Abstract
Using structural equation modeling, this study examined the relationship of caregiver network support on caregiver and child mental health need, as well as child mental health service use among 1075 8-year-old children participating in the LONGSCAN study. The final model showed acceptable fit (χ2 = 301.476, df = 136, p<0.001; RMSEA = 0.052; CFI = 0.95). Caregiver and child mental health needs were positively related. As predicted, caregiver network support exerted a protective effect, with greater levels of caregiver network support predictive of lower caregiver and child need. Contrary to prediction, however, caregiver network support was not directly related to child service use. Higher child need was directly related to child service use, especially among children whose caregivers had mental health problems. The findings appear to indicate that lower levels of caregiver network support may exert its impact on child service use indirectly by increasing caregiver and child need, rather than by directly increasing the likelihood of receiving services, especially for African American children.
Keywords: Social network, Maltreatment, Child mental health, Child service use
1. Introduction
Maltreated children (child abuse or neglect) and those at risk for maltreatment are at increased risk for experiencing mental health problems, yet many from this group do not receive treatment (Humphreys, 1995; Staudt, 2003; Stiffman, Chen, Elze, Dore, & Cheng, 1997). While all maltreated youth are not involved in the child welfare system, the most extensive research on formal mental health service use has been done with children in the child welfare system (Burns et al., 2004; Farmer et al., 2001; Horwitz, Hulburt, & Zhang, 2010; Lyons & Rogers, 2004). For example, data from the National Survey of Child and Adolescent Well-Being indicate that only 23% of children with behavioral problems in the clinical range received mental health services (inpatient or outpatient) within 12 months after an initial investigation of maltreatment (Burns et al., 2004). This is particularly concerning given some evidence that as many as one in three families who access community mental health clinics have a history of physical abuse (Walrath, Nickerson, Crowel, & Leaf, 1998).
Extant studies of maltreated youth who are involved in the child welfare system suggest that mental health service use for this population is likely associated with a confluence of factors including increased age, race (African Americans less likely), type of abuse (physical), residing in a group home setting, and higher threshold of mental health service need (Burns et al., 2004; Horwitz et al., 2010). Despite these findings, there has been remarkably little research on the underlying family-level factors or mechanisms leading to mental health service use for maltreated youth. This information might help to explain barriers associated with service access and point to discernible ways to improve mental health service use, especially among African American youth who by several accounts have the lowest rates of mental health service use.
Family-level factors such as caregiver mental health and social network support have been found to play a critical role in service access among all youth (Brannan, Heflinger, & Foster, 2003; Flisher et al., 1997; Harrison, McKay, & Bannon, 2004). However, with a few exceptions (Ezzell, Swenson, & Faldowski, 1999; Kolko, Seleyo, & Brown, 1999; Martinez & Lau, 2011), limited studies have included the role of caregiver factors in predicting child mental health service use among maltreated or child welfare involved children. Indeed, the family environment of maltreated children is likely to be characterized by disorganization and stressful family interactions (Ellis, Zucker, & Fitzgerald, 1997; Farmer et al., 2001; Flisher et al., 1997; Thompson et al., 2007). There is evidence that families of maltreated children may access support networks to offset the challenges presented with caretaking of a child with mental health needs, particularly when caregivers struggle with their own psychopathology (Lindsey et al., 2008). The extent of support networks and the influence of these networks on caregiver and child mental health need and child service use remain understudied among maltreated children. Once understood, however, these perspectives may provide important insights to improve service use, and potentially outcomes related to service use. Indeed, research has found that children in the CW system use a substantial proportion of expenditures for mental health services (Berkowitz, 1992) and, yet, may be experiencing little benefit from these services (McCray, Barth, & Guo, 2010). The purpose of this study is to examine the relationship between social network support, caregiver mental health problems, child need for mental health services, and child mental health service use among a national sample of maltreated youth or those at-risk for maltreatment.
