Abstract
Objective
The objective of this study was to retrospectively analyse the treatment results of clinically localised angiosarcoma of the scalp and face.
Methods
The records of 48 patients who were treated between 1987 and 2009 were reviewed. single modality or a combination of surgery, radiotherapy, chemotherapy and immunotherapy were administered. The median follow-up of all 48 patients was 13.7 months (range 2.5–105.9 months).
Results
At the time of analysis, 45 of 48 patients (93.8%) had disease recurrences, and the lung was the most frequent site for recurrence (37 patients). In multivariate analysis, performance status (PS) and number of tumours were significant predictors of lung-metastasis-free (LMF) rate. For patients with multifocal tumours, chemotherapy use significantly decreased the LMF rate (p=0.0072). The 2-year actuarial overall survival (OS), progression-free survival and local control rates in all 48 patients were 22.1%, 10.7% and 46.3%, respectively. In multivariate analysis, PS, number of tumours, surgery and radiotherapy were significant prognostic factors for OS. Patients treated with both surgery and radiotherapy (2-year OS: 45.8%) had a significantly more favourable OS (p<0.0001) than patients treated with either surgery or radiotherapy (2-year OS: 11.1%) and patients treated with neither surgery nor radiotherapy (2-year OS: 0%).
Conclusions
Our results indicated that PS and number of tumours were significant predictors for developing lung metastases. Our results also indicated that PS, number of tumours, surgery use and radiotherapy use were independent prognostic factors for OS. Multimodal treatments including surgery and radiotherapy were effective in improving OS for patients with these tumours.
Advances in knowledge
Multimodal treatments including surgery and radiotherapy are effective in improving overall survival for patients with angiosarcoma of the scalp and face.
Angiosarcomas are rare malignant vascular tumours, which account for approximately 2% of all soft tissue sarcomas. Cutaneous angiosarcomas can occur as lesions in any part of the body, but most frequently arise on the scalp and face of elderly people [1,2]. Several investigators have suggested that angiosarcomas of the scalp and face form a distinctive subgroup due to their extremely poor prognosis, with 5-year survival of only 10–15% [1-3]. This highly aggressive tumour spreads widely through the skin, recurs locally and metastasises early. It is well known that this tumour frequently metastasises to the lung, often inducing repeated pneumothorax and/or haemothorax as a result of rupture of enlarged cystic tumours arising in the peripheral lung field [4,5].
Although previous reports have emphasised the poor prognosis of this disease, effective treatment strategies have yet to be elucidated. Surgery was the mainstay of treatment, but the high frequency of local recurrence of this strategy is discouraging [1,2]. Radiotherapy was generally performed in cases of widely spread and unresectable tumours, but the outcomes were also unsatisfactory [1,3]. Therefore, several authors advocated a combination of surgery and radiotherapy for these tumours [3,6,7]. Recently, chemotherapy and immunotherapy using recombinant interleukin-2 (rIL-2) have been studied as potential treatments [8,9]. However, the optimal treatment for these tumours has not been clearly established.
In the current study, we retrospectively analysed the results of different treatment modalities for clinically localised angiosarcoma of the scalp and face, and investigated the optimal management for these tumours.
Methods and patients
Patient and disease characteristics
A retrospective review of medical records at the University of the Ryukyus Hospital and Okinawa Prefectural South Medical Center in Okinawa, Japan, between the years 1987 and 2009 identified 48 patients who were treated for histologically confirmed clinically localised angiosarcoma of the scalp and face. Angiosarcoma was diagnosed clinically, histopathologically and immunohistopathologically as anti-CD31, anti-CD34 and factor VIII-related antigen. Patient characteristics in all 48 patients are shown in Table 1. The median age of all patients was 76.5 years (range 58–94 years) and the median Eastern Cooperative Oncology Group performance status (PS) was 1 (range 0–3). The clinical maximal primary tumour size ranged from 2 to 14 cm (median 5 cm). In the current study, we analysed the presence of ulceration as well as nodules on the primary tumour, since angiosarcoma of the scalp and face is generally composed of the purpura (bruise-like macule) with or without ulceration and/or nodules. Also, in the current study, numbers of tumours were defined as the numbers of purpura with or without ulceration and/or nodules. This study has been approved by the institutional review board of our institution.
