Abstract
Objective
To evaluate the clinical utility of the meniscal extrusion transverse ratio of the medial meniscus in the diagnosis of meniscal root tear compared with the gold standard of arthroscopic diagnosis.
Methods
This retrospective study sample included 32 males and 35 females who underwent MRI at our institution. There were 24 meniscal root tear cases. The control groups were 18 cases of medial meniscal tears without root tears and 25 cases of negative meniscal findings on arthroscopy. Meniscal extrusion (L) and maximal transverse lengths (T) of the medial meniscus were measured, and L/T ratios were calculated. These results were correlated with arthroscopic findings and analysed statistically. With arthroscopic findings used as the standard of reference, the sensitivity and specificity of 10%, 11% and 12% extrusion thresholds, and 3 mm of medial meniscal extrusion (MME) as diagnostic thresholds, were calculated.
Results
The mean length of the meniscal extrusions of meniscal root tears was twice as long as the control group. The mean L/T ratio of the meniscal root tears was approximately 13%, while those of the control groups were 5%. The differences in the L and L/T between the meniscal root tears and normal and meniscal root tears and other meniscal tears were statistically significant (p<0.001), but those between normal and other meniscal tears were not. The best diagnostic discrimination was achieved using an extrusion ratio threshold of 10% (79% sensitivity, 86% specificity). The 3 mm of MME threshold demonstrated high specificity (98%), but not high sensitivity (54%).
Conclusion
The mean L/T ratio of the meniscal root tears was approximately 13% and was statistically significant. The best diagnostic discrimination was achieved using an extrusion ratio threshold of 10%.
Advances in knowledge
The use of the L/T ratio in combination with MME can be a useful method for evaluating medial meniscal root tears.
The meniscal roots are the sites where the knee meniscus attaches to the central tibial plateau [1]. In many cases, a meniscal root tear is not prominent on a single MRI image as the structures follow oblique courses. Medial meniscal extrusion (MME) is a significant medial displacement of the medial meniscus with respect to the central margin of the medial tibial plateau and is closely associated with medial meniscal root tears (MMR) [2]. The meniscus is considered “extruded” when it extends beyond the tibial margin; this results from disruption of collagen fibres within the meniscus that provide hoop strength [3]. The critical length of extrusion is approximately 3 mm [4-5]. There is some uncertainty regarding the length of the extrusion because the transverse diameter of the medial meniscus varies with age and individual; uniform length criteria can be replaced with length ratios. The current study was performed to evaluate the clinical utility of the meniscal extrusion transverse ratio of the medial meniscus in the diagnosis of the meniscal root tears as compared with the gold standard of arthroscopic diagnosis.
Methods and materials
Case selection
We retrospectively evaluated 67 patients with knee pain who underwent knee MRI and arthroscopy. The population was composed of 32 (48%) males and 35 (52%) females, who underwent MRI at our institution between January 2010 and May 2011. All patients experienced knee pain and impaired mobility. There were 24 meniscal root tear cases (mean age: 53.7±10.6 years, range: 25–73 years). All cases were posterior root tears. There were two control groups. One consisted of 18 patients with medial meniscal tears without root tears on arthroscopy (mean age: 48.8±10.9 years, range: 24–64 years). This group was composed of four radial tear cases, seven horizontal tear cases five complex tear cases, one longitudinal tear case and one flap tear case. The second control group consisted of 25 patients with negative meniscal findings on arthroscopy (mean age: 36.3±16.4 years, range: 8–68 years). The candidates for arthroscopy were patients who reported unbearable symptoms. The exclusion criteria included the presence of fractures, tumours, severe osteoarthritis more than Kellgren–Lawrence Grade III, anterior cruciate ligament injury, lateral meniscal tears, and a previous history of knee surgery. This study was approved by our Institutional Ethics Review Board, and the requirement for informed consent was waived due to the retrospective nature of the study.
MRI parameters
All MRI examinations were performed using the same protocol on a 1.5-T magnet MRI scanner (Intera; Philips Healthcare, Best, Netherlands) using an extremity coil. The sequences and imaging parameters are summarised in Table 1.
