Abstract
Objective
The potential risks associated with ionising radiation are well documented. We have previously reported the “black bone” MRI sequence, useful when imaging cortical bone. The objective of this paper is to report our initial experience of this technique in patients undergoing imaging of the head and neck region.
Methods
Using the departmental database those patients having had “black bone” sequences of the head and neck performed as part of their MRI examination in the preceding 5 years were identified. The radiological reports were reviewed to identify those cases where “black bone” or conventional MRI sequences had been performed in place of the requested CT, and the patient medical records for these cases were reviewed. Medical record review was also conducted for those cases where it was considered that the pathological condition requiring imaging would ordinarily be investigated with CT.
Results
The “black bone” sequence had been performed in 69 patients as part of routine MRI of the head and neck. Of these, 67% (n=46) were performed in combination with CT imaging, the majority of cases being primary tumours. In four cases, an MRI was performed in place of the requested CT scan. We present eight clinical cases illustrating the potential benefits of the “black bone” sequence.
Conclusions
“Black bone” MRI offers a radiation-free method of imaging the head and neck, and has been successfully utilised in a range of benign and malignant conditions affecting this region.
Advances in knowledge
Adoption of this approach, where feasible, would be a significant advance in radiation protection.
Hounsfield, in his 1973 paper on CT, stated that “the exposure of the patient to x-rays must be restricted” [1]. The potential risks of ionising radiation are well documented; however, we continue to fall short of Hounsfield’s advice because of increased imaging demands through a combination of defensive medicine, a decrease in exploratory surgery and the ability to meet the increased requests for CT. The largest increases in CT use have been in paediatric diagnosis and adult screening [2]. Further concern relates to the use of cone-beam CT, with scanners being installed and used in a rapidly increasing number of dental practices within the UK [3]. During the year 2002–3 the National Health Service in England [4] reported 1.7 million CT examinations, representing 8% of all X-ray examinations, and 6% of all imaging investigations. By 2009–10 this had risen to over 3.7 million: 13% and 10%, respectively. The United Nations Scientific Committee estimated that CT constitutes 5% of all X-ray examinations worldwide while accounting for about 34% of the resultant collective dose [5].
The consensus among radiology professionals is that steps should be taken to reverse, or at least arrest, radiation exposure from CT [6]; yet for maxillo-cranio-facial imaging this has largely consisted of radiation reduction techniques and the introduction of cone-beam CT. The superior quality of bony imaging on CT and the ability to create three-dimensional (3D) rendered images of the craniofacial skeleton has maintained CT as the gold standard for this region.
However, we have been increasingly utilising MRI when imaging the head and neck, following close collaboration between the MRI and oral and maxillofacial departments. In particular, we have previously reported the “black bone” MRI sequence for imaging cortical bone as a potential replacement for CT [7]. The technique utilises a low flip angle, with short repetition and echo times, to produce uniform contrast of the soft tissues, with densely black cortical bone. The imaging parameters are shown in Table 1. We present our experience of this technique in patients undergoing craniofacial imaging.
Table 1. Black bone MRI scanning parameters.
| Parameter | Value |
| TR | 8.6 ms |
| TE | 4.2 ms |
| Slice thickness | 2.4 mm |
| Slice spacing | −1.2 mm |
| Scan FOV | 24 cm |
| Phase encode | 256 |
| Frequency encode | 256 |
| Receive bandwidth | 31.25 |
| ZIP | 2, 512 |
FOV, field of view; TE, echo time; TR, repetition time; ZIP, zero fill interpolation.
Methods and materials
Using the departmental database those patients having had “black bone” sequences of the head and neck performed as part of their MRI examination in the preceding 5 years were identified. The accuracy of the database was confirmed by performing a retrospective review of the hospital picture archiving and communication system (PACS) (Centricity© Enterprise V3.0, GE Medical Systems, Amersham, UK). As Centricity© has no inherent searching facility for “black bone”, sequential review of MR images requested by oral and maxillofacial surgeons was conducted. The “black bone” sequence was included in the MRI examination by the supervising radiologist when it appeared that it could add to the investigation, and possibly prevent the patient undergoing CT. The “black bone” sequence was completed on either a 1.5 or 3.0 T magnet (GE Medical Systems).
