Abstract
Objective
To study the diagnostic potential of fluorescence spectroscopy and its comparison with different screening methods, including Pap smear and colposcopy, in detecting early cervical neoplasia.
Method
The study was conducted on patients with gynecological complaints. A full gynecological workup of the patients was done along with Pap smear and colposcopy. Cervical biopsy was done in suspected cases and fresh tissue was sent to IIT for spectroscopy.
Result
There is a definite increase in NADH fluorescence (67.4 %) and a decrease in collagen fluorescence (74 %) in dysplastic tissues. When epithelial fluorescence and stromal fluorescence are considered together, diagnostic accuracy is increased to 96.5 %.
Conclusion
The clinical diagnosis of cervical neoplasia by spectroscopic methods is potentially a reliable, fast, and cost-effective alternative to the conventional smear test which needs trained personnel for its interpretation. Research is still continuing to obtain a statistically significant cutoff value from in vitro studies and then use them for in vivo study.
Keywords: Fluorescence spectroscopy, Nicotinamide adenine dinucleotide dehydrogenase (NADH), Cervical cancer
Introduction
Carcinoma cervix is the second most common cancer among women globally. The reported incidence of preclinical invasive carcinoma in India is around 1.5/1,000 [1]. Widespread population screening using Papanicolaou (Pap) smear has had a major role in the reduction of the incidence and mortality of cervical cancer in North America, Western Europe, and elsewhere [2]. Pap smear has become a routine method of cervical cancer screening. Colposcopy is complementary to cytology. In addition to the limited performance of Pap smear for screening and colposcopy for diagnosis, the current clinical strategy is extremely expensive. Over $6 billion is spent annually in the evaluation and treatment of low-grade lesions, suggesting that there is a significant need for new technologies which improve the detection process and reduce cost. Interest in the use of optical technologies to detect premalignant lesions has grown in recent years. Fluorescence spectroscopy is an emerging optical technology that offers particular promise for the diagnosis of the disease.
The aim is to study the diagnostic potential of fluorescence spectroscopy and its comparison with different screening methods, including Pap smear and colposcopy, in detecting early cervical neoplasia.
Materials and Methods
All patients attending the outpatient clinic between Jan 2006 and Nov 2007 with complains of discharge per vaginum, low backache, pain in the abdomen, irregular bleeding and postcoital bleeding were studied. In every patient, pelvic examination and vaginal cytology were done. Patients with abnormal Pap smear, suspicious looking cervix, postcoital bleeding, postmenopausal bleeding, leukoplakia, persistent vaginal discharge, pruritis vulvae, and irregular bleeding were subjected to colposcopy. One hundred and Forty eight patients with suspected colposcopic findings were subjected to colposcopic-directed biopsy. Due to limitations on the number of cases in which fluorescence spectroscopy could be performed, samples of only 46 patients were sent to the Laser spectroscopy lab, IIT, Kanpur, which consisted of tissue from colposcopically normal (taken as control) and abnormal areas of the same dysplastic cervix placed in saline solution for maintaining an ionic equilibrium and kept in an ice box and transported within 2 h of sample collection for fluorescence spectroscopy.
Principle of Fluorescence
The basic principle is to irradiate tissue samples with CW laser and detect the native fluorescence from fluorophores such as proteins, amino acids, and co-enzymes present in the tissues, in vitro and in vivo. The fluorescence spectra provide crucial information on biochemical as well as morphological aspects of the tissue. Any change in the concentrations, quantum efficiency, or binding sites gets reflected in their fluorescence properties, giving rise to a contrast in fluorescence between the normal and the cancerous tissue sites.
