Abstract
Buccal bifurcation cyst (BBC) is a rare inflammatory odontogenic cyst that typically occurs at the buccal region of the first or second mandibular molars of children. In the current case, a 9-year-old boy complained of an extraoral soft tissue painful swelling. Intraoral examination revealed a partial eruption of the right permanent mandibular first molar with drainage of purulent material and clinical absence of the left mandibular first molar. Panoramic radiographic and computed tomography showed two well-defined areas surrounding the mandibular first molars consistent with cystic lesions. Surgical enucleations were performed and histopathologic analysis revealed inflammatory cysts. Based on the clinical, microscopic, radiographic, and CT images, the diagnosis of bilateral BBC was established. Patient has been under follow-up for about 1 year showing normal bone repair and eruption of the involved teeth. Although BBC is uncommon, it is important to recognize this entity.
Keywords: Pediatric, Molar pathology, Mandibular diseases, Radiography, Furcation defects, Therapy
Introduction
Buccal bifurcation cyst (BBC) is an uncommon inflammatory odontogenic cyst that was first reported in 1983 by Stoneman and Worth [1]. The BBC has been described with several names, such as mandibular infected buccal cyst-molar area [2], circumferential dentigerous cyst [3], buccal bifurcation cyst [4] and juvenile paradental cyst [5]. In 1992, it was included by the World Health Organization (WHO) in their histologic typing of odontogenic tumors listed in the category of “paradental cyst” and named “mandibular infected buccal cyst” [6].
BBC occurs in children between 4 and 14 years and predominantly affects the mandibular first molar. Occasionally, the mandibular second molar may be the involved tooth. Delayed tooth eruption and swelling at the affected area is commonly observed. In some cases, partial tooth eruption with crown buccal tilting and deep periodontal pockets may be present. BBC is often asymptomatic but infection, with drainage of pus, and pain can be present [4].
Radiographically, it is characterized by a well-defined radiolucent lesion circumscribing the roots of the involved tooth with intact lamina dura. Histologically, the cyst wall shows a chronic inflammatory infiltration and is lined by a non-keratinized stratified squamous epithelium. Enucleation without tooth extraction is the treatment of choice [7]. The aim of the current paper is to report an additional case of bilateral BBC and to review the literature.
Case Report
A 9-year-old boy was referred with a chief complaint of abrupt asymmetric enlargement of the face. Extraoral clinical examination revealed a painful swelling on the right side of the face (Fig. 1). Intraoral clinical examination revealed bilateral enlargement of the lower posterior alveolar ridge and partial eruption of the right permanent mandibular first molar with discharge of purulent material, as well as clinical absence of the left permanent mandibular first molar. On palpation, buccal bone expansion covered by normal mucosa adjacent to the mandibular first molars was observed bilaterally (Fig. 2). The patient brought radiographs and computed tomography imaging, ordered by his parents who are dentists. Interestingly, although the swelling was on the right site, the panoramic radiograph showed a radiolucent well-defined lesion on the left side involving the periapical region of the permanent first mandibular molar (Fig. 3). Computed tomography and 3D reconstruction displayed more details of the left-sided lesion where buccal expansion could be seen with a preserved cortical bone. A similar lesion was observed on the right, involving the permanent mandibular first molar, both consistent with cystic lesions (Fig. 4). The patient’s parents also brought a panoramic radiograph ordered 2 years earlier to evaluate teeth eruption, and this showed a radiolucent area surrounding both the right and the left mandibular permanent first molar, suggesting a thickening of the dental follicle (Fig. 5). In order to control infection, amoxicillin was prescribed at the first visit for a 7-day period. After 1 week, there was no swelling, pain, or drainage. Therefore, surgical curettage was performed on the left-sided lesion and microscopic analyses showed a thin non-keratinized stratified squamous epithelium and chronic inflammation, compatible with an inflammatory cyst (Fig. 6). Based on clinical, radiographic, and histopathologic findings, the diagnosis of BBC was made. The same surgical procedure was performed on the right side resulting in the same diagnosis. The patient has been under follow-up for approximately 1 year, demonstrating bone healing and a normal eruption pattern (Fig. 7).