Table 1. Imaging parameters for MRI sequences.
| Imaging parameter | Coronal FS T2 FSE | Coronal PD FSE | Sagittal PD FSE | Axial FS PD FSE | Sagittal FS T2 FSE |
| TR (ms) | 3600 | 3000 | 3000 | 3000 | 4200 |
| TE (ms) | 70 | 35 | 35 | 36 | 70 |
| Flip angle (°) | 90 | 90 | 90 | 90 | 90 |
| Matrix size | 256×200 | 256×200 | 256×200 | 256×256 | 256×200 |
| Field of view (cm) | 15 | 15 | 15 | 15 | 15 |
| Slice thickness (mm) | 4 | 4 | 4 | 4 | 4 |
| Interslice gap (mm) | 1 | 1 | 1 | 1 | 1 |
| Bandwidth (kHz) | 260 | 250 | 250 | 190 | 190 |
| Echo train length | 14 | 10 | 12 | 15 | 15 |
| Signal average | 2 | 2 | 2 | 2 | 2 |
| Scan time (min:s) | 2:07 | 2:27 | 2:07 | 2:13 | 2:02 |
FS, fat saturation; FSE, fast spin echo; PD, proton density; TE, echo time; TR, repetition time.
Image analysis
MRI examinations were interpreted by two fellowship-trained academic musculoskeletal radiologists with 12 and 10 years of experience who were blinded to clinical information and radiological reports. Assessment for possible MME was carried out on the central coronal slices observed to pass through the medial collateral ligament. A vertical line was drawn along the peripheral margin of the medial tibial plateau at the point of transition from horizontal to vertical. The distance between this line and a second vertical line drawn along the outer margin of the meniscus was measured (Figure 1). Assessment of the maximal transverse length of the medial meniscus was carried out in the posterior coronal slices, which transected the posterior horn of the meniscus if seen on an axial image (Figure 2). The length was measured twice and the average of those two values was used. The ratio (%) of extrusion length (L) to maximal transverse length (T) was calculated.
Figure 1.
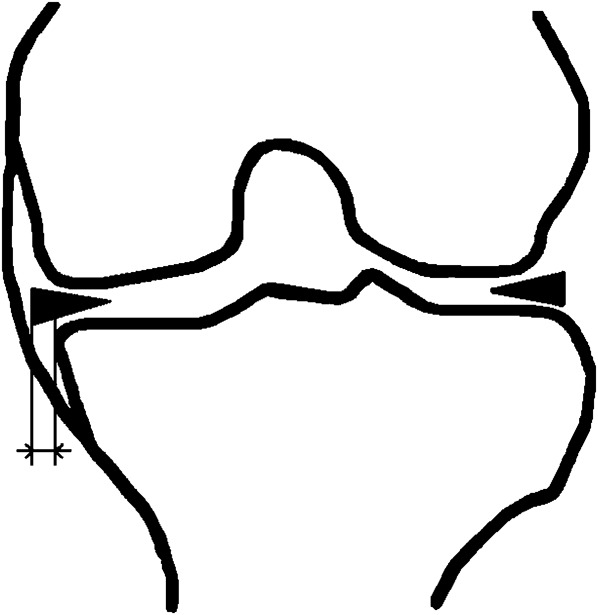
Schematic showing medial meniscal extrusion. Meniscal extrusion is measured by the distance from the perpendicular line to the edge of the tibial plateau and the outer edge of the meniscus (at the point of the mid-portion of its maximal thickness).
Figure 2.
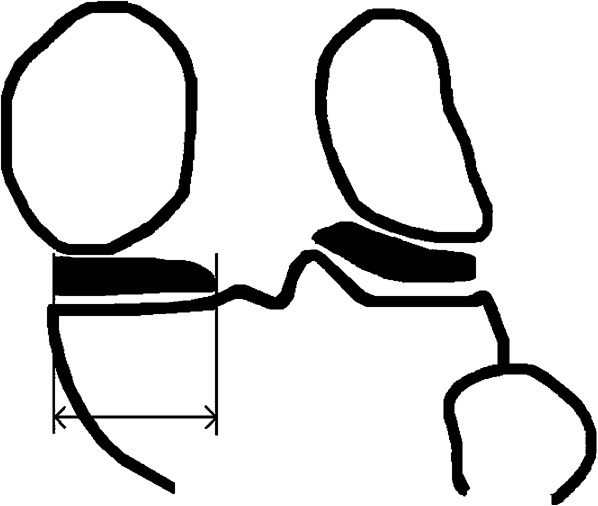
Schematic demonstrating the maximal transverse length of the medial meniscus.
