Abstract
The symptoms of bipolar disorder affect and are affected by the functioning of family environments. Little is known, however, about the stability of family functioning among youth with bipolar disorder as they cycle in and out of mood episodes. This study examined family functioning and its relationship to symptoms of adolescent bipolar disorder, using longitudinal measures of family cohesion, adaptability and conflict. Parent and adolescent-reported symptom and family functioning data were collected from 58 families of adolescents with bipolar disorder (mean age =14.48 + 1.60; 33 female, 25 male) who participated in a 2-year randomized trial of family-focused treatment for adolescents (FFT-A). Cohesion and adaptability scores did not significantly change over the course of the study. Parent-reported conflict prior to psychosocial treatment moderated the treatment responses of families, such that high-conflict families participating in FFT-A demonstrated greater reductions in conflict over time than low-conflict families. Moreover, adolescent mania symptoms improved more rapidly in low-conflict than in high-conflict families. For all respondents, cohesion, adaptability, and conflict were longitudinally correlated with adolescents’ depression scores. Finally, decreases in parent-reported conflict also predicted decreases in adolescents’ manic symptoms over the 2-year study. Findings suggest that family cohesion, adaptability, and conflict may be useful predictors of the course of adolescent mood symptoms. Family conflict may be an important target for family intervention in early-onset bipolar disorder.
Keywords: cohesion, conflict, adaptability, expressed emotion
Bipolar disorder (BD) affects and is affected by the environments in which patients relapse and recover. Functional attributes of the family environment, particularly those measured following an illness episode, have been found to be correlated with symptom severity in bipolar disorder (BD) and major depressive disorder in both cross-sectional and longitudinal research. High levels of expressed emotion (EE; critical, hostile, or emotionally overinvolved attitudes) among caregivers, negative affective communication styles, and low levels of maternal warmth have all been associated with more severe mood disorder symptoms in youth (e.g., Asarnow, Tompson, Woo & Cantwell, 2001; Birmaher, Ryan & Williamson, 1996; Dietz et al., 2008; Geller, Tillman, Bolhofner & Zimerman, 2008; Silk, Ziegler, Whalen, Dahl, Ryan, Dietz et al., 2009) and adults (e.g., Miklowitz, Goldstein, Nuechterlein, Snyder & Mintz, 1988; O’Connell, Mayo, Flatow, Cuthbertson & O’Brien, 1991; Priebe, Wildgrube & Muller-Oerlinghausen, 1989; Simoneau, Miklowitz, Richards, Saleem & George, 1999; Yan, Hammen, Cohen, Daley & Henry, 2004; for a review, see Miklowitz & Johnson, 2009).
Research suggests that dimensions of family functioning drawn from family systems theory – specifically, familial conflict, adaptability (flexibility in discipline, negotiation, roles, and leadership) and cohesion (close but permeable family boundaries, emotional closeness between family members, and amount of time spent together; Robertson, Kutcher, Bird & Grasswick, 2000) – may be correlated with symptom severity in adolescent BD. Families of patients with BD report lower levels of family cohesion and adaptability and higher levels of conflict than families of healthy children or population norms (Belardinelli, Hatch, Olvera, Rene, Fonseca, Caetano et al., 2008; Robertson et al., 2001; Sullivan & Miklowitz, 2010). Over an 8-week study of pharmacotherapy, youth from lower conflict families demonstrated greater improvement in depressed symptoms than youth from high conflict families (Townsend, Demeter, Youngstrom, Drotar & Findling, 2007). Esposito-Smythers and colleagues (2006) demonstrated that youth with lower levels of family cohesion had greater rates of comorbidity with attention deficit and hyperactivity disorder, oppositional defiant disorder and other disorders that frequently are co-diagnosed with BD. Finally, several studies find that maladaptive levels of family functioning characterize youth who are genetically predisposed to BD (Chang, Blasey, Ketter & Steiner, 2001; Du Rocher Schudlich, Youngstrom, Calabrese & Findling, 2008; Romero, DelBello, Soutullo, Stanford & Strakowski, 2005).
Our understanding of family constructs such as conflict, cohesion and adaptability as they apply to childhood mood disorders is limited. With the exception of Townsend and colleague’s (2007) eight-week study interval, investigations of the associations between family functioning and BD symptoms have been cross-sectional. For the families of adolescents with BD, we do not know if family functioning variables remain stable or change over time, or how longitudinal trajectories of family functioning scores covary with the cyclic nature of BD symptoms. Furthermore, we do not know if family cohesion, adaptability, or conflict change in response to participation in family therapy.
In this study, we examined parent- and adolescent-reported family cohesion, adaptability, and conflict in the context of a two-year randomized trial of family-focused treatment for adolescents (FFT-A; Miklowitz et al., 2008). In this trial, FFT-A was shown to be effective in combination with pharmacological treatment in stabilizing depressive symptoms, delaying mood disorder recurrences, and reducing the amount of time depressed among adolescents with BD. FFT-A emphasizes the role of family psychoeducation, communication training and problem-solving skills training in enhancing the protective effects of the family environment after an episode of mania or depression. The regular collection of adolescent symptom and family functioning data in the trial (i.e., every 3-6 months) presented an opportunity to examine the relationships between symptoms, family functioning, and family treatment.
This study had four main objectives. First, we examined the longitudinal course of parent- and adolescent-reported cohesion, adaptability and conflict over a 2-year period. We hypothesized that levels of family functioning would improve over time (i.e. levels of family conflict would decrease and levels of adaptability and cohesion would increase), and that pretreatment levels of these variables would influence their longitudinal trajectory. Second, we predicted that baseline, pretreatment levels of family functioning would predict the course of mania and depression symptoms among youth over time. Third, we hypothesized that longitudinal improvements in family functioning would be correlated with improvements in adolescents’ symptoms of depression and mania. Finally, we examined the influence of treatment on these relationships. We predicted that improvements in family functioning would be more pronounced among families in intensive family treatment (FFT-A) than among families enrolled in briefer family psychoeducation (enhanced care, or EC).