Fig. 1.

The extraoral examination revealed a painful swelling on the right side of the face
Fig. 2.

Intraoral view showing absence of the lower first molars and peripheral enlargement
Fig. 3.
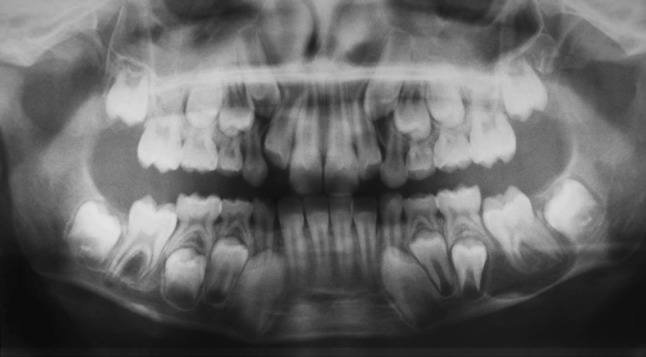
Panoramic radiograph showing bilateral, well-defined radiolucent lesions associated with the roots of the mandibular first molars
Fig. 4.
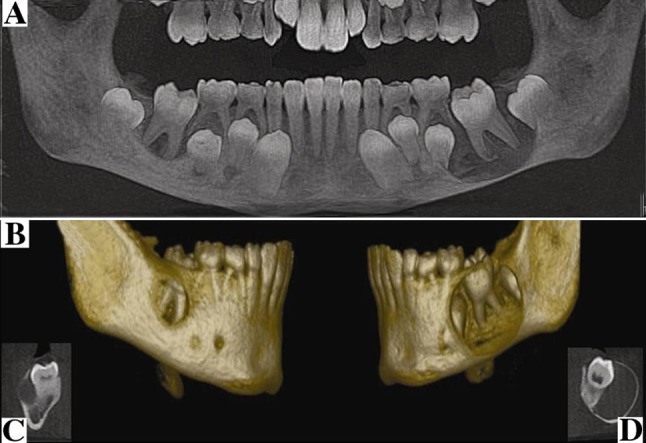
a Computerized tomography showing hypodense areas associated with the lower first permanent molars bilaterally; b 3D reconstruction, showing involvement of the area of cementum-enamel of the permanent molars, with greater involvement on the left side expanding to the base of the mandible; c right sagittal sections and d left sagittal sections
Fig. 5.

Radiograph showing enlargement of the first mandibular permanent molars on the right and left
Fig. 6.
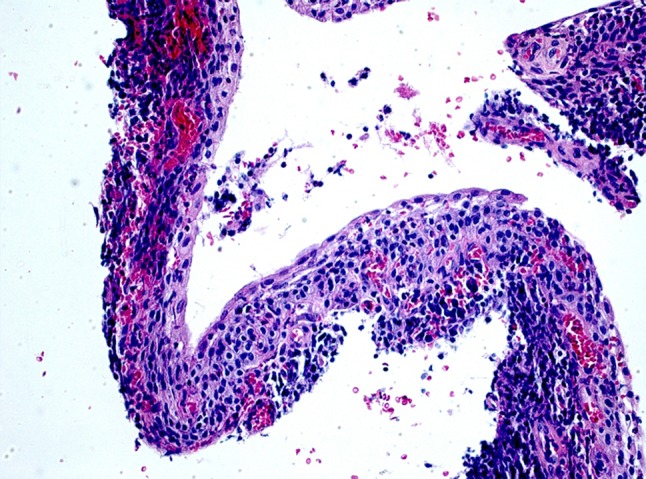
Photomicrograph of cyst lining with hematoxylin-eosin stains (original magnification ×20)
Fig. 7.

Panoramic radiograph 8 months after enucleation. Both teeth demonstrate bony fill, healing of the lesion, and a normal eruption pattern
Discussion
The etiology of BBC is still uncertain; however, it is postulated that the tooth breaks the oral mucosa during eruption, thereby causing inflammation and activating the proliferation of epithelial cells, which ultimately forms a cyst. It is also speculated that the tilted mesiobuccal cusp and deep periodontal pockets may be the origin of the inflammation [1, 8]. Other local predisposing factors include enamel projections from the cemento-enamel junction into the furcation and covered by reduced enamel epithelium that lead to cyst formation [9].