Study of Fluorescence in Cervical Tissue
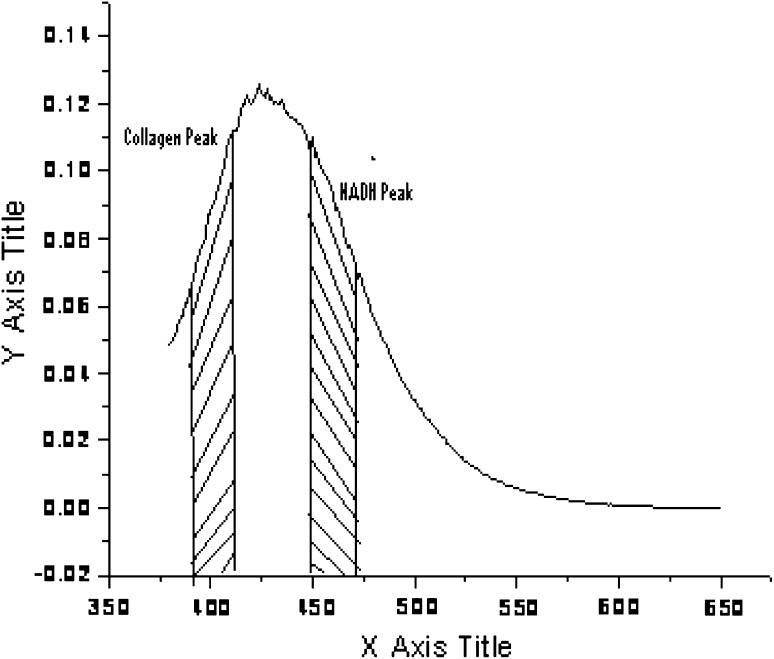
The dominant fluorophores found in the cervical tissue are collagen (peak around 400 nm) and NADH (peak around 460 nm) [3] (Fig. 1). Collagen is a structural protein, the crosslinks of which break when a healthy tissue develops into a cancerous one. NADH is basically the indicator of the metabolic activities inside a cell and hence increases in cancer tissue. NADH is the dominant fluorophore in the epithelial layer, while collagen is the dominant fluorophore in the stromal layer.
Fig. 1.
The collagen and NADH peaks in the emitted spectra and the 20 nm band area
Firstly, the 350 nm wavelength is focused on the cervical tissue (both normal and abnormal tissue) kept in the sample compartment of the fluorimeter, and the corresponding fluorescence spectra are recorded.
Contribution of Collagen in Cervical Tissue Spectra
The collagen peak is around 400 nm and is known to decrease in cancerous tissue. A band of 20 nm (i.e., 400 ± 10 nm) is chosen to incorporate the collagen peaks, and the area under it is calculated for both normal and abnormal tissues. Finally, the ratio of the area under 20 nm band in normal to that in abnormal is calculated.
NADH Contribution in Cervical Tissue
The fluorescence yield of NADH is known to be higher in cancerous tissues. Similarly, the ratio of NADH fluorescence of the epithelial layer in normal to cancerous tissue was taken at 460 ± 10 nm band area.
Results
The sensitivity of cytology was calculated to be 80.45 %, whereas the specificity was determined as 93.44 % (Table 1).
Table 1.
Correlation of cytological findings with histopathologic findings in 148 patients
| Cytological findings | Histologic diagnosis | ||||
|---|---|---|---|---|---|
| Inflammatory | CIN-I | CIN-II | CIN-III | Carcinoma | |
| Normal | 8 | 5 | – | – | – |
| Inflammatory | 49 | 10 | 2 | – | – |
| Dysplasia mild | 4 | 37 | 3 | 1 | – |
| Moderate | – | 4 | 15 | 2 | – |
| Severe | – | – | – | 7 | – |
| Carcinoma | – | – | – | – | 1 |
| Total | 61 | 56 | 20 | 10 | 1 |
Sensitivity = 80.45 %, specificity = 93.44 %, positive predictive value = 94.59 %, negative predictive value = 77.02, false positive = 6.55 %, false negative = 19.54 %
The sensitivity of colposcopy was calculated to be 100 % as no patient of cervical dysplasia was missed. However, the specificity was 86.88 % with no false negatives and 13.11 % false positives (Table 2).
Table 2.
