Abstract
Background and purpose:
A 64-year-old man with acute onset neck pain was referred to physical therapy by a neurosurgeon. The purpose of this case study is to examine the process of differential diagnosis in a patient with neck pain and to discuss common diagnostic errors that can occur in the outpatient setting.
Case description:
The patient had an 8-week history of neck pain, which was worse when running and lifting objects. He presented with imaging of the cervical spine demonstrating degenerative changes. During the examination, several differential diagnoses were considered. A thorough physical examination of the cervical spine and upper quarter failed to reproduce his symptoms. At that time, the physical therapist was suspicious that the origin of the patient’s neck pain was non-mechanical in nature. Additional testing during the examination included having the patient exercise briefly on gym equipment; this reproduced his symptoms. After additional positional and postural changes did not alleviate the symptoms, he stopped exercising, and his pain ceased.
Outcomes:
The patient was referred back to his primary care physician who ordered cardiovascular testing including an electrocardiogram and echocardiogram. These tests revealed significant cardiac abnormalities including multi-vessel blockage of the coronary arteries and evidence of infarction. He underwent a coronary artery bypass graft 4 days later.
Discussion:
To make an appropriate differential diagnosis, physical therapists must use a patient-centered model of clinical reasoning and meta-cognition and have an awareness of diagnostic errors such that they can be avoided. The goal of the physical therapy examination, including differential diagnosis, is to efficiently classify the patient for treatment or to direct patients to the proper healthcare provider, thereby minimizing and preventing mortality and morbidity.
Keywords: Cervical spine, Differential diagnosis, Neck pain, Cardiovascular, Angina pectoris
Background and Purpose
Neck pain is a common complaint for which patients seek physical therapy. It is estimated that between 22 and 70% of the population experience neck pain at some point in their lives.1,2 Prevalence of neck pain is known to increase with age.2 There are many diagnoses that need to be considered in the case of neck pain. Neck pain may be caused by osteoarthritis, discogenic disorders, tumors, infection, myofascial pain, whiplash, trauma, spinal cord compression, cervical artery dysfunction, and referred pain from viscera.3
As with any patient presenting to an outpatient orthopedic clinic, all differential diagnoses, both musculoskeletal and non-musculoskeletal need to be considered during the examination. Therapists use subjective information offered by the patient, objective data from the clinical exam, diagnostic imaging, and other tools to formulate a diagnosis. In 46 states in the USA, patients may directly access physical therapy without a physician’s referral, and therefore physical therapists (PTs) must use their knowledge of the musculoskeletal system to act as front-line providers. An accurate diagnosis is imperative to treat a patient safely, effectively, and efficiently. Diagnostic errors can include incorrect, missed, or delayed diagnoses.4 Inaccurately diagnosing a patient can lead to increased costs associated with inappropriate tests and referrals and a potential decline in the patient’s condition.5,6
To arrive at an appropriate differential diagnosis, PTs must use a patient-centered model of clinical reasoning and meta-cognition and have an awareness of diagnostic errors such that they can be avoided during the examination.5,7–10 Clinical reasoning is a process that is hypothetico-deductive, meaning that the practitioner generates and tests hypotheses based on data collected from the examination.11 Robust tools such as meta-cognition, defined as reflecting upon one’s thought process and pattern recognition, are useful for the expert clinician.11
Through the process of differential diagnosis, the PT can serve as a consultant in situations when it is appropriate to refer the patient to another medical provider due to potentially serious conditions. The purpose of this paper is to describe the clinical reasoning process that led to a differential diagnosis of non-mechanical pain in a patient with complaints of neck pain. The patho-anatomical pathway for neck pain caused by angina pectoris is explored, as this may be a relatively under-recognized differential diagnosis for neck pain. Several diagnostic errors will be reflected upon to assist PTs in recognizing these errors in the clinic and therefore attempting to avoid them.
Case Description
Patient characteristics and history
The patient was a 64-year-old male who presented for his initial physical therapy evaluation with a referral from a neurosurgeon for neck pain. Approximately 8 weeks prior to the physical therapy evaluation, the patient had developed neck pain. The patient enjoyed running several times a week up until the onset of the neck pain and had subsequently stopped exercising due to his neck pain. He worked full-time as a scientist. His past medical history included hypertension, depression, anxiety, dislipidemia, hypothyroidism, gastro-esophageal reflux disorder, peptic ulcer disorder, erectile dysfunction, allergic rhinitis, and recent thyroidectomy. The patient was taking the following medications: esomeprazole, fluticasone propionate nasal spray, gabapentin, levothyroxine sodium, losartan potassium/hydrochlorothiazide, and tadalafil. His body mass index was 31.3.