1.1. Caregiver mental health in relation to child mental health and child service use
There is clear evidence that caregiver mental health problems predict child mental health need (Horwitz, Gary, Briggs-Gowan, & Carter, 2003). This is also true of children whose parents have diagnosable mental health disorders, such as depression or serious mental illness (Beardslee, Versage, & Gladstone, 1998; Ford, Collishaw, Meltzer, & Goodman, 2007; Ohannessian et al., 2004). For example, parent depression is associated with increased risk for child mental health problems, in general (Beardslee et al., 1998; Hammen & Brennan, 2003; Kim et al., 2003), and with a fourfold increase in the risk of affective disorder, specifically (Lavoie & Hodgins, 1994). Parental depression also predicts other child mental health needs including delinquent behavior, substance use, and school and interpersonal problems (Davies & Windle, 1997; Lewinsohn, Olino, & Klein, 2005). Although other parent mental health issues (e.g. anxiety or substance abuse disorders) are less frequently studied, extant evidence indicates that these disorders also predict child mental health need (Ellis et al., 1997; Hammen, Brennan, & Shih, 2004; Lindsey et al., 2008).
The relationship between parent mental health problems and children’s mental health service use is, however, far less clear. Some research has found that parent mental health problems increase the likelihood of children receiving mental health services (Farmer, Stangl, Burns, Costello, & Angold, 1999). This may be especially true of parents who, themselves, have received mental health services (Wu et al., 2001). Other research has found, however, that caregiver mental health problems increase the risk that children’s mental health needs will go unmet (Flisher et al., 1997). In particular, parental depression may inhibit help-seeking for children with needs (Barlow, Wildman, & Stancin, 2005; Burns et al., 2010). Parent mental health needs are likely to increase child mental health needs more than they increase the likelihood of service receipt. Yet, some elevation in receipt of children’s mental health services may occur if maternal mental health problems trigger services for her and these, in turn, result in referrals for her child. Thus, the available evidence offers no strong prediction about whether children of parents with mental health problems will have more unmet mental health service needs. This is likely to be true whether a child has been involved with child welfare services or not.
1.2. Caregiver network support regarding child mental health and service use
Although a variously defined construct in the literature, social network support generally indicates an individual’s perception of the amount of practical and emotional support received; the size and density of networks; and the level of connection to supportive resources (Bussing et al., 2003; Martinez & Lau, 2011; Pescosolido, 1992). Indeed, social network support (herein defined as practical/emotional support and connection to supportive resources) experienced by the caregiver may be an important factor in a child’s mental health need. The evidence for this link is, however, limited and mixed. Caregiver network support protects youth from negative mental health outcomes (Bussing et al., 2003; Ghuman, Weist, & Shafer, 1999), with caregiver network support associated with a range of positive child outcomes, including but not limited to mental health (Hoagwood, 2005). Among children involved in the child welfare services, Coohey (2007) reports that more limited social network support is related to inadequate supervision by mothers. More broadly, positive neighborhood attributes appear to be protective, especially for at-risk children (Runyan et al., 1998). Of course, social networks may not always exert a positive influence on child outcomes. O’Brien-Caughy et al. (Caughy, O’Campo, & Muntaner, 2003) found, for example, that in impoverished neighborhoods the size of parents’ social networks predicts more child behavioral problems. Lindsey et al. (2008) also found among a sample of African Americans that caregiver network support related to higher parent reports of child mental health needs, although the increased network support may actually help caregivers better identify their child’s mental health needs rather than actually increase those needs.
The findings regarding the effects of caregiver network support on child mental health service use are also mixed. Caregiver network support may facilitate service use (Harrison et al., 2004), although the relationship is not consistently shown (Brannan et al., 2003), and other research suggests that caregiver network support may actually reduce the likelihood of children receiving mental health services, particularly among African American children and families (Bussing et al., 2003). Bussing et al. (2003) note at least one possible reason for their counter-intuitive finding; namely, that caregiver network support may reduce the burden that a child’s behavioral problems pose for a parent, thus reducing their felt need to seek services for the child. Thompson argues that caregiver network support reduces service use in cases of mild to moderate child problems, but facilitates service use in the case of severe problems (Thompson et al., 2007). Finally, the nature of social involvement and support may be an important determinant of its impact on service use. For example, knowing someone else who sought services increases the likelihood of seeking services (Vogel, Wade, Wester, Larson, & Hackler, 2007). In contrast, in some marginalized communities, network members may promote a set of norms around service use that fosters suspiciousness and fear of exploitation (Snowden, 2005). Greater social involvement may also make treatment seeking more embarrassing for parents (dosReis, Mychailyszyn, Myers, & Riley, 2007), although there is some evidence that the impact of stigma on service use may be overstated (Nadeem et al., 2007).
