Abstract
Objectives:
Describe short- and long-term outcomes observed in individuals with hip osteoarthritis (OA) treated with a pre-selected, standardized set of best-evidence manual therapy and therapeutic exercise interventions.
Methods:
Fifteen consecutive subjects (9 males, 6 females; mean age: 52±7.5 years) with unilateral hip OA received an identical protocol of manual therapy and therapeutic exercise interventions. Subjects attended 10 treatment sessions over an 8-week period for manual therapy interventions and performed the therapeutic exercise as a home program.
Results:
Baseline to 8-week follow-up outcomes were as follows: Harris Hip Scale (HHS) scores improved from 60.3(±10.4) to 80.7(±10.5), Numerical Pain Rating Scale (NPRS) scores improved from 4.3(±1.9) to 2.0(±1.9), hip flexion range of motion (ROM) improved from 99 degrees (±10.6) to 127 degrees (±6.3) and hip internal rotation ROM improved from 19 degrees (±9.1) to 31 degrees (±11.5). Improvements in HHS, NPRS, and hip ROM measures reached statistical significance (P<0.05) at 8-weeks and remained significant at the 29-week follow-up. Mean changes in NPRS and HHS scores exceeded the minimal clinically important difference (MCID) at 8-weeks and for the HHS scores alone at 29 weeks. The 8 and 29 week mean Global Rating of Change scores were 5.1(±1.4) and 2.1(±4.2), respectively.
Improved outcomes observed following a pre-selected, standardized treatment protocol were similar to those observed in previous studies involving impairment-based manual therapy and therapeutic exercise for hip OA. Future studies might directly compare the two approaches.
Discussion:
Keywords: Hip, Osteoarthritis, Physical therapy, Manual therapy, Therapeutic exercise, Orthopedic manual physical therapy, Hip OA, Exercise
Introduction
Osteoarthritis (OA) is the leading cause of lower-limb related disability in the elderly.1 OA also represents a considerable and increasing financial burden on society, with the annual costs related to OA in the United States expected to reach 100 billion dollars by the year 2020.2 The hip is the second most common site for large joint OA, affecting 3–11% of the western population over 35 years of age.3 This rate is expected to rise in the future as a consequence of the aging population.4
The high healthcare costs associated with hip OA are largely attributable to surgical and pharmacologic interventions.5 The frequency of hip joint arthroplasty, the most common surgery performed for individuals with hip OA, has risen 158% since 1990.6 Pharmacological interventions for individuals with hip OA most commonly involve non-steroidal anti-inflammatory drugs as well as medications to help counteract the serious gastrointestinal side effects commonly experienced by these individuals.5,7 Because of the financial costs and potential side effects associated with these interventions, identifying effective non-pharmocological and non-operative interventions for hip OA has been recognized as a priority for future research.8
Hip OA is characterized by radiographic and clinical findings, although many individuals with radiographic evidence of hip OA have no symptoms.9 The most common objective clinical findings are loss of hip internal rotation (HIR) and hip flexion (HF) range of motion (ROM).10 Additionally, hip joints affected by OA have been found to exhibit reduced capsular elasticity and altered intracapsular pressures.11 Many individuals suffering from hip OA develop considerable physical disability as a consequence of the acquired limitations in ambulation and activities of daily living.5 The natural history of hip OA is not favorable; symptom severity and disability levels tend to worsen over time.5
Several interventions for hip OA administered by physical therapists have been reported in the medical literature, including education, therapeutic exercise, aquatic exercise therapy and manual therapy.12–15 Land-based and aquatic exercise have both been shown to decrease pain and improve function, and education has been associated with short-term pain relief.13–15 Unfortunately, the beneficial effects from exercise deteriorate and eventually disappear within three to nine months following cessation of the supervised exercise program.15
Research into the effectiveness of manual therapy for patients with hip OA is limited, but initial studies have yielded positive results.12 Hoeksma and colleagues16 compared the effectiveness of manual therapy and exercise therapy in a randomized clinical trial of patients with hip OA. Exercise therapy consisted of an adaptation of an exercise program previously found to be beneficial for patients suffering from hip OA.17 Manual therapy interventions consisted of clinician-assisted manual stretching of hip musculature followed by a traction manipulation technique to the involved hip. The treatment period for both groups consisted of nine sessions over a duration of five weeks. Subjects receiving manual therapy demonstrated greater improvements in hip function (measured with the Harris Hip Score), walking speed, hip ROM, and pain at the conclusion of the five-week treatment period. Improvements in pain, function and ROM were maintained at three and six month follow-ups.
MacDonald et al.18 reported clinical outcomes in a case series of seven subjects with hip OA following a median of five treatment sessions of manual therapy combined with therapeutic exercise. Impairment-based interventions included thrust and non-thrust manipulations and an exercise program targeted at improving hip joint mobility and muscle strength. Following a median of five treatment sessions all subjects experienced reductions in pain and clinically meaningful improvements in function. Because a cause and effect relationship cannot be inferred from a case series, future research will need to corroborate the results of this combined treatment approach and eventually determine whether the addition of an exercise program adds meaningful benefit over manual therapy alone in patients with a diagnosis of hip OA.
