Abstract
de Moura DR, Costa JC, Santos IS, Barros AJD, Matijasevich A, Halpern R, Dumith S, Karam S, Barros FC. Risk factors for suspected developmental delay at age 2 years in a Brazilian birth cohort. Paediatric and Perinatal Epidemiology 2010; 24: 211–221.
Many children are at risk of not achieving their full potential for development. Epidemiological studies have the advantage of being able to identify a number of associated factors potentially amenable to intervention. Our purpose was to identify risk factors for suspected developmental delay (SDD) at age 2 years among all children born in the city of Pelotas, Brazil, in 2004. This study was part of the 2004 Pelotas Birth Cohort. The Battelle Screening Developmental Inventory (BSDI) was administered to cohort children at age 2 years. A hierarchical model of determination for SDD with confounder adjustment was built including maternal sociodemographic, reproductive and gestational characteristics, as well as child and environmental characteristics. Multivariable analysis was carried out using Poisson regression. Prevalence ratios (PR) and 95% confidence intervals [95% CI] were calculated.
In the results, 3.3% of the 3869 children studied screened positive for SDD. After confounder control, children more likely to show SDD were: those with positive BSDI at age 12 months (PR = 5.51 [3.59, 8.47]); with 5-min Apgar <7 (PR = 3.52 [1.70, 7.27]); with mothers who had <4 years of schooling (PR = 3.35 [1.98, 5.66]); from social classes D and E (PR = 3.00 [1.45, 6.19]); with a history of gestational diabetes (PR = 2.77 [1.34, 5.75]); born <24 months after the last sibling (PR = 2.46 [1.42, 4.27]); were not told child stories in the preceding week (PR 2.28 [1.43, 3.63]); did not have children's literature at home (PR = 2.08 [1.27, 3.39]); with low birthweight (PR = 1.75 [1.00, 3.07]); were born preterm (PR = 1.74 [1.07, 2.81]); with <6 antenatal care appointments (PR = 1.70 [1.07, 2.68]); with history of hospitalisation (PR = 1.65 [1.09, 2.50]); and of male sex (PR = 1.43 [1.00, 2.04]). These risk factors may constitute potential targets for intervention by public policies and may provide help to paediatricians in preventing developmental delay.
Keywords: child development, Pelotas Birth Cohort, Apgar score, maternal education, social class, maternal gestational diabetes, inter-birth interval, parenting, birthweight, gestation
Introduction
It is estimated that, worldwide, 200 million children under 5 years of age are at risk of not fully achieving their developmental potential.1 Human development is shaped by a dynamic and continuous interaction between biology and experience.2 Individual developmental pathways throughout the life cycle are influenced by interactions among risk factors that, on one side, increase the probability of a poor outcome and on the other side are protective factors that increase the probability of a positive outcome.3 The American Academy of Pediatrics recommends that surveillance and monitoring instruments for developmental delay are systematically used in order to identify children at risk and to introduce stimulation measures in a timely manner. There is evidence that early intervention can reduce the risk of developmental delay in older children.4,5 Stimulation can lead to not only functional, but also structural modification of the brain.6
Given the multifactorial character of developmental delay, epidemiological studies have the advantage of being able to identify a large number of associated factors potentially amenable to intervention. Most of the research on child development comes from developed countries; few studies are conducted in under-developed settings.7 The present study aimed to identify risk factors for suspected developmental delay (SDD) at age 2 years among all children born in the city of Pelotas, Brazil, in 2004.
Methodology
Population and study design
The population of the present study was a cohort of children born in 2004 in Pelotas, a city with a population of 340 thousand inhabitants, located near the Southern border of Brazil with Uruguay and Argentina. The population originates mostly from European (Portuguese, Spanish and German) and African immigrants, and native Americans. The main economic activities are agriculture (mostly rice and cattle raising), commerce and education.
All livebirths (n = 4231) from mothers living in the urban area of Pelotas and in the Jardim America neighbourhood (which belongs to the neighbouring municipality of Capão do Leão), were included in the study. Children were included in the cohort at birth, during their stay at the hospital of delivery, and were followed up at ages 3, 12 and 24 months. A total of 3869 children were visited at home at 24 months of age.
The outcome and the Battelle Screening Developmental Inventory
The outcome was investigated using the Battelle Screening Developmental Inventory (BSDI),8 which was administered to the children at home, within ±30 days of their second birthday, by a trained female interviewer. The BSDI test consists of 96 items with three administration formats: structured administration, observation, and interviews with parents or other sources.9 The BSDI was translated into Portuguese from the Spanish version, and the resulting text was pre-tested with interviewers for clarity and revised by the investigators for fidelity to the original meaning. The test was performed by interviewers who were trained by a paediatrician who was specialised in child development. The test evaluates child development in five domains: personal-social, adaptive, motor, communication and cognitive development. The sum of the scores for each domain generates a total score. Individual results were classified as either ‘normal’ or ‘suspected delay’ according to a cut-off point of −1 SD in the table of total scores of the reference population.
The explanatory variables
The explanatory variables were obtained from questionnaires administered to mothers in the hospital at the time of the child's birth (perinatal), and on the occasion of the 12- and 24-month follow-up visits. To identify the variables that were independently associated with SDD a conceptual framework was used.10 This framework was organised in levels that were then used in the multivariable analyses. Family income and mother's years of schooling years are at the most distal level, followed by maternal and gestational characteristics. These variables may determine the occurrence of perinatal events, maternal and child morbidity which, in turn, may influence the child's development. Some of the proximal factors linked to the caregiver's quality of care giving, such as telling the child stories and watching television, may also have an effect on the child's development. Although this conceptual hierarchical framework is derived from the field of child health in less-developed countries, the general principles also apply to a number of other health problems both in developed and less-developed countries.10 Furthermore, the same hierarchical framework has been used in other birth cohort studies to assess risk factors for SDD.11,12
During the perinatal interview, information on maternal sociodemographic, reproductive and gestational characteristics was obtained using structured questionnaires.