Table 1. Patient and treatment characteristics.
| Parameter | No. of patients | Percentage of patients |
| Maximal tumour diameter (cm) | ||
| 0–4.9 | 22 | 45.8 |
| 5–10 | 21 | 43.8 |
| >10 | 5 | 10.4 |
| ECOG performance status | ||
| 0 | 17 | 35.4 |
| 1 | 11 | 22.9 |
| 2 | 9 | 18.8 |
| 3 | 11 | 22.9 |
| Age (years) | ||
| <70 | 5 | 10.4 |
| 70–79 | 24 | 50.0 |
| 80–89 | 14 | 29.2 |
| 90+ | 5 | 10.4 |
| Ulceration in primary tumour | ||
| Yes | 17 | 35.4 |
| No | 31 | 64.6 |
| Nodule in primary tumour | ||
| Yes | 32 | 66.7 |
| No | 16 | 33.3 |
| Tumour site | ||
| Scalp | 46 | 95.8 |
| Face | 2 | 4.2 |
| Gender | ||
| Female | 19 | 39.6 |
| Male | 29 | 60.4 |
| Clinically positive neck lymph nodes | ||
| Absent | 45 | 93.8 |
| Present | 3 | 6.2 |
| Number of tumours | ||
| Single | 28 | 58.3 |
| Multifocal | 20 | 41.7 |
| Treatments | ||
| RT+SR+CH+IT | 5 | 10.4 |
| RT+SR+CH | 2 | 4.2 |
| RT+SR+IT | 9 | 18.8 |
| RT+SR | 1 | 2.1 |
| RT+CH+IT | 5 | 10.4 |
| RT+CH | 5 | 10.4 |
| RT+IT | 10 | 20.8 |
| RT | 5 | 10.4 |
| SR+CH+IT | 2 | 4.2 |
| IT | 4 | 8.3 |
CH, chemotherapy; ECOG, Eastern Cooperative Oncology Group; IT, immunotherapy; RT, radiotherapy; SR, surgery.
Treatment
Treatment characteristics in all 48 patients are shown in Table 1. In total, radiotherapy, surgery, chemotherapy and immunotherapy were administered in 42 patients, 19 patients, 19 patients and 35 patients, respectively. For each treatment, informed consent was obtained from all 48 patients. Radiotherapy was delivered with a 6- to 12-MV electron beam or a 4-MV X-ray linear accelerator. Daily fractions of 1.8–2.0 Gy at 5 days per week were used in 37 patients, and daily fractions of 3–4 Gy at 5 days per week were used in the remaining 5 patients. Acrylic plates were used to achieve the desired skin dose as necessary. Planning target volume (PTV) included 3- to 5-cm margins for clinical target volume in all 48 patients. The total radiation doses ranged from 26 to 71.6 Gy (median 60 Gy), and the PTV included the primary tumour in 39 patients, and primary tumour and the clinically positive lymph node area in 3 patients. Surgery was performed in 19 patients, and the resection included the primary tumour along with 3- to 5-cm margins. Surgical margins at the primary tumour were positive in 10 patients, negative in 6 patients and unknown in the remaining 3 patients. For the 19 patients receiving chemotherapy, docetaxel was given at 25–30 mg m−2 weekly for 3 weeks, with a 1-week rest until disease progression or unacceptable toxicity was reached. Immunotherapy using rIL-2 was performed in 35 patients via systemic administration or intratumoral injection. The total dose of rIL-2 ranged from 30×105 to 194×105 units (systemic: 30×105 to 119×105 units; intratumoral: 3.5×105 to 194×105 units), administered at a dose of 3.5×105 to 10×105 units weekly (systemic: 3.5×105 to 10×105 units; intratumoral: 3.5×105 to 5×105 units).
Statistical analysis
The median follow-up of all 48 patients was 13.7 months (range 2.5–105.9 months). Distant metastases, including lung metastases, were defined as an apparent tumour recurrence detected by CT scans and/or bone scans after initial treatment. Overall survival (OS), progression-free survival (PFS), lung metastases-free (LMF) rate and local control (LC) rate were calculated actuarially according to the Kaplan–Meier method, and were measured starting from the day of initial treatment. Differences between groups were estimated using the log-rank test. Multivariate analysis was performed using the Cox regression model. A probability level of 0.05 was chosen to denote statistical significance. Statistical analysis was performed using the SPSS software package (v. 11.0; SPSS Inc., Chicago, IL).