1.3. Child mental health service use models
In recent years, several emergent models in the mental health services research literature help explain the influence of family environment and social network support on child mental health service use (Cauce et al., 2002; Costello, Pescosolido, Angold, & Burns, 1998; Finkelhor, Wolak, & Berliner, 2001; Logan & King, 2001; Stiffman, Pescosolido, & Cabassa, 2004). A consistent theme among the child-focused models of mental health service use is the role that parents and caregivers play in problem identification and service use. The most notable of the child mental service use models is the Costello et al. (1998) model, which extends the Network-Episode Model (Pescosolido, 1992; NEM) by focusing more prominently on the social network influences of caregivers given children rarely, if ever, refer themselves to treatment. Like the NEM for adults, the Costello model views service use as a social, not individual process. According to the model, child mental health service use may occur as a result of the following sequence of actions among the caregiver and her/his social network: (1) child expresses behavioral problems or mental health symptoms that is causing some impairment in functioning; (2) caregiver(s) and members of the caregiver’s social support network help to identify the child’s mental health symptoms or behavioral problems; (3) network members offer help regarding what should be done to relieve the symptoms; and (4) network members assist the caregiver by facilitating or delaying the child’s mental health service use (Costello et al., 1998). Rarely do caregivers act alone in recognizing symptoms and getting help for the affected child. The help offered by network members, however, may “push” families to services or serve as a prohibitive factor, even among children involved in the child welfare system (Martinez & Lau, 2011).
1.4. Focus of the current study
Staudt (2003) acknowledged a need for more conceptualization and confirmation of the processes underlying how maltreated children and their families access and use mental health services. Such knowledge has the potential to guide interventions to improve access to services by identifying barriers and prohibitive factors that such interventions should address. Importantly, existing models of mental health service use (Costello et al., 1998; Pescosolido, 1992) may apply to the maltreated children, but there has been limited investigation of the applicability of these models to this population. The social networks of children who have substantiated cases of maltreatment may have a different influence on mental health service use than that of the social networks of children who are at risk for maltreatment, but have not had substantiated maltreatment. Consistent with prior recommendations by Staudt (2003), the current study begins to explicate the role of caregiver network support on child service use among a sample of children with documented cases of maltreatment or who may be at-risk for maltreatment.
Using multiple group structural equation modeling, we first examined whether the latent constructs for caregiver network support, caregiver mental health problems, child need for mental health services and child mental health service use would differ by maltreatment status (maltreated versus at-risk for maltreatment). We offered no differential hypotheses in subsequent analyses given the limited literature examining differences between maltreated and at-risk children in this regard. Next, based on structural equation modeling, we examined the relationship between caregiver network support, caregiver mental health problems and child need for mental health services. Higher perceived caregiver network support was hypothesized to be associated with lower caregiver mental health problems and child need for mental health services. Third, we examined the relationship between caregiver mental health problems and child need for mental health services. Higher caregiver mental health problems were hypothesized to be associated with increased child need for mental health services. Fourth, we examined the relationship between caregiver network support and child mental health service use. Given the mixed evidence regarding the role of caregiver network support (Bussing et al., 2003; Harrison et al., 2004) on child mental health service use, we did not indicate any directional hypotheses. We expected to find a significant association between the two constructs, however. Fifth, we explored gender and racial influences on the associations between caregiver network support, caregiver and child mental health needs and child service use. Finally, we explored indirect relationships among the study constructs and demographic factors. In particular, we sought to determine the association between caregiver network support and child mental health service utilization after accounting for caregiver mental health problems and child need for mental health services, and the association between caregiver mental health problems and child mental health service utilization through child need for mental health services.