The first level: maternal sociodemographic variables
Mother's age was recorded in completed years. Skin colour was self-reported, and classified as white, black or mixed. For economic classification, the Brazilian Criterion for Economic Classification, of the Brazilian Association of Market Research Companies was used. Economic class status was divided into five groups: A (wealthiest), B, C, D and E (poorest).13,14 Maternal schooling corresponds to completed years of formal education.
The second level: maternal reproductive variables
Birth spacing corresponded to the time interval between the birth of the current and immediately preceding children, classified as primipara, <24 and ≥24 months. The number of antenatal care appointments was obtained from the mother's pregnancy card or, if unavailable, was directly reported by the mother.
The third level: gestational variables
History of anaemia, diabetes mellitus and arterial hypertension during pregnancy were considered positive only when the mother declared having been diagnosed with one of these conditions by a physician. Information on smoking during pregnancy was also collected, considering as smokers those mothers who reported smoking at least one cigarette, on a daily basis, during any trimester of pregnancy.
The fourth level: perinatal variables
Data on the newborn baby included mode of delivery (vaginal or caesarean section), 5-min Apgar, weight and gestational age. Newborns weighing <2500 g were considered as low birthweight (LBW). For assessing gestational age at birth an algorithm proposed by the National Center for Health Statistics15 was applied. The estimated age was based on the last menstrual period whenever it was consistent with birthweight, length and head circumference, based on the normal curves for these parameters for each week of gestational age.16 In case the last menstrual period-based gestational age was unknown or inconsistent, we adopted the clinical maturity estimate based on the Dubowitz method, which was performed on all newborns.17 Babies were categorised in terms of weight-for-gestational age according to the Williams criterion,16 into adequate, small or large-for-gestational-age at birth.
The fifth level: child nutritional variables and mother–child morbidity
The result of BSDI evaluation of SDD administered to the subject at home within ±30 days of his or her first birthday was extracted from the 12-month follow-up. Variables pertaining to nutrition, mother and child morbidity, and environmental stimuli were obtained at the 24-month follow-up. Duration of breast feeding was categorised into five groups: <1, 1–3, 4–6, 7–12 and ≥13 months. Length-for-age deficit and excess weight-for-length were defined according to World Health Organization standards, using cut-off points corresponding to −2.00 and +2.00 SD Z scores, respectively.18 Information on history of febrile and non-febrile seizures was directly reported by the mother. All hospital admissions during the first 2 years of life were recorded. Maternal depression at 24 months post-delivery was assessed using the Edinburgh Postnatal Depression Scale (EPDS).19 The EPDS was validated with a sample of mothers from the 2004 Pelotas Birth Cohort, showing a sensitivity of 59.5% and a specificity of 88.4% for diagnosis of maternal depression (at the cut-off point ≥13).20
The sixth level: variables related to stimulation
Environmental stimuli studied included presence of children's books or comic books in the household, whether the child had been exposed to stories in the last week (as long as told by a person or recording, but excluding television or video programmes), and time spent watching television.
Quality control
All interviews were carried out by trained interviewers. Interviewers went through retraining sessions every 2 months aimed at maintaining a high level of standardisation. Also for quality control purposes, 5% of all interviews were repeated using an abbreviated version of the questionnaire, and 40% of mothers were contacted by telephone to ascertain that interviews were being carried out adequately and in full. Data were entered twice, by two independent technicians, using Epi Info software. v. 6.4.
Statistical analysis and the hierarchical model
For analysis purposes, a hierarchical model of determination, based on the conceptual framework, was constructed. This model allows quantifying the contribution of each level to SDD (Fig. 1). Confounder control was carried out for variables in the same level or immediately superior levels. Variables with P values below 0.20 were maintained in the final multivariable analysis model. In both univariable and multivariable analysis, the associations between explanatory variables and the outcome were assessed using the Wald test, with a 5% significance threshold. Prevalence ratios (PR) and 95% confidence intervals [CI] were also calculated. Multivariable analyses were carried out using Poisson regression, which provides more reliable estimates of the relative risk than logistic regression when analysing binary outcomes from cross-sectional studies.21 Data consistency assessment, variable edition and statistical analyses were carried out using STATA software, v. 8.
Figure 1.
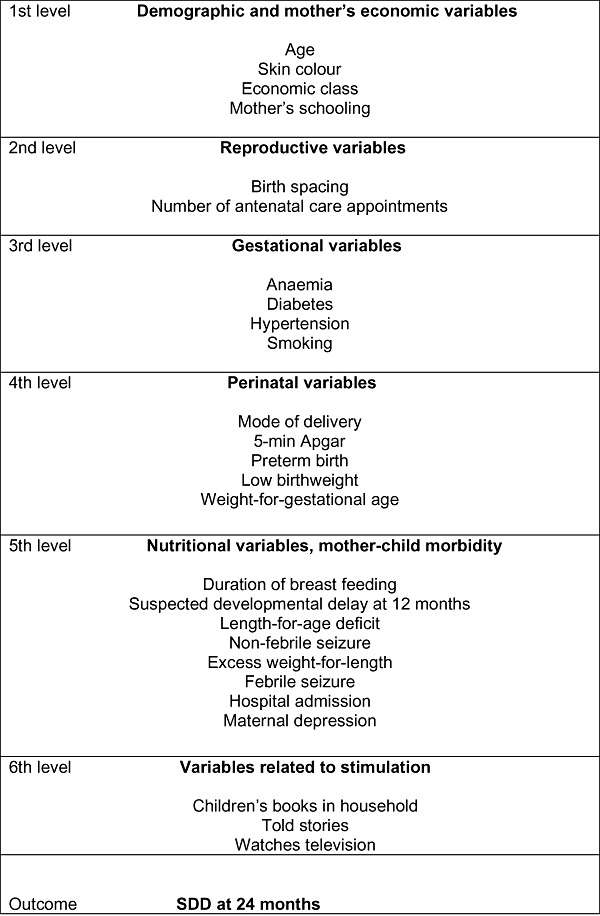
Conceptual hierarchical model for the causality of suspected developmental delay (SDD) at age 24 months.