There are some similarities between dentigerous cysts, paradental cysts, and BBCs, particularly the fact that they all are associated with the crown tooth. Dentigerous cysts and paradental cysts occur with more frequency in the third mandibular molars of adults [10, 11]. A dentigerous cyst has been considered a developmental cyst involving a crown of a non-erupted tooth. Interestingly, there is a variant of dentigerous cyst called “circumferential dentigerous cyst” that occurs in the first or second mandibular molars and interferes with tooth eruption [5]. On the other hand, a paradental cyst is classified as an inflammatory cyst arising on the lateral side of a vital tooth. However, some authors have used the term “inflamed dentigerous cyst” in these cases arguing that it may be difficult to determine if the inflammation was a cause of the dentigerous cyst, or a secondary feature arising in a previous dentigerous cyst [6, 12].
In addition, paradental cysts and BBC are associated with tooth eruption. Paradental cysts on the buccal side have many similar characteristics to the BBC. These common features have caused confusion and different names have been previously used to classify the same lesion [1, 5, 6]. Although both cysts are inflammatory, BBC develops more commonly on the buccal side of the first and second mandibular molars of children. These unique characteristics should help facilitate their recognition. Moreover, it seems more reasonable to consider dentigerous cysts, paradental cysts, and BBCs as different entities.
Radiologic features are also very important to help recognize and distinguish between these cystic lesions. Although cysts normally have a well-demarcated radiolucency with a corticated margin, they may present some peculiar features. Dentigerous cysts present as a radiolucent area around the crown of a non-erupted tooth, while paradental cysts arise on the lateral crown of a partially erupted tooth. However, the radiographic distinction of BBC from circumferential dentigerous cysts may be a challenge as both are characterized by radiolucency involving the whole tooth. Computed tomography is extremely useful, as axial and coronal views may show buccal expansion, which is normally found in BBC. In addition, BBC may show bone loss in the furcation of the involved tooth [13]. Surgical findings, such as the presence of bone cavitation and cystic content, are also notable features [14].
The association of clinical, radiographic, and computed tomography displaying a cystic lesion with buccal expansion involving a mandibular first molar in a young patient can strongly suggest BBC as a differential diagnosis and histologic examination is needed to confirm the diagnosis. The current case had typical clinical features of BBC, as reported in the literature, including young age (in the first decade), association with a vital mandibular first molar, and buccal swelling [1, 5].
Currently, to the best of our knowledge, there are only 16 manuscripts published in the English-language literature describing 56 cases of BBC. The largest series was reported by Stoneman and Worth [1] in 1983 where 17 cases were described. The bilateral manifestation is even rarer and only fifteen cases have been reported, corresponding to about 26% of all BBC cases (Table 1). The present patient also had bilateral manifestation.
Table 1.