Arthroscopic comparison
The majority of the arthroscopic studies were performed as soon as possible following MRI, with a mean MRI to arthroscopy interval of 15 days. No medical treatment (such as non-steroidal anti-inflammatory drugs or physical therapy) was administered during the interval time period. A knee fellowship-trained academic orthopaedic surgeon with 30 years of experience performed all surgical procedures. We obtained arthroscopic data after reviewing images from official medical records and discussion with the operating surgeon.
Statistical analysis
The length of the extrusion and transverse diameter of each group were compared using paired Student's t-tests. Interobserver agreement between the two radiologists was analysed using intraclass correlation coefficient (ICC). ICC values of <0.40 indicate poor reproducibility, ICC values of 0.40–0.75 indicate fair to good reproducibility, and ICC values greater than 0.75 indicate excellent reproducibility [6]. With arthroscopic findings used as the standard of reference, the sensitivity and specificity with 95% confidence intervals of 10%, 11% and 12% extrusion thresholds and 3 mm of MME were calculated. SAS v. 9.1 software (SAS Institute, Cary, NC) was used to perform the analysis. A p-value ≤0.05 was considered statistically significant.
Results
The interclass correlation coefficients of the length and ratio between two readers were 0.970 and 0.978, respectively, indicating excellent interobserver agreement. The mean length of the meniscal extrusion of meniscal root tears was twice as long as that in the control group (2.91–2.97 vs 1.21–1.33; Table 2). The mean transverse diameter of the meniscus was smaller in cases of meniscal root tears, but this was not statistically significant. The mean L/T ratio of the meniscal root tears was approximately 13%, while those of the control groups were 4–5% (Figures 3–6). The p-values of the measurement analysis between the groups are given in Table 3. The differences in the L and L/T between meniscal root tear cases and normal and between meniscal root tear and other meniscal tear cases were statistically significant (p<0.001), but those between normal and other meniscal tear cases were not (p>0.05).
Table 2. The mean length of meniscal extrusion, transverse diameter and ratio of extrusion.
| Parameter | Meniscal root tear |
Other meniscal tear |
Normal |
|||
| Reader 1 | Reader 2 | Reader 1 | Reader 2 | Reader 1 | Reader 2 | |
| Length of extrusion (L) | 2.97 (±1.23) | 2.91 (±1.19) | 1.33 (±0.70) | 1.22 (±0.76) | 1.22 (±1.13) | 1.21 (±1.14) |
| Transverse diameter of medial meniscus (T) | 23.13 (±1.81) | 23.29 (±2.08) | 26.77 (±2.25) | 26.02 (±3.31) | 24.66 (±3.14) | 24.37 (±3.40) |
| L/T | 0.13 (±0.06) | 0.13 (±0.06) | 0.05 (±0.03) | 0.04 (±0.03) | 0.05 (±0.04) | 0.05 (±0.04) |
Length of meniscal extrusion and transverse diameter values are in millimetres. Data in parentheses are standard deviations.