Results
Recurrence patterns
At the time of analysis, 45 patients (93.8%) had disease recurrence (local only in 3 patients, regional lymph nodes only in 2 patients, lung only in 14 patients and multiple sites in 26 patients). Of the 26 patients with multiple recurrences, 18 patients had simultaneous local recurrence, and 23 patients had simultaneous lung recurrence. In total, local recurrence occurred in 21 patients (43.8%), and lung metastases occurred in 37 patients (77.1%). Overall, lungs were the most frequent site for recurrence. Among the 37 patients with lung metastases, the median survival time after the appearance of lung metastases was 4.0 months (range 0.2–33.1 months).
The high frequency of lung metastases observed prompted us to investigate potential predictive factors for developing lung metastases. Table 2 shows the univariate analysis of various potential prognostic factors for LMF rates. In this analysis, PS and the number of tumours were significantly correlated with LMF rates. Additionally, PS (relative risk: 0.210; 95% confidence interval: 0.089–0.498; p<0.001) and number of tumours (relative risk: 0.321; 95% confidence interval: 0.155–0.668; p=0.002) remained significant independent prognostic factors for LMF rates in multivariate analysis. We further investigated whether radiotherapy, surgery, chemotherapy and immunotherapy could prevent or delay the occurrence of lung metastases for patients with PS of 2–3 and those with multifocal tumours (Table 3). No significant differences in LMF rates were noted in response to radiotherapy, surgery, chemotherapy and immunotherapy among patients with PS of 2–3. On the other hand, among patients with multiple tumours, significant differences in LMF rates were noted between patients treated with chemotherapy and those treated without chemotherapy (p=0.0072; Figure 1).
Table 2. Univariate analysis of various potential prognostic factors for lung metastasis-free rates in patients with angiosarcoma of the scalp or face.
| Parameter | No. of patients | Univariate analysis |
|
| LMF, 1-year rate (%) | p-value | ||
| Age (years) | |||
| <80 | 29 | 36.1 | 0.9358 |
| ≥80 | 19 | 11.8 | |
| Gender | |||
| Female | 19 | 41.1 | 0.8036 |
| Male | 29 | 34.2 | |
| Tumour size (cm) | |||
| <5 | 22 | 29 | 0.1138 |
| ≥5 | 26 | 44.5 | |
| ECOG performance status | |||
| 0–1 | 28 | 47.0 | 0.0099 |
| 2–3 | 20 | 20.0 | |
| Ulceration in primary tumour | |||
| Yes | 17 | 43.8 | 0.0883 |
| No | 31 | 17.7 | |
| Nodule in primary tumour | |||
| Yes | 37 | 36.4 | 0.2075 |
| No | 11 | 8.2 | |
| Tumour site | |||
| Scalp | 46 | 34.7 | 0.6940 |
| Face | 2 | 0 | |
| Clinically positive neck lymph nodes | |||
| Negative | 45 | 36.8 | 0.9610 |
| Positive | 3 | 33.3 | |
| Tumour number | |||
| Single | 28 | 54.7 | 0.0034 |
| Multifocal | 20 | 6.9 | |
ECOG, Eastern Cooperative Oncology Group; LMF, lung metastasis-free.
Table 3. Lung metastasis-free (LMF) rates in patients with ECOG performance status of 2–3 and patients with multifocal tumours according to treatment modalities.
| Patient population | Treatment | No. of patients | LMF, 1-year rate (%) | p-value |
| ECOG performance status 2–3 (n=20) | ||||
| Radiotherapy | Yes | 15 | 25.0 | 0.1157 |
| No | 5 | 0 | ||
| Surgery | Yes | 8 | 25.0 | 0.7997 |
| No | 12 | 14.6 | ||
| Chemotherapy | Yes | 4 | 0 | 0.3340 |
| No | 16 | 26.8 | ||
| Immunotherapy | Yes | 14 | 18.4 | 0.8146 |
| No | 6 | 25.0 | ||
| Multifocal tumours (n=20) | ||||
| Radiotherapy | Yes | 17 | 7.4 | 0.1712 |
| No | 3 | 0 | ||
| Surgery | Yes | 4 | 25.0 | 0.6267 |
| No | 16 | 0 | ||
| Chemotherapy | Yes | 6 | 16.7 | 0.0072 |
| No | 14 | 0 | ||
| Immunotherapy | Yes | 14 | 10.7 | 0.3098 |
| No | 6 | 0 | ||
ECOG, Eastern Cooperative Oncology Group.