Data of patients with buccal bifurcation cyst (BCC)
| Year | Author | n° of cases | Treatment | Folow-up |
|---|---|---|---|---|
| 1970 | Stanback [15] | 1 bilateral | Marsupialization | 2 years |
| 1979 | Fantasia [16] | 3 | WD | WD |
| 1980 | Swerdloff [17] | 2 (1 bilateral) | Enucleation | 6 months |
| 1983 | Stoneman and Worth [1] | 17 | Enucleation/tooth extraction | 0 |
| 1985 | Trask et al. [18] | 1(1 bilateral) | Enucleation/tooth extraction | 0 |
| 1989 | Vedtolfe and Praetorius [19] | 5 (2 bilateral) | Enucleation | 1–6 years |
| 1989 | Camarda et al. [20] | 2 | Enucleation | 5 years |
| 1990 | Packota et al. [21] | 5 (1bilateral) | Enucleation | 6 months |
| 1992 | Bohay et al. [22] | 2 (1bilateral) | Enucleation | 8 months |
| 1995 | Martinez-Conde et al. [7] | 2 (1bilateral) | Enucleation/tooth extraction | 0 |
| 1998 | David et al. [8] | 3 (3 bilateral) | No procedure/Irrigation with saline and hydrogen peroxide in 1 case | 1–2 years |
| 2003 | Shohat [2] | 5 (2 bilateral) | Enucleation/tooth extraction | 2–3 years |
| 2007 | Gallego [23] | 1 bilateral | Enucleation left side/no procedure right side | 1 year |
| 2009 | Iatrou [24] | 4 | Enucleation/tooth extraction | WD |
| 2010 | Borgonov [25] | 2 | Enucleation | 1 year |
| 2011 | Corona-Rodriguez et al. [26] | 1 bilateral | Enucleation left side/no procedure right side | 6 months |
WD without data
Treatment of BBC includes enucleation of the cyst and maintenance of the involved tooth as possible [4, 27]. However, different approaches have been reported, particularly regarding tooth extraction [1]. Iatrou [24], in his study, reported enucleation plus extraction of the associated tooth in almost all cases, but in the discussion the authors suggested that their patients were referred for orthodontic treatment for space closure. In addition, three other reports described five cases where no surgical intervention was performed. The approach consisted in irrigation of the periodontal pocket and close follow-up, with complete resolution being observed [8, 23, 26]. In the current case, both lesions were enucleated without tooth extraction.
In summary, BBC typically involves the buccal region of the mandibular first molar and usually appears during the first decade of life. The diagnosis is established by correlation of clinical, radiographic, surgical, and histologic findings. Surgical management by enucleation of the cyst without extraction of the involved tooth is the treatment of choice. Therefore, knowledge of the characteristic features is helpful to appropriately diagnose these lesions and better manage the patients.
References
- 1.Stoneman DW, Worth HM. The mandibular infected buccal cyst-molar area. Dent Radiogr Photogr. 1983;56:1–14. [PubMed] [Google Scholar]
- 2.Shohat I, Buchner A, Taicher S. Mandibular buccal bifurcation cyst: enucleation without extraction. Int J Oral Maxillofac Surg. 2003;32:610–613. doi: 10.1054/ijom.2002.0431. [DOI] [PubMed] [Google Scholar]
- 3.Mader C, Wendelburg L. Circumferential dentigerous cyst. Oral Surg Oral Med Oral Pathol. 1979;47:493. doi: 10.1016/0030-4220(79)90139-7. [DOI] [PubMed] [Google Scholar]
- 4.Pompura JR, Sandor GK, Stoneman DW. The buccal bifurcation cyst: a prospective study of treatment outcomes in 44 sites. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:215–221. doi: 10.1016/S1079-2104(97)90008-1. [DOI] [PubMed] [Google Scholar]
- 5.Shear M, Speight PM. Cyst of the oral and maxillofacial regions. 4 th edn. Sheffield: Oxford; 2007.
- 6.Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumors. World Health Organization. 2nd edn. Berlin: Springer; 1992. pp. 40–2.
- 7.Martinez-Conde R, Aguirre JM, Pindborg JJ. Paradental cyst of the second molar: report of a bilateral case. J Oral Maxillofac Surg. 1995;53:1212–1214. doi: 10.1016/0278-2391(95)90638-X. [DOI] [PubMed] [Google Scholar]
- 8.David LA, Sandor GK, Stoneman DW. The buccal bifurcation cyst: in non-surgical treatment an option? J Can Dent Assoc. 1998;64:712–716. [PubMed] [Google Scholar]