The patient reported that the onset of anterior and posterior neck pain occurred while running one day. The pain came on after about 15 minutes of running and was so intense that he had to stop. Since that time, each attempt he made at either running or walking briskly was cut short by neck pain. He also reported neck stiffness in the mornings and pain in his neck when lifting things, like his briefcase.
The patient saw several medical providers in different specialty areas for this complaint. Initially, his chief complaint was documented as throat pain. First he saw his primary care physician (PCP) several days after the onset of his symptoms. His symptoms were suggested to be a result of seasonal allergies, and he was told to take Claritin and ibuprofen. After 1 week, he saw his PCP again and he was noted to have enlarged lymph nodes; a referral to an otolaryngologist was made. The otolaryngologist performed a flexible laryngoscopy, which did not detect any abnormal findings. He theorized that the cervical spine could be the source of the pain or it could be anxiety-related. He ordered a cervical spine computed tomography (CT) with contrast. The results of the CT showed ‘severe R-sided C3-4 facet arthrosis with associated grade 1 anterolisthesis.’ The patient was noted to have a ‘mixed solid/cystic mass in the left thyroid lobe measuring approximately 4 cm’. At the follow-up appointment with the otolaryngologist, a fine needle aspiration of the thyroid was performed and surgical removal of the thyroid mass was recommended. He was also referred to a neurosurgeon. At this point, it was approximately 6 weeks after the initial onset of symptoms. The patient underwent a lobectomy of his thyroid and had an uneventful post-operative course. A pre-operative electrocardiogram (ECG) detected abnormalities that ‘could suggest an old myocardial infarct’. He was then seen by the neurosurgeon who referred him to PT with a diagnosis of cervicalgia. The patient’s goal for PT was to be able to return to running.
Clinical impression #1
The patient’s chief complaint was anterior neck pain that started at the sternal notch and radiated bilaterally to the jaw line; the patient also described diffuse posterior neck pain which was bilateral and extended from occiput to upper thoracic area and was slightly more to the right-sided than left (Fig. 1). He rated the pain at worst 6/10 on the visual analog scale (VAS).
Figure 1.
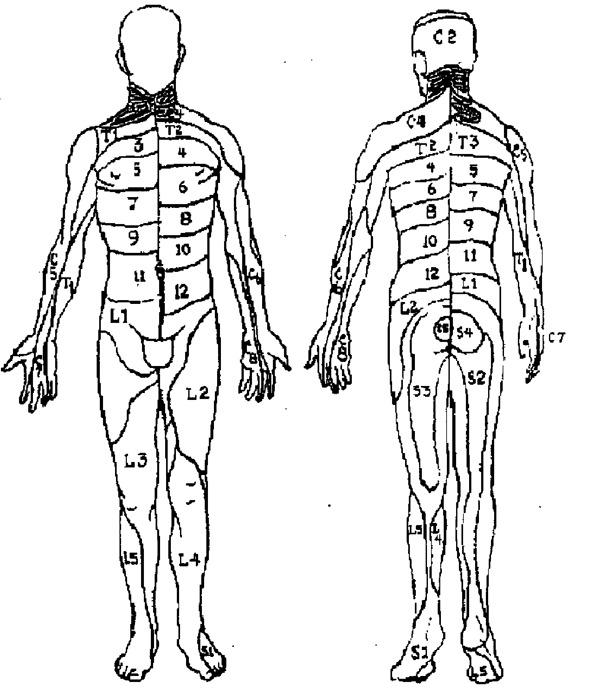
Pain Diagram.
At this point, the PT developed an initial hypothesis that the patient’s symptoms were musculoskeletal in origin, but that several non-musculoskeletal differential diagnoses needed to be investigated. During the subjective exam, the patient was asked, ‘Do you have a history of heart problems?’ to which he answered ‘No’. He also reported no family history of cardiovascular disease.
The patient was queried about other associated symptoms (i.e. nausea, shortness of breath, dysarthria, diplopia, dysphagia, dizziness, headaches, etc.) and about pain behavior (nature, intensity, duration, exacerbating, and alleviating factors). He was asked about previous episodes of neck pain, previous trauma to the area, radiating pain to the upper extremities, numbness, and tingling. He denied each of these questions. He described the pain as ‘dull’ and ‘pressure’ and intermittent. Interestingly, his pain was not affected by working for extended periods of time at the computer. Neck pain that is musculoskeletal in nature is common in populations of workers who use computers extensively.12 Initial outcome measures are noted in Table 1.