Correlation of colposcopic findings in relation to histopathologic diagnosis (using colposcopic index)
| Colposcopic index | Histologic diagnosis | ||||
|---|---|---|---|---|---|
| Inflammatory (%) | CIN I (%) | CIN-II (%) | CIN-III (%) | Carcinoma (%) | |
| 0 | – | – | – | – | – |
| 1 | 30 | 16 | – | – | – |
| 2 | 23 | 22 | – | – | – |
| 3 | 6 | 10 | 6 | – | – |
| 4 | 2 | 8 | 7 | 3 | – |
| 5 | – | – | 5 | 5 | – |
| 6 | – | – | 2 | 2 | – |
| 7 | – | – | – | – | – |
| 8 | – | – | – | – | 1 |
| Total | 61 | 56 | 20 | 10 | 1 |
Sensitivity = 100 %, specificity = 86.88 %, positive predictive value = 91.57 %, negative predictive value = 100 %, false positive = 13.11 %, false negative = 0
Fluorescence Spectroscopy
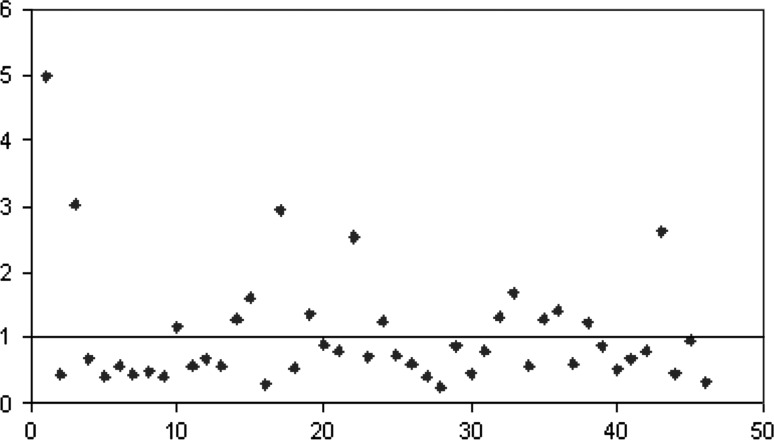
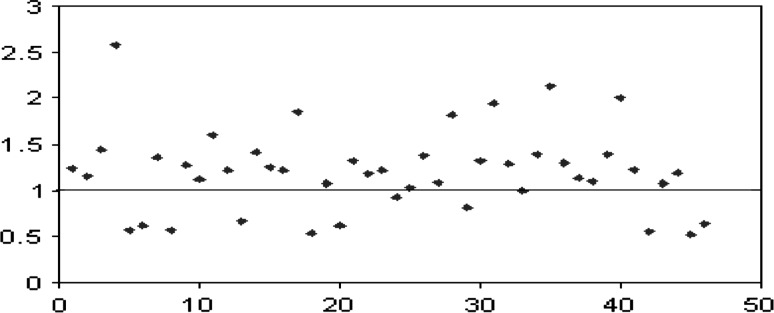
The mean fluorescence intensity of the epithelial layer (NADH) in linear, arbitrary units was 6.4 ± 4.2 for normal tissue and 8.9 ± 18.4 for dysplastic tissue, showing an increase in NADH fluorescence in dysplastic tissue. The statistical significance of this difference could not be established (t = 0.89; p > 0.05), probably due to certain constraints such as a small sample size, confounding factors like age, and due to the fact that tissue from a colposcopically normal area from the dysplastic cervix was taken as the control as tissue from a totally normal cervix cannot be obtained due to ethical considerations. The mean fluorescence intensity of the stromal layer (collagen) in linear, arbitrary units was 107.23 ± 247.55 in normal tissue and 75.08 ± 247.55 in dysplastic tissue, showing an overall decrease in stromal fluorescence, but the difference is not statistically significant (t = 0.62; p > 0.05) for the same reason as cited above. There is a definite increase in NADH fluorescence (67.4 %) (Fig. 2) and a decrease in collagen fluorescence (74 %) (Fig. 3) in dysplastic tissues. When epithelial and stromal fluorescence are considered together, diagnostic accuracy is increased to 96.5 %. Hence, it could be highly effective in the screening of cervical neoplasia (Tables 3, 4).
Fig. 2.
The scatter plot of the ratio of area under 20 nm band around 440 nm (NADH) of normal to cancer for intrinsic fluorescence
Fig. 3.
The scatter plot of the ratio of area under 20 nm band around 400 nm (collagen) of normal to cancer for intrinsic fluorescence
Table 3.
Result of fluorescence spectroscopy in 46 cases
| Fluorescence spectroscopy | No. of cases detected | Percentage |
|---|---|---|
| NADH | 31 | 67.4 |
| Collagen | 34 | 74 |
| Combineda | 44 | 95.6 |
NADH Fluorescence had diagnostic accuracy of 67.4 %, whereas collagen fluorescence had a diagnostic accuracy of 74 %. However, a combined technique can detect 95.6 % of cases
aCombined cases are those which show changes in either NADH or collagen fluorescence or both
Table 4.