- 9.Craig GT. The paradental cyst. A specific inflammatory odontogenic cyst. Br Dent J. 1976;141:9–14. doi: 10.1038/sj.bdj.4803781. [DOI] [PubMed] [Google Scholar]
- 10.Philipsen HP, Reichart PA, Ogawa I, Suei Y, Takata T. The inflammatory paradental cyst: a critical review of 342 cases from a literature survey, including 17 new cases from the author’s files. J Oral Pathol Med. 2004;33:147–155. doi: 10.1111/j.0904-2512.2004.00139.x. [DOI] [PubMed] [Google Scholar]
- 11.Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med. 2006;35:500–507. doi: 10.1111/j.1600-0714.2006.00455.x. [DOI] [PubMed] [Google Scholar]
- 12.Neville B, Damm DD, Allen CM, Bouquot J, editors. Oral and maxillofacial pathology. 3. Philadelphia: WB Saunders; 2009. [Google Scholar]
- 13.Colgan CM, Henry J, Napier SS, Cowan CG. Paradental cysts: a role for food impaction in the pathogenesis? A review of cases from Northern Ireland. Br J Oral Maxillofac Surg. 2002;40:163–168. doi: 10.1054/bjom.2001.0750. [DOI] [PubMed] [Google Scholar]
- 14.Damante JH, Fleury RN. A contribution to the diagnosis of the small dentigerous cyst or the paradental cyst. Pesqui Odontol Bras. 2001;15:238–246. doi: 10.1590/S1517-74912001000300010. [DOI] [PubMed] [Google Scholar]
- 15.Stanback JS., III The management of bilateral cysts of the mandible. Oral Surg Oral Med Oral Pathol. 1970;30:587–591. doi: 10.1016/0030-4220(70)90378-6. [DOI] [PubMed] [Google Scholar]
- 16.Fantasia JE. Lateral periodontal cyst. An analysis of forty-six cases. Oral Surg Oral Med Oral Pathol. 1979;48:237–243. doi: 10.1016/0030-4220(79)90010-0. [DOI] [PubMed] [Google Scholar]
- 17.Swerdloff M, Alexander SA, Ceen RF, Ferguson FS. Bilateral mandibular dentigerous cysts in a seven-year-old child. J Pedod. 1980;5:77–84. [PubMed] [Google Scholar]
- 18.Trask GM, Sheller BL, Morton TH., Jr Mandibular buccal infected cyst in a six-year-old girl: report of case. ASDC J Dent Child. 1985;52:377–379. [PubMed] [Google Scholar]
- 19.Vedtofte P, Praetorius F. The inflammatory paradental cyst. Oral Surg Oral Med Oral Pathol. 1989;68:182–188. doi: 10.1016/0030-4220(89)90190-4. [DOI] [PubMed] [Google Scholar]
- 20.Camarda AJ, Pham J, Forest D. Mandibular infected buccal cyst: report of two cases. J Oral Maxillofac Surg. 1989;47:528–534. doi: 10.1016/0278-2391(89)90292-9. [DOI] [PubMed] [Google Scholar]
- 21.Packota GV, Hall JM, Lanigan DT, Cohen MA. Paradental cysts on mandibular first molars in children: report of five cases. Dentomaxillofac Radiol. 1990;19:126–132. doi: 10.1259/dmfr.19.3.2088785. [DOI] [PubMed] [Google Scholar]
- 22.Bohay RN, Weinberg S, Thorner PS. The paradental cyst of the mandibular permanent first molar: report of a bilateral case. ASDC J Dent Child. 1992;59:361–365. [PubMed] [Google Scholar]
- 23.Gallego L, Baladron J, Junquera L. Bilateral mandibular infected buccal cyst: a new image. J Periodontol. 2007;78:1650–1654. doi: 10.1902/jop.2007.060500. [DOI] [PubMed] [Google Scholar]
- 24.Iatrou I, Theologie-Lygidakis N, Leventis M. Intraosseous cystic lesions of the jaws in children: a retrospective analysis of 47 consecutive cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:485–492. doi: 10.1016/j.tripleo.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Borgonovo AE, Speroni S, Fabbri A, Grossi GB. Paradental cyst of the first molar: a report of two cases. J Indian Soc Pedod Prev Dent. 2010;28:116–120. doi: 10.4103/0970-4388.66753. [DOI] [PubMed] [Google Scholar]
- 26.Corona-Rodriguez J, Torres-Labardini R, Velasco-Tizcareno M, Mora-Rincones O. Bilateral buccal bifurcation cyst: case report and literature review. J Oral Maxillofac Surg. 2011;69:1694–1696. doi: 10.1016/j.joms.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 27.Thompson IO, Waal J, Nortje CJ. Mandibular infected buccal cyst and paradental cyst: the same or separate entities? J Dent Assoc S Afr. 1997;52:503–506. [PubMed] [Google Scholar]