2. Methods
2.1. Sample
Data for this study come from children and their caregivers participating in the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN). As a research consortium, LONGSCAN includes a coordinating center at the University of North Carolina at Chapel Hill and five independent, prospective longitudinal investigations located in different regions of the United States. Each site shares common measures and protocols for data collection, management, and entry. Sites differ systematically by sampling children who are at risk of maltreatment (southern and eastern sites), have been reported for maltreatment (northwestern site), or have been identified as maltreated and involved in remedial intervention by social service or other treatment agencies (Midwestern and Southwestern sites) (Runyan et al., 1998). Risk of maltreatment was defined in a variety of ways, varying by site, including demographic risk factors, such as extreme poverty and very young maternal age at birth, and clinical factors, such as children treated in Failure to Thrive clinics or caregivers receiving substance abuse treatment. Children were defined as maltreated if there had been a report to Child Protective Services (CPS) regarding the child as a victim of maltreatment. Assessments of children, their caregivers, and their teachers occur periodically. Analyses herein focus on assessments conducted when children were 8 years old (which was the latest wave of data available at this study’s inception).
The sample analyzed here was restricted to all LONGSCAN children who were African American or Caucasian, had completed age 8 interviews, and had a review of their Child Protective Services maltreatment record through the date of their age 8 interview. This analysis sub-sample includes data gathered from 1075 children and their primary caregivers who participated at baseline. Due to attrition, however, our final sample size at age eight was 902 African American and Caucasian children, representing an attrition rate of 16%. Our rationale for excluding our analyses to African American and Caucasian children only is based on prior studies that consistently show the lower use of mental health services among African American children who are maltreated or in the child welfare system relative to their Caucasian counterparts (Burns et al., 2004; Horwitz et al., 2010; Staudt, 2003).
Fifty-nine percent of the sample had a substantiated case of maltreatment based on CPS report. Females represented a majority (52%) of the children in the sample. The majority of the caregivers in the sample reported their child’s ethnicity as African American (67%). The most common marital status of caregivers was single (43%), and, on average, caregivers had less than a 12th grade education. On average, African American children had close to 10 network members (including family members, friends, neighbors) relative to an average of 8 network members for Caucasians (t = −6.480, p <0.000). For all children and caregivers in the study, it appears that most of their support system consisted of family members given the average family size was seven (SD = 4.17).
2.2. Procedure
Local Institutional Review Boards approved all study site protocols. At each assessment, the child’s primary caregiver completed a two-hour face-to-face interview consisting of mostly standardized measures. At age four, children received brief developmental testing. At ages six and eight, separate face-to-face interviews were conducted with the caregiver and the child by trained project staff.
2.3. Measures
2.3.1. Child mental health need
The Child Behavior Checklist (CBCL) was used to assess child behavior problems at age eight. The parent-report CBCL (Achenbach, 1991) is a widely used, empirically based measure of children’s competencies and behavior problems. The validity and reliability of the 113-item Problem Checklist are well established (Achenbach, 1991). For each item, the child’s primary caregiver is asked to report on the frequency of that behavior “now or within the past six months.” The Internalizing (that is, social withdrawal, somatic complaints, and anxiety/depression) and Externalizing (that is, delinquent behavior, aggression) Problems subscales derived from the CBCL were used in these analyses. Higher scores indicate more behavior problems. T scores of 61 to 63 are considered borderline clinical, and scores above 63 are in the clinical range (Hunter et al., 2003). The Cronbach’s alpha coefficient for the current sample was 0.81.
2.3.2. Caregiver mental health need
The Brief Symptom Inventory (Derogatis, 1993) was administered to the caregiver at the child’s age 8 interview to identify self-reported psychological symptoms. The BSI consists of 53 items covering nine symptom dimensions: Somatization, Obsessive–Compulsive, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism; and three global indices of distress: Global Severity Index (BSI), Positive Symptom Distress Index (PSDI), and Positive Symptom Total (Hunter et al., 2003). For analyses in this study, we used the depression, anxiety, and obsessive–compulsive subscales as indicators of caregivers’ mood-related problems and a fourth sub-scale assessing caregivers’ levels of psychotic symptoms. Each subscale is sensitive to caregivers’ distress levels and the number of symptoms they experience in each domain. Additionally, caregiver mood-related problems and other more serious mental health outcomes are highly related to child mental health outcomes (Beardslee et al., 1998; Ford et al., 2007; Ohannessian et al., 2004). Higher scores indicate high symptom expression among respondents. The Cronbach’s alpha coefficients among the four subscales ranged from 0.71 (psychoticism) to 0.85 (depression) (Hunter et al., 2003).