Ethics
The 2004 Pelotas Birth Cohort Study was approved by the Research Ethics Committee of the University of Pelotas School of Medicine and by the Ethics Committee of the World Health Organization (Geneva). Prior to providing written consent, a term of informed consent explaining the study's goals and procedures was read out to mothers. Confidentiality of collected information, voluntary participation, and the possibility of leaving the study without any consequences for either mother or child were ensured to all participants.
Results
Figure 2 shows the numbers of children born in Pelotas in 2004, followed up in the subsequent visits, and losses and refusals up to 24 months. Over 90% of children were traced in all follow-ups. Table 1 describes the characteristics of mothers and 3869 children included in the current study. Table 1 also presents the prevalence of SDD according to the explanatory variables, as well as the results of univariable and multivariable adjusted analyses.
Figure 2.
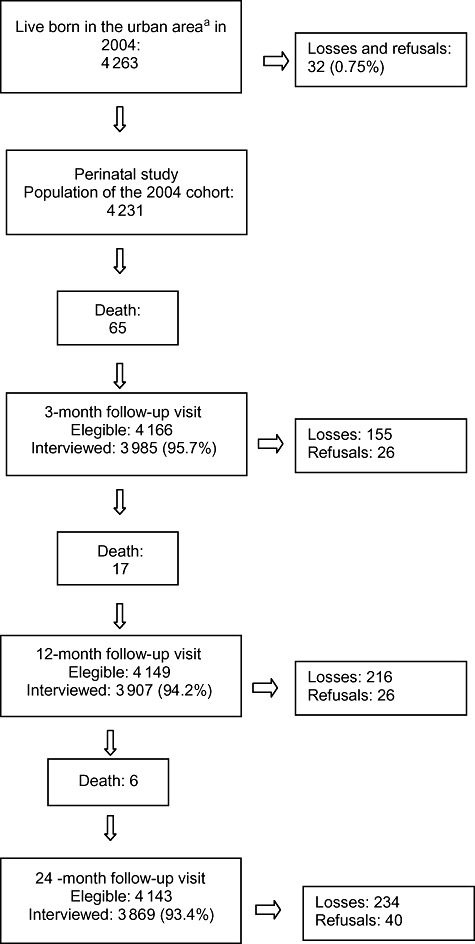
Diagram indicating the number of births, deaths, losses and refusals in the Pelotas Birth Cohort, 2004. aIncludes children born of mothers living in the Jardim América neighbourhood, which is contiguous to the Pelotas urban area but belongs to the municipality of Capão do Leão.
Table 1.
Prevalence of positive Battelle Screening Developmental Inventory (BSDI) and crude and adjusted prevalence ratios (PR) according to explanatory variables: 2004 Pelotas Birth Cohort, Pelotas, Brazil, 2008
| Univariable analysis | Multivariable analysis | ||||||
|---|---|---|---|---|---|---|---|
| Level | Variables | n | Positive BSDI (%) | PR [95% CI] | P | PRa[95% CI] | P |
| Child sex | 0.058 | 0.053 | |||||
| Male | 2011 | 3.8 | 1.40 [0.99, 2.00] | 1.43 [1.00, 2.0]) | |||
| Female | 1858 | 2.7 | 1.00 Reference | 1.00 Reference | |||
| 1 | Mother's skin colour | 0.090 | 0.972b | ||||
| White | 2372 | 2.8 | 1.00 Reference | 1.00 Reference | |||
| Mixed | 782 | 4.1 | 1.47 [0.97, 2.22] | 1.04 [0.68, 1.59] | |||
| Black | 633 | 4.1 | 1.48 [0.94, 2.30] | 0.98 [0.61, 1.55] | |||
| 1 | Mother's age (years) | 0.695 | 0.470b | ||||
| ≤19 | 722 | 3.3 | 1.06 [0.69, 1.66] | 0.83 [0.52, 1.33] | |||
| 20–35 | 2734 | 3.1 | 1.00 Reference | 1.00 Reference | |||
| ≥36 | 411 | 3.8 | 1.25 [0.74, 2.11] | 1.26 [0.74, 2.17] | |||
| 1 | Mother's schooling (years) | <0.001 | <0.001c | ||||
| 0–4 | 588 | 7.3 | 5.29 [3.24, 8.64] | 3.35 [1.98, 5.66] | |||
| 5–8 | 1504 | 3.6 | 2.64 [1.64, 4.25] | 1.81 [1.12, 2.94] | |||
| ≥9 | 1737 | 1.3 | 1.00 Reference | 1.00 Reference | |||
| 1 | Economic class | <0.001 | <0.001c | ||||
| A/B | 784 | 1.0 | 1.00 Reference | 1.00 Reference | |||
| C | 1599 | 2.3 | 2.21 [1.03, 4.73] | 1.51 [0.71, 3.21] | |||
| D/E | 1387 | 5.6 | 5.44 [2.64, 11.20] | 3.00 [1.45, 6.19] | |||
| 2 | Birth spacing | <0.001 | 0.005b | ||||
| <24 months | 319 | 8.5 | 4.72 [2.81, 7.94] | 2.46 [1.42, 4.27] | |||
| ≥24 months | 1742 | 3.2 | 1.76 [1.12, 2.78] | 1.29 [0.82, 2.04] | |||
| Primiparae | 1507 | 1.8 | 1.00 Reference | 1.00 Reference | |||
| 2 | No. antenatal care appointments | <0.001 | 0.023b | ||||
| 0–5 | 661 | 7.9 | 3.43 [2.42, 4.86] | 1.70 [1.07, 2.68] | |||
| ≥6 | 3048 | 2.3 | 1.00 Reference | 1.00 Reference | |||
| 3 | Gestational hypertension | 0.095 | 0.238b | ||||
| No | 2951 | 2.9 | 1.00 Reference | 1.00 Reference | |||
| Yes | 910 | 4.1 | 1.39 [0.94, 2.01] | 1.28 [0.85, 1.93] | |||
| 3 | Gestational diabetes | 0.222 | 0.006b | ||||
| No | 3751 | 3.2 | 1.00 Reference | 1.00 Reference | |||
| Yes | 115 | 5.2 | 1.64 [0.73, 3.65] | 2.77 [1.34, 5.75] | |||
| 3 | Gestational anaemia | 0.262 | 0.083b | ||||