Table 1. Outcomes Measures.
| Neck disability index | Worst pain (visual analog scale) | Global rating of function | |
| Initial | 18% | 6/10 | 40% |
| Follow-up (1 month post-surgery) | 0% | 0/10 | —* |
Note: *Not collected due to surgery that occurred in the interim that affected his overall function.
Examination
The patient was examined using elements of the patient response method. This method relies on determining positions, movements, and accessory joint motions that provoke or diminish the patient’s concordant sign. The concordant sign defined as the pain or symptom that is familiar to the patient, i.e. usually the symptom for which the patient is seeking physical therapy.13 In this case, the concordant sign was neck pain (primarily anterior). Any test or measure that does not provoke the concordant sign is called non-concordant.
Observation
A well-healed thyroidectomy scar was noted in the anterior cervical area, and moderate forward head posture and rounded shoulders were observed.
Cervical active range of motion
The patient demonstrated mildly limited range of motion in all cardinal planes (normal for age). These motions were non-concordant, except for bilateral cervical lateral flexion and extension which provoked stffness in his posterior neck. Each motion was further investigated with gentle overpressure to which there was no difference response from the patient. Next, quadrant testing was performed. Quadrant testing is combined motion testing; the right posterior quadrant test involves extension, right rotation, and right lateral flexion.14 The patient reported stiffness in his posterior neck with bilateral posterior quadrant testing.
Neurological screen
Motor and sensory (light touch) testing and deep tendon reflexes of bilateral upper extremities and spinal cord reflexes (Hoffman’s test) were normal.
Shoulder screen
All motions were within normal limits and non-concordant.
Accessory motions of the cervical spine
In supine, bilateral side-glides were non-concordant. In prone, cervical and thoracic unilateral posterior–anterior spring testings and central posterior–anterior spring testings were non-concordant.15 Central posterior–anterior spring testing is performed by applying varying amount of pressure through the spinous process in posterior to anterior direction. Unilateral posterior–anterior spring testing is defined as applying varying amount of pressure through the facet pillars in a posterior to anterior direction along each side of the spine.14
Palpation
The thyroidectomy surgical scar was supple and non-tender. Cervical musculature was of normal texture and non-tender.
Special tests
Seated axial compression and distraction and Spurling’s test16 were each negative for reproduction of the patient’s symptoms.
Clinical impression #2
At this point in the examination, the PT has been unable to reproduce the patient’s concordant sign. Reaffirming that the patient’s main functional limitation was the inability to exercise, the PT decided to focus the remainder of the examination on this goal. The patient was then placed on the NuStep (Ann Arbor, MI, USA). The NuStep is described as a recumbent cross-trainer. This machine was the closest approximation to the recumbent bike on which the patient had recently attempted to exercise. The PT’s thinking was two-fold: (1) to use a functional test to assess for the concordant sign, and (2) to attempt postural/positional modifications to allow the patient to exercise on a recumbent machine at the gym.
After 4 minutes of exercise, the patient was breathing fairly heavy, and he reported that his anterior neck started to hurt (5/10 on the VAS). The PT confirmed that this was the concordant symptom. The PT then made several attempts at postural modifications (lumbar support, and upper extremities in various positions,) but the patient’s neck pain did not change. He was asked to stop exercising and within 5 minutes his neck pain gradually receded to 0/10.
Intervention
At the conclusion of the examination, the PT discussed the findings with the patient. Specifically that she could not reproduce his neck pain during the examination other than when he was exercising on the NuStep. This information, in addition to his description of neck pain with exertion and further reflection upon his past medical history, convinced the PT that a cardiovascular source of his pain could not be ruled out. He was told that he should follow up with his PCP for further testing before proceeding further with PT. The patient verbalized understanding of the rationale differential diagnosis, but stated that he was sure that the PT was incorrect. The PT did not contact the physician as the patient stated that he had an appointment with him in several days. In addition, his symptoms had been stable for several weeks, and the PT did not consider this to be a medical emergency.