Another unanswered question involving the application of manual therapy in patients with hip OA is whether an ‘impairment-based’ approach produces similar outcomes to that of a pre-selected, standardized set of manual therapy and exercise interventions. There is evidence indicating that for patients with lower back pain, standardizing physical therapy intervention leads to superior outcomes compared to a non-standardized treatment approach.19,20 One advantage of standardizing treatment protocols is that it allows researchers to communicate details of the interventions performed with clarity, which may improve the ability of practicing clinicians to reproduce clinical outcomes observed in clinical research.
Considering these unanswered questions as well as the paucity of research on manual therapy and exercise for this population, the aims of this study were to (1) describe the management of 15 patients with unilateral hip OA using manual therapy and exercise interventions and (2) observe the magnitude of short- and long-term changes in clinical outcomes using a generalizable, standardized protocol that would represent the best available research on a manual therapy and exercise approach for individuals with hip OA.
Methods
Participants
Consecutive patients with a primary complaint of unilateral hip pain referred by physicians or physical therapists to the Physical Therapy department of Brooke Army Medical Center in San Antonio, TX were screened for study inclusion. Individuals were included in the study if they were between 35 and 80 years of age, had a primary complaint of unilateral hip pain and met the American College of Rheumatology criteria for hip OA (Table 1).21 Patients were excluded from the study if they had rheumatoid arthritis, severe lower back pain, recent spinal, hip or knee orthopedic surgery, radicular pain below the knee, osteoporosis, bilateral hip pain, or refused to receive mobilization/manipulation interventions.
Table 1. American College of Rheumatology criteria for classification of hip osteoarthritis21.
| Test Cluster 1 |
| Pain reported in the hip |
| <115 degrees hip flexion range of motion (ROM) |
| <15 degrees hip internal rotation ROM |
| Test Cluster 2 |
| Pain with hip internal rotation ROM |
| <60 minutes of morning stiffness |
| >50 years of age |
Note: All three findings from either test cluster must be present in order for subject to meet clinical criteria for hip OA as defined by Altman et al.21
Consenting patients were enrolled in succession until the fifteenth subject had consented to participate in the study. Subject enrollment took place from February to October 2008. All subjects were informed of the purpose of the study and signed informed consent forms approved by the Institutional Review Board at Brooke Army Medical Center.
Examination procedures
Following enrollment in the study, subjects completed several self-report measures and underwent a routine history and physical examination. In addition to a full history, patients were questioned on the presence and severity of LBP and a systems review examination was administered to screen for systemic disease.
The physical examination included a gait assessment, lumbar spine ROM testing, a neurological assessment, bilateral ROM and muscle strength testing of the hip and knee, muscle length testing of the rectus femoris, iliopsoas, and piriformis muscles, and a palpation examination of the lumbar spine and hip regions.
Intervention
All subjects in the study received the same pre-selected set of manual therapy and therapeutic exercise interventions. Subjects were also given general information regarding osteoarthritis, advice to engage in regular cardiovascular exercise and the potential benefits of weight reduction on their condition. Manual therapy interventions were delivered during ten 30-minute treatment sessions over an 8-week period and consisted of manual muscle stretching, non-thrust and thrust manipulation techniques. These were selected through consideration of two primary factors: (1) the interventions inclusion in published clinical research involving manual therapy for hip OA16,18 and (2) the extent to which the interventions addressed common impairments found in individuals with hip OA.10,21,22 Manual therapy interventions are described in Fig. 1. Brief rationales for technique selection are provided in Table 2.
Figure 1.