MATERIAL AND METHODS
Participants
Adolescents with bipolar disorder and their family members were enrolled in a two-site randomized trial of FFT-A (21 family sessions over 9 months) and pharmacotherapy in comparison with EC (3 weekly sessions of family education plus case management for 9 months) and pharmacotherapy. Referrals to the study came from private and public inpatient and outpatient facilities near Boulder, CO or Pittsburgh, PA. Eligible adolescents met the following criteria: 1) between the ages of 12 years, 0 months and 17 years, 11 months; 2) Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV; American Psychiatric Association, 2000) diagnosis of bipolar I, bipolar II, or bipolar not otherwise specified (NOS) disorder, as revealed by both structured diagnostic interview and separate physician evaluation; 3) at least one hypomanic, manic, mixed or depressive episode within the past three months; 4) family members (at minimum, one parent) were available for treatment sessions; and 5) willingness of the adolescent to take mood stabilizing medications and meet with a study psychiatrist throughout the 2-year study. Participants were excluded if they met current (i.e., previous 3 months) DSM-IV criteria for a substance abuse or dependence disorder, substance-induced mood disorder, pervasive developmental disorders, schizoaffective disorder, or life-threatening eating disorders. Additional information regarding eligibility criteria, adolescent diagnosis and intake procedures is given in Miklowitz et al. (2008).
This study was approved by the institutional review boards of both universities. Participating adolescents and family members signed informed assent and consent forms after receiving a full explanation of the study procedures.
Procedures
Diagnostic assessments
Children’s current/lifetime diagnoses were assessed with the Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime Version (KSADS-PL; Kaufman et al., 1997), based on separate child and parent interviews. The mood sections of the KSADS-PL were replaced with the KSADS Mania Rating Scale (MRS; Axelson et al., 2003) and Depression Rating Scale (DRS; Chambers et al., 1985) and covered the most severe 1-2 weeks in the month prior to intake, and separately, the most severe 1-2 weeks over the adolescent’s lifetime. These interviews, containing items rated on 1-6 scales of severity, offer more extensive coverage of affective symptoms and a greater range of response choices than the traditional KSADS-PL and supplements (Axelson et al., 2006). MRS and DRS final scores were based on a consensus of parent and adolescent reports in the interviews. Interrater reliability for KSADS DRS and MRS scores (51 ratings) were 0.97 and 0.89 (intraclass rs), respectively. Agreement on the presence or absence of any comorbid disorder was 0.70 (kappa statistic).
Questionnaire measures of family functioning
At the time of study intake, parents and adolescents completed a battery of questionnaires. The Family Adaptability and Cohesion Evaluation Scale, II (FACES-II: Olson, Russell & Sprenkle, 1983; Olson & Tiesel, 1991), a well-validated self-report measure, contains 30 items regarding family behaviors, which are rated 1 (almost never) to 5 (almost always) on Likert-type scales. Items are divided between cohesion and adaptability scales, with lower scale scores indicating more impairment. Scores on the cohesion (range: 15-80) and adaptability (range: 15-70) scales are divided between four levels of family functioning (for cohesion: disengaged, separated, connected, and very connected; for adaptability: rigid, structured, flexible, and very flexible). Typical items from the cohesion subscale include “In our family, everyone goes his/her own way” and “Family members feel very close to each other”. Typical items from the adaptability subscale include “Our family tries new ways of dealing with problems” and “When problems arise, we compromise”. When summed, these scales indicate the degree to which a family is ‘balanced’. Previous research has suggested that these dimensions are most useful when analyzed separately, rather than combined as a summary of functioning (e.g. Place, Hulsmeier, Brownrigg & Soulsby, 2005). Cronbach’s alpha for parent-reported FACES-II scores was .71. Cronbach’s alpha for adolescent-reported FACES-II scores was .86.
The Conflict Behavior Questionnaire (CBQ; Prinz, Foster, Kent & O’Leary, 1979) is a self-report measure of interpersonal conflict within the family. Respondents answer “true/false” questions regarding their relationship with their offspring or parent (e.g. the mother about the adolescent or the child about the father). Typical items include, “My child is easy to get along with” or “My mother thinks my opinions don’t count”. Responses are assigned a score of 0 or 1, dependent on whether or not the response reflects conflict; items are summed to generate a total conflict score (range: 0-20; higher scores indicate greater conflict). Internal consistency (Cronbach’s alpha) of the CBQ was .86 for parent scores and .88 for adolescent scores in this study. Mean CBQ scores for healthy and distressed families are provided elsewhere (Sullivan & Miklowitz, 2010).
Pharmacological and psychosocial treatment
Following their baseline assessments, eligible patients and families were randomly assigned to FFT-A (50%) or EC (50%), based on an adaptation of Efron’s biased coin toss (Begg & Iglewicz, 1980). Treatment assignments were stratified by study site.
A standard pharmacological protocol was implemented by study psychiatrists as soon as the patient became eligible for the study. Study physicians, who were not involved in any of the psychosocial treatments, determined the most effective psychopharmacological profile for each subject, according to the best practices known at the time of treatment. Additional pharmacotherapy for comorbid disorders (e.g., psychostimulants) was permitted. Physician appointments were scheduled approximately monthly, or more frequently if needed throughout the 2-year duration of the study.