Figure 1.
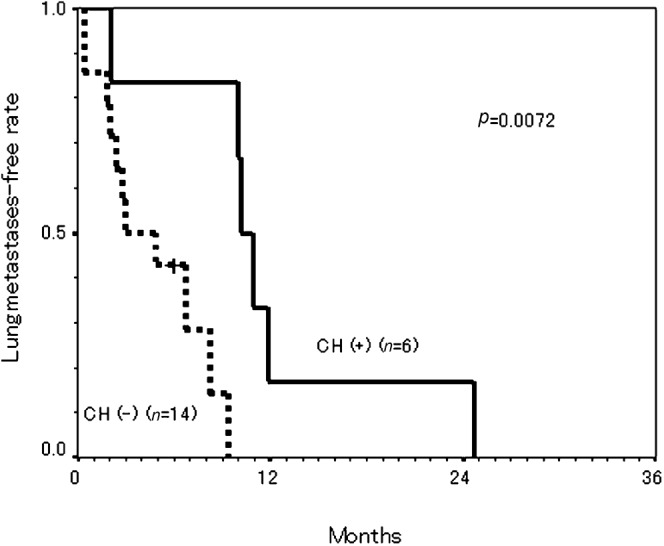
Lung metastasis-free rates in patients with multiple tumours according to chemotherapy (CH) use.
The 2-year actuarial LC rate in all 48 patients was 46.3%. Because both surgery and radiotherapy have been reported to be effective treatments for local therapy [6,7], we compared the LC rates according to the treatment modality and total radiation dose. Table 4 shows the LC status of radiotherapy with or without surgery according to total radiation dose. Among patients treated with radiotherapy only, in-field recurrence occurred in 4 of 11 patients (36.4%) treated with <70 Gy, but none of 14 patients treated with ≥70 Gy had in-field recurrence. Concerning patients treated with both radiotherapy and surgery, in-field recurrence occurred in 2 of 6 patients (33.3%) treated with <60 Gy, while none of 11 patients treated with ≥60 Gy had in-field recurrence.
Table 4. Incidences of local control according to the treatment modality and radiation dose.
| Treatment |
Total radiation |
No. of patients | Locally controlled | Local recurrence |
||
| In field | Marginal field | Out field | ||||
| Modality | Dose | |||||
| RT | <70 Gy | 11 | 3 | 4 (36.4%) | 2 | 2 |
| ≥70 Gy | 14 | 11 | 0 | 1 | 2 | |
| SR+RT | <60 Gy | 6 | 3 | 2 (33.3%) | 1 | 1 |
| ≥60 Gy | 11 | 5 | 0 | 1 | 4 | |
RT, radiotherapy; SR, surgery.
Survival
At the time of analysis, 46 of 48 patients (95.8%) had died, and the median survival time, 2-year OS rate and 2-year PFS rate in all 48 patients were 13.4 months, 22.1% and 10.7%, respectively. Patients with PS of 2–3 had a significantly poorer OS than patients with PS of 0–1. Also, patients with multifocal tumours had a significantly poorer OS than patients with single tumours. In univariate analysis, PS, number of tumours, surgery, radiotherapy and chemotherapy all had a significant impact on OS (Table 5). In multivariate analysis, PS (relative risk: 0.457; 95% confidence intervals: 0.226–0.923; p=0.029), number of tumour (relative risk: 0.403; 95% confidence intervals: 0.196–0.825; p=0.013), surgery use (relative risk: 2.423; 95% confidence intervals: 1.157–5.074; p=0.019) and radiotherapy use (relative risk: 4.458; 95% confidence intervals: 1.629–12.197; p=0.004) remained significant independent prognostic factors for OS.