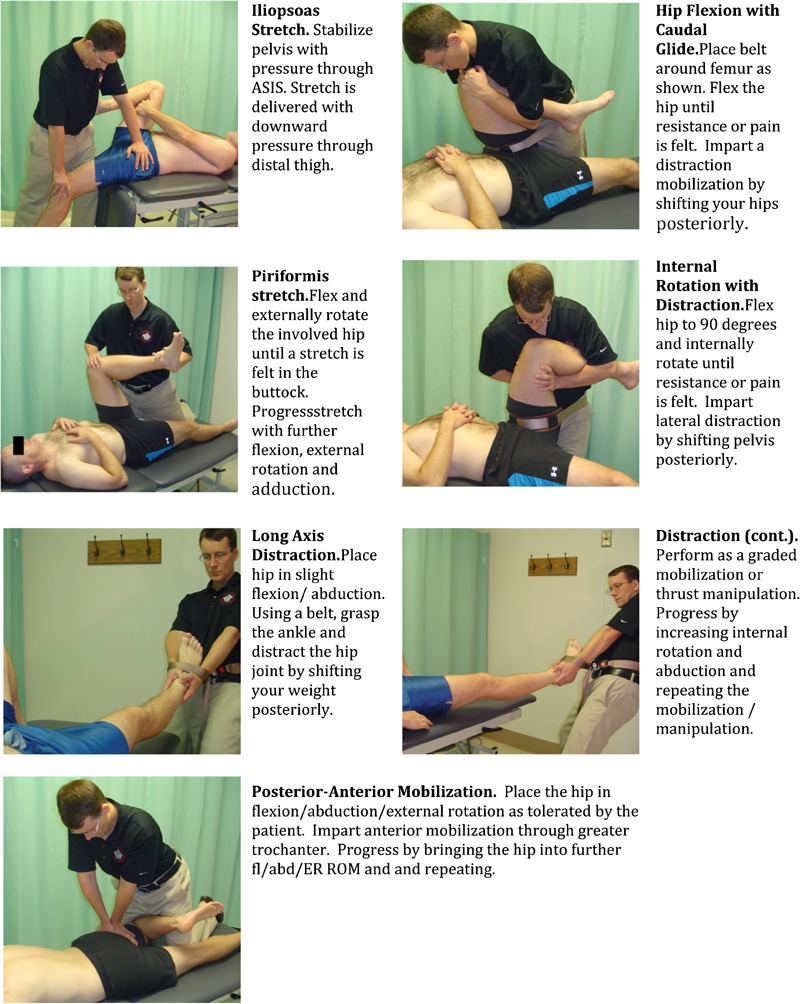
Manual therapy interventions.
Table 2. Rationale for manual therapy intervention selection.
| Manual therapy technique | Rationale for inclusion in protocol |
| Iliopsoas stretch | Improve hip extension range of motion by addressing soft-tissue restrictions. |
| Piriformis stretch | The piriformis, along with the other hip external rotators, has intimate connections with the hip joint capsule. Stretching this muscle group may therefore reduce across the joint capsule, thus improving pain and range of motion.11 |
| Long-axis distraction | Increase capsule elasticity and thus improve pain and hip range of motion.16 |
| Hip flexion with caudal glide | Improve hip flexion range of motion |
| Internal rotation with lateral glide | Improve hip internal rotation range of motion |
| Posterior–anterior mobilization | Improve hip extension range of motion |
Although the manual interventions were pre-selected, the treating clinicians were permitted to vary aspects of the techniques. Manual therapy techniques (excluding the stretches) were introduced as gentle, graded mobilizations. This was to familiarize the subject with the techniques and ensure the interventions were well tolerated. The interventions were then progressed and varied at the discretion of the treating clinician. The clinical reasoning approach described by Maitland was used to guide this decision making.23 A central principle of this approach is to continually evaluate the patient’s response to treatment and alter aspects of the techniques accordingly.23 Using this approach, decisions on how to vary aspects of the technique such as vigor or grade of mobilization, patient position and duration of the technique are adjusted according to the patient’s symptom response to the intervention(s) both immediately (within session) and between sessions. Treating clinicians identify salient clinical findings, both subjective and objective, to judge the effect of interventions. For example, if a patient reported they had difficulty donning socks and exhibited a pronounced loss of HF ROM then these measures were re-assessed immediately following a manual therapy intervention as well as at the start of a treatment session to guide decision making. If an intervention was delivered and the patient did not demonstrate immediate improvement in HF ROM or the improvement was minor, then the clinician may have chosen to deliver the mobilization with more vigor or progress the technique to a thrust manipulation. Alternatively, the clinician may have elected to perform a graded mobilization for a longer duration to achieve the desired effects. Conversely, if upon returning for a treatment session, this patient reported increased pain and difficulty donning socks since their last treatment session and HF ROM had either worsened or not improved, the treating clinician may have determined that all or some of the interventions were performed with excessive vigor and therefore delivered that session’s interventions as gentle stretches and graded mobilizations of shorter duration.
The exercise component was designed to reinforce these pre-selected manual therapy interventions as well as to address common strength and flexibility impairments found in individuals with hip OA.24,25 The therapeutic exercise interventions are described in Fig. 2. Compliance with the home exercise program was tracked with a log given to patients at the baseline examination. Patients were categorized as ‘compliant’ if they performed their exercises (on average) at least four days per week and ‘non-compliant’ if they only performed the program three or fewer days per week.
Figure 2.