| No | 1286 | 2.9 | 1.00 Reference | 1.00 Reference | |||
| Yes | 2556 | 3.5 | 1.24 [0.84, 1.82] | 1.48 [0.95, 2.29] | |||
| 3 | Smoking during pregnancy | <0.001 | 0.213b | ||||
| No | 2812 | 2.6 | 1.00 Reference | 1.00 Reference | |||
| Yes | 1057 | 5.0 | 1.93 [1.36, 2.73] | 1.29 [0.86, 1.92] | |||
| 4 | Preterm birth | <0.001 | 0.025b | ||||
| No | 3332 | 2.5 | 1.00 Reference | 1.00 Reference | |||
| Yes | 532 | 7.7 | 3.13 [2.18, 4.51] | 1.74 [1.07, 2.81] | |||
| 4 | Mode of delivery | 0.192 | 0.516b | ||||
| Vaginal | 2113 | 3.6 | 1.00 Reference | 1.00 Reference | |||
| C-section | 1756 | 2.9 | 0.79 [0.55, 1.12] | 1.14 [0.77, 1.69] | |||
| 4 | Low birthweight | <0.001 | 0.049b | ||||
| No | 3520 | 2.7 | 1.00 Reference | 1.00 Reference | |||
| Yes | 348 | 8.6 | 3.19 [2.15, 4.74] | 1.75 [1.00, 3.07] | |||
| 4 | Apgar 5 | <0.001 | 0.001b | ||||
| 0–6 | 62 | 17.7 | 5.89 [3.35, 10.38] | 3.52 [1.70, 7.27] | |||
| 7–10 | 3787 | 3.1 | 1.00 Reference | 1.00 Reference | |||
| 4 | Weight-for-gestational age | 0.014 | 0.543b | ||||
| Small | 480 | 5.2 | 1.87 [1.21, 2.88] | 1.28 [0.74, 2.22] | |||
| Adequate | 3116 | 2.8 | 1.00 Reference | 1.00 Reference | |||
| Large | 269 | 4.1 | 1.47 [0.79, 2.71] | 1.29 [0.66, 2.51] | |||
| 5 | Z-scores length-for-age | <0.001 | 0.191b | ||||
| <−2.00 | 190 | 13.7 | 5.02 [3.35, 7.54] | 1.48 [0.82, 2.68] | |||
| ≥−2.00 | 3669 | 2.7 | 1.00 Reference | 1.00 Reference | |||
| 5 | Z-scores weight-for-age | 0.095 | 0.178b | ||||
| <2.00 | 3586 | 3.4 | 1.00 Reference | 1.00 Reference | |||
| ≥2.00 | 273 | 1.5 | 0.43 [0.16, 1.16] | 0.49 [0.18, 1.38] | |||
| 5 | Duration of breast feeding (months) | <0.001 | 0.355c | ||||
| <1 | 426 | 6.1 | 2.64 [1.58, 4.41] | 1.41 [0.78, 2.57] | |||
| 1–3 | 898 | 4.6 | 1.97 [1.24, 3.14] | 1.12 [0.65, 1.95] | |||
| 4–6 | 589 | 2.0 | 0.88 [0.45, 1.71] | 1.23 [0.63, 2.39] | |||
| 7–12 | 653 | 2.5 | 1.06 [0.58, 1.93] | 1.17 [0.61, 2.27] | |||
| ≥13 | 1297 | 2.3 | 1.00 Reference | 1.00 Reference | |||
| 5 | Hospital admission | <0.001 | 0.018b | ||||
| No | 2823 | 2.09 | 1.00 Reference | 1.00 Reference | |||
| Yes | 962 | 6.55 | 3.13 [2.21, 4.43] | 1.65 [1.09, 2.50] | |||
| 5 | Non-febrile seizure | <0.001 | 0.061b | ||||
| No | 3803 | 0.3 | 1.00 Reference | 1.00 Reference | |||
| Yes | 65 | 18.5 | 6.15 [3.58, 10.59] | 2.22 [0.97, 5.10] | |||
| 5 | Febrile seizure | 0.673 | 0.938b | ||||
| No | 3741 | 3.2 | 1.00 Reference | 1.00 Reference | |||
| Yes | 128 | 3.9 | 1.20 [0.50, 2.90] | 1.03 [0.49, 2.18] | |||
| 5 | Positive Battelle at 12 months | <0.001 | <0.001b | ||||
| No | 3411 | 1.9 | 1.00 Reference | 1.00 Reference | |||
| Yes | 372 | 15.6 | 8.44 [6.01, 11.86] | 5.51 [3.59, 8.47] | |||
| 5 | Maternal depression | 0.030 | 0.896b | ||||
| No | 3209 | 2.9 | 1.00 Reference | 1.00 Reference | |||
| Yes | 612 | 4.6 | 1.58 [1.04, 2.39] | 0.97 [0.60, 1.56] | |||
| 6 | Presence of children's books | <0.001 | 0.003b | ||||
| No | 1721 | 5.8 | 4.80 [3.13, 7.35] | 2.08 [1.27, 3.39] | |||
| Yes | 2146 | 1.2 | 1.00 Reference | 1.00 Reference | |||
| 6 | Child told stories | <0.001 | <0.001b | ||||
| No | 1813 | 5.2 | 3.46 [2.32, 5.16] | 2.28 [1.43, 3.63] | |||
| Yes | 2047 | 1.5 | 1.00 Reference | 1.00 Reference | |||
| 6 | Child watches television | 0.001 | 0.685b | ||||
| No | 642 | 5.6 | 1.00 Reference | 1.00 Reference | |||
| ≤2 h | 2170 | 2.7 | 0.48 [0.32, 0.72] | 0.81 [0.50, 1.31] | |||
| >2 h | 949 | 3.1 | 0.55 [0.34, 0.88] | 0.85 [0.49, 1.49] | |||
| – | Total | 3869 | 3.3 | – | – | – | – |
PRs shown for the adjusted analysis are adjusted only for variables presenting a P value <0.20 in the same or in the upper levels of the conceptual model.
