waist circumference (cm) ‡ | 0.06 | |||
| <80 / <94† | 51 (32.9) | 49 (22.2) | 1.0 | |
| 80-87.9 / 94-101.9 | 43 (27.7) | 77 (34.8) | 0.5 (0.3-0.9) | |
| ≥88 / ≥102 | 61 (39.4) | 95 (43.0) | 0.6 (0.4-1.02) | |
| Waist-hip ratio‡ | 0.02 | |||
| <0.80 / <0.90† | 5 (3.2) | 23 (10.4) | 1.0 | |
| 0.80-0.84 / 0.90-0.94 | 21 (13.5) | 39 (17.6) | 2.5 (0.8-7.5) | |
| ≥0.85 / ≥0.95 | 129 (83.2) | 159 (71.9) | 3.7 (1.4-10.1) | |
| Neck circumference ≥P90 | 20 (9.0) | 18 (11.8) | 1.3 (0.7-2.6) | 0.4 |
Cuttoff points for men <40mg/dL and for women <50 mg/Dl;
Reference category;
Cutoff point established separately for men and women.
Table 2 presents the odds ratios of different anthropometric indices for significant coronary stenosis, after the adjustment for the full setting of confounding variables. Waist-hip ratio and neck circumference were associated with significant coronary stenosis, even after control for BMI. Body mass index presented a dose response relationship with CAD, after fully adjustment for confounding factors, including waist-hip ratio.
Table 2.
Association of anthropometric indices and significant coronary stenosis adjusted for age and other confounding factors [OR (95% CI)]
| Model 1* | Model 2* | |
|---|---|---|
| Body mass index (kg/m2) | ||
| <25† | 1.0 | 1.0¶ |
| 25-29 | 1.2 (0.7-2.0) | 1.7 (1.0-3.0) |
| ≥30 | 1.3 (0.7-2.4) | 2.3 (1.1-4.7) |
| P value | 0.7 | 0.03** |
| Waist circumference (cm)‡ | ||
| <80 / <94† | 1.0 | 1.0§ |
| 80-84.9 / 94-101.9 | 0.5 (0.3-0.9) | 0.7 (0.4-1.4) |
| ≥85 / ≥102 | 0.6 (0.4-1.0) | 1.1 (0.5-2.6) |
| P value | 0.05 | 0.2 |
| Waist-hip ratio‡ | ||
| <0.80/<0.90† | 1.0 | 1.0§ |
| 0.80-0.84/0.90-0.94 | 2.5 (0.8-7.6) | 2.4 (0.7-8.1) |
| ≥0.85/≥0.95 | 3.5 (1.3-9.6) | 4.0 (1.3-12.1) |
| P value | 0.04 | 0.03 |
| Neck Circumference‡ | ||
| <P90† | 1.0 | 1.0¶ |
| ³ P90 | 1.6 (0.8-3.3) | 2.4 (1.1-5.3) |
| P value | 0.15 | 0.04** |
Model 1: adjusted for age; Model 2: adjusted for age, sex, years at school, smoking, hypertension, HDL-cholesterol and diabetes mellitus;
Reference category;
Cutoff point established separately for men and women;
Additionally adjusted for BMI;
Additionally adjusted for WHR;
P for trend.
Figures 1 and 2 show that there were marked differences in neck circumference and waist-hip ratio between men and women. However, neck circumference and WHR were not associated with the extent of coronary artery disease, as measured by the number of vessels with at least 50% stenosis.
Figure 1.