The radiological reports were reviewed to identify those cases where a “black bone” or conventional MR sequences had been performed in place of the requested CT, and the patient medical records for these cases were reviewed. Medical record review was also conducted for those cases where it was considered that the pathological condition requiring imaging would ordinarily be investigated with CT. In addition, although likely to under-report the number of patient exposures, all imaging performed on the head and neck region for each patient documented on the PACS was recorded.
As the “black bone” sequence forms part of our routine clinical practice, ethical approval for this study was not required.
Results
In total, the “black bone” sequence has been performed in 69 patients as part of routine MRI of the head and neck. Of these, 33% (n=23) avoided CT examination. In these patients MRI was performed for a range of head and neck conditions including benign mandibular lesions (n=6), benign maxillary lesions (n=4), orbital fractures (n=3), facial pain (n=4) and surveillance of malignant head and neck tumours (n=6). In four cases, an MRI was performed in place of a requested CT scan. These cases are presented below (Table 2). A further four cases ordinarily deemed to be investigated with CT were also included as a representation of our experience with “black bone.”
Table 2. Presentation of eight cases in whom CT imaging was avoided.
| Patient number | Age (years) | Sex | Diagnosis | Black bone sequence |
| 1 | 31 | Female | Zygomatic asymmetry | In place of requested CT |
| 2 | 38 | Male | Orbital fracture | In place of requested CT |
| 3 | 62 | Male | Mandibular keratocyst | In place of requested CT |
| 4 | 46 | Female | Maxillary giant cell granuloma | Follow-up in place of CT |
| 5 | 58 | Male | Periodontal inflammation | Requested |
| 6 | 56 | Female | Mandibular keratocyst | Follow-up in place of CT |
| 7 | 26 | Female | Maxillary odontogenic cyst | As part of requested MRI examination |
| 8 | 23 | Male | Suspected zygomatic fracture | As part of requested MRI examination |
For the remaining 67% (n=46) of patients, the “black bone” sequence was performed in combination with CT imaging (Table 3). The majority of these cases had multimodal imaging performed for tumour staging or clinical suspicion of tumour recurrence. In one case, CT was performed in addition to MRI and the “black bone” sequence to further delineate the bone in a complex case of probable fibrous dysplasia.
Table 3. Indication for black bone MRI with or without CT examination.
| Diagnosis | Black bone MRI only | Black bone MRI + CT | Total |
| Benign mandibular lesions | 6 | 3 | 9 |
| Benign maxillary lesions | 4 | 4 | 8 |
| Orbital fractures | 3 | 0 | 3 |
| Facial pain | 4 | 0 | 4 |
| Malignancy and surveillance | 6 | 39 | 45 |
| Total | 23 | 46 | 69 |
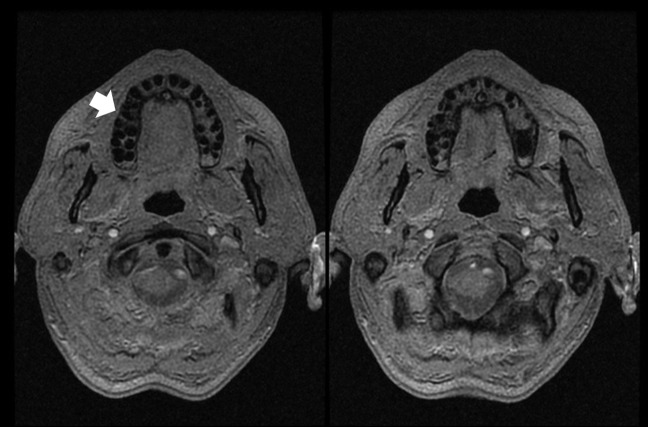
Patient 1
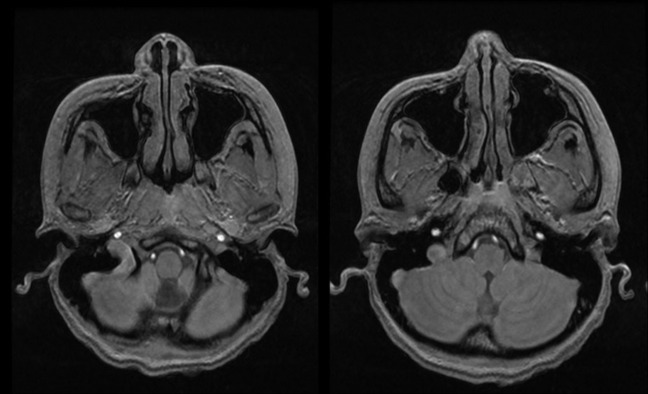
A 31-year-old female was referred for CT imaging to investigate increased prominence of the right zygoma. Asymmetry of the facial features had been noted by friends of the patient 2 months prior to presentation, with no further progression during this period. Of note was an injury to this side of her face in childhood, which required no intervention. Radiography performed by the referring physician was normal. MRI was performed in place of the requested CT for radiation protection. Imaging demonstrated the zygomatic bodies to be within normal limits, with an acute angle between the anterior and lateral walls. The “black bone” sequence was useful in demonstrating a normal cortical pattern of the zygomatic bodies, with normal marrow signal from the medulla (Figure 1). There was no evidence of a mass in the surrounding tissues. However, mucosal thickening in the left maxillary antrum was noted and the medial half of the anterior wall immediately below the orbital rim bulged into the cheek. The patient has been reassured that there is no significant pathology and remains under review.