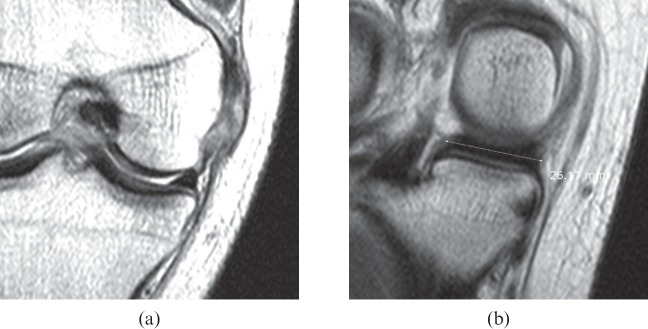
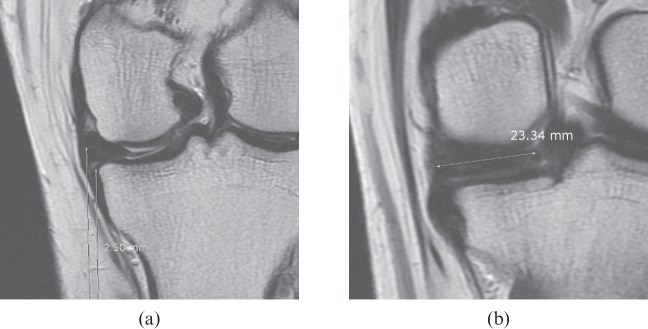
Figure 3.
A 25-year-old male with knee pain. (a) Proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) of the knee at the mid-point demonstrates no definite extrusion of the medial meniscus. A medial collateral ligament tear is seen. (b) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) 15 mm behind (a) shows a 26.2 mm transverse meniscus length. The meniscal extrusion transverse ratio was 0. An intact medial meniscus was confirmed arthroscopically.
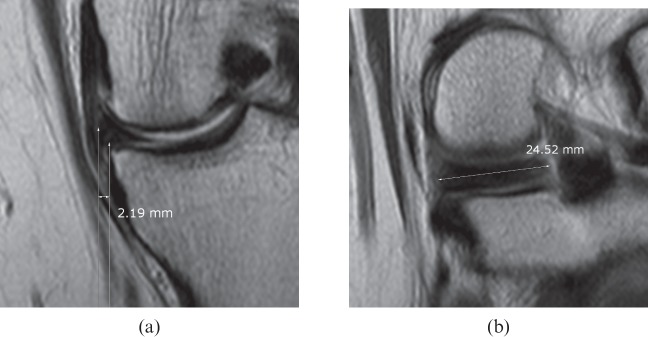
Figure 6.
A 55-year-old female with knee joint pain. (a) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) of the knee at the mid-point shows extrusion of the medial meniscus with a distance of 2.19 mm. (b) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) 15 mm behind (a) shows a 24.5 mm transverse meniscus length. The meniscal extrusion transverse ratio was 0.09. A small radial tear of the posterior horn of the medial meniscus was seen on arthroscopy but a root tear was not observed.
Table 3. p-values of the measurements.
| Parameter | Meniscal root tear vs normal |
Meniscal root tear vs other meniscal tear |
Normal vs other meniscal tear |
|||
| Reader 1 | Reader 2 | Reader 1 | Reader 2 | Reader 1 | Reader 2 | |
| Length of extrusion (L) | <0.001 | <0.001 | <0.001 | <0.001 | 0.708 | 0.974 |
| L/T | <0.001 | <0.001 | <0.001 | <0.001 | 0.868 | 0.699 |
T, transverse diameter of the medial meniscus.
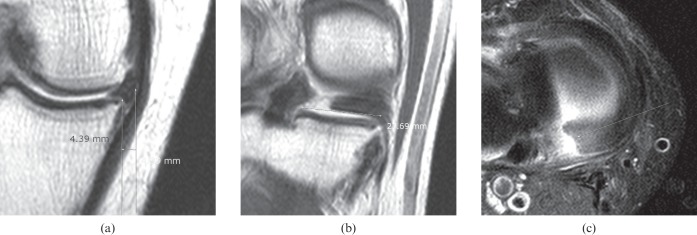
Figure 4.
A 59-year-old male with knee joint swelling. (a) Proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) of the knee at the mid-point shows extrusion of the medial meniscus with a distance of 4.39 mm. (b) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) 15 mm behind (a) shows a 27.7 mm transverse meniscus length. The meniscal extrusion transverse ratio was 0.16. Complete disruption of the medial meniscal root is seen. (c) Fat-saturated proton density imaging (repetition time, 3000 ms; echo time, 36 ms) reveals a definite tear of the posterior root of the medial meniscus. The posterior root tear was confirmed arthroscopically.