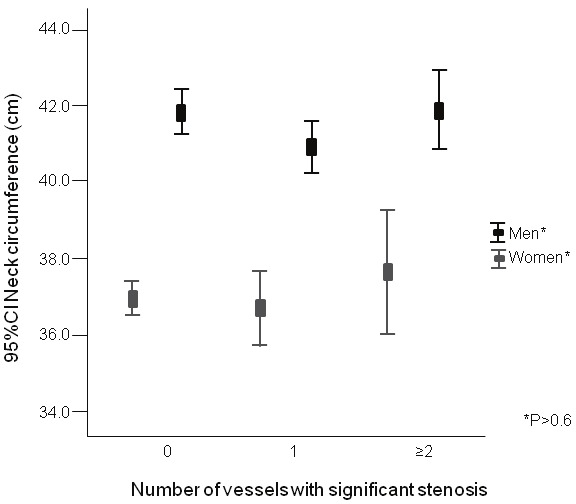
Neck circumference according to the number of coronary arteries with significant stenosis (CAD; at least one coronary artery with ≥50% diameter stenosis involving either on major epicardial vessels or any branches with >2.5 mm diameter).
Figure 2.
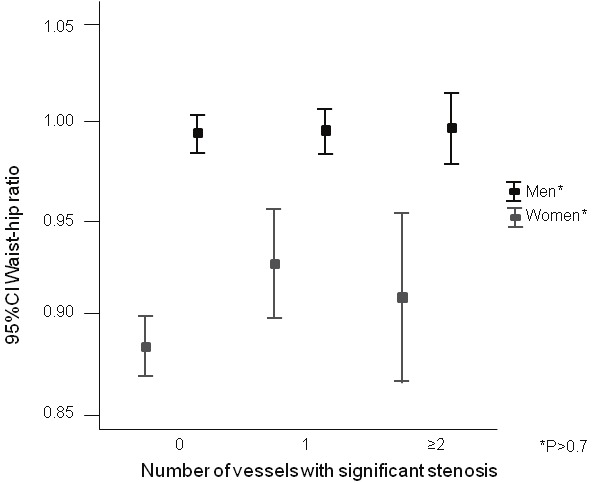
Waist-hip ratio according to the number ofcoronary arteries with significant stenosis (CAD; atleast one coronary artery with ≥50% diameter stenosisinvolving either on major epicardial vessels or anybranches with >2.5 mm diameter).
Discussion
In this case-control study, conducted in patients referred for elective coronary angiography, we identified that central obesity, assessed by the waist-hip ratio, and the accumulation of fat in the neck are independent risk factors for coronary artery disease. These associations showed to be independent of overall excess of adiposity, represented by the BMI, and of other traditional risk factors for atherosclerosis. BMI was an independent risk factor for CAD as well.
The association between excess of adiposity - not mediate by the classic risk factors, particularly hypertension, lipid abnormalities and diabetes - and CAD has been debated. In epidemiological studies, the risk has been mostly ascribed to the traditional and intermediate risk factors and not to obesity [18].
In studies with coronary angiography the findings have been controversial [19,20]. Some studies failed to identify independent associations between excess of adiposity, identified by BMI, and CAD outcomes [21,22]. On the other hand, in other studies an independent association emerged [19], particularly for the central distribution of adiposity [23]. Our findings demonstrate that the excess of obesity, determined by the overall distribution of fat (BMI), by central obesity (WHR) and by deposition of fat in the neck were all risk factors for CAD diagnosed by coronary angiography, independently of traditional risk factors and of the other anthropometric indexes. Large neck circumference has been associated with metabolic risk factors [24], blood pressure [25], and CHD [26]. To the best of our knowledge, this is the first description of the association between neck circumference and CAD diagnosed by coronary angiography.
The independent risk of excess of adiposity, independently of its distribution (overall, in the abdomen and in the neck), for CAD should therefore be explained by mechanisms independent of traditional risk factors. Other risk factors for CAD not controlled in our study, such as obstructive sleep apnea [27], could be the mediators of such risk. In addition, mechanisms linking directly excess of fat with CAD could be responsible for the association. Inflammatory activity generated by the fat tissue [28], release of other mediators [29] could be another mechanisms linking directly excess of fat with CAD. Epicardial and subcutaneous adipose tissue as sources of inflammatory mediators [30] and perivascular adipose tissue proinflammatory phenotype [31,32] may have augmented interaction through a complex process affects not only inflammation, but smooth muscle cell proliferation, and vasoreactivity [33,34].