Table 5. Univariate analysis of various potential prognostic factors for overall survival in patients with angiosarcoma of the scalp or face.
| Parameter | No. of patients | Univariate analysis |
|
| OS, 2-year rate (%) | p-value | ||
| Age (years) | |||
| <80 | 29 | 30.3 | 0.2473 |
| ≥80 | 19 | 10.5 | |
| Gender | |||
| Female | 19 | 15.8 | 0.6229 |
| Male | 29 | 26.2 | |
| Maximal tumour size (cm) | |||
| <5 | 22 | 25.6 | 0.4459 |
| ≥5 | 26 | 19.2 | |
| ECOG performance status | |||
| 0–1 | 28 | 38.5 | 0.0010 |
| 2–3 | 20 | 10.0 | |
| Ulceration in primary tumour | |||
| Yes | 17 | 11.8 | 0.0124 |
| No | 31 | 27.0 | |
| Nodule in primary tumour | |||
| Yes | 32 | 26.9 | 0.1476 |
| No | 16 | 12.5 | |
| Tumour site | |||
| Scalp | 46 | 23.1 | 0.5066 |
| Face | 2 | 0 | |
| Clinically positive neck lymph nodes | |||
| Absent | 45 | 21.3 | 0.7741 |
| Present | 3 | 33.3 | |
| Number of tumour | |||
| Single | 28 | 34.6 | 0.0002 |
| Multifocal | 20 | 0.5 | |
| Chemotherapy use | |||
| Yes | 19 | 36.1 | 0.0455 |
| No | 29 | 13.8 | |
| Radiotherapy use | |||
| Yes | 42 | 25.3 | 0.0008 |
| No | 6 | 0 | |
| Immunotherapy use | |||
| Yes | 35 | 25.7 | 0.1457 |
| No | 13 | 15.4 | |
| Surgery | |||
| Yes | 19 | 40.7 | 0.0021 |
| No | 29 | 10.4 | |
ECOG, Eastern Cooperative Oncology Group; OS, overall survival.
In order to evaluate the efficacy of surgery and radiotherapy, we divided patients into three groups according to the use of surgery and radiotherapy (patients treated with both surgery and radiotherapy; patients treated with either surgery or radiotherapy; patients treated with neither surgery nor radiotherapy). The 2-year OS rates in patients treated with both surgery and radiotherapy, patients treated with either surgery or radiotherapy and patients treated with neither surgery nor radiotherapy were 45.8%, 11.1% and 0%, respectively (Figure 2). There were significant differences on OS among the groups (p<0.0001).
Figure 2.
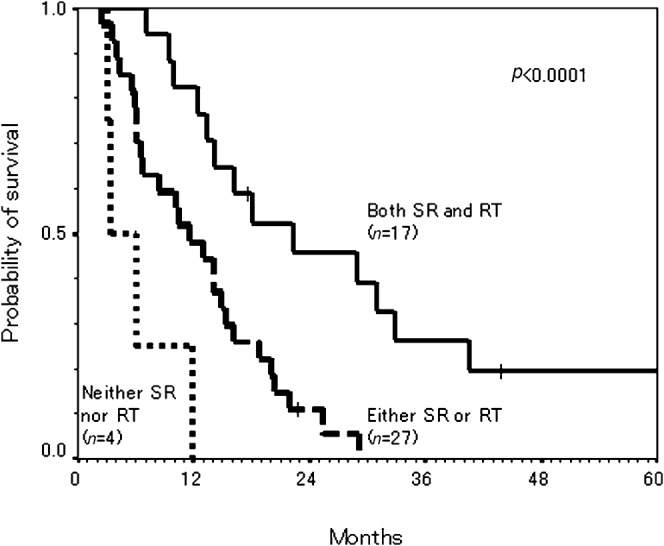
Overall survival (OS) curves by Kaplan–Meier method according to administration of radiotherapy (RT) and surgery (SR) in patients with angiosarcoma of the face and scalp.
Long-term survivors
There were four patients (8.3%) who survived for more than 3 years. All four patients had PS of 0–1 and also had a single tumour. Three patients were treated with a combination of surgery, radiotherapy, chemotherapy and immunotherapy, and the remaining one patient received a combination of surgery, radiotherapy and immunotherapy. No late complications were observed in any of the four patients. Three patients died of angiosarcoma (survival times: 105.9 months, 82.8 months and 40.5 months), and the remaining one patient is alive and free of disease (survival time: 43.8 months).
Discussion
The current study indicated that lungs were the most frequent site for recurrence in patients with angiosarcoma of the scalp and face. Several authors have previously reported high frequencies of lung metastases with this disease [4,5]. Moreover, patients with scalp and face lesions had frequent pulmonary complications because of lung metastases, such as pneumonia, haemothorax, atelectasis and pneumothorax, compared with patients with non-scalp lesions. In the current study, the median survival time after lung metastases was 4 months, which is in complete agreement with the estimated mean survival of 4 months previously reported [10]. As the prognoses of patients who developed lung metastases are poor, it is imperative to elucidate the risk factors for developing lung metastases in these patients.