Figure 1.
Axial “black bone” images of Patient 1 demonstrating normal cortical appearances of the zygomatic bones.
Patient 2
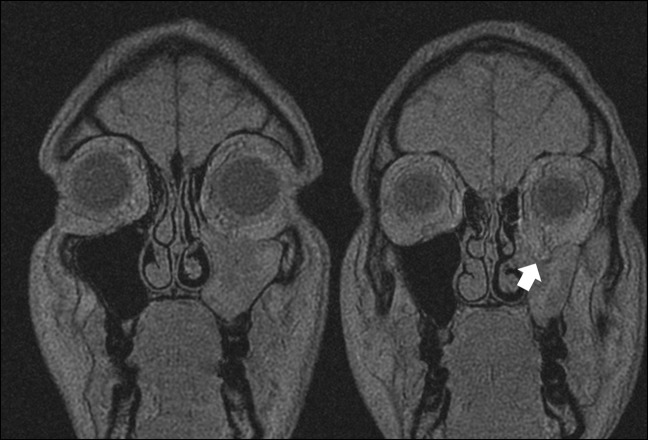
A 38-year-old male was referred from the Emergency Department following a rugby injury. He complained of a “popping” sensation in the left globe when blowing his nose. On clinical examination there was a small palpable step in the left infraorbital rim, with no associated paraesthesia or eye symptoms. Facial radiographs performed by the referring team revealed an undisplaced fracture of the left zygoma. With no significant symptoms, the patient opted for non-surgical management and was discharged. The patient re-presented 4 weeks later with diplopia on upward gaze. On clinical examination at this time he had mild enophthalmos and hypoglobus of the left orbit. CT imaging of the left orbit was requested but replaced by MRI for radiation protection. MRI demonstrated inferior displacement of almost all of the orbital floor on the left, with a mild degree of enophthalmos. A fracture was noted to extend into the inferior part of the medial wall but with no true medial wall blow-out into the ethmoid sinuses. The underlying antrum was almost completely occupied by extensive mucosal swelling with proteinaceous effusion in the remaining cavity. The “black bone” sequence demonstrated that the lateral antral wall was in a normal position, and the zygoma appeared to be intact (Figure 2). The patient subsequently underwent open reduction and fixation of orbital fracture with autologous bone grafting.
Figure 2.
Coronal black bone images of Patient 2, demonstrating inferior displacement of the left orbital floor (arrow), and fluid within the left maxillary sinus.
Patient 3
A 62-year-old male presented with presumed recurrence of a left mandibular keratocyst, previously excised 16 years earlier. An orthopantogram (OPG) showed radiolucency of the left sigmoid notch and condyle. MRI was performed in place of the requested CT examination. The imaging confirmed a bilobed expansile lesion in the neck of the mandible on the left. This extended into the base of the mandibular head with sparing of a rim of medulla on the superior aspect of the lesion. Overall, the lesion measured approximately 2×2×1 cm and extended anteroinferiorly from the mandibular neck into the proximal ramus. The “black bone” sequence demonstrated thinning and loss of the cortex on the medial aspect of the lower margin of the lesion and again at its maximum convexity on the medial aspect of the mandible (Figure 3). There was also a small area of cortical loss on the lateral aspect of the mandibular neck. However, there was no detectable extension into the soft tissues. He underwent further excision of this lesion, with histological examination confirming recurrence of the odontogenic keratocyst.