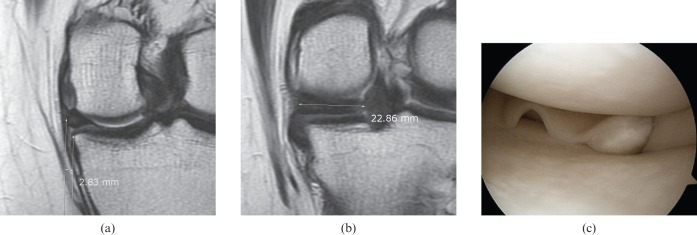
Figure 5.
A 35-year-old female with knee joint pain. (a) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) of the knee at the mid-point shows extrusion of the medial meniscus with a distance of 2.83 mm. (b) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) 15 mm behind (a) shows a 22.9 mm transverse meniscus length. The meniscal extrusion transverse ratio was 0.12. (c) Arthroscopic imaging demonstrates a retracted and avulsed tear of the posterior root of the medial meniscus.
The sensitivities and specificities of a MME threshold of length (2.8, 3 and 3.2 mm) and extrusion ratios with thresholds of 10%, 11% and 12% for the diagnosis of medial meniscal root tears are presented in Table 4. The best diagnostic discrimination was achieved using an extrusion ratio threshold of 10% (79% sensitivity, 86–91% specificity). The threshold value of 2.8, 3.0 and 3.2 mm of MME demonstrated high specificity (98%) but not high sensitivity (42–63%). In six cases of medial meniscal root tears (25%), the MMEs were <3 mm but the L/T ratios were above 10% (Figure 7).
Table 4. Sensitivity and specificity of extrusion ratios in the diagnosis of meniscal root tears.
| Sensitivity (%) |
Specificity (%) |
|||
| Measurement | Reader 1 | Reader 2 | Reader 1 | Reader 2 |
| Extrusion with 2.8 mm threshold | 63 (15/24) | 58 (14/24) | 91 (39/43) | 98 (42/43) |
| Extrusion with 3 mm threshold | 54 (13/24) | 54 (13/24) | 98 (42/43) | 98 (42/43) |
| Extrusion with 3.2 mm threshold | 46 (11/24) | 42 (10/24) | 98 (42/43) | 98 (42/43) |
| Extrusion with 10% threshold | 79 (19/24) | 79 (19/24) | 86 (37/43) | 91 (39/43) |
| Extrusion with 11% threshold | 70 (17/24) | 71 (17/24) | 93 (40/43) | 95 (41/43) |
| Extrusion with 12% threshold | 50 (12/24) | 63 (15/24) | 95 (41/43) | 98 (42/43) |
Numbers in parentheses are the number of patients used to calculate the percentages.
Figure 7.
A 42-year-old female with knee joint pain lasting for 3 months. (a) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) of the knee at the mid-point shows extrusion of the medial meniscus with a distance of 2.50 mm. (b) A proton density coronal image (repetition time, 3000 ms; echo time, 35 ms) 15 mm behind (a) shows a 23.3 mm transverse meniscus length. The meniscal extrusion transverse ratio was 0.11. A posterior root tear of the medial meniscus was diagnosed on arthroscopy.