2.3.3. Caregiver network support
The Neighborhood Short Form (Hunter et al., 2003) was administered at the child’s age eight interviews to assess the primary caregiver’s perceptions of neighborhood quality. The measure includes nine items including the following: “People in my community help each other out” and “There are a lot of drugs in this neighborhood” (Hunter et al., 2003). The form is a shortened version of a neighborhood scale developed by Martinez (2000). Respondents rank each item on a four-point Likert-type scale ranging from 1 = very much like my neighborhood to 4 = not at all like my neighborhood. The three subscales among the nine items are Safety, Support, and Pride/Morale, and satisfaction scores are produced by summing across all nine items, with higher scores indicating higher levels of satisfaction among the domains of query (Hunter et al., 2003). The Cronbach’s alpha coefficient for the current sample was 0.87.
The Social Provisions Scale (Cutrona & Russell, 1987) was administered to caregivers at the age eight interviews to examine the degree to which respondent’s social relationships provide various dimensions of social support. The 24-item measure contains four items in each of the following domains: Attachment, Social Integration, Reassurance of Worth, Reliable Alliance, Guidance, and Opportunity for Nurturance. Respondents indicate on a four-point Likert-type scale (1 = strongly disagree to 4 = strongly agree) the extent to which each statement describes her or his current social network. Total scores are calculated as the mean value of the 24 items (Hunter et al., 2003). The Cronbach’s alpha coefficient for the current sample was 0.93.
Practical support was assessed at the age eight interviews. This 10-item measure was derived for the current study based on items in the Maternal Social Support Index (Pascoe, Ialongo, Horn, Reinhart, & Perradatto, 1988; MSSI). Items assess the extent to which the caregiver perceived members of their network as providing assistance for personal matters, including fixing meals, grocery shopping, and assistance with paying bills, among other items. Higher scores indicated a greater amount of perceived practical support. The Cronbach’s alpha coefficient for the current sample was 0.80.
Participation in supportive activities was assessed at the age eight interviews. This 5-item measure was also derived for the current study based on items in the MSSI. Items assessed the amount of supportive activities caregivers participated in, including attendance at religious services, educational meetings, social meetings, political meetings, and other supportive meetings. Higher scores indicated a greater amount of participation in activities perceived by caregivers to be supportive. That the Cronbach’s alpha coefficient for the current sample was 0.46 suggests the character of the MSSI is more of an inventory than a measure of a single latent construct, reflecting the reality that participation in one kind of social activity may or may not be associated with participation in other types, though a general tendency of a modest degree for people to socialize or not is reflected by the alpha statistic observed. In any event, (Drewes, 2009) notes that low alphas do not necessarily mean lack of scalability.
2.3.4. Child mental health service utilization
A measure created by LONGSCAN PIs was administered at the age eight interviews to assess child mental health care utilization (Hunter et al., 2003). Caregivers were asked whether in the past year their child had received “any type of counseling for their child, outside of school, for a psychological or behavioral problem.” If they responded yes, children received a score of 1 and, if not, a score of 0 (Hunter et al., 2003).
2.4. Statistical analyses
After preliminary analyses (frequencies and contingency tables), the main path models in the present study were tested via Mplus 6.0. Mplus, a structural equation modeling (SEM) program, combines the advantages of factor analysis and multiple regression. The main advantage of SEM over multiple regression is that SEM can model and reduce the biasing effects of measurement error (Klem, 2000). SEM programs such as Mplus 6.0 also allow exceptionally easy, and statistically sound, handling of missing data. All missing data were handled using the full information maximum likelihood (FIML) capabilities of Mplus 6.0 This approach has been shown repeatedly to yield good parameter estimates and reasonable standard errors in the missing data case (Graham, Cumsille, & ElekFisk, 2003; Schafer & Graham, 2002). Missingness in the final SEM model was approximately 21%. The estimates of indirect effects were based on coefficient product testing as provided in Mplus, and interpreted following recommendations outlined by MacKinnon, Lockwood, Hoffman, West, and Sheets (2002).
3. Results
3.1. Descriptive statistics
Means and frequencies for demographic and study variables are summarized in Table 1. In terms of child mental health need, 21% of the sample reported internalizing needs at the borderline or clinical range on the CBCL, while 30% reported externalizing needs in that same range on the CBCL. Overall, 33% of the children in the sample received mental health services.
Table 1.