Figure 3.
Axial “black bone” images of Patient 3, demonstrating thinning and loss of the cortex on the medial aspect of the lower margin of the left mandibular keratocyst (arrow).
Patient 4
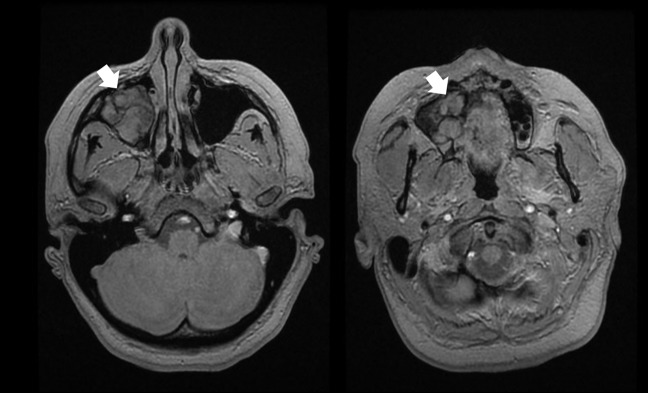
A 46-year-old female presented with buccal swelling and loosening of the upper right second premolar and first molar teeth. On OPG, an area of radiolucency of the maxilla was noted, and the patient underwent exploration of the region with excision of a mass. Histologically this was confirmed as a giant cell granuloma. Post-operatively the patient had recurrence of the mass, and was managed with calcitonin therapy, to which she had a good response. Follow-up with sequential scanning has been necessary, with preference for MRI for radiation protection. “Black bone” sequences were of sufficient quality to negate the need for CT (Figure 4). MR demonstrated minimal expansion of the right antrum, which appeared to be completely occupied by the granuloma. There was expansion of the root of the right superior alveolus without displacement of the cortex or the teeth. The patient remains under clinical review.
Figure 4.
Axial black bone images of Patient 4, demonstrating granuloma within the right maxillary sinus (arrows).
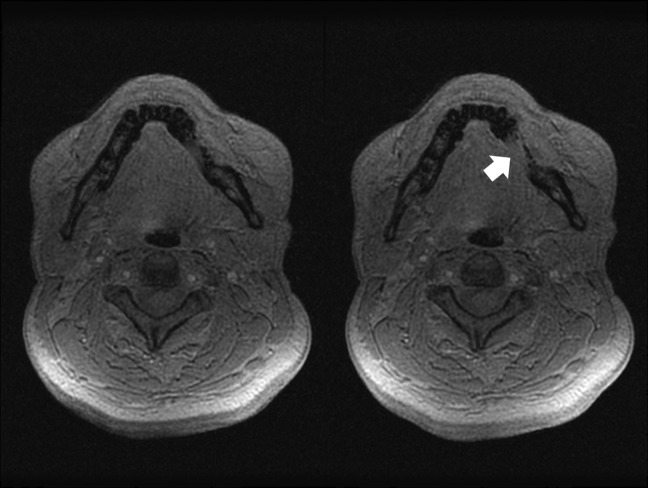
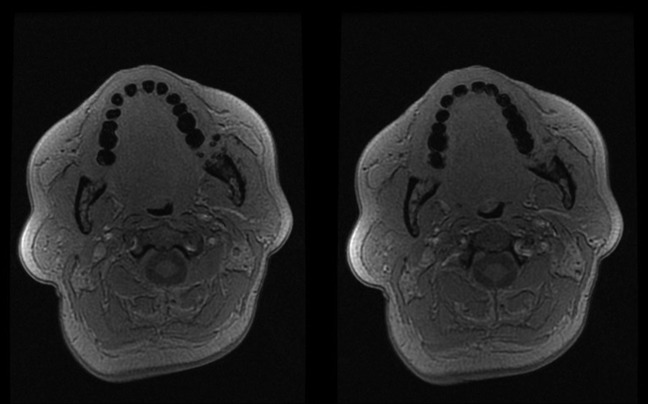
Patient 5
A 58-year-old male presented with an intermittently painful lump in the region of the right upper second premolar. This had been present for 4 months, during which time it had gradually increased in size. On examination an 8 mm bony hard lump was noted over the apex of the right upper premolar. OPG showed restoration of the second premolar, but no other pathology. A “black bone” MRI was specifically requested to investigate this region (Figure 5). Imaging demonstrated no evidence of bony expansion of the right superior alveolus. There was altered signal around the roots of both right upper fifth and sixth teeth in keeping with periodontal inflammation, and a small effusion in the base of the right maxillary antrum was present. In addition, a well-defined signal change was noted around the root of the right lower third tooth, in keeping with apical abscess. Under local anaesthesia the region was explored, and pus found above the distobuccal root of upper first molar tooth, which was curetted out. The patient was subsequently referred back to his primary care dentist for root canal therapy.