Family-focused treatment for adolescents (FFT-A)
FFT-A sessions were administered over 21 hour-long sessions in 9 months, and included the patient, at least one parent, and any available siblings. Treatment goals were addressed through three modules. Within the psychoeducation module, families were educated about the symptoms and management of adolescent BD. The communication enhancement training module included instruction and practice of skills such as expressing positive feelings, active listening, and making positive requests for change. Sessions of the problem solving module focused on defining specific family disagreements, discussing and evaluating potential solutions, and discussing implementation plans. Up to 3 additional maintenance sessions were scheduled throughout the remainder of the study (up to 24 months) and focused on reiteration of FFT-A goals and skills.
Enhanced care treatment (EC)
This treatment condition included three weekly family sessions focused on education about BD, development of coping strategies, and relapse prevention. Content from these sessions was similar to that covered in the psychoeducational module of FFT-A. Additional case management or crisis sessions were available as needed throughout the remainder of the study (up to 24 months). This condition was intended to reflect the brief, education-focused therapy typically provided in the community. Therapist training and adherence measurement are described in detail elsewhere (Miklowitz et al., 2008).
Follow up assessments
Independent study evaluators, blind to treatment condition, completed follow up assessments with adolescents and at least one parent throughout the 2-year study. Assessments were conducted every 3 months during the first year (months 3, 6, 9 and 12) and every 6 months in year 2. These follow up assessments included administration of the MRS and DRS, measures of social functioning and medication adherence, and the family functioning questionnaires described above. Follow up MRS and DRS interviews focused on the most symptomatic 1-2 weeks in the month prior to the follow up appointment. Completion of family functioning questionnaires was somewhat inconsistent during these follow up appointments, particularly for appointments taking place in the second year of the study (Table 1). Follow up participation did not differ across treatment groups. (See Miklowitz et al. [2008] for additional information regarding the follow-up procedures)1.
Table 1. Family Functioning Protocols Completed by Follow Up Appointment.
| Family Functioning Questionnaire |
Follow Up Assessment: Mean Score (standard deviation, number of completed protocols) | ||||||
|---|---|---|---|---|---|---|---|
| Intake | 3 mo | 6 mo | 9 mo | 12 mo | 18mo | 24mo | |
| Parent Report | |||||||
| FACES-IIa:Cohesion | 54.5(10.1;35) | 56.3(9.6;33) | 55.5(9.4;32) | 54.5(9.9,29) | 53.7(9.3;25) | 53.0(11.1;16) | 55.4(5.1;12) |
| FACES-II:Adaptability | 46.5(6.4;35) | 47.0(5.5;32) | 46.8(8.2;32) | 46.5(6.6;29) | 47.7(5.6;25) | 47.9(6.4;16) | 47.4(3.8;12) |
| CBQb | 12.1(5.3;46) | 9.9(6.6;40) | 9.4(6.2;38) | 9.7(5.9;34) | 8.8(6.2;32) | 8.6(6.1;21) | 6.7(6.1;18) |
| Adolescent Report | |||||||
| FACES-II:Cohesion | 51.1(11.7;39) | 52.4(14.8;34) | 54.3(12.2;29) | 50.1(11.3;29) | 52.2(11.7;27) | 51.8(10.8;14) | 47.8(11;13) |
| FACES-II:Adaptability | 39.9(10.3;39) | 43.9(12.0;34) | 45.6(12.3;29) | 43.5(10.3;29) | 44.0(10.7;27) | 42.7(8.7;15) | 42.2(9.6;13) |
| CBQ | 6.9(5.4;45) | 5.4(5.6;40) | 4.6(4.7;34) | 5.2(5.4;35) | 4.9(4.9;33) | 5.1(5.5;23) | 4.8(4.9;19) |
FACES-II = Family Adaptability and Cohesion Evaluation Scales -II
CBQ = Conflict Behavior Questionnaire
STATISTICAL ANALYSIS
Family adaptability and cohesion data were determined from FACES-II protocols, and family conflict scores were calculated from CBQ protocols for each assessment point. For each family, a single parent score and single adolescent score was determined for each variable at each time point. When data were available from a single parent, or from an adolescent regarding a single parent, the raw data were used from the relevant questionnaire. When data were available from two parents, or from an adolescent regarding both parents, the mean of the two reported scores was calculated to represent the parent and adolescent scores used in the analyses. Although not statistically ideal, this procedure was preferable to selecting one parent’s scores when two parent reports were available, or selecting one from two available adolescent responses, as we did not have sufficient information to determine which of the two scores would best represent the family’s score (Baucom & Sher, 1987).
The majority of the families in this sample had maladaptive scores on the CBQ and FACES-II at baseline (Sullivan & Miklowitz, 2010). For this reason, use of the measure-defined cutoff scores (based on normative and non-psychiatric distressed samples) created imbalanced group distributions. Instead, we calculated median splits of intake (baseline) CBQ and FACES-II scores to categorize families as either high or low in the areas of conflict, cohesion, and adaptability at study entry. These medians were different for parent-rated and adolescent-rated scale scores. For parents’ reports, families whose raw scores were above 12 on the CBQ were categorized as high conflict; families with scores above 12 were categorized as high-conflict. Similarly, families with parent-reported cohesion scores lower than 55 (a score falling within the ‘separated’ category of this subscale) were classified as low-cohesion. Adaptability scores lower than 46 (‘structured’) were classified as low in adaptability. Adolescents’ scores were generally lower than parents’ scores and were differently distributed. Thus, we used different cutoff scores to classify families when using adolescents’ versus parents’ FACES-II or CBQ scores. Adolescent-reported conflict scores of 6, cohesion scores of 50 (‘disengaged’), or adaptability scores of 39 (‘rigid’) were used as the cutoffs to separate families who were high and low on these attributes.