There are some limitations that deserve to be mention. The lack of a temporal line linking neck circumference and coronary artery disease precludes establishing a causal relationship. Based on other studies, it is possible to link neck circumference with sleep apnea [35] and significant coronary artery disease preceding coronary artery disease. The absent association of number of vessels with significant stenosis with neck circumference reduced the force of an argument in favor of a causal relationship. However, as previously discussed, there are several potential mechanisms that could explain this relationship [36,37] and, barely, this would be linear. On the other hand, the selection of controls among patients submitted to coronary angiography allows infer that they come from the same population, precluding selection bias.
In conclusion, excess of adiposity, centrally distributed or not, and accumulated in the neck, is a risk factor for significant CAD. This risk is not explained by traditional risk factors for CAD, suggesting that other consequences of excess or obesity may mediate the risks for CAD.
Acknowledgement
This study was funded, in part, by National Counsel of Technological and Scientific Development (CNPq), CAPES (Coordination for the Improvement of Higher Education Personnel), Laboratório Weinmann (Laboratory), and FIPE-Hospital de Clínicas de Porto Alegre, RS, Brazil.
References
- 1.Logue J, Murray HM, Welsh P, Shepherd J, Packard C, Macfarlane P, Cobbe S, Ford I, Sattar N. Obesity is associated with fatal coronary heart disease independently of traditional risk factors and deprivation. Heart. 2011;97:564–568. doi: 10.1136/hrt.2010.211201. [DOI] [PubMed] [Google Scholar]
- 2.Uretsky S, Messerli FH, Bangalore S, Champion A, Cooper-Dehoff RM, Zhou Q, Pepine CJ. Obesity paradox in patients with hypertension and coronary artery disease. Am J Med. 2007;120:863–870. doi: 10.1016/j.amjmed.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Shirzad M, Karimi A, Dowlatshahi S, Ahmadi SH, Davoodi S, Marzban M, Movahedi N, Abbasi K, Fathollahi MS. Relationship Between Body Mass Index and Left Main Disease: The Obesity Paradox. Archives of Medical Research. 2009;40:618–624. doi: 10.1016/j.arcmed.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, Narayan KM, Williamson DF. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Corral A, Somers VK, Sierra-Johnson J, Jensen MD, Thomas RJ, Squires RW, Allison TG, Korinek J, Lopez-Jimenez F. Diagnostic performance of body mass index to detect obesity in patients with coronary artery disease. European Heart Journal. 2007;28:2087–2093. doi: 10.1093/eurheartj/ehm243. [DOI] [PubMed] [Google Scholar]
- 6.Khattab AA, Daemen J, Richardt G, Rioux P, Amann FW, Levy R, Horvath IG, Teles RC, Ordoubadi F, Pieters M, Wittebols K, Stoll HP, Serruys PW. Impact of body mass index on the one-year clinical outcome of patients undergoing multivessel revascularization with sirolimuseluting stents (from the Arterial Revascularization Therapies Study Part II) Am J Cardiol. 2008;101:1550–1559. doi: 10.1016/j.amjcard.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 7.Hoefle G, Saely CH, Aczel S, Benzer W, Marte T, Langer P, Drexel H. Impact of total and central obesity on vascular mortality in patients undergoing coronary angiography. Int J Obes (Lond) 2005;29:785–791. doi: 10.1038/sj.ijo.0802985. [DOI] [PubMed] [Google Scholar]
- 8.Canoy D, Boekholdt SM, Wareham N, Luben R, Welch A, Bingham S, Buchan I, Day N, Khaw KT. Body fat distribution and risk of coronary heart disease in men and women in the European prospective investigation into cancer and nutrition in Norfolk cohort - A population-based prospective study. Circulation. 2007;116:2933–2943. doi: 10.1161/CIRCULATIONAHA.106.673756. [DOI] [PubMed] [Google Scholar]