Figure 5.
Axial black bone images of Patient 5, demonstrating no evidence of bony expansion of the right superior alveolus (arrow).
Patient 6
A 56-year-old female presented with recurrence of a left retromolar keratocyst. This had previously been enucleated 6 years prior to presentation. The patient underwent repeat encluceation, and histology confirmed an odontogenic keratocyst. Recurrent imaging at 1 year has demonstrated good bony infill with no evidence of cyst recurrence. The “black bone” sequence demonstrated normal cortical morphology, with evidence of trabecular sclerosis in keeping with healing (Figure 6). The patient remains under review.
Figure 6.
Axial “black bone” images of Patient 6, demonstrating normal cortical morphology, with evidence of trabecular sclerosis at site of previous left retromolar keratocyst.
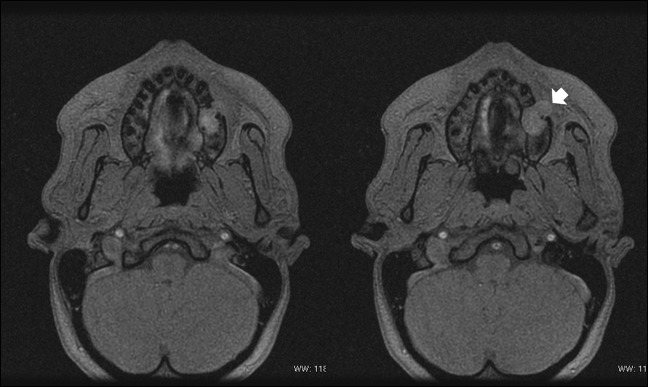
Patient 7
A 26-year-old female presented with a 3-week history of a slowly enlarging non-painful lesion affecting the left upper jaw. Routine OPG demonstrated a radiolucency in the region of the second premolar/first molar. MRI was requested, which demonstrated a high T2 signal lesion arising between the roots of the left upper sixth tooth. “Black bone” imaging demonstrated the lesion extending superiorly into the alveolus and breaching the lateral cortex with a dumbbell extension into the subcutaneous tissues of the cheek (Figure 7). The findings suggested a slow-growing lesion such as a keratocyst or ameloblastoma. A fine needle aspiration of the region confirmed a diagnosis of a benign odontogenic cyst, and the remnants were excised following root canal treatment of the adjacent teeth.
Figure 7.
Axial “black bone” images of Patient 7, demonstrating a lesion within the left maxillary alveolus which breaches the lateral cortex with extension into the subcutaneous tissues of the cheek (arrow).