Multilevel analyses with restricted maximum likelihood estimation, using methods outlined by Singer and Willett (2003; see also Raudenbush & Bryk, 2002), were used to examine longitudinal changes in family functioning, longitudinal changes in patient symptoms (MRS and DRS ratings, based on a consensus of parent and adolescent reports), and relationships between the two. Specific models used for each analysis are outlined below. The Proc Mixed application in the SAS/STAT software (SAS Institute Inc., Cary, North Carolina) was used to model the effects of time, treatment condition and baseline family functioning classification (high versus low level of conflict, adaptability, or cohesion). Degrees of freedom used in model denominators were determined as outlined by Kenward and Roger (1997).
To investigate the longitudinal relationship between parent and adolescent ratings of family functioning, we modeled parent-rated family functioning as a function of longitudinal adolescent-reported family functioning and linear time (centered). Linear time and adolescent-reported family functioning were within-family predictors, and were allowed random intercepts and slopes across families. To compare parent- and adolescent-reported scores, a difference score was calculated for each time point with parent and adolescent data. This difference score was modeled as a function of linear time (centered). Once again, random intercepts and slopes for linear time were allowed.
Longitudinal changes in family functioning variables were modeled as a function of intake categorization (e.g., high- or low-cohesion), treatment condition, centered linear time and the 2-way and 3-way interactions between these variables. Time was a within-family predictor, while treatment and intake categorization were between-family predictors.
To investigate the relationship between baseline family functioning and changes in mood symptoms, we modeled symptoms as a function of intake categorization, treatment condition, centered linear time, and their 2-way and 3-way interactions. Time was a within-family predictor, while treatment and intake categorization were between-family predictors. Finally, we modeled symptoms as a function of longitudinal family functioning, treatment condition, centered linear time, and the 2-way interaction between longitudinal family functioning and treatment condition. Time and family functioning were within-family predictors; treatment condition was a between-family predictor. Random intercepts and slopes for linear time and longitudinal family functioning were modeled as a function of treatment condition.
RESULTS
Sample Demographics
A total of 58 adolescents (38 with BD I, 6 with BD II, and 14 with BD NOS) and their families participated in the treatment study. Demographic data are presented in Table 2. Further data on the sample, including a family participation Flowchart, and comparisons between site and other demographic variables, are given elsewhere (Miklowitz et al., 2008).
Table 2. Sample Demographic and Diagnostic Characteristics.
| Variable | Values | |
|---|---|---|
| Mean (SD) | ||
| Age in years | 14.48 | (1.60) |
| Depression Rating Scale Score | 24.28 | (9.46) |
| Mania Rating Scale Score | 28.59 | (9.38) |
| Session Attendance: ECa | 4.96c | (3.68) |
| Session Attendance: FFT-Ab | 19.3c | (7.8) |
| Number (%) | ||
| Sex: Female | 33 | (56.89) |
| Race: | ||
| Caucasian | 52 | (94.80) |
| African American | 1 | (1.72) |
| Native American | 1 | (1.72) |
| Asian/Pacific Islander | 1 | (1.72) |
| Biracial | 3 | (5.17) |
| Hispanic Ethnicity | 3 | (5.17) |
| Live in Dual Parent Household | 37 | (63.79) |
| Bipolar I | 38 | (65.52) |
| Bipolar II | 6 | (10.34) |
| Bipolar Not Otherwise Specified | 14 | (24.14) |
| Comorbid ADHDd diagnosis | 11 | (19.00) |
| Comorbid ODDe diagnosis | 7 | (12.10) |
| Comorbid Anxiety diagnosis | 2 | (3.5) |
EC: Enhanced Care
FFT-A: Family-Focused Treatment for Adolescents
Means for FFT-A and EC conditions include additional crisis sessions conducted throughout the 9 months of active treatment
ADHD: attention deficit hyperactivity disorder
ODD: oppositional defiant disorder
Comparison of Patients with Completed or Missing Family Functioning Measures
Baseline patient symptom and demographic data for completed and missing protocols were compared (see Table 1). Initial depression severity was greater for adolescents who did not complete a CBQ at study entry, as compared to adolescents who did complete a CBQ (F(1,58) = 6.55, p < .05). All other comparisons between participants with missing versus completed family questionnaires, including intake symptom severity, gender, race, and age, were nonsignificant (for all, ps > .05).
Comparison of Parent- and Adolescent-Reported Scores
For all family functioning variables, adolescent-reported scores significantly predicted parent-reported scores (cohesion: β=.21, F(1,153)=16.91, p < .0001; adaptability: β=.17 F(1,120)=16.06, p=.0001; conflict: β=.38, F(1,23.6)=12.59, p=.002). However, adolescent-reported scores were consistently lower than parent-reported scores for all family functioning variables (cohesion: β=3.22, F(1,37.9)=3.96, p =.05; adaptability: β=4.14, F(1,35.9)=11.36, p=.002; conflict: β=3.86, F(1,38.9)=18.75, p=.0001). Given this distinction between adolescent- and parent-reported scores, we analyzed their data separately.
Family Functioning Over Time
For both parent and adolescent respondents, neither cohesion nor adaptability changed across the 2-year study interval as a function of time (p > .10 for all). In addition, two- and three-way interactions including linear change, intake categorization, or treatment condition were not significant predictors of parent- or adolescent-reported cohesion or adaptability (p >.10 for all).