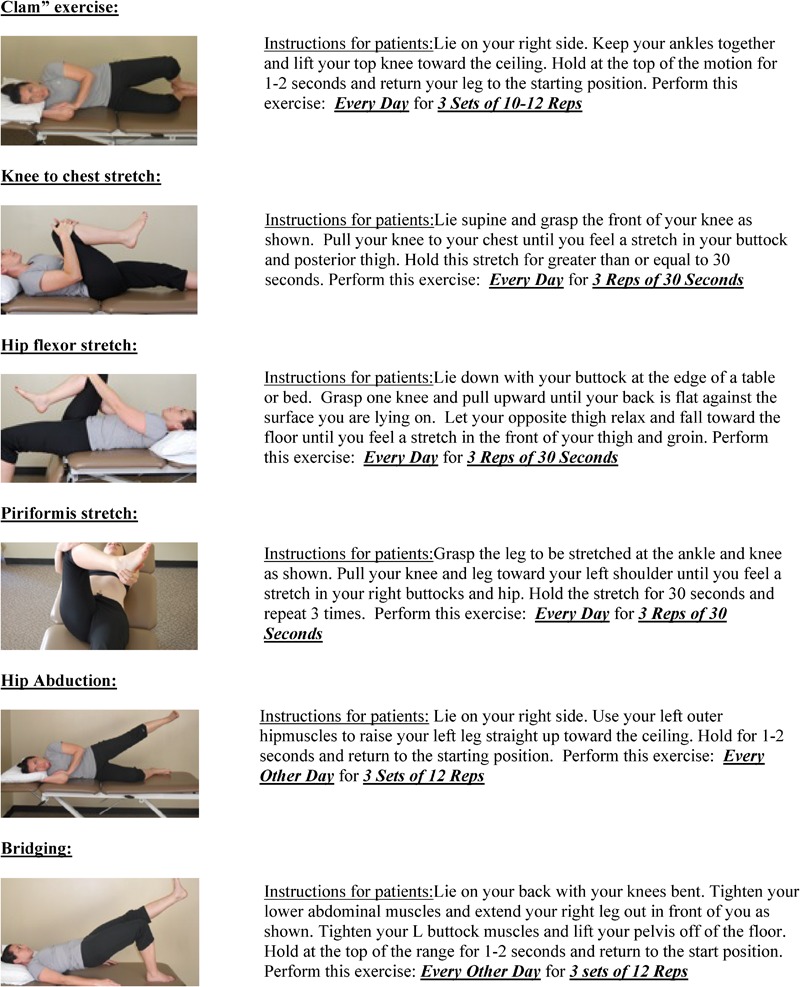
Therapeutic exercise interventions.
Follow-up
Follow-up examinations were conducted at the end of the treatment period (8-weeks) and at the 29-week interval.
Outcome measures
The primary outcome measure was the Harris Hip Scale (HHS). The HHS is the most widely used instrument for quantifying pain and function in patients with hip OA in the United States and has been used extensively in clinical research.26 The instrument consists of 10 items representing pain, walking ability, activities of daily living and ROM of the hip.27 Scores range from 0 (maximum disability) to 100 (no disability).27 The HHS has been shown to be a reliable, valid and responsive measurement for patients with hip OA.27–29 Hoeksma et al. observed that a change of at least four points corresponded with detectable clinical improvement.
Pain was also measured with the Numeric Pain Rating Scale (NPRS), an 11-point scale used to quantify pain intensity.30 Subjects rated their current, least and worst amount of pain over the previous 24 hours. The average of the three ratings was recorded. The NPRS has been shown to be a reliable and valid measure of pain intensity.30,31 A two point change or greater has been reported to represent a clinically meaningful change in pain intensity.32,33
Patient-perceived improvement following treatment was measured with the Global Rating of Change (GRC) instrument. Subjects rated their overall improvement since initiation of treatment on a scale from −7 (a very great deal worse) to zero (about the same) to +7 (a very great deal better).34 Juniper et al.35 proposed a classification system which states: scores of −1, 0 and +1 are associated with no change in the subject’s condition, scores of ±2–3 represent minimal change, ±4–5 represent moderate change and ±6–7 represent large changes in their condition.
Hip mobility was assessed by measuring HIR and HF passive range of motion (PROM). Limitations in HIR and HF PROM are common impairments found in individuals with hip OA.10,21,22 Additionally, limited PROM of the hip has been shown to be highly correlated with disability in individuals with hip OA.36 Measurements were taken with a standard long-arm goniometer. HF and HIR PROM values taken with a long-arm goniometer have been shown to have good intra-rater reliability (ICC = 0.82 to 0.92) and adequate inter-rater reliability (ICC = 0.58 to 0.71).37–39
Initial and post-treatment values for the HHS, NPRS and HF and HIR PROM were collected at baseline, 8- and 29-week follow-up examinations. The GRC was administered at the 8- and 29-week follow-up examinations. Exercise compliance logs were collected at the 8- and 29-week follow-up examinations.
Data analysis
Data were assessed for normality using a Kolmogorov-Smirnov test. A one-way repeated measures analysis of variance was used to determine differences in PROM values, HHS and NPRS scores between baseline, 8 weeks and 29 weeks. An alpha level of 0.05 was used for all comparisons. Statistical analysis was conducted using SPSS, version 18.0, statistical software package.
Results
Fifteen individuals (9 male) participated in the study. Participants had an average age of 52(±7.4) years and experienced hip pain, on average, for 23 months (range 3 to 144). Demographic and baseline characteristics are provided in Table 3. All 15 subjects completed the 8-week follow-up exam. Between the 8- and 29-week follow-up period one subject elected to receive a total hip arthroplasty and therefore was not included in the 29-week analysis. On average, subjects attended a total of 8 treatment sessions (range 6 to 10) over a period of 8 weeks (range 5 to 12).