Wald test for heterogeneity.
Wald test for linear trend.
Suspected developmental delay was evaluated in 3869 children located at age 24 months, yielding a prevalence of 3.3% [95% CI 2.7, 3.8], accounting for 128 children. After adjustment for confounders, the variables listed below showed statistically significant associations with SDD.
Maternal sociodemographic variables
In the first level, boys presented a risk of SDD 43% higher than girls. Both maternal schooling and economic class were inversely associated with SDD. Children of mothers with between 0 and 4 years of schooling were over three times more likely to show SDD than those of mothers with ≥9 years of schooling. For the children of mothers with 5–9 years of schooling, prevalence was 81% greater than that of children in the ≥9 years group. In relation to classes A and B, taken as a reference, risk of SDD was 1.5- and threefold higher among children from classes C and D/E, respectively.
Maternal reproductive variables
Among reproductive variables, after allowing for maternal schooling, economic class and child's sex, a higher PR was found for birth spacing shorter than 24 months (PR = 2.46; [1.42, 4.27]) and for <6 antenatal care appointments (PR = 1.70; [1.07, 2.68]).
Gestational variables
At the level of gestational variables, children born to diabetic mothers presented an almost threefold higher PR for SDD than their controls (PR = 2.77; [1.34, 5.75]). Variables from the third level were adjusted for each other and for child's sex, mother's schooling, economic class, birth spacing and number of antenatal care appointments.
Perinatal variables
At the fourth level (perinatal variables), preterm birth (PR = 1.74; [1.07, 2.81]), LBW (PR = 1.14; [0.77, 1.69]) and 5-min Apgar <7 (PR = 3.52; [1.70, 7.27]) were associated with greater likelihood of SDD. The multivariable model included all the potential confounders for variables of the third level in addition to maternal diabetes and anaemia during pregnancy.
Child nutritional variables and mother–child morbidity
At the level of variables related to child morbidity (adjusting for preterm birth, LBW, 5′Apgar, height-for-age z-score, weight-for-height z-score and history of non-febrile seizures, besides the potential confounders of the previous levels), children with history of hospital admission (PR = 1.65; [1.09, 2.50]) and positive BSDI at 12 months (PR = 5.51; [3.59, 8.47]) presented greater PRs for SDD.
Variables related to stimulation
In the final level – factors associated with stimulation – after allowing for the above potential confounders, children whose households lacked children's books (PR = 2.08; [1.7, 3.39]) and who had not been told stories during the preceding week (PR = 2.28; [1.43, 3.63]) showed over twofold higher PRs of SDD than their counterparts.
Discussion
The current study found that, after adjustment for potential confounders, child's sex, economic class, mother's schooling, birth spacing, gestational diabetes, preterm birth, LBW, 5-min Apgar, hospital admission, SDD at 12 months, children's books at home and child told stories were associated with SDD at 24 months of age.
Strengths of this study include its cohort design, which allows for temporality of the association between exposures and the outcome. In terms of external validity, socio-economic and contextual characteristics of Pelotas are likely to represent the reality of most of the middle-sized cities from middle-income countries. This study also has some limitations. First, the BSDI has not been previously validated in a Brazilian population. Thus, it is likely that the observed accuracy with the population in which it was first tested8 does not correspond to the one when applied to Brazilian children. Second, information on maternal and child characteristics was gathered by maternal recall, and thus may suffer from information bias.
The association between economic class and SDD has also been reported by Pilz and Schermann in a study carried out in another Brazilian municipality.22 The finding that mother's schooling is independently associated with SDD is also in agreement with results from other authors.23,24 Associations with birth spacing of <24 months and with <6 antenatal care appointments were also reported in another study carried out in the same Brazilian state.22
In univariable analysis, diabetes was not significantly associated with the outcome. This association was clouded by a likely negative confounding effect of social class and maternal schooling. Mothers from more affluent social classes and with greater schooling (conditions that are shown to be protective against SDD) had a larger proportion of diabetics. This association has high biological plausibility, given that children of diabetic mothers are subject to metabolic events in the neonatal period that, depending on the quality of care, may lead to neurological lesions with sequelae that may affect child development.