Comparison of Pap smear, colposcopy, and fluorescence spectroscopy
| Parameters | PAP smear (%) | Colposcopy (%) | NADH fluorescence (%) | Collagen fluorescence (%) | Combined (%) |
|---|---|---|---|---|---|
| Sensitivity | 80.45 | 100 | 67.4 (accuracy) | 74 (accuracy) | 95.6 (accuracy) |
| False negative | 17.24 | 0 | 32 | 26 | 4.34 |
| False positive | 6.55 | 13.11 | a | a | a |
The table shows that Pap smear is a sensitive technique, but limited by its high false negative results, thus missing many cases. Colposcopy is highly sensitive, but limited by its false positive results, leading to overdiagnosing the cases and causing unnecessary biopsies. Fluorescence spectroscopy has high diagnostic accuracy when the results of NADH and collagen fluorescence are considered together with only 4.34 % false negative. However, false positive could not be calculated due to lack of control
aFalse positive rates could not be calculated in the case of fluorescence spectroscopy as tissue from normal subjects could not be studied
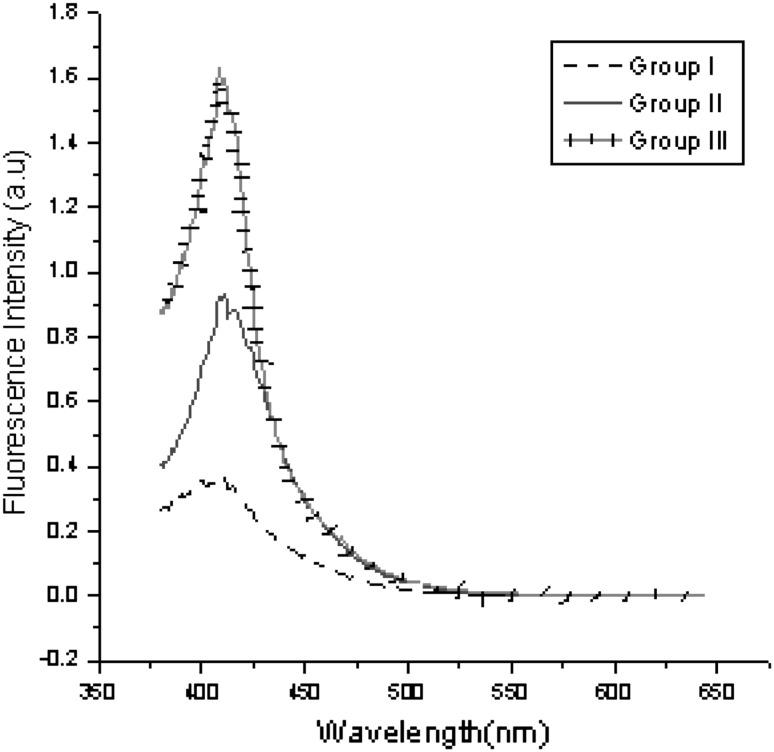
It has been shown that the intensity of native NADH and collagen fluorescence is influenced by the patient’s age and the presence of dysplasia. Age is an important factor having a significant effect on the magnitude of remitted fluorescence and spectra. From the spectra plotted for three different patients in three different age groups, it is clearly seen that the emitted fluorescence is seen to increase with age (Fig. 4). This may be because light may more easily penetrate the stroma of older patients due to the thinner epithelium of older patients and the fact that the amount of collagen increases with age.
Fig. 4.
Fluorescence spectra of three patients in different age groups (Group I—30–39 years, Group II—40–49 years, Group III—≥ 50 years)
Discussion
There are many problems associated with conventional cytology:
Incorrect and inadequate sampling in 5–10 % of cases as only up to 20 % of harvested cells are transferred on the slide [4].
Inter-observer variation in the interpretation of cytological abnormality, making reporting subjective and poorly reproducible.
Epidemiological data suggest that the current method of Pap smear testing is unlikely to prevent more than 60 % of cases of cervical cancer [2].
Colposcopy was developed as an important non-invasive technique for detection of preinvasive cervical lesions, and most importantly to locate the lesion for directed biopsy. However, its main limitations are due to its availability only at referral centers and the need of an expert colposcopist for its interpretation.
Ramanujam et al. [5] differentiated SILs from non-SILs with a sensitivity and specificity of 82 and 68 %, respectively. However, sensitivity and specificity could not be calculated in our study due to lack of a proper control.