Table 3. Participant demographics and baseline characteristics (n = 15).
| Variable | Value |
Age ( ±SD) ±SD) |
52±7.4 |
| Gender (no. of participants) | |
| Male | 9 |
| Female | 6 |
Body Mass Index ( ±SD) ±SD) |
27.8±3.8 |
Symptom duration (months)( ±SD) ±SD) |
23±34.2 |
| Range (months) | 3–144 |
| Analgesic use (no. of participants (%)) | |
| Infrequent (<1×/wk) | 2 (13.4) |
| Moderate (1–3×/wk) | 6 (40) |
| Frequent (4–6×/wk) | 1 (6.7) |
| Regular (>6×/wk) | 6 (40) |
| *Radiographic evidence of hip OA (no. of subjects (%)) | |
| None | 2 (13.4) |
| Mild OA | 7 (46.7) |
| Moderate OA | 4 (26.7) |
| Severe OA | 2 (13.4) |
| Lower back pain (no. of subjects (%)) | |
| None | 3 (20) |
| Mild | 7 (46.7) |
| Moderate | 5 (33) |
| Involved hip | |
| Right | 11 |
| Left | 4 |
Note: *Radiographic evidence as characterized by radiologist from plain film X-ray.
Improvements in HHS, NPRS, and hip ROM measures reached statistical significance (P<0.05) at 8-weeks and remained significant at the 29-week follow-up. Mean changes in NPRS and HHS scores exceeded the MCID for both of these measures at 8-weeks and for the HHS scores alone at 29 weeks. At 8 weeks the mean GRC score was 5.1(±1.4), which corresponds to a statement of ‘quite a bit better’. At 29 weeks the mean GRC score was 2.1(±4.2), which corresponds to a statement of ‘somewhat better’. Mean values with associated 95% confidence intervals for baseline, 8- and 29-week outcomes for the HHS, NPRS and hip PROM tests are described in Table 4 and Figs. 3 and 4.
Table 4. Results.
| Outcome measure | Value | 95% CI* |
| Harris Hip Scale | ||
| 0-week | 61.5 (±10.4) | 55.9, 67.0 |
| 8-week | 81.7 (±9.3) | 76.5, 86.8 |
| 29-week | 79.1 (±11.3) | 72.5, 85.6 |
| NPRS | ||
| 0-week | 4.4 (±1.6) | 3.5, 5.4 |
| 8-week | 1.9 (±1.9) | 0.8, 3.0 |
| 29-week | 2.9 (±2.4) | 1.5, 4.3 |
| HF ROM | ||
| 0-week | 99.6 (±10.9) | 92.7, 106.6 |
| 8-week | 127.5 (±6.9) | 123.4, 131.7 |
| 29-week | 124.1 (±11.5) | 117.1, 131.0 |
| HIR ROM | ||
| 0-week | 20.2 (±10.1) | 13.9, 26.6 |
| 8-week | 30.1 (±11.0) | 23.5, 37.8 |
| 29-week | 29.6 (±11.0) | 23.0, 36.2 |
Note: Values are means (±standard deviations).
NPRS = Numeric Pain Rating Scale, HF = hip flexion, ROM = range of motion, HIR = hip internal rotation.
*95% CI = 95% confidence intervals around observed mean values.
Figure 3.
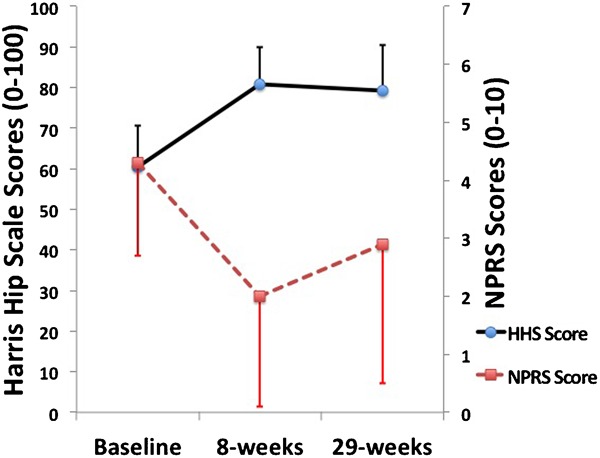
Mean Harris Hip Scale (HHS) and Numerical Pain Rating Scale (NPRS) values at baseline, 8 and 29 weeks.
Figure 4.
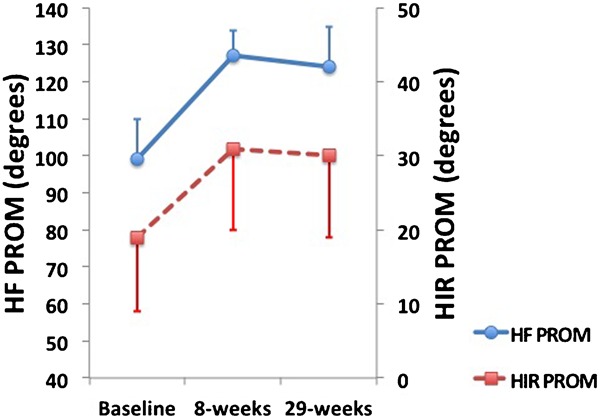
Mean hip flexion (HF) and hip internal rotation (HIR) passive range of motion (PROM) values at baseline, 8 and 29 weeks.