In the present population, 27% of mothers smoked during pregnancy; however, this exposure was not associated with SDD. Another study investigating smoking during pregnancy and its effects on cognitive development and children's skills also failed to detect an association between these variables after control for confounders.23 The lack of association between smoking during pregnancy and SDD may be due to the way the variable was constructed. Smoking was a dichotomic variable (yes or no), independently of the intensity of smoking. A recent study has found an association with intellectual disabilities when mothers smoked 20 or more cigarettes per day.25 The higher PRs observed between preterm and LBW births with SDD in comparison, respectively, with full-term and non-LBW births are in agreement with the results of several other studies.26–30 LBW and preterm birth were also shown to be independently associated with specific delays in motor and social development.23 Lack of association between mode of delivery and SDD has been reported by other authors.31,32
Being either small or large for gestational age was not associated with positive screening for SDD, as previously shown by another author.33 However, being small for gestational age appeared as a risk factor for delays in skill acquisition in another study.34
Children with 5′Apgar <7 were three times more likely to show SDD at 24 months. The biological mechanism underlying this finding is unclear, given that no single parameter (Apgar, cord pH or heartbeat frequency) can be used as a synonym for asphyxia. Other authors have shown that sequelae are more closely related to one of the three stages of ischaemic hypoxic encephalopathy than to any specific indicator.35–37
In the analysis of nutritional determinants, neither maternal malnutrition nor obesity was associated with SDD. Several studies have indicated breast feeding as a promoting factor for child development.38–42 Univariable analysis of the current data showed that the longer the child was breast fed, the lower the prevalence of SDD; however, the statistical significance of this association was lost after adjustment for confounders. Another study also failed to detect an association between duration of breast feeding and child development at 12 months.33 However, given the moderate specificity of BSDI, it is possible that children with more severe delays were detected to the expense of milder cases. It is therefore possible that children with mild SDD, usually related to insufficient stimulation, would benefit the most from breast feeding. It is also possible that the benefits of breast feeding in terms of cognitive skills may emerge only at a later age. Recent studies have demonstrated that the interaction between individual genetic characteristics and environmental factors can play a role in child intelligence.43 It could also be possible that maternal recall of breast-feeding duration was not accurate. However, a review study reported that maternal recall of breast-feeding duration is reliable, mainly when information is collected with a time interval lower than 3 years.44 In the 2004 Pelotas Birth Cohort, data on breast feeding was obtained from follow-ups at 3, 12 and 24 months of age, very close to the moment of weaning.
History of hospital admission has been shown to be a risk factor for SDD in studies of preterm and LBW babies.45,46 In the present study, this variable was associated with the outcome even after control for confounders. The frequency of children hospitalised at least once during their first year of life was 19.2%.
Children with a history of non-febrile convulsions in the first 2 years of life were 2.5 times more likely to show SDD; however, in the multivariable analysis, the inclusion of the variable SDD at 12 months to the model turned this association statistically non-significant. Another study reported non-association between non-febrile convulsions in the first 2 years and developmental delay.47 The present study also provides support for the benign character of febrile convulsions, which were not associated with the outcome in either univariable or multivariable analysis.
In the current study, prevalence of SDD was 3.3% at age 24 months, whereas prevalence of SDD at 12 months was about 10%, showing that the trajectory is to improve with time across all domains of development. No specific interventions to manage developmental issues were delivered to children that were positive at the 12-month screening. These children continued to receive the usual paediatric care from the health system of the city. From children who screened positive at 12 months, 15.6% [95% CI 11.9, 19.3] remained positive for SDD at 24 months. Further analyses showed that the following were prognostic factors for persistence of SDD: Apgar 5′ <7, low socio-economic level, intergestational interval <24 months, breast-feeding duration ≤6 months and not having been told stories in the previous 2 weeks (unpublished data).48
Among environmental variables related to stimulation, having been told stories in the previous week and presence of children's literature (books, comic books) in the household were found to be highly protective, even after confounder control. This finding is potentially relevant for intervention purposes, since children's literature was absent from almost half of the households. However, this may be due to reverse causality, i.e. children without developmental delay may request more attention from their parents, including asking them to tell them stories, than children with developmental delay.
As to exposure to television, the American Academy of Pediatrics recommended in 2001 that children under the age of 2 years not watch television.49 Several studies have shown a negative effect of duration of exposure to television on child cognitive development.50,51 In the current study no association was found between television viewing and child development. However, a distinction must be made between programmes created for adults and those created for children. It is possible that the content of the television programmes watched may determine what influence television has on child development.52
Another analysis of the 2004 Pelotas Birth Cohort, aiming to examine child development at 2 years of age and its psychosocial determinants, employed five markers of cognitive stimulation (whether someone read or told a story to the child; whether the child went to a park or playground; whether the child went to some other people's houses; whether the child watched TV; and whether the child had a story book) that were recorded and summed in a score ranging from 0 to 5.53 This analysis found that child development was strongly associated with socio-economic position, maternal schooling and stimulation. Having been told a story and owning a book were the least frequent markers among children with low scores.
Conclusion
Identifying risk factors is important for establishing policies for prevention of developmental delay. Local studies aimed at identifying risk factors play an important role in the establishment of intervention strategies.1 The present results suggest certain public policies for prevention of developmental delay. These include increasing the number of antenatal care appointments, increasing spacing between pregnancies, reducing preterm delivery and improving the quality of care at delivery. Encouraging the practice of telling or reading stories and improving the availability of children's literature in the household are a feasible, perhaps less costly intervention, that deserve to be formally tested to prevent developmental delay.
Acknowledgments
This article is based on data from the study ‘Pelotas Birth Cohort, 2004’ conducted by the Postgraduate Program in Epidemiology at Universidade Federal de Pelotas. The 2004 birth cohort study is currently supported by the Wellcome Trust Initiative entitled Major Awards for Latin America on Health Consequences of Population Change. Previous phases of the study were supported by the World Health Organization, National Support Program for Centers of Excellence (PRONEX), the Brazilian National Research Council (CNPq), the Brazilian Ministry of Health and the Children's Mission.