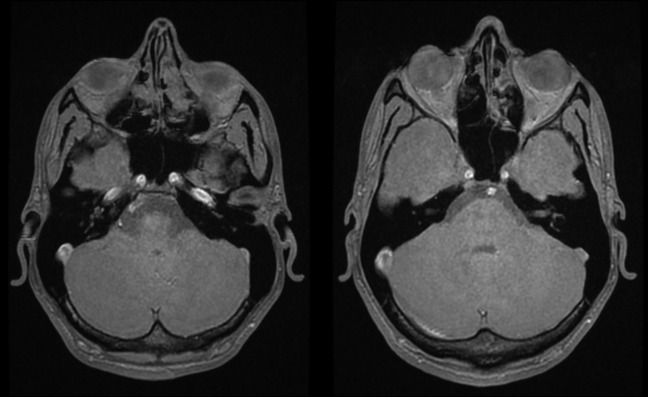
Patient 8
A 23-year-old male presented following an alleged assault, having fallen to the ground hitting his face. On examination he had mild left infraorbital anaesthesia and slight flattening of the left malar region. Radiographs showed a minimally displaced left zygomatic fracture. He failed to attend follow-up, but returned 3 weeks later complaining of worsening diplopia. However, the patient had a long-standing squint for which he was not currently using his prescription glasses. A Hess chart used to assess diplopia, by demonstrating the position of the non-fixing eye in all positions of gaze when the other eye was fixing, showed no change. Routine MRI was requested. Coronal images demonstrated that the left orbital floor was normal. There was no evidence of surrounding fracture on the “black bone” images (Figure 8). The patient was reassured, and discharged from further follow-up.
Figure 8.
Axial “black bone” images of Patient 8, with normal appearances of the orbital bones.
All of these presented patients avoided CT examination by utilising the “black bone” sequence.
In total, 169 radiographs and 88 CT scans of the head and neck were identified on PACS for the 69 patients with “black bone” imaging of the head and neck. This represents an average of 1.6 plain films (n=36) and 0.8 CT scans (n=18) for patients with benign conditions, and 2.9 (n=133) and 1.5 (n=70), respectively, for those with a history of head and neck malignancy.
Discussion
We have demonstrated the potential benefits of “black bone” MRI when imaging the maxillo-cranio-facial region. This is of particular value in patients who are young with benign conditions, in whom radiation protection is paramount. The sequence results in uniform contrast of the soft tissues, with densely “black bone”, which aids in delineating pathology involving the facial skeleton. The key limitation of the technique is in areas where “black bone” abuts black air, such as the sinuses, which makes separation of the two particularly challenging. However, the sequence has been successfully utilised to both exclude and identify fractures of the facial skeleton, and benign and malignant infiltrating tumours. With increasing use of cone-beam CT, and its introduction into dental care in the community, we have demonstrated an alternative, radiation-free method of examining dental pathology. As with other MR sequences, “black bone” is also susceptible to artefact and degradation of image quality in the region of dental amalgam and implanted materials.
The “black bone” sequence has been used in our institution for a number of years, and is slowly finding its place in routine imaging. With increasing familiarity of the technique, among both radiologists and referring clinicians, it is increasingly being utilised in place of CT. To date, the sequence has largely been confined to imaging the head and neck, in view of the specialist interests of the authors. However, we are further exploring the potential of its use in other aspects of bony imaging.
Familiarity with the technique is currently one of its key limitations. We currently continue to employ multimodal imaging, particularly in cases of malignancy. A shift from CT to “black bone” imaging in these patients may occur in the future as confidence with “black bone” imaging develops. The appearance of black as opposed to the white bone seen on CT certainly requires continued clinical practice.
The potential adverse consequences of repeated radiation exposure of the head and neck have been well documented [8,9]. Review of the 69 patients in this study demonstrated that the number of plain films and CT scans performed in patients with pathology of the head and neck are significant. This is more concerning when it is acknowledged that these numbers are likely to severely under-report the actual number of imaging procedures each patient undergoes. A significant proportion of patients are seen in primary care and at alternative units prior to referral and for local follow-up, where further ionising imaging will probably be performed. Although the effective dose from CT scans of the head and neck is considerably lower than those for imaging the chest or abdomen, the head and neck region, as shown in this study, is more frequently imaged and the collective dose for cranial imaging is therefore higher [5]. Smyth et al [10] reported two cases to highlight the concern of repeated radiation exposure in children. The first was an 18-year-old male, diagnosed with hydrocephalus as an infant, ultimately requiring 23 ventriculoperitoneal shunt revisions, each of which was preceded by CT imaging. Additionally, he had 25 plain skull radiographs before the age of 17 years. Aged 17, he developed a neck mass, confirmed as Hodgkin’s lymphoma. The second case had a similar history. He had 14 head CT scans prior to the age of 15 years. He succumbed to a gliosarcoma at the age of 19 years. The radiation risk from diagnostic imaging is the subject of much controversy, and estimates of cancer induction and death should be interpreted with caution [11]. However, there is direct evidence from epidemiological studies that the organ doses corresponding to a common CT study (two or three scans, resulting in a dose in the range 30–90 mSv) result in an increased risk of cancer. This risk is greater for children, who are inherently more radiosensitive and have more remaining years of life during which a radiation-induced cancer could develop [2,12]. Superficial radiosensitive organs, such as the thyroid, eyes and breasts, receive a greater proportion of radiation because of increased scatter and the lack of overlying other tissues to partially absorb some of the dose [13]. The threshold dose for detectable lens opacities is quoted to be 0.5–2 Gy [14]. With accumulated risk, CT-induced lens opacification is a highly feasible possibility in patients undergoing multiple examinations throughout their lifetime. Clinicians and radiologists should make every effort to minimise exposure to radiation for their patients.