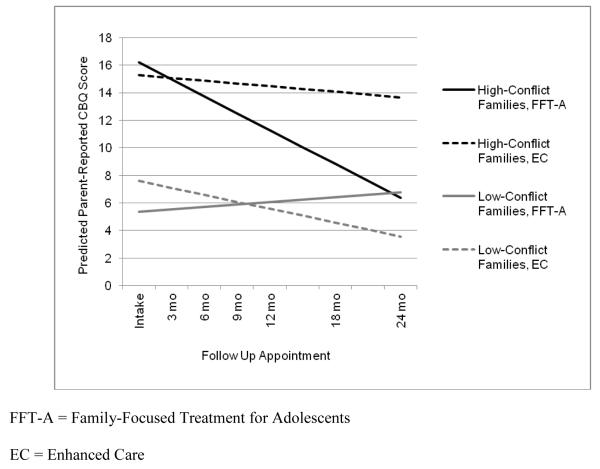
Parent-reported conflict levels dropped significantly over the course of the study, independent of treatment condition and baseline levels of conflict (β = −.15, F(1,19.4)=9.07, p=.007). However, a 3-way interaction between intake family categorization (high or low parent-reported conflict), treatment condition and linear time significantly predicted parent-reported conflict (β = −.57, F(1, 19.4)=8.50, p=.009; Fig. 1). Specifically, for parents who reported high levels of conflict at baseline, parent conflict scores dropped significantly among those in FFT-A (β = −0.40, F(1,9.53)=12.80, p=.005), but not among those in EC (β = −0.11, F(1,6.8)=1.10, p=.33). For families classified as low-conflict, the linear time change (β = −0.04, F(1,5.33)=.27, p=.62) and treatment condition terms (β = 0.62, F(1,11.8)=.09, p=.77) did not significantly predict changes in parent-reported conflict scores over time.
Figure 1.
Predicted parent-reported conflict behavior questionnaire (CBQ) scores over time: By treatment and intake conflict categorization
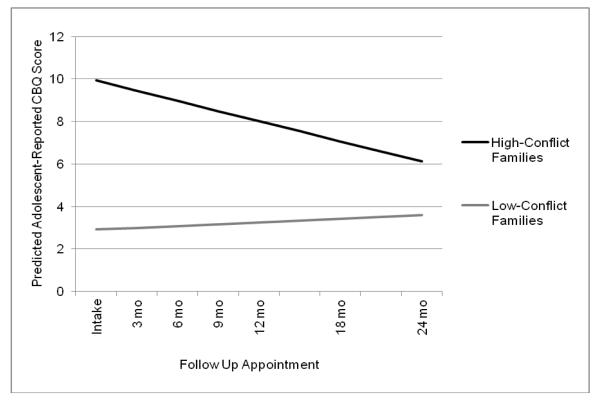
There was a significant interaction between linear time and intake categorization, based on adolescents’ baseline reports of high or low conflict, on adolescent-reported conflict at follow up (β = −.23, F(1, 20.5) = 6.03, p=.023, Fig. 2). Across treatment conditions, teen-reported conflict levels decreased over time in high-conflict families (β = −.19, F(1, 14.1) = 4.55, p=.05), but not low-conflict families (β = .03, F(1, 3.46) = .26, p=.64). The three-way interaction between linear change, intake categorization and treatment condition was not significant in models predicting adolescent-reported conflict (β = −.32, F(1, 20.5) = 2.93, p=.10).
Figure 2.
Predicted adolescent-reported conflict behavior questionnaire (CBQ) scores over time: By intake conflict categorization
Family Functioning and Consensus Ratings of Patients’ Symptoms
Pretreatment family functioning
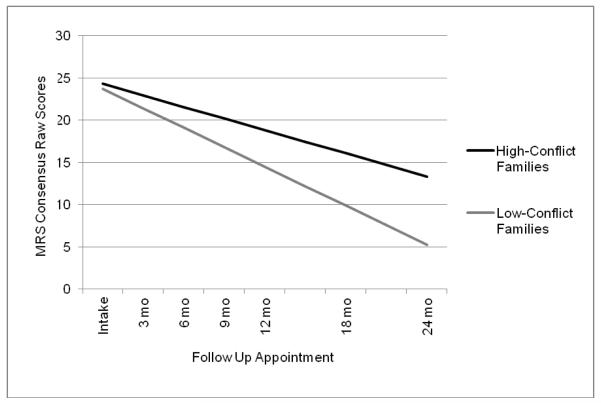
Baseline levels of parent- and adolescent-reported cohesion and adaptability did not significantly influence linear changes in either depression or mania scores. All two- and three-way interactions within these models were not significant (for all, p > .05). However, parent-reported intake categorization as high- or low-conflict significantly predicted average levels of mania over the study interval, such that adolescents in high-conflict families had higher levels of mania over time than adolescents in low-conflict families (low-conflict: M: 16.62, SD: 12.00; high-conflict: M: 19.53, SD: 10.67; F(1, 42.7) = 4.13, p=.04). Baseline levels of parent-reported conflict also predicted linear changes in mania over time (β = 0.28, F(1,229)=4.10, p=.04, Fig. 3). Specifically, mania scores decreased more rapidly in adolescents with parents who reported low conflict at baseline (β = −0.77, p<.0001), as compared to those whose parents were categorized as high-conflict (β = −0.46, p<.0001). Terms testing for relationships between parent-reported intake conflict levels and depression scores were not significant (for all, p > .50).
Figure 3.
Predicted values of mania rating scale (MRS) scores over time: By baseline level of parent-reported conflict
Adolescent-reported categorization as high- or low-conflict at intake predicted average MRS scores across the 2-year study interval, with teens from high-conflict families having higher average mania scores than teens from low-conflict families (low-conflict: M: 15.46, SD: 11.23; high-conflict: M:19.73, SD:11.17; F(1,36.2)=4.41, p=.04). Baseline levels of adolescent-reported conflict, however, did not significantly predict longitudinal changes in mania scores (β=.13, F(1,196)=.73, p=.4). Adolescent-reported intake categorization of family conflict was not significantly related to changes in their depression scores (for all, p > .10).
Longitudinal measurement of family functioning
Results are presented in Table 3. Longitudinal ratings of family cohesion from both parents and adolescents were significantly related to adolescents’ depression scores over time (parent report: F(1,148)=5.02, p =.03; adolescent report: F(1,156)=9.40, p=.003), such that higher ratings of family cohesion were associated with lower depression ratings over time (Table 3). Parent and adolescent ratings of adaptability demonstrated a similar association with depression scores, although this relationship was at the trend level for parent reports of adaptability (parent report: F(1,155)=3.21, p=.07; adolescent report: F(1, 161)=5.76, p=.02). For all respondents, longitudinal ratings of cohesion and adaptability did not significantly predict adolescents’ longitudinal mania scores (for all, p >.10).