References
- 1.Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shonkoff JP, Phillips DA, National Research Counical and Institute of Medicine, editors. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 3.Werner EE. Protective factors and resilience. In: Shonkoff JP, Meisels SJ, editors. Handbook of Early Childhood Intervention. 2nd. Cambridge: Cambridge University Press; 2000. pp. 115–134. [Google Scholar]
- 4.Developmental surveillance and screening of infants and young children. Pediatrics. 2001;108:192–196. doi: 10.1542/peds.108.1.192. [DOI] [PubMed] [Google Scholar]
- 5.Werner EE, Honzik MP, Smith RS. Prediction of intelligence and achievement at ten years from twenty months pediatric and psychologic examinations. Child Development. 1968;39:1063–1075. [PubMed] [Google Scholar]
- 6.Als H, Duffy FH, McAnulty GB, Rivkin MJ, Vajapeyam S, Mulkern RV, et al. Early experience alters brain function and structure. Pediatrics. 2004;113:846–857. doi: 10.1542/peds.113.4.846. [DOI] [PubMed] [Google Scholar]
- 7.Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007;369:145–157. doi: 10.1016/S0140-6736(07)60076-2. [DOI] [PubMed] [Google Scholar]
- 8.Newborg J, Stock JR, Wnek L, Guidubaldi J, Svinicki J. Battelle Developmental Inventory. Itasca, IL: Riverside Publishing; 1988. [Google Scholar]
- 9.Berls AT, McEwen IR. Battelle developmental inventory. Physical Therapy. 1999;79:776–783. [PubMed] [Google Scholar]
- 10.Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. International Journal of Epidemiology. 1997;26:224–227. doi: 10.1093/ije/26.1.224. [DOI] [PubMed] [Google Scholar]
- 11.Halpern R, Giugliani ER, Victora CG, Barros FC, Horta BL. [Risk factors for suspicion of developmental delays at 12 months of age] Jornal De Pediatria. 2000;76:421–428. doi: 10.2223/jped.88. (In Portuguese) [DOI] [PubMed] [Google Scholar]
- 12.Deave T, Heron J, Evans J, Emond A. The impact of maternal depression in pregnancy on early child development. BJOG. 2008;115:1043–1051. doi: 10.1111/j.1471-0528.2008.01752.x. [DOI] [PubMed] [Google Scholar]
- 13.Critério Padrão De Classificação Econômica Brasil/2008. São Paulo: Associação Brasileira de Empresas de Pesquisa; 2007. [Google Scholar]
- 14.Critério De Classificação Econômica Brasil. Dados Com Base No Levantamento Sócio Econômico – 2000. São Paulo: IBOPE; 2003. [Google Scholar]
- 15.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2003. National Vital Statistics Reports. 2005;54:1–116. [PubMed] [Google Scholar]
- 16.Williams RL, Creasy RK, Cunningham GC, Hawes WE, Norris FD, Tashiro M. Fetal growth and perinatal viability in California. Obstetrics and Gynecology. 1982;59:624–632. [PubMed] [Google Scholar]
- 17.Barros AJ, da Silva dos Santos I, Victora CG, Albernaz EP, Domingues MR, Timm IK, et al. [The 2004 Pelotas birth cohort: methods and description] Revista De Saude Publica. 2006;40:402–413. doi: 10.1590/s0034-89102006000300007. [DOI] [PubMed] [Google Scholar]
- 18.WHO Child Growth Standards: Methods and Development Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age. Geneva: WHO; 2007. [Google Scholar]
- 19.Cox J, Holden J, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 20.Santos IS, Matijasevich A, Tavares BF, Barros AJ, Botelho IP, Lapolli C, et al. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in a sample of mothers from the 2004 Pelotas Birth Cohort Study. Cadernos de Saude Publica. 2007;23:2577–2588. doi: 10.1590/s0102-311x2007001100005. [DOI] [PubMed] [Google Scholar]
- 21.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Medical Research Methodology. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pilz EM, Schermann LB. [Environmental and biological determinants of neuropsychomotor development in a sample of children in Canoas/RS] Ciencia & Saude Coletiva. 2007;12:181–190. doi: 10.1590/s1413-81232007000100021. [DOI] [PubMed] [Google Scholar]
- 23.Hediger ML, Overpeck MD, Ruan WJ, Troendle JF. Birthweight and gestational age effects on motor and social development. Paediatric and Perinatal Epidemiology. 2002;16:33–46. doi: 10.1046/j.1365-3016.2002.00393.x. [DOI] [PubMed] [Google Scholar]
- 24.Campbell TF, Dollaghan CA, Rockette HE, Paradise JL, Feldman HM, Shriberg LD, et al. Risk factors for speech delay of unknown origin in 3-year-old children. Child Development. 2003;74:346–357. doi: 10.1111/1467-8624.7402002. [DOI] [PubMed] [Google Scholar]
- 25.Braun JM, Daniels JL, Kalkbrenner A, Zimmerman J, Nicholas JS. The effect of maternal smoking during pregnancy on intellectual disabilities among 8-year-old children. Paediatric and Perinatal Epidemiology. 2009;23:482–491. doi: 10.1111/j.1365-3016.2009.01056.x. [DOI] [PubMed] [Google Scholar]
- 26.Rijken M, Wit JM, Le Cessie S, Veen S. The effect of perinatal risk factors on growth in very preterm infants at 2 years of age: the Leiden Follow-Up Project on Prematurity. Early Human Development. 2007;83:527–534. doi: 10.1016/j.earlhumdev.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Stoelhorst GM, Martens SE, Rijken M, Van Zwieten PH, Zwinderman AH, Wit JM, et al. Behaviour at 2 years of age in very preterm infants (gestational age <32 weeks) Acta Paediatrica. 2003;92:595–601. [PubMed] [Google Scholar]
- 28.Brown NC, Doyle LW, Bear MJ, Inder TE. Alterations in neurobehavior at term reflect differing perinatal exposures in very preterm infants. Pediatrics. 2006;118:2461–2471. doi: 10.1542/peds.2006-0880. [DOI] [PubMed] [Google Scholar]