In the current study, PS and the number of tumours were significant risk factors for developing lung metastases. To our knowledge, this is the first report indicating the potential risk factors for developing lung metastases among patients treated for angiosarcoma of the scalp and face. Although lung metastases of angiosarcoma are often the main cause of death, optimal treatment strategies for preventing or treating lung metastases have not been documented. In the current study, no significant differences in LMF rates were noted in response to radiotherapy, surgery, chemotherapy and immunotherapy among patients with PS 2–3. One of the reasons for the absence of significant differences may be that patients with PS 2–3 have often been treated with fewer-combination treatments or lesser doses of radiotherapy. On the other hand, in the current study, chemotherapy use (docetaxel) was effective in delaying the occurrence of lung metastases in patients with multifocal tumours. A meta-analysis of localised soft tissue sarcomas of adults has provided evidence that adjuvant doxorubicin-based chemotherapy is useful in this regard as it significantly improved the distant recurrence-free time [11]. Recently, several reports have indicated that, owing to its angiogenic activity, taxane-based chemotherapy offers clinical benefit to patients with angiosarcoma [8,12]. Isogai et al [12] reported that docetaxel treatment of a patient with angiosarcoma of the scalp with lung metastases resulted in complete remission of lung metastases. These results suggest that chemotherapy, especially taxane-based chemotherapy, may be effective in preventing or treating lung metastases in patients with these tumours. Further studies are required to confirm these preliminary findings.
Despite intensive therapies, local recurrences in patients with angiosarcoma of the scalp and face are frequent, ranging in frequency from 35% to 86% [7,9,13]. For local therapy, several authors indicated that radiotherapy as well as the combination of surgery and radiotherapy were significantly associated with improved LC in patients with angiosarcoma of the scalp and face [1,7,9,14]. However, the optimal management of radiotherapy, such as radiation field and radiation dose, has not been clarified. Since the involved dermis, as well as a considerable area of surrounding skin, can be treated while the brain and other normal tissues are spared, wide-field electron beam radiotherapy using 3- to 5-cm margins seems to be a rational therapeutic approach for angiosarcoma of the scalp and face [2,9]. In terms of radiation dose, several authors generally recommend approximately 60 Gy in 30 fractions for treatment of a primary tumour [3,14]. In the current study, of the patients treated with radiotherapy only (macroscopic disease), in-field recurrence occurred in 4 of 11 patients (36.4%) treated with less than 70 Gy, while none of 14 patients treated with 70 Gy or more had in-field recurrence. These results suggest that total doses of 70 Gy or more in conventional fractionations are effective in preventing local recurrence in patients with macroscopic disease. Concerning patients treated with both radiotherapy and surgery (microscopic disease), in-field recurrence occurred in 2 of 6 patients (33.3%) treated with less than 60 Gy, while none of 11 patients treated with 60 Gy or more had in-field recurrence. These results suggest that total doses of 60 Gy or more in conventional fractionations are effective in preventing local recurrence in patients with microscopic disease. However, recurrence outside the radiation field remains a problem in patients treated with radiotherapy, as well as patients treated with radiotherapy and surgery. In order to reduce the marginal and out-field recurrence, other techniques, such as intensity-modulated radiotherapy and high dose rate brachytherapy with a surface mould technique, may be necessary to achieve optimal results [15,16].
Several previous studies have suggested potential prognostic factors associated with tumour size, tumour type, age and radiotherapy use in patients with angiosarcoma of the scalp and face [2,7,13,14,17]. In the current study, concerning patient characteristics, PS and number of tumours were independent prognostic factors for OS. In many cancers, PS has been a strong predictor for survival [18]. Indeed, our results suggest that patients with PS of 2–3 had a significantly poorer OS than patients with PS of 0–1. Additionally, patients with multifocal tumours had a significantly poorer OS than patients with solitary tumour in the current study. Multifocal lesions on presentation may be due to a delay in the clinical diagnosis of angiosarcoma, which allows the lesion to progress unfettered, resulting in an eventual worse prognosis. Pawlik et al [7] reported that the presence of multifocal lesions was significantly predictive of shorter time to recurrence. While we did not find maximum tumour size to be a significant predictor of OS, this may be due to the fact that clinical tumour sizes measured in the current study were underestimated in some patients because of the difficulty in correctly evaluating the degree of peripheral extension [7].