After 1 week, the PT attempted to contact the patient for follow-up, but was unable to reach him and left a voicemail message. Approximately 1 month after his physical therapy evaluation, the patient did see his PCP. He was referred for several cardiac tests, including an electrocardiogram (ECG) and echocardiogram that revealed cardiac abnormalities including significant coronary atherosclerosis and evidence of previous myocardial infarctions. He then underwent a cardiac magnetic resonance imaging and cardiac catheterization. The results detailed three vessel partial or full occlusions (100% occluded left anterior descending artery, a 99% ramus lesion, and a 70% right posterolateral artery lesion). The patient underwent a coronary artery bypass graft 4 days later. He was successfully discharged home on post-operative day 4.
The cardiologist on the case confirmed the anterior neck pain as a symptom of angina pectoris caused by coronary artery disease. Angina pectoris is defined typically as crushing, squeezing, or heavy pain in the chest area. Anterior neck (throat) pain is a less common presentation of angina, while left arm pain, interscapular and chest pain are much more readily recognizable by most medical providers.17 The pain is caused by a lack of blood flow (ischemia) to the heart and may precede myocardial infarction.17,18 Pain referred to the neck and jaw is thought to occur through the convergence of afferent input onto the cervical spinothalamic tract at the C1–C3 level, therefore effecting somatic receptive fields of these levels.18 Angina pectoris can be accompanied by shortness of breath, dizziness, and fatigue, but it can also occur alone.19
The patient was mailed outcome measures for comparison to those collected on the initial visit. These results are in Table 1. One month after surgery, he was able to walk 1.5 miles and had experienced no neck pain.
Discussion
There are several diagnostic errors or pitfalls that can be highlighted from this case. Following a systematic, patient-centered examination and evaluation process including pattern recognition and meta-cognition, can assist in decreasing common diagnostic errors.5,10,11
The differential diagnosis process begins with a thoughtful subjective examination. It has been shown that a thorough subjective history leads to generating working hypotheses that can be reflected upon throughout the objective examination.8 This increases the likelihood of a correct diagnosis, and it can also decrease unnecessary medical tests and leads to more efficient treatment.20 Early in the patient history, of course, it is imperative to identify possible red flags. Red flags are signs or symptoms that may be suggestive of possible serious pathology.6
Prior to attending PT, the patient had seen his PCP four times, an otolaryngologist twice, and a neurosurgeon once for this specific complaint. Each of the medical providers that the patient encountered, had documented that the patient had ‘no cardiac history’ which was at least in part based on the patient’s perception that he had no cardiovascular history, specifically previous myocardial infarctions, or treatments for heart-related conditions, etc. He was asked this question verbally and on questionnaires concerning past medical history. This is a type of diagnostic error called an ‘unpacking error’.10 An unpacking error is a failure to elicit all relevant information in a patient’s medical history. A more sensitive line of questioning might have included the following questions: (1) have you ever had any abnormal heart tests?; (2) has any doctor ever told you that here might be concerns about your heart? The pitfall here is to avoid ambiguous language in communicating with patients and offer follow-up questions.21
In addition, a comprehensive investigation of his cardiovascular risk factors (hypertension, dislipidemia, obesity, and age greater than 45 years old) would have revealed that he was at a moderate risk for cardiovascular disease; adding in pain in the neck that ‘may result from ischemia’ would place him at a high risk.19 In fact, he also had an abnormal ECG prior to his thyroidectomy, and two physicians had told him that a cardiovascular issue could be a differential diagnosis for his symptoms. Neither the physicians nor the patient had followed up on this information.
Another common pitfall made by medical providers is reliance upon tests such as imaging to formulate a diagnosis.22 This can be considered confirmation bias.10 Confirmation bias is the tendency to look for evidence (positive radiology findings) to make the diagnosis despite other evidence (pattern of symptoms) that refutes it.10 The results from any magnetic resonance imaging or CT scan should be correlated with the clinical findings to make the best diagnosis and treatment plan.22 In this case, because there were degenerative findings in the anatomical area of the patients’ symptoms, an assumption was made for causation despite the fact that his subjective history and clinical exam did not bear out a mechanical pain. Cervical abnormalities found in imaging studies are highly prevalent, even in asymptomatic individuals.23
In this case, there were several clinical reasoning mechanisms that led to a successful differential diagnosis. Early in the examination, the PT used pattern recognition to determine that the patient’s presentation of anterior neck pain fell outside of typical presentation of mechanical neck pain. Further in the exam process, the PT took a mental ‘time-out’ to reflect on the data that had been collected thus far. Meta-cognition allowed the PT to recognize that a working diagnosis of mechanical neck had not been supported by any clinical findings. The PT proceeded through the systematic approach to attempt to further elicit the pain during exercise as was described by the patient. During the final phase of the differential diagnosis, the PT was able to confidently reject her initial hypothesis of mechanical neck pain for a more feasible diagnosis of non-mechanical pain. Having a set of tools to minimize diagnosis error such as pattern recognition, meta-cognition, mental checklists of differential diagnoses and red flags, and openly discussing misdiagnosis among peers is imperative for healthcare professionals.