- 9.Page JH, Rexrode KM, Hu F, Albert CM, Chae CU, Manson JE. Waist-Height Ratio as a Predictor of Coronary Heart Disease Among Women. Epidemiology. 2009;20:361–366. doi: 10.1097/EDE.0b013e31819f38f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang L, Samarasinghe YP, Kane P, Amiel SA, Aylwin SJ. Visceral adiposity is closely correlated with neck circumference and represents a significant indicator of insulin resistance in WHO grade III obesity. Clin Endocrinol (Oxf) 2010;73:197–200. doi: 10.1111/j.1365-2265.2009.03772.x. [DOI] [PubMed] [Google Scholar]
- 11.Bernaards CM, Twisk JW, Snel J, Van Mechelen W, Kemper HC. Is calculating pack-years retrospectively a valid method to estimate lifetime tobacco smoking? A comparison between prospectively calculated pack-years and retrospectively calculated pack-years. Addiction. 2001;96:1653–1661. doi: 10.1046/j.1360-0443.2001.9611165311.x. [DOI] [PubMed] [Google Scholar]
- 12.Moreira LB, Fuchs FD, Moraes RS, Bredemeier M, Cardozo S, Fuchs SC, Victora CG. Alcoholic beverage consumption and associated factors in Porto Alegre, a southern Brazilian city: a population-based survey. J Stud Alcohol. 1996;57:253–259. doi: 10.15288/jsa.1996.57.253. [DOI] [PubMed] [Google Scholar]
- 13.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 14.Sonmez K, Akcakoyun M, Akcay A, Demir D, Duran NE, Gencbay M, Degertekin M, Turan F. Which method should be used to determine the obesity, in patients with coronary artery disease? (body mass index, waist circumference or waist-hip ratio) Int J Obes Relat Metab Disord. 2003;27:341–346. doi: 10.1038/sj.ijo.0802238. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Report of a WHO consultation. Geneva, Switzerland: 1999. Consultation on obesity. Obesity: preventing and managing the global epidemic; p. 894. [PubMed] [Google Scholar]
- 16.Assoc AD. Standards of medical care in diabetes 2008. Diabetes Care. 2008;31:S12–S54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- 17.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 18.Mann DM, Lee J, Liao Y, Natarajan S. Independent effect and population impact of obesity on fatal coronary heart disease in adults. Prev Med. 2006;42:66–72. doi: 10.1016/j.ypmed.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Auer J, Weber T, Berent R, Lassnig E, Maurer E, Lamm G, Kvas E, Eber B. Obesity, body fat and coronary atherosclerosis. Int J Cardiol. 2005;98:227–235. doi: 10.1016/j.ijcard.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 20.Rossi R, Iaccarino D, Nuzzo A, Chiurlia E, Bacco L, Venturelli A, Modena MG. Influence of body mass index on extent of coronary atherosclerosis and cardiac events in a cohort of patients at risk of coronary artery disease. Nutr Metab Cardiovasc Dis. 2011;21:86–93. doi: 10.1016/j.numecd.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Poludasu S, Cavusoglu E, Khan W, Marmur JD. Impact of body mass index on long-term all-cause mortality after percutaneous coronary intervention in African-Americans. J Invasive Cardiol. 2009;21:20–25. [PubMed] [Google Scholar]
- 22.Sarno G, Garg S, Onuma Y, Buszman P, Linke A, Ischinger T, Klauss V, Eberli F, Corti R, Wijns W, Morice MC, di Mario C, van Geuns RJ, Eerdmans P, Garcia-Garcia HM, van Es GA, Goedhart D, de Vries T, Juni P, Meier B, Windecker S, Serruys P. The impact of body mass index on the one year outcomes of patients treated by percutaneous coronary intervention with Biolimus- and Sirolimus-eluting stents (from the LEADERS Trial) Am J Cardiol. 2010;105:475–479. doi: 10.1016/j.amjcard.2009.09.055. [DOI] [PubMed] [Google Scholar]