At the 8-week follow-up 13 of 15 subjects reported that they performed their home exercise program at least 4 days per week. At the 29-week follow-up, only 3 subjects reported performing their HEP at least 4 days per week.
Discussion
The aims of this prospective case series were to observe outcomes in individuals with hip OA treated with a standardized protocol of manual therapy and exercise interventions as well as describe the management of these individuals with a level of detail that would permit practicing clinicians to replicate this approach in their own practice. While previous research has investigated the effect of manual therapy and therapeutic exercise in individuals with hip OA,16,18 we believe this is the first study to do so with a pre-selected set of combined manual therapy and therapeutic exercise interventions.
Subjects in our study demonstrated large and clinically meaningful improvements in clinical outcomes over the short term (8-weeks). The majority of these improvements were maintained at the long-term follow-up (29-weeks). Our observed improvements in HHS scores, pain and ROM were consistent with findings from Hoeksma et al.16 These authors used a protocol of stretching and repeated hip traction manipulations for the manual therapy intervention. Our manual therapy interventions were coupled with exercise interventions targeted at improving muscle performance, flexibility and joint ROM. We believe that by combining manual therapy with exercise and patient education, our protocol represents the best available evidence regarding physical therapy management of hip OA.
Our results were also similar to those of MacDonald and colleagues who treated a series of patients suffering from hip OA with manual therapy and therapeutic exercise.18 These authors utilized an impairment-based approach for manual therapy intervention selection. Joint end-feels and accessory motions were assessed to determine which particular techniques would be delivered. Because of this individualized approach, the particular interventions varied among patients.
The majority of studies establishing manual therapy as a beneficial treatment approach for musculoskeletal conditions have utilized this impairment-based model of clinical reasoning for intervention selection.40–43 However, despite compelling evidence, manual therapy remains an underutilized management strategy among physical therapists for many conditions in which it has been shown to be effective.44–46 Although the reasons for this underutilization are likely multifactorial, perhaps one contributing factor is the lack of confidence in the average clinician to reproduce this approach in their own clinical practice. We believe that by front-loading or incorporating our clinical reasoning process in the selection of techniques we have been able to standardize the interventions in this study and reduce the ambiguity of the clinical decision-making process. Additionally, because we are able to provide detailed descriptions of the treatment received by each subject, we believe novice clinicians managing patients with hip OA could feasibly reproduce this treatment protocol.
It is currently unknown if standardizing treatment improves outcomes over those seen with an impairment based approach in patients with hip OA. While our study design precludes us from determining this, we believe this study does take a critical first step in establishing an evidenced based, comprehensive protocol that could serve as a starting point for future studies seeking to answer this question.
Although initial (8-week) improvements in HHS scores and PROM values were maintained at the 29-week follow-up, the improvements in GRC and NPRS scores dropped below clinically important changes at 29-weeks. A potential contributor to this decline could be the poor long-term compliance rates with the home exercise program. By 29 weeks, only three of the 14 subjects reported performing their home exercises at least 4 days per week. Our small sample size in this study precludes any direct comparison of clinical outcomes between compliant and non-compliant subjects. Despite this limitation, there appears to be a clinically meaningful difference in GRC scores; one of 2 outcome measures that did not maintain improvement at 29-weeks. The mean GRC score was 2.0 (‘somewhat better’) for the noncompliant and 5.6 (‘quite a bit better’) for the compliant participants. More notably, the two subjects that performed their HEP 6–7 times per week maintained their improvement in primary (HHS) and secondary (HHS, GRC, hip ROM) clinical outcomes between the 8- and 29-week follow-up points. Conversely, the two subjects that performed their exercise program only 0–1 times per week revealed a decline in their primary (HHS) and two of the secondary (GRC, NPRS) outcome measures. While these two groups demonstrate a stark contrast in outcomes, subjects performing their home exercise program 2 to 5 times per week were more variable in their ability to maintain improvement in long-term outcomes. Our findings are consistent with those of Pisters et al.,47 who found that patients with hip or knee OA who were adherent to a physical therapist prescribed home exercise program demonstrated superior clinical outcomes, out to 60 months, compared to patients who were non-adherent. Due to the degenerative and progressive nature of hip OA, some authors have suggested that periodic ‘booster’ sessions (one or two) of manual therapy and therapeutic exercise at periodic intervals (e.g. every 16 weeks) could prevent this decline in clinical outcomes and exercise compliance rates.47–49 Future research will be required to determine the optimal frequency for home exercise participation and what role, if any, booster sessions should play in the physical therapist’s management of hip OA.