As discussed, the main advantage of the “black bone” MRI sequence is the avoidance of radiation exposure in our patient groups. However, it must be stated that there are some limitations which require consideration, including the increased cost and scanning time associated with MRI compared with CT, and the exclusion of those patients with significant metal foreign bodies (e.g. pacemakers), and those unable to tolerate MRI due to claustrophobia or increased body mass index. The “black bone” MRI sequence adds approximately 5 min to the examination time, but may eliminate the costs of a second examination in the form of a CT, which is commonly utilised in head and neck imaging.
We have presented a novel potential alternative to CT scanning. The biometric accuracy of the “black bone” sequence has been demonstrated [7]. The development of 3D rendering techniques is currently being investigated. With these traditional methods of image visualisation similar to CT, we feel that “black bone” MRI will become a routine alternative to CT examination.
Footnotes
Project no. C-09-1W was supported by the AO Research Fund of the AO Foundation
References
- 1.Hounsfield GN. Computerized transverse axial scanning (tomography): Part I. Description of system. Br J Radiol 1973;46:1016–22 [DOI] [PubMed] [Google Scholar]
- 2.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84 [DOI] [PubMed] [Google Scholar]
- 3.Holroyd JR, Gulson AD. The radiation protection implications of the use of cone beam computed tomography (CBCT) in dentistry—what you need to know. London, UK: Health Protection Agency; 2009 [Google Scholar]
- 4.DH. Hospital activity statistics—imaging and radiodiagnostics. [cited 3 November 2010]; Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/HospitalActivityStatistics/DH_077487. [Google Scholar]
- 5.Tack D, Gevenois PA. Radiation dose from adult and paediatric multidetector computed tomography. 1st edn. Berlin, Germany; Springer; 2007 [Google Scholar]
- 6.Lewis MA, Edyvean S. Patient dose reduction in CT. Br J Radiol 2005;78:880–3 [DOI] [PubMed] [Google Scholar]
- 7.Eley KA, McIntyre AG, Watt-Smith SR, Golding SJ. “Black bone” MRI: a partial flip angle technique for radiation reduction in craniofacial imaging. Br J Radiol 2012;85:272–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polhemus DW, Koch R. Leukemia and medical radiation. Pediatrics 1959;23:453–61 [PubMed] [Google Scholar]
- 9.Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA 2003;100:13761–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smyth MD, Narayan P, Tubbs RS, Leonard JR, Parks TS, Loukas M, et al. Cumulative diagnostic radiation exposure in children with ventriculoperitoneal shunts: a review. Childs Nerv Syst 2008;24:493–7 [DOI] [PubMed] [Google Scholar]
- 11.Hadley JL, Agola J, Wong P. Potential impact of the American College of Radiology appropriateness criteria on CT for trauma. AJR Am J Roentgenol 2006;186:937–42 [DOI] [PubMed] [Google Scholar]
- 12.Callahan MJ. CT dose reduction in practice. Pediatr Radiol 2011;41Suppl. 2:488–92 [DOI] [PubMed] [Google Scholar]
- 13.Hopper KD. Orbital, thyroid, and breast superficial radiation shielding for patients undergoing diagnostic CT. Semin Ultrasound CT MR 2002;23:423–7 [DOI] [PubMed] [Google Scholar]
- 14.Zammit-Maempel I, Chadwick CL, Willis SP. Radiation dose to the lens of eye and thyroid gland in paranasal sinus multislice CT. Br J Radiol 2003;76:418–20 [DOI] [PubMed] [Google Scholar]