Discussion
The meniscal roots are critical attachment sites of the menisci to the tibial plateau and are adjacent to the tibial insertions of the cruciate ligaments [7]. The medial meniscus is subjected to more force during weight bearing than the lateral meniscus. Without firm insertion on the tibia, the medial meniscus tends to subluxate medially and lose some of its tension, affecting the ability of the meniscus to absorb and dissipate loads through hoop stresses [8]. The posterior root attachment site of the medial meniscus is critical for maintaining normal meniscal positioning, preventing extrusion and preserving meniscal function [5]. In the current study, 24 of 24 medial meniscal root tear cases (100%) were posterior root tears. The medial meniscal extrusion is not an abnormality itself in subjects with knee pain, but instead a secondary finding that is not uncommon and an important indirect sign of meniscal root tears. MME is present in 79% of patients with complete medial meniscal root tears and in 64% of patients with partial medial meniscal tears. Other causes that result in meniscal extrusion are large radial tears, large complex tears and meniscal degeneration [5]. Other conditions, such as osteoarthritis and joint effusion, also cause extrusion. Previous studies [4-5] have suggested 3 mm as a critical value of extrusion. Miller et al [9] used the transverse width ratio in the diagnosis of extrusions. They set 25% as the minimum amount of displacement, but this was not based on arthroscopic diagnosis, and there was no organised analysis of the transverse ratio with regard to the sensitivity and specificity of meniscal root tears compared with the gold standard of arthroscopic diagnosis. We analysed 10%, 11% and 12% L/T ratios, and compared these with the length threshold. We also analysed 9% and 13% L/T ratios as thresholds, but the results were disappointing. The 10% L/T threshold had a relatively high sensitivity (79%) and specificity (86–91%). The 3 mm threshold had a high specificity but low sensitivity, similar to the 12% L/T threshold. As previously discussed, many (25%) cases exhibited an extrusion length <3 mm but had L/T ratios >10%. Therefore, we recommend use of the L/T ratio criteria instead of 3 mm of extrusion. Because medial menisci have a “C” shape and a curved contour, the transverse diameter as seen on coronal views does not represent the maximal diameter of the medial meniscus, but, on a constant axis and slice thickness, the transverse diameter can reflect the individual medial meniscal size. Costa et al [4] evaluated the correlation of radial tears and meniscal extrusion, and reported that small radial tears involving <50% of the meniscal width had no correlation with meniscal extrusion, but large radial tears involving ≥50% of the meniscal width are associated with meniscal extrusions >3 mm. In the current study, the mean extrusion of the four radial tear cases was 1.68 mm and the L/T ratio was 6%. Therefore, a correlation between radial tears and MME was not identified.
This study has some limitations. The population bias of the patients with regard to osteoarthritis and joint effusion could not be completely removed. As severe osteoarthritis and joint effusion can result in meniscal extrusion, we excluded severe cases of osteoarthritis and joint effusion of more than moderate grade as our intent was to investigate the value of the L/T ratio as an indirect method for diagnosing meniscal root tears. However, milder cases (osteoarthritis of Kellgren–Lawrence Grade 1 or 2) may still have influenced our results to some degree. Another limitation was the relatively small number of positive cases. Additionally, the interval between the MRI and arthroscopy was problematic; however, the arthroscopic studies were performed as soon as possible following MRI, and therapy was performed in the interval time period; therefore, we assumed any change was minimal.
In conclusion, the mean L/T ratio of the meniscal root tears was approximately 13% and was statistically significant. The best diagnostic discrimination was achieved using an extrusion ratio threshold of 10%. The threshold of 3 mm of MME had high specificity but not high sensitivity. Therefore, the use of the L/T ratio in combination with the MME may be a useful method for evaluating medial meniscal root tears.
References
- 1.Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 2006;239:805–10 [DOI] [PubMed] [Google Scholar]
- 2.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 2004;33:569–74 [DOI] [PubMed] [Google Scholar]
- 3.Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 1999;54:502–6 [DOI] [PubMed] [Google Scholar]
- 4.Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol 2004;183:17–23 [DOI] [PubMed] [Google Scholar]
- 5.Jones AO, Houang MT, Low RS, Wood DG. Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol 2006;50:306–13 [DOI] [PubMed] [Google Scholar]
- 6.Rosner B. Fundamentals of biostatics. 6th edn. Belmont, CA: Duxbury Press; 2005 [Google Scholar]
- 7.Brody JM, Hulstyn MJ, Fleming BC, Tung GA. The meniscal roots: gross anatomic correlation with 3-T MRI findings. AJR Am J Roentgenol 2007;188:W446–50 [DOI] [PubMed] [Google Scholar]
- 8.Lee SY, Jee WH, Kim JM. Radila tear of the medial meniscal root: reliability and accuracy of MRI for diagnosis. AJR Am J Roentgenol 2008;191:81–5 [DOI] [PubMed] [Google Scholar]
- 9.Miller TT, Staron RB, Feldman F, Cepel E. Meniscal position on routine MR imaging of the knee. Skeletal Radiol 1997;26:424–7 [DOI] [PubMed] [Google Scholar]