- 29.Gutbrod T, Wolke D, Soehne B, Ohrt B, Riegel K. Effects of gestation and birth weight on the growth and development of very low birthweight small for gestational age infants: a matched group comparison. Archives of Disease in Childhood. Fetal and Neonatal Edition. 2000;82:208–214. doi: 10.1136/fn.82.3.F208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vohr BR, Wright LL, Poole WK, McDonald SA. Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks' gestation between 1993 and 1998. Pediatrics. 2005;116:635–643. doi: 10.1542/peds.2004-2247. [DOI] [PubMed] [Google Scholar]
- 31.Silva PA, Buckfield P, Spears GF. Mode of delivery and developmental characteristics in a thousand Dunedin three year olds: a report from the Dunedin Multidisciplinary Child Development Study. New Zealand Medical Journal. 1979;89:79–81. [PubMed] [Google Scholar]
- 32.Wadhawan R, Vohr BR, Fanaroff AA, Perritt RL, Duara S, Stoll BJ, et al. Does labor influence neonatal and neurodevelopmental outcomes of extremely-low-birth-weight infants who are born by cesarean delivery? American Journal of Obstetrics and Gynecology. 2003;189:501–506. doi: 10.1067/s0002-9378(03)00360-0. [DOI] [PubMed] [Google Scholar]
- 33.Slykerman RF, Thompson JM, Clark PM, Becroft DM, Robinson E, Pryor JE, et al. Determinants of developmental delay in infants aged 12 months. Paediatric and Perinatal Epidemiology. 2007;21:121–128. doi: 10.1111/j.1365-3016.2007.00796.x. [DOI] [PubMed] [Google Scholar]
- 34.Grantham-McGregor SM, Lira PI, Ashworth A, Morris SS, Assuncao AM. The development of low birth weight term infants and the effects of the environment in northeast Brazil. Journal of Pediatrics. 1998;132:661–666. doi: 10.1016/s0022-3476(98)70357-9. [DOI] [PubMed] [Google Scholar]
- 35.Robertson CM, Finer NN. Long-term follow-up of term neonates with perinatal asphyxia. Clinics in Perinatology. 1993;20:483–500. [PubMed] [Google Scholar]
- 36.Msall ME, Bier JA, LaGasse L, Tremont M, Lester B. The vulnerable preschool child: the impact of biomedical and social risks on neurodevelopmental function. Seminars in Pediatric Neurology. 1998;5:52–61. doi: 10.1016/s1071-9091(98)80019-3. [DOI] [PubMed] [Google Scholar]
- 37.Nelson KB, Ellenberg JH. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36–44. [PubMed] [Google Scholar]
- 38.Quinn PJ, O'Callaghan M, Williams GM, Najman JM, Andersen MJ, Bor W. The effect of breastfeeding on child development at 5 years: a cohort study. Journal of Paediatrics and Child Health. 2001;37:465–469. doi: 10.1046/j.1440-1754.2001.00702.x. [DOI] [PubMed] [Google Scholar]
- 39.Goldman AS, Hopkinson JM, Rassin DK. Benefits and risks of breastfeeding. Advances in Pediatrics. 2007;54:275–304. doi: 10.1016/j.yapd.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 40.Sacker A, Quigley MA, Kelly YJ. Breastfeeding and developmental delay: findings from the millennium cohort study. Pediatrics. 2006;118:e682–e689. doi: 10.1542/peds.2005-3141. [DOI] [PubMed] [Google Scholar]
- 41.Anderson JW, Johnstone BM, Remley DT. Breast-feeding and cognitive development: a meta-analysis. American Journal of Clinical Nutrition. 1999;70:525–535. doi: 10.1093/ajcn/70.4.525. [DOI] [PubMed] [Google Scholar]
- 42.Drane DL, Logemann JA. A critical evaluation of the evidence on the association between type of infant feeding and cognitive development. Paediatric and Perinatal Epidemiology. 2000;14:349–356. doi: 10.1046/j.1365-3016.2000.00301.x. [DOI] [PubMed] [Google Scholar]
- 43.Caspi A, Williams B, Kim-Cohen J, Craig IW, Milne BJ, Poulton R, et al. Moderation of breastfeeding effects on the IQ by genetic variation in fatty acid metabolism. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:18860–18865. doi: 10.1073/pnas.0704292104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li R, Scanlon KS, Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews. 2005;63:103–110. doi: 10.1111/j.1753-4887.2005.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 45.Were FN, Bwibo NO. Two year neurological outcomes of very low birth weight infants. East African Medical Journal. 2006;83:243–249. doi: 10.4314/eamj.v83i5.9429. [DOI] [PubMed] [Google Scholar]
- 46.Feldman HM, Ploof DL, Hofkosh D, Goehring EL., Jr Developmental needs of infants and toddlers who require lengthy hospitalization. American Journal of Diseases of Children. 1993;147:211–215. doi: 10.1001/archpedi.1993.02160260101034. [DOI] [PubMed] [Google Scholar]
- 47.Tuchman RF, Moshe SL, Rapin I. [Neurodevelopmental disorders and epilepsy.] Revista de Neurologia. 2005;40(Suppl 1):S3–S10. (In Spanish) [PubMed] [Google Scholar]
- 48.Moura DR, Costa JC, Santos IS, Barros AJD, Matijasevich A, Halpern R, et al. Natural history of suspected developmental delay between 12 and 24 months of age in the 2004 Pelotas birth cohort. Journal of Paediatrics and Child Health. 2010 doi: 10.1111/j.1440-1754.2010.01717.x. in press. [DOI] [PubMed] [Google Scholar]
- 49.American Academy of Pediatrics: children, adolescents and television. Pediatrics. 2001;107:423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 50.Wachs TD. Ambient background noise and early development. Children's Environments Quarterly. 1986;3:23–33. [Google Scholar]
- 51.Carew JV. Experience and the development of intelligence in young children at home and in day care. Monographs of the Society for Research in Child Developments. 1980;45:N6–N7. Serial No. 187. [PubMed] [Google Scholar]
- 52.Anderson DR, Pempek TA. Television and very young children. American Behavioral Scientist. 2005;48:505–522. [Google Scholar]
- 53.Barros AJ, Matijasevich A, Santos IS, Halpern R. Child development in a birth cohort: effect of child stimulation is stronger in less educated mothers. International Journal of Epidemiology. 2010;39:285–294. doi: 10.1093/ije/dyp272. [DOI] [PMC free article] [PubMed] [Google Scholar]