Table 3. Longitudinal Correlations between Family Functioning Variables and Adolescent Symptoms.
| Family Functioning Variable |
Depression Rating Scale β (SE) |
Mania Rating Scale β (SE) . |
|---|---|---|
| Parent Report | ||
| FACES-IIa: Cohesion | −0.25 (.11)* | −0.16 (.12) |
| FACES-II: Adaptability | −0.28 (.15) | −0.19 (.17) |
| CBQb | 0.39 (.14)** | 0.31 (.13)* |
| Adolescent Report | ||
| FACES-II : Cohesion | −0.21 (.07)** | −0.11 (.07) |
| FACES-II: Adaptability | −0.18 (.07)* | −0.07 (.08) |
| CBQ | 0.40 (.14)** | 0.18 (.15) |
= p < .05
= p < .01
FACES-II = Family Adaptability and Cohesion Evaluation Scales -II
CBQ = Conflict Behavior Questionnaire
Longitudinal changes in parent- and adolescent-reported family conflict were significantly associated with changes in adolescents’ DRS scores (parent report: F(1,101)=7.83, p=.006; adolescent report: F(1,190)=7.55, p=.007). Parent reports of conflict over time were also associated with changes in MRS scores (F(1, 96.2)=5.43, p=.02). In each of these relationships, decreasing levels of conflict were associated with decreasing levels of symptoms over time.
For all respondents, the longitudinal relationships between family functioning and patients’ symptom scores did not vary by treatment condition. Specifically, 2-way interactions between treatment condition and family functioning over time were not significant predictors of changes in depression or mania scores (for all, p > .10).
DISCUSSION
This study investigated the stability of family functioning over time, and the relationships between family functioning and mood symptoms in a sample of adolescents undergoing family treatment and pharmacotherapy for bipolar disorder. Our findings demonstrated that longitudinal measures of family functioning are associated with adolescents’ symptom levels over time. Specifically, baseline levels of family conflict predicted the severity of adolescents’ manic symptoms over time. In contrast, levels of cohesion and adaptability remained stable over time. Finally, pre-treatment parent-reported conflict scores moderated whether parents reported reductions in conflict in the more intensive family-focused treatment.
We were unable to determine the temporal order of the relationships between changes in family functioning and changes in mood symptoms. Much of the prior literature suggests that problems in the family environment may be contributing factors in the development or worsening of mood disorders (e.g., Du Rocher Schudlich et al., 2008). Alternately, it is possible that a worsening of family conflict results from the onset of mood symptoms in adolescents, rather than family factors playing a causal role in patients’ symptoms. Nonetheless, our findings suggest that family characteristics at the time that treatment begins may have a prognostic, if not necessarily a causal role in the subsequent course of the adolescent bipolar illness.
Prior analyses from this sample demonstrated that an observational measure of the family environment, expressed emotion (EE), moderated the effects of FFT-A (Miklowitz et al., 2009). Specifically, compared to patients in low-EE families, patients from high-EE families showed greater improvement in depression and mania scores over 2 years if they were treated with FFT-A than if they were treated with EC. The present study adds the observation that parent-reported family conflict during the pretreatment period moderated longitudinal changes in family conflict, such that greater decreases in conflict were seen in high-conflict families participating in FFT-A.
Parent-reported conflict at baseline also predicted the course of mania symptoms over time, such that greater levels of conflict were associated with slower decreases in manic symptoms. Similarly, Townsend and colleagues (2007) found that greater levels of family conflict predicted a poorer response among adolescents with depression to pharmacotherapy. These findings suggest that baseline family conflict may be a useful predictor of the course of symptoms in adolescent BD. Unfortunately, our limited sample size and missing data precluded directly testing the mediational pathways between baseline family functioning scores, changes in family functioning, and patients’ symptom scores over time. Longitudinal designs that include more frequent longitudinal assessments of family functioning (for example, monthly ratings of family conflict, cohesion, or adaptability) would likely be better suited to questions regarding the temporal association between putative treatment mediators and symptomatic change.
Community mental health centers with limited financial resources may be able to assess family impairment with some of the more streamlined questionnaires used in this study (for example, the CBQ) rather than the more expensive and time-intensive EE assessment. Assessments of family impairment may assist clinicians in selecting candidates for more intensive psychosocial treatment (i.e., patients in high-EE or high-conflict families). Although the present study focused on FFT-A, a number of psychosocial treatments have demonstrated efficacy in open trials with adolescent BD populations (e.g., Feeny, Danielson, Schwartz, Youngstrom & Findling, 2006; Goldstein, Axelson, Birmaher & Brent, 2007; Hlastala, Kotler, McClellan & McCauley, 2010). Replication of the current findings in larger samples undergoing a variety of psychosocial and pharmacological treatments, such as those typically given in community care centers, will be necessary to determine if family functioning measures are clinically useful predictors of treatment outcomes.
As previously reported (Sullivan & Miklowitz, 2010), average scores for cohesion and adaptability were at maladaptive levels for most families prior to their participation in the study. Contrary to our current hypothesis, these measures of family functioning did not improve from their initially maladaptive levels over the two-year study for the majority of families. Thus, the skills taught in FFT-A and EC may not strongly influence family cohesion and adaptability, at least over short-term intervals. Alternatively, self-report measures may not be sensitive to real changes that occur among families over time.