There are two major limitations to this study. First, because there was no comparison group we cannot infer a cause and effect relationship between the interventions delivered and the results observed. Secondly, we failed to blind the individuals collecting outcomes. This was a minor issue for the self-report measures as these are not inherently subject to rater-bias. However, ROM measurements were collected by the treating clinician and were therefore subject to bias.
In conclusion, subjects in this prospective case-series demonstrated clinically meaningful short and long-term improvements in outcomes following a standardized protocol of manual therapy and therapeutic exercise interventions. Our results, when considered with previous studies utilitizing manual therapy and exercise in patients with hip OA, strengthens the body of evidence suggesting that manual therapy and therapeutic exercise represents an effective approach for physical therapist management of individuals with hip OA.16,18 Future research will be required to determine if standardizing protocols of manual therapy and therapeutic exercise interventions offers advantages in outcomes or degree of utilization over the pragmatic approach of an individually-tailored, impairment-based clinical reasoning model. Future research will also be required to determine what role booster sessions should play in the physical therapist management of hip OA.
References
- 1.Odding E, Valkenburg HA, Stam HJ, Hofman A. Determinants of locomotor disability in people aged 55 years and over: the Rotterdam Study. Eur J Epidemiol. 2001;17:1033–41 [DOI] [PubMed] [Google Scholar]
- 2.Elders MJ. The increasing impact of arthritis on public health. J Rheumatol Suppl. 2000;60:6–8 [PubMed] [Google Scholar]
- 3.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504 [DOI] [PubMed] [Google Scholar]
- 5.Bijlsma JW, Knahr K. Strategies for the prevention and management of osteoarthritis of the hip and knee. Best Pract Res Clin Rheumatol. 2007;21:59–76 [DOI] [PubMed] [Google Scholar]
- 6.Liu SS, Gonzalez Della Valle A, Besculides MC, Gaber LK, Memtsoudis SG. Trends in mortality, complications, and demographics for primary hip arthroplasty in the United States. Int Orthop. 2008;33:643–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tannenbaum H, Bombardier C, Davis P, Russell AS. An evidence-based approach to prescribing nonsteroidal antiinflammatory drugs. Third Canadian Consensus Conference. J Rheumatol. 2006;33:140–57 [PubMed] [Google Scholar]
- 8.Zhang W, Doherty M, Arden N, Bannwarth B, Bijlsma J, Gunther KP, et al. EULAR evidence based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2005;64:669–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christmas C, Crespo CJ, Franckowiak SC, Bathon JM, Bartlett SJ, Andersen RE. How common is hip pain among older adults? Results from the Third National Health and Nutrition Examination Survey. J Fam Pract. 2002;51:345–8 [PubMed] [Google Scholar]
- 10.Birrell F, Croft P, Cooper C, Hosie G, Macfarlane G, Silman A. Predicting radiographic hip osteoarthritis from range of movement. Rheumatology (Oxford). 2001;40:506–12 [DOI] [PubMed] [Google Scholar]
- 11.Tarasevicius S, Kesteris U, Gelmanas A, Smailys A, Wingstrand H. Intracapsular pressure and elasticity of the hip joint capsule in osteoarthritis. J Arthroplasty. 2007;22:596–600 [DOI] [PubMed] [Google Scholar]
- 12.French HP, Brennan A, White B, Cusack T. Manual therapy for osteoarthritis of the hip or knee – a systematic review. Man Ther. 2011;16:109–17 [DOI] [PubMed] [Google Scholar]
- 13.Hinman RS, Heywood SE, Day AR. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87:32–43 [DOI] [PubMed] [Google Scholar]
- 14.Hopman-Rock M, Westhoff MH. The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee. J Rheumatol. 2000;27:1947–54 [PubMed] [Google Scholar]
- 15.van Baar ME, Dekker J, Oostendorp RA, Bijl D, Voorn TB, Bijlsma JW. Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months’ follow up. Ann Rheum Dis. 2001;60:1123–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoeksma HL, Dekker J, Ronday HK, Heering A, van der Lubbe N, Vel C, et al. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: a randomized clinical trial. Arthritis Rheum. 2004;51:722–9 [DOI] [PubMed] [Google Scholar]
- 17.van Baar ME, Dekker J, Oostendorp RA, Bijl D, Voorn TB, Lemmens JA, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol. 1998;25:2432–9 [PubMed] [Google Scholar]
- 18.MacDonald CW, Whitman JM, Cleland JA, Smith M, Hoeksma HL. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: a case series. J Orthop Sports Phys Ther. 2006;36:588–99 [DOI] [PubMed] [Google Scholar]
- 19.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute ‘nonspecific’ low back pain: results of a randomized clinical trial. Spine (Phila Pa 1976). 2006;31:623–31 [DOI] [PubMed] [Google Scholar]