Description of the sample (N = 1075).
| Main continuous variables | Mean (SD) or proportion |
|---|---|
| Caregiver network support | |
| Neighborhood Short Form | 27.36 (6.65) |
| Social Provisions Scale | 68.20 (9.12) |
| MSSI: Amount of practical support received | 4.46 (2.91) |
| MSSI: Participation in supportive activities | 1.58 (0.985) |
| Caregiver mental health problems | |
| BSAT – Depression | 49.42 (8.89) |
| BSAT – Anxiety | 46.81 (9.82) |
| BSAT – Obsessive Compulsive | 48.92 (10.63) |
| BSAT – Psychoticism | 52.38 (8.94) |
| Child need for mental health services | |
| CBCL internalizing | 51.47 (10.64) |
| 59 or less (normal) | 79% |
| 60+ (borderline+clinical) | 21% |
| CBCL externalizing | 53.94 (11.16) |
| 59 or less (normal) | 70% |
| 60+ (borderline+clinical) | 30% |
| Child mental health service utilization | 33.1% |
Notes: Maternal Social Support Index (MSSI); Brief Symptom Inventory (BSAT); Child Behavior Checklist (CBCL).
Table 2 indicates the correlations among study variables included in the SEM analyses. Caregiver support significantly correlated with each indicator of caregiver mental health need, albeit in a negative direction. The magnitude of these relationships, however, was small. The BSI subscales were moderately to highly correlated with each other. The caregiver social network variables significantly correlated with each other, except for caregiver support and caregiver practical support (r = 0.074, p>0.05) and caregiver practical support and caregiver participation in supportive activities (r = 0.018, p>0.05). Finally, CBCL internalizing and externalizing subscales moderately correlated (r = 0.647, p<0.05).
Table 2.
Correlation matrix among variables in the SEM models (N = 902).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Caregiver support | - | ||||||||
| 2. Neighborhood satisfaction | 0.290** | - | |||||||
| 3. MSSI – Practical support | 0.074 | 0.268** | - | ||||||
| 4. MSSI – Participation in supportive activities | 0.245** | 0.163* | 0.018 | - | |||||
| 5. BSAT – Depression | −0.142** | −0.165** | −0.108 | 0.039 | - | ||||
| 6. BSAT – Anxiety | −0.067* | −0.134** | −0.102 | 0.056 | 0.674** | - | |||
| 7. BSAT – Obsessive Compulsive | −0.066* | −0.134** | −0.097 | 0.044 | 0.656** | 0.683** | - | ||
| 8. BSAT – Psychoticism | −0.198** | −0.176** | −0.162* | −0.030 | 0.745** | 0.610** | 0.638** | - | |
| 9. CBCL – Internalizing | 0.037 | −0.127** | 0.069 | 0.119 | 0.396** | 0.435** | 0.489** | 0.390** | - |
| 10. CBCL – Externalizing | 0.044 | −0.143** | 0.049 | 0.038 | 0.279** | 0.329** | 0.383** | 0.315** | 0.647** |
Notes: Maternal Social Support Index (MSSI); Brief Symptom Inventory (BSAT); Child Behavior Checklist (CBCL).
p<0.05.
p<0.01.
3.2. Latent constructs
The latent construct Caregiver Network Support was composed of the Neighborhood Short Form, the Social Provisions Scale, and items from the Maternal Social Support Index, which indicated caregiver’s perceptions of practical support and their participation in supportive activities. Fig. 1 shows the factor loadings for these items in the final model. Each loading was significant at p<.001. Caregiver Mental Health Problems was composed of the depression, obsessive compulsive, anxiety, and psychoticism subscales of the Brief Symptom Inventory. The factor loadings were significant at the p<0.001 level for all components. Child Need for Mental Health Services was indicated by the CBCL internalizing and externalizing subscales and the factor loading for the externalizing subscale was significant at p<0.001.
Fig. 1.