Concerning treatment characteristics, radiotherapy and surgery were independent prognostic factors for OS in the current study. Since several reports have provided proof of a treatment efficacy of radiotherapy and surgery for patients with angiosarcoma of the scalp and face, this treatment combination has been recommended as an ideal treatment of these tumours [1,6,7,14]. Guadagnolo et al [14] analysed 70 patients with angiosarcoma of the scalp and face and found that combined surgery and radiotherapy was associated with improved OS, disease-specific survival and LC compared with surgery or radiotherapy alone. Hodgkinson et al [1] demonstrated that 2 of 13 patients treated with both surgery and radiotherapy survived for more than 5 years. In the current study, patients treated with both surgery and radiotherapy had a significantly more favourable OS than patients treated with either surgery or radiotherapy alone, or patients treated with neither surgery nor radiotherapy. These results indicate that multimodal treatments including surgical resection and radiotherapy are effective in improving OS for patients with these tumours. However, because patients with PS 2–3 tend to be treated with a more limited combination of treatment, further studies are needed to investigate the optimal treatment strategy for these patients.
Although a combination of surgery and radiotherapy appears as an effective treatment for local therapy, most patients ultimately develop distant metastases, especially in the lung. In the current study, chemotherapy using docetaxel was effective in delaying lung metastases, thereby reinforcing the notion that chemotherapy is a promising strategy for delaying/preventing distant metastases. Furthermore, rIL-2 has emerged as an attractive strategy for preventing distant metastases. rIL-2 activates lymphokine-activated killer cells and natural killer (NK) cells, which subsequently injure vascular endothelial cells by adhering to the cells and causing their lysis [19]. Several reports have indicated that a combination of radiotherapy plus rIL-2 may produce an addictive sensitising effect [9,13]. Ohguri et al [9] found that arterial or intratumoral administration combined with systemic administration of rIL-2 resulted in better distant metastasis-free survival rates. Recently, bevacizumab, a recombinant humanised antibody against vascular endothelial growth factor (VEGF), has also emerged as a promising strategy, since VEGF is overexpressed in approximately 80% of human angiosarcomas. Koontz et al [20] reported that one of two patients with nasal angiosarcomas achieved complete response when treated with bevacizumab and radiotherapy. Further studies are needed to investigate the role of chemotherapy, rIL-2 and bevacizumab for angiosarcoma of the scalp and face.
In the current study, 4 patients (8.3%) survived for more than 3 years. All four patients had PS of 0–1 and also had a single tumour. Three of these patients were treated with a combination of surgery, radiotherapy, chemotherapy and immunotherapy, and the remaining one patient received a combination of surgery, radiotherapy and immunotherapy. Therefore, for patients with a favourable prognosis, intensive treatments using surgery, radiotherapy, chemotherapy and immunotherapy may provide a long-term survival. Further prospective studies are needed to assess the efficacy of intensive treatment strategies using surgery, radiotherapy, chemotherapy and immunotherapy for these tumours.
In conclusion, our results indicated that the incidences of lung metastases were frequent among patients treated for angiosarcoma of the scalp and face, and a PS of 2–3 and multifocal tumours were found to be significant risk factors for developing lung metastases. For patients with multifocal tumours, taxane-based chemotherapy may delay or prevent the lung metastases. Our results also indicated that PS, number of tumours, radiotherapy and surgery were independent prognostic factors for OS. Multimodal treatments including surgery and radiotherapy were effective in improving OS for patients with these tumours, and the addition of chemotherapy and immunotherapy may further improve OS. However, since this study is retrospective and includes various treatment modalities, further prospective studies are required to confirm our results.