- 20.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine (Phila Pa 1976). 2003;28:1363–71; discussion 72 [DOI] [PubMed] [Google Scholar]
- 21.Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–14 [DOI] [PubMed] [Google Scholar]
- 22.Bierma-Zeinstra SM, Oster JD, Bernsen RM, Verhaar JA, Ginai AZ, Bohnen AM. Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care. J Rheumatol. 2002;29:1713–8 [PubMed] [Google Scholar]
- 23.Hengeveld E B K, Wells P, editors. Maitland’s peripheral manipulation. 4th ed. Philadelphia, PA: Elsevier; 2005 [Google Scholar]
- 24.Dekker J, Boot B, van der Woude LH, Bijlsma JW. Pain and disability in osteoarthritis: a review of biobehavioral mechanisms. J Behav Med. 1992;15:189–214 [DOI] [PubMed] [Google Scholar]
- 25.Sims K. Assessment and treatment of hip osteoarthritis. Man Ther. 1999;4:136–44 [DOI] [PubMed] [Google Scholar]
- 26.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83 [DOI] [PubMed] [Google Scholar]
- 27.Hoeksma HL, Van Den Ende CH, Ronday HK, Heering A, Breedveld FC. Comparison of the responsiveness of the Harris Hip Score with generic measures for hip function in osteoarthritis of the hip. Ann Rheum Dis. 2003;62:935–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–61 [DOI] [PubMed] [Google Scholar]
- 29.Soderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–97 [DOI] [PubMed] [Google Scholar]
- 30.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–92 [DOI] [PubMed] [Google Scholar]
- 31.Jensen MP, Miller L, Fisher LD. Assessment of pain during medical procedures: a comparison of three scales. Clin J Pain. 1998;14:343–9 [DOI] [PubMed] [Google Scholar]
- 32.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30:1331–4 [DOI] [PubMed] [Google Scholar]
- 33.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58 [DOI] [PubMed] [Google Scholar]
- 34.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–15 [DOI] [PubMed] [Google Scholar]
- 35.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994;47:81–7 [DOI] [PubMed] [Google Scholar]
- 36.van Baar ME, Dekker J, Lemmens JA, Oostendorp RA, Bijlsma JW. Pain and disability in patients with osteoarthritis of hip or knee: the relationship with articular, kinesiological, and psychological characteristics. J Rheumatol. 1998;25:125–33 [PubMed] [Google Scholar]
- 37.Browder DEK, Fritz J. Intertester reliability of hip rnage of motion measurements and special tests. J Orthop Sports Phys Ther. 2004;34:A115844280 [Google Scholar]
- 38.Holm I, Bolstad B, Lutken T, Ervik A, Rokkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–8 [DOI] [PubMed] [Google Scholar]
- 39.Klassbo M, Harms-Ringdahl K, Larsson G. Examination of passive ROM and capsular patterns in the hip. Physiother Res Int. 2003;8:1–12 [DOI] [PubMed] [Google Scholar]
- 40.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126–37 [DOI] [PubMed] [Google Scholar]
- 41.Deyle GD, Allison SC, Matekel RL, Ryder MG, Stang JM, Gohdes DD, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85:1301–17 [PubMed] [Google Scholar]
- 42.Walker MJ, Boyles RE, Young BA, Strunce JB, Garber MB, Whitman JM, et al. The effectiveness of manual physical therapy and exercise for mechanical neck pain: a randomized clinical trial. Spine (Phila Pa 1976). 2008;33:2371–8 [DOI] [PubMed] [Google Scholar]
- 43.Whitman JM, Flynn TW, Childs JD, Wainner RS, Gill HE, Ryder MG, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: a randomized clinical trial. Spine (Phila Pa 1976). 2006;31:2541–9 [DOI] [PubMed] [Google Scholar]
- 44.Karels CH, Polling W, Bierma-Zeinstra SM, Burdorf A, Verhagen AP, Koes BW. Treatment of arm, neck, and/or shoulder complaints in physical therapy practice. Spine (Phila Pa 1976). 2006;31:E584–9 [DOI] [PubMed] [Google Scholar]
- 45.Poitras S, Blais R, Swaine B, Rossignol M. Management of work-related low back pain: a population-based survey of physical therapists. Phys Ther. 2005;85:1168–81 [PubMed] [Google Scholar]
- 46.Walsh NE, Hurley MV. Evidence based guidelines and current practice for physiotherapy management of knee osteoarthritis. Musculoskeletal Care. 2009;7:45–56 [DOI] [PubMed] [Google Scholar]
- 47.Pisters MF, Veenhof C, Schellevis FG, Twisk JW, Dekker J, De Bakker DH. Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res (Hoboken). 2010;62:1087–94 [DOI] [PubMed] [Google Scholar]
- 48.Abbott JH, Robertson MC, McKenzie JE, Baxter GD, Theis JC, Campbell AJ. Exercise therapy, manual therapy, or both, for osteoarthritis of the hip or knee: a factorial randomised controlled trial protocol. Trials. 2009;10:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Flanagan T, Coburn P, Harcourt P, Zylinski M, Jull G. Justifying the on-going physiotherapy management of long-term patients. Man Ther. 2003;8:254–6 [DOI] [PubMed] [Google Scholar]