- 23.Welborn TA, Dhaliwal SS. Preferred clinical measures of central obesity for predicting mortality. Eur J Clin Nutr. 2007;61:1373–1379. doi: 10.1038/sj.ejcn.1602656. [DOI] [PubMed] [Google Scholar]
- 24.Ben-Noun LL, Laor A. Relationship between changes in neck circumference and cardiovascular risk factors. Exp Clin Cardiol. 2006;11:14–20. [PMC free article] [PubMed] [Google Scholar]
- 25.Ben-Noun LL, Laor A. Relationship between changes in neck circumference and changes in blood pressure. Am J Hypertens. 2004;17:409–414. doi: 10.1016/j.amjhyper.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Fink B, Manning JT, Neave N. The 2nd-4th digit ratio (2D:4D) and neck circumference: implications for risk factors in coronary heart disease. Int J Obes (Lond) 2006;30:711–714. doi: 10.1038/sj.ijo.0803154. [DOI] [PubMed] [Google Scholar]
- 27.Massierer D, Martinez D, Fuchs SC, Pellin PP, Garcia MS, Zacharias AL, Antunes IF, Wainstein MV, Moreira LB, Ribeiro JP, Fuchs FD. Obstructive sleep apnea, detected by the Berlin Questionnaire: an associated risk factor for coronary artery disease. Cad Saude Publica. 2012;28:1530–1538. doi: 10.1590/s0102-311x2012000800011. [DOI] [PubMed] [Google Scholar]
- 28.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 29.Selcuk MT, Selcuk H, Temizhan A, Maden O, Saydam GS, Dogan M, Ulupinar H, Aydin C, Topcu DI, Sasmaz A. Impact of plasma adiponectin levels to the presence and severity of coronary artery disease in patients with metabolic syndrome. Coron Artery Dis. 2008;19:79–84. doi: 10.1097/MCA.0b013e3282f3c40b. [DOI] [PubMed] [Google Scholar]
- 30.Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, Sarov-Blat L, O'Brien S, Keiper EA, Johnson AG, Martin J, Goldstein BJ, Shi Y. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108:2460–2466. doi: 10.1161/01.CIR.0000099542.57313.C5. [DOI] [PubMed] [Google Scholar]
- 31.Baker AR, Silva NF, Quinn DW, Harte AL, Pagano D, Bonser RS, Kumar S, McTernan PG. Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovasc Diabetol. 2006;5:1. doi: 10.1186/1475-2840-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chatterjee TK, Stoll LL, Denning GM, Harrelson A, Blomkalns AL, Idelman G, Rothenberg FG, Neltner B, Romig-Martin SA, Dickson EW, Rudich S, Weintraub NL. Proinflammatory phenotype of perivascular adipocytes: influence of high-fat feeding. Circ Res. 2009;104:541–549. doi: 10.1161/CIRCRESAHA.108.182998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blomkalns AL, Chatterjee T, Weintraub NL. Turning ACS outside in: linking perivascular adipose tissue to acute coronary syndromes. Am J Physiol Heart Circ Physiol. 2010;298:H734–735. doi: 10.1152/ajpheart.00058.2010. [DOI] [PubMed] [Google Scholar]
- 34.Rajsheker S, Manka D, Blomkalns AL, Chatterjee TK, Stoll LL, Weintraub NL. Crosstalk between perivascular adipose tissue and blood vessels. Curr Opin Pharmacol. 2010;10:191–196. doi: 10.1016/j.coph.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davies RJ, Stradling JR. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. Eur Respir J. 1990;3:509–514. [PubMed] [Google Scholar]
- 36.Riedner CE, Rhoden EL, Fuchs SC, Wainstein MV, Goncalves SC, Wainstein RV, Zago A, Bourscheit F, Katz N, Zago AJ, Ribeiro JP, Fuchs FD. Erectile dysfunction and coronary artery disease: an association of higher risk in younger men. J Sex Med. 2011;8:1445–1453. doi: 10.1111/j.1743-6109.2011.02224.x. [DOI] [PubMed] [Google Scholar]
- 37.Hasan RK, Ginwala NT, Shah RY, Kumbhani DJ, Wilensky RL, Mehta NN. Quantitative angiography in South Asians reveals differences in vessel size and coronary artery disease severity compared to Caucasians. Am J Cardiovasc Dis. 2011;1:31–37. [PMC free article] [PubMed] [Google Scholar]