To make a correct differential diagnosis, it is necessary to practice ‘worst-case scenario’ thinking and be knowledgeable about common diagnostic errors.5
References
- 1.Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain. 1989;37:215–22 [DOI] [PubMed] [Google Scholar]
- 2.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine (Phila Pa 1976). 1994;19:1307–9 [DOI] [PubMed] [Google Scholar]
- 3.Childs JD, Clealand JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopeadic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38:A1–34 [DOI] [PubMed] [Google Scholar]
- 4.Newman-Toker DE, Pronovost PJ. Diagnostic errors — the next frontier for patient safety. JAMA. 2009;301:1060–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trowbridge RL. Twelve tips for teaching avoidance of diagnostic errors. Med Teach. 2008;30:496–500 [DOI] [PubMed] [Google Scholar]
- 6.Cook C, Hegedus E. Diagnostic utility of clinical tests for spinal dysfunction. Man Ther. 2011;16:21–5 [DOI] [PubMed] [Google Scholar]
- 7.Meadows JTS. Orthopedic differential diagnosis in physical therapy: a case study approach. New York: McGraw-Hill, Health Professions Division; 1999. p. xix [Google Scholar]
- 8.Higgs J, Jones MA. Clinical reasoning in the health professions. 2nd ed. Oxford; Boston, MA: Butterworth-Heinemann; 2000. p. xiv [Google Scholar]
- 9.Croskerry P. Cognitive forcing strategies in clinical decisionmaking. Ann Emerg Med. 2003;41:110–20 [DOI] [PubMed] [Google Scholar]
- 10.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78:775–80 [DOI] [PubMed] [Google Scholar]
- 11.Jones MA. Clinical reasoning in manual therapy. Phys Ther. 1992;72:875–84 [DOI] [PubMed] [Google Scholar]
- 12.Gerr F, Marcus M, Ensor C, Kleinbaum D, Cohen S, Edwards A, et al. A prospective study of computer users: I. study design and incidence of musculoskeletal symptoms and disorders. Am J Ind Med. 2002;41:221–35 [DOI] [PubMed] [Google Scholar]
- 13.Cook C. Orthopedic manual therapy: an evidence-based approach. Upper Saddle River, NJ: Pearson/Prentice Hall; 2007 [Google Scholar]
- 14.Cook C, Hegedus EJ. Orthopedic physical examination tests: an evidence-based approach. Upper Saddle River, NJ: Pearson/Prentice Hall; 2008. p. xv [Google Scholar]
- 15.Jull G, Bogduk N, Marsland A. The accuracy of manual diagnosis for cervical zygapophysial joint pain syndromes. Med J Aust. 1988;148:233–6 [DOI] [PubMed] [Google Scholar]
- 16.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003;28:52–62 [DOI] [PubMed] [Google Scholar]
- 17.Foreman RD. Mechanisms of cardiac pain. Annu Rev Physiol. 1999;61:143–67 [DOI] [PubMed] [Google Scholar]
- 18.Frownfelter DL, Dean E. Principles and practice of cardiopulmonary physical therapy. 3rd ed. St Louis, MO: Mosby-Year Book; 1996. p. xxii [Google Scholar]
- 19.Thompson W, Gordon N, Pescatello L, eds. ACSM’s guidelines for exercise testing and prescription. 8th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2010 [Google Scholar]
- 20.Whiting P, Harbord R, de Salis I, Egger M, Sterne J. Evidence-based diagnosis. J Health Serv Res Policy. 2008;13 Suppl 3:57–63 [DOI] [PubMed] [Google Scholar]
- 21.Redelmeier DA, Schull MJ, Hux JE, Tu JV, Ferris LE. Problems for clinical judgement: 1. eliciting an insightful history of present illness. CMAJ. 2001;164:647–51 [PMC free article] [PubMed] [Google Scholar]
- 22.Elliott JM, Flynn TW, Al-Najjar A, Press J, Nguyen B, Noteboom JT. The pearls and pitfalls of magnetic resonance imaging for the spine. J Orthop Sports Phys Ther. 2011;41:848–60 [DOI] [PubMed] [Google Scholar]
- 23.Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:1178–84 [PubMed] [Google Scholar]