References
- 1.Hodgkinson DJ, Soule EH, Woods JE. Cutaneous angiosarcoma of the head and neck. Cancer 1979;44:1106–13 [DOI] [PubMed] [Google Scholar]
- 2.Holden CA, Spittle MF, Jones EW. Angiosarcoma of the face and scalp, prognosis and treatment. Cancer 1987;59:1046–57 [DOI] [PubMed] [Google Scholar]
- 3.Mendenhall WM, Mendenhall CM, Werning JW, Reith JD, Mendenhall NP. Cutaneous angiosarcoma. Am J Clin Oncol 2006;29:524–8 [DOI] [PubMed] [Google Scholar]
- 4.Kitagawa M, Tanaka I, Takemura T, Matsubara O, Kasuga T. Angiosarcoma of the scalp: report of two cases with fatal pulmonary complications and a review of Japanese autopsy registry data. Virchows Arch A Pathol Anat Histopathol 1987;412:83–7 [DOI] [PubMed] [Google Scholar]
- 5.Nomura M, Nakaya Y, Saito K, Miyoshi H, Kishi F, Hibino S, et al. Hemopneumothorax secondary to multiple cavitary metastasis in angiosarcoma of the scalp. Respiration 1994;61:109–12 [DOI] [PubMed] [Google Scholar]
- 6.Ward JR, Feigenberg SJ, Mendenhall NP, Marcus RB, Jr, Mendenhall WM. Radiation therapy for angiosarcoma. Head Neck 2003;25:873–8 [DOI] [PubMed] [Google Scholar]
- 7.Pawlik TM, Paulino AF, McGinn CJ, Baker LH, Cohen DS, Morris JS, et al. Cutaneous angiosarcoma of the scalp: a multidisciplinary approach. Cancer 2003;98:1716–26 [DOI] [PubMed] [Google Scholar]
- 8.Nagano T, Yamada Y, Ikeda T, Kanki H, Kamo T, Nishigori C. Docetaxel: a therapeutic option in the treatment of cutaneous angiosarcoma: report of 9 patients. Cancer 2007;110:648–51 [DOI] [PubMed] [Google Scholar]
- 9.Ohguri T, Imada H, Nomoto S, Yahara K, Hisaoka M, Hashimoto H, et al. Angiosarcoma of the scalp treated with curative radiotherapy plus recombinant interleukin-2 immunotherapy. Int J Radiat Oncol Biol Phys 2005;61:1446–53 [DOI] [PubMed] [Google Scholar]
- 10.Morgan MB, Swann M, Somach S, Eng W, Smoller B. Cutaneous angiosarcoma: a case series with prognostic correlation. J Am Acad Dermatol 2004;50:867–74 [DOI] [PubMed] [Google Scholar]
- 11.Sarcoma Meta-analysis Collaboration Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997;350:1647–54 [PubMed] [Google Scholar]
- 12.Isogai R, Kawada A, Aragane Y, Tezuka T. Successful treatment of pulmonary metastasis and local recurrence of angiosarcoma with docetaxel. J Dermatol 2004;31:335–41 [DOI] [PubMed] [Google Scholar]
- 13.Sasaki R, Soejima T, Kishi K, Imajo Y, Hirota S, Kamikonya N, et al. Angiosarcoma treated with radiotherapy: impact of tumor type and size on outcome. Int J Radiat Oncol Biol Phys 2002;52:1032–40 [DOI] [PubMed] [Google Scholar]
- 14.Guadagnolo BA, Zagars GK, Araujo D, Ravi V, Shellenberger TD, Sturgis EM. Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp. Head Neck 2011;33:661–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakamura R, Harada S, Obara T, Ehara S, Yoshida A, Akasaka T, et al. Iridium-192 brachytherapy for hemorrhagic angiosarcoma of the scalp: a case report. Jpn J Clin Oncol 2003;33:198–201 [DOI] [PubMed] [Google Scholar]
- 16.Bedford JL, Childs PJ, Hansen VN, Warrington AP, Mendes RL, Glees JP. Treatment of extensive scalp lesions with segmental intensity-modulated photon therapy. Int J Radiat Oncol Biol Phys 2005;62:1549–58 [DOI] [PubMed] [Google Scholar]
- 17.Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol 2010;11:983–91 [DOI] [PubMed] [Google Scholar]
- 18.Karnofsky DA. Problems and pitfalls in the evaluation of anticancer drugs. Cancer 1965;18:1517–28 [DOI] [PubMed] [Google Scholar]
- 19.Damle NK, Doyle LV, Bender JR, Bradley EC. Interleukin 2-activated human lymphocytes exhibit enhanced adhesion to normal vascular endothelial cells and cause their lysis. J Immunol 1987;138:1779–85 [PubMed] [Google Scholar]
- 20.Koontz BF, Miles EF, Rubio MA, Madden JF, Fisher SR, Scher RL, et al. Preoperative radiotherapy and bevacizumab for angiosarcoma of the head and neck: two case studies. Head Neck 2008;30:262–6 [DOI] [PubMed] [Google Scholar]