The generalizability of our findings is limited to families who were able to participate in a 2-year randomized control trial that included brief or intensive family treatment, as well as mood stabilizing medications for the adolescent. Given the requirements for study participation, our sample may have included families who were especially distressed at study entry. Relatedly, the limited range of baseline cohesion, adaptability and conflict scores (most of which were in the maladaptive range) may have reduced our power to detect relationships with key criterion variables, such as the adolescents’ severity of symptoms. Finally, missing outcome data in the second study year reduced our power to detect interactions between the study variables (for example, treatment and baseline family attributes) on symptomatic outcomes. Thus, caution is required in generalizing from these results and underlines the importance of replication and extension in larger samples. Given the amount of missing data, however, it is noteworthy that we found the relationships presented above. General agreement between analyses using adolescent- and parent-reported scores suggests that these findings may be clinically informative.
In this study, the enhanced care (EC) control treatment was not an attention control; families enrolled in FFT-A received significantly more clinician attention than those enrolled in EC. We cannot exclude the possibility that our findings regarding changes in family conflict could have resulted from the greater intensity of clinician contact associated with FFT-A. Although all patients were treated by study psychiatrists who followed a medication protocol, we did not control the pharmacotherapy regimens of patients. Thus, variability in medication regimens may have explained some of the associations we observed between family functioning scores and symptom improvement.
Given the demonstrated association between interpersonal stressors and the symptom course of adolescent BD (e.g., Kim, Miklowitz, Biuckians & Mullen, 2007), the present findings suggest that familial conflict may be a potent target in the treatment of adolescent BD. Investigating the relationships between family functioning and treatment adherence (i.e., psychotherapy session attendance or medication consistency) may also prove useful in improving the treatment of adolescent BD. Finally, this study did not address whether family functioning variables affect the peer or academic functioning of adolescents, two variables which are frequently impaired in early-onset BD population (Keenan-Miller & Miklowitz, 2011).
Highlights.
Study of family functioning and relationship to bipolar disorder symptoms in youth.
Adolescents were participants in randomized control trial of family treatment.
Intake family conflict levels decreased over time and predicted adolescent mania.
Family functioning and bipolar symptoms were longitudinally correlated.
Family functioning variables may inform treatment of adolescent bipolar disorder.
Acknowledgements
The authors thank Drs. Boris Birmaher, Elizabeth George, Dawn Taylor, Adrine Biuckians,Tina Goldstein, Eunice Kim, Kimberley Mullen, Chad Morris, and Victoria Cosgrove; and Christopher Hawkey, Amy Schlonski, Tim Winbush, Susan Wassick, Amy Mechels, Laura Wagenknecht, Lindsey Gagnon, Zachary Millman and Mary Beth Hickey for their assistance with the study.
ROLE OF THE FUNDING SOURCE
This study was supported by National Institute of Mental Health (NIMH) grants MH62555, MH073871, and MH077856 (Dr. Miklowitz) and a Distinguished Investigator Award from the National Alliance for Research on Schizophrenia and Depression (Dr. Miklowitz). These organizations were not involved with the design of the study, in the collection, analysis, or interpretation of study data, or in the decision to submit this paper for publication.
Footnotes
An additional measure used in the randomized trial, the Adolescent Longitudinal Follow-up Evaluation (ALIFE; Birmaher et al., 2006; Keller et al., 1987), allowed independent evaluators to make weekly ratings of symptom fluctuations over 3-6 month retrospective intervals. This measure was not included in the present analyses, as it was considered less relevant to the timepoints considered in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- American Psychological Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed Vol. 2000. American Psychiatric Press; Washington, DC: 2000. [Google Scholar]
- Asarnow JR, Tompson M, Woo S, Cantwell DP. Is expressed emotion a specific risk factor for depression or a nonspecific correlate of psychopathology? Journal of Abnormal Child Psychology. 2001;29(6):573–583. doi: 10.1023/a:1012237411007. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. Journal of Child and Adolescent Psychopharmacology. 2003;13:463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Strober M, Gill MK, Valeri S, Chiappetta L, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63(10):1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Baucom DH, Sher TG. Application of marital research and methodology to the study of the family. In: Hahlweg K, Goldstein MJ, editors. Understanding major mental disorder: The contribution of family interaction research. Family Process Press; New York: 1987. pp. 290–313. [Google Scholar]
- Begg CB, Iglewicz B. A treatment allocation procedure for sequential clinical trials. Biometrics. 1980;36:81–90. [PubMed] [Google Scholar]
- Belardinelli C, Hatch JP, Olvera RL, Fonseca M, Caetano SC, Nicoletti M, Soares JC. Family environment patterns in families with bipolar children. Journal of Affective Disorders. 2008;107(1-3):299–305. doi: 10.1016/j.jad.2007.08.011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiapetta L, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63(2):175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE. Depression in children and adolescents: Clinical features and pathogensis. In: Shulman KI, Tohen M, Kutcher SP, editors. Mood disorders across the life span (51-81) Wiley-Liss; New York, New York: 1996. [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorder in children and adolescents by semi-structured interview: test-retest reliability. Archives of General Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Chang K, Blasey C, Ketter TA, Steiner H. Family environment of children and adolescents with bipolar parents. Bipolar Disorders. 2001;3(2):73–78. doi: 10.1034/j.1399-5618.2001.030205.x. [DOI] [PubMed] [Google Scholar]