The use of fresh tissue sections is of vital importance as oxygenation occurs as the frozen tissue thaws prior to fluoroscopic examination, converting any NADH to NAD+ which is non-fluorescent [6]. In this study, significant epithelial fluorescence was observed in most of the fresh tissue sections and the fluorescence intensity increased at 460 nm excitation in dysplastic samples relative to normal samples from the same patient. NADH is likely to be the source of this epithelial fluorescence as NADH is the dominant epithelial fluorophore at 460 nm excitation. Hence, we can conclude that the significance of the NADH fluorescence decreases if fresh tissue is not analyzed as the concentration of NADH decreases.
The strong influence of the patient’s age on fluorescence spectra cannot be ignored since age may be a confounding factor in analysis of spectra because some changes related to age are similar to changes observed with the presence of dysplasia.
Conclusion
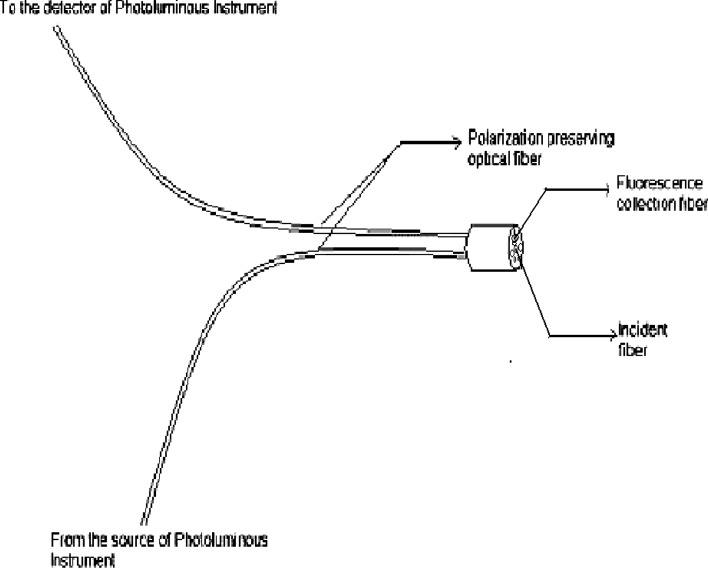
Due to the inherent limitations of Pap smear and colposcopy, the clinical diagnosis of cervical neoplasia by spectroscopic methods seems to be a potentially reliable, fast, and cost-effective alternative to the conventional smear test. However, it is currently limited by significant inter-patient variation in the spectroscopic properties of the cervix. The characterization of suitable in space vitro models of the spectroscopic changes that take place during neoplastic progression may prove to be a significant step toward the successful development of reliable in vivo systems. In this study, we used an in vitro model of cervical tissue to analyze changes in the fluorescence properties of surface squamous epithelium that are associated with the development of neoplastic disease. The main objective of this in vitro work is to implement it for in vivo using an optical fiber probe (Fig. 5).
Fig. 5.
Design of polarization-preserving optical fiber probe
References
- 1.Singh V, Sehgal A, Luthra UK. Screening for cervical cancer by direct inspection. Br Med J. 1992;304:534–535. doi: 10.1136/bmj.304.6826.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sasleni PD. HPV screening and cervical cancer prevention. J Am Med Womens Assoc. 2000;44:538–549. [PubMed] [Google Scholar]
- 3.Brookner CK, Follen M, Boio I, et al. Auto fluorescence patterns in short-term cultures of normal cervical tissue. Photochem Photobiol. 2000;71(6):730–736. doi: 10.1562/0031-8655(2000)071<0730:APISTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Janicek MF, Averette HE. Cervical cancer: prevention, diagnosis and therapeutics. CA Cancer J Clin. 2001;51:92–114. doi: 10.3322/canjclin.51.2.92. [DOI] [PubMed] [Google Scholar]
- 5.Ramanujam N, Mitchell MF, Mahadevan A, et al. Development of a multivariate statistical algorithm to analyse human cervical tissue fluorescence spectra acquired in vivo. Lasers Surg Med. 1996;19:46–62. doi: 10.1002/(SICI)1096-9101(1996)19:1<46::AID-LSM7>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 6.Drezek R, Sokolov K, Utzinger U, et al. Understanding the contributions of NADH and collagen to cervical tissue fluorescence spectra: modeling, measurements, and implications. J Biomed Optics. 2001;6:385–396. doi: 10.1117/1.1413209. [DOI] [PubMed] [Google Scholar]