- Dietz LJ, Birmaher B, Williamson DE, Silk JS, Dahl RE, Axelson DA, Ryan ND. Mother-child interactions in depressed children and children at high risk and low risk for future depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(5):574–582. doi: 10.1097/CHI.0b013e3181676595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Youngstrom EA, Calabrese JR, Findling RL. The role of family functioning in bipolar disorder in families. Journal of Abnormal Child Psychology. 2008;36(6):849–863. doi: 10.1007/s10802-008-9217-9. [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, Birmaher B, Valeri S, Chiappetta L, Hunt J, Ryan N, Keller M. Child comorbidity, maternal mood disorder, and perceptions of family functioning among bipolar youth. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(8):955–964. doi: 10.1097/01.chi.0000222785.11359.04. [DOI] [PubMed] [Google Scholar]
- Feeny NC, Danielson CK, Schwartz L, Youngstrom EA, Findling RL. Cognitive-behavioral therapy for bipolar disorders in adolescents: a pilot study. Bipolar Disorders. 2006;8:508–515. doi: 10.1111/j.1399-5618.2006.00358.x. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B. Prospective continuity with adult bipolar I disorder; Characteristics of second and third episodes; Predictors of 8-year outcome. Archives of General Psychiatry. 2008;65(10):1125–1133. doi: 10.1001/archpsyc.65.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Axelson DA, Birmaher B, Brent DA. Dialectical behavior therapy for adolescents with bipolar disorder: A 1-year open trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(7):820–830. doi: 10.1097/chi.0b013e31805c1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlastala SA, Kotler JS, McClellan JM, McCauley EA. Interpersonal and social rhythm therapy for adolescents with bipolar disorder: Treatment development and results from an open trial. Depression and Anxiety. 2010;27(5):457–464. doi: 10.1002/da.20668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher BJ, Rent D, Roa U, Flynn C, Moreci P, Ryan N. Schedule for affective disorders and schizophrenia for school-age children - present and lifetime version (KSADS-PL); initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Miklowitz DJ. Interpersonal functioning in pediatric bipolar disorder. Clinical Psychology: Science and Practice. 2011;18(4):342–356. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation: a Comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, Brent DA. Family-focused treatment for adolescents with bipolar disorder: Results of a 2-year randomized trial. Archives of General Psychiatry. 2008;65(9):1053–1061. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, George EL, Taylor DO, Schneck CD, Sullivan AE, Birmaher B. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(6):643–651. doi: 10.1097/CHI.0b013e3181a0ab9d. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Archives of General Psychiatry. 1988;45:225–231. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Johnson SL. Social and familial factors in the course of bipolar disorder: Basic processes and relevant interventions. Clinical Psychology: Science and Practice. 2009;16(2):281–296. doi: 10.1111/j.1468-2850.2009.01166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell RA, Mayo JA, Flatow L, Cuthbertson B, O’Brien BE. Outcome of bipolar disorder on long-term treatment with lithium. British Journal of Psychiatry. 1991;159:123–129. doi: 10.1192/bjp.159.1.123. [DOI] [PubMed] [Google Scholar]
- Olson DH, Russell CS, Sprenkle DH. Circumplex model of marital and family systems: VI. Theoretical update. Family Process. 1983;22:69–83. doi: 10.1111/j.1545-5300.1983.00069.x. [DOI] [PubMed] [Google Scholar]
- Olson DH, Tiesel J. FACES II:Linear scoring and interpretation. Available from: Life Innovations, Family Inventories Project, P.O. Box 190; Minneapolis, MN: 1991. pp. 55440–0190. [Google Scholar]
- Place M, Hulsmeier J, Brownrigg A, Soulsby A. The family adaptability and cohesion scale (FACES): An instrument worthy of rehabilitation? Psychiatric Bulletin. 2005;29:215–218. [Google Scholar]
- Priebe S, Wildgrube C, Muller-Oerlinghausen B. Lithium prophylaxis and expressed emotion. The British Journal of Psychiatry. 1989;154:396–399. doi: 10.1192/bjp.154.3.396. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster SL, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavior Analysis. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd edition Sage; Newbury Park, CA: 2002. [Google Scholar]
- Robertson HA, Kutcher SP, Bird D, Grasswick L. Impact of early onset bipolar disorder on family functioning: Adolescents’ perceptions of family dynamics, communication, and problems. Journal of Affective Disorders. 2001;66:25–37. doi: 10.1016/s0165-0327(00)00281-0. [DOI] [PubMed] [Google Scholar]
- Romero S, Delbello MP, Soutullo CA, Stanford K, Strakowski SM. Family environment in families with versus families without bipolar disorder: A preliminary comparison study. Bipolar Disorders. 2005;7(6):617–622. doi: 10.1111/j.1399-5618.2005.00270.x. [DOI] [PubMed] [Google Scholar]
- Silk JS, Ziegler ML, Whalen DJ, Dahl RE, Ryan ND, Dietz LJ, Williamson DE. Expressed emotion in mothers of currently depressed, remitted, high-risk and low-risk youth: Links to child depression status and longitudinal course. Journal of Clinical Child and Adolescent Psychology. 2009;38(1):36–47. doi: 10.1080/15374410802575339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoneau TL, Miklowitz DJ, Saleem R. Expressed emotion and interactional patterns in the families of bipolar patients. Journal of Abnormal Psychology. 1998;107(3):497–507. doi: 10.1037//0021-843x.107.3.497. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; New York, NY: 2003. [Google Scholar]
- Sullivan AE, Miklowitz DJ. Family functioning among adolescents with bipolar disorder. Journal of Family Psychology. 2010;24(1):60–67. doi: 10.1037/a0018183. [DOI] [PubMed] [Google Scholar]
- Townsend LD, Demeter CA, Youngstrom E, Drotar D, Findling RL. Family conflict moderates response to pharmacological intervention in pediatric bipolar disorder. Journal of Child and Adolescent Psychopharmacology. 2007;17(6):843–851. doi: 10.1089/cap.2007.0046. [DOI] [PubMed] [Google Scholar]
- Yan LJ, Hammen C, Cohen AN, Daley SE, Henry RM. Expressed emotion versus relationship quality variables in the prediction of recurrence in bipolar patients. Journal of Affective Disorders. 2004;83:199–206. doi: 10.1016/j.jad.2004.08.006. [DOI] [PubMed] [Google Scholar]