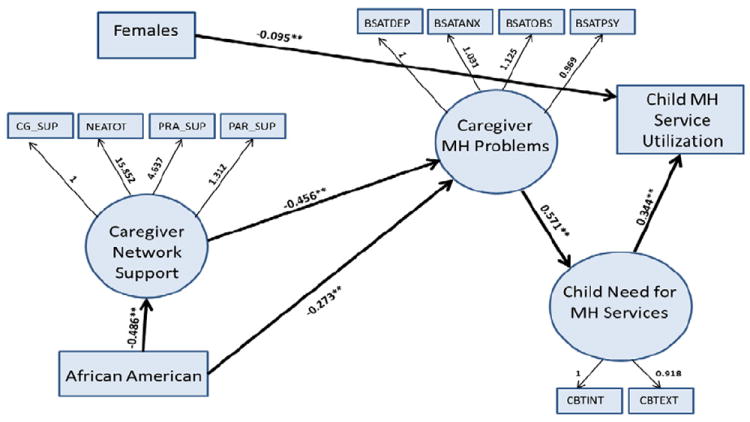
Final model.
Notes:
Mental Health (MH)
#Correlations were controlled for in the cases where regression coefficients were not estimated
ˆPath relationships are depicted by standardized estimates
*Significant paths of any degree are indicated in asterisks (**).
3.3. Path model results
3.3.1. Variance of models for maltreated children versus children at-risk for maltreatment
The present study conducted multiple group analysis of the proposed model of the associations between caregiver social support, caregiver mental health problems, child need for mental health service, and child service utilization. However, before testing these differences, it was important to verify first that the factor structures for this set of variables was equivalent between maltreated and children at-risk for maltreatment. Following Jreskog (1996) recommendations for testing the equivalence of factor structures in multiple groups, we were able to show that the factor structures for maltreated and being at-risk for maltreatment were invariant in terms of the basic pattern of the factor structure and, more importantly, in terms of the actual factor loadings. In the latter case, the model in which all factor loadings were constrained to be equal for maltreated and being at-risk for maltreatment fit no worse than a model in which factor loadings were allowed to be estimated freely in each group (χ2 difference = 8.115, df = 7, ns). Other measures of goodness of fit were not utilized since chi-square was not significant. Chi-square is known to be sensitive to small changes in model fit for large sample sizes; however, this sensitivity causes chi-square to be statistically significant, but does not cause an erroneous non-significant chi-square. As these factor loadings were not significantly different between groups, we were justified in constraining them to be equal (same meaning of all factors for maltreated and being at-risk for maltreatment), and in testing whether the b-weights of our path model were the same or different across groups. The next models assessed whether the b-weights were equal between the groups. Similarly, there was no statistically significant change in model fit due to constraining the b-weights to be equal between maltreated and non-maltreated youth (χ2 difference = 15.719, df = 12, ns).
3.3.2. Relationship of caregiver network support on caregiver and child mental health problems/need and child mental health service utilization
Table 3 presents the unstandardized (with confidence intervals) and standardized beta weights of the path model were tested via SEM analyses relevant to study hypotheses 1–2 and the exploratory aims. The significant paths and coefficients are indicated in Table 3 and highlighted in Fig. 1. An assessment of this model yielded acceptable model fit (χ2 = 301.476, df = 136, p <0.001; RMSEA = 0.052; CFI = 0.95). The model indicated that caregiver network support was associated with less mental health problems in caregivers. Caregiver mental health problems were associated with increased child need for mental health services. Increased child need for mental health services was associated with higher mental health service use by the child. Caregiver network support, however, was not directly associated with child mental health need or child service utilization as hypothesized. In terms of demographic factors, being a caregiver of an African American child was associated with lower perceived network support and caregivers’ lower mental health problems. Child race was not significantly associated with child need for mental health service or child service use. Being a female child was associated with lower receipt of mental health services, but child gender was not associated with child need for mental health services.
Table 3.
Unstandardized and standardized values for the structural model (N = 902).
| Parameter estimate | Unstd. coeff. [95% CI] | Std. coeff. |
|---|---|---|
| Race on caregiver network support | −0.234 [0.179, 0.288] | −0.486 |
| Race on caregiver mental health need | −4.710 [2.93, 6.49] | −0.273 |
| Race on child mental health need | −1.859 [−3.81, 0.087] | −0.089 |
| Race on child service utilization | −0.077 [−0.173, 0.019] | −0.075 |
| Gender on child mental health need | −0.447 [−1.59, 0.7] | −0.026 |
| Gender on child service utilization | −0.081 [0.024, 0.138] | −0.095 |
| Caregiver network support on caregiver mental health need | −16.352 [10.15, 22.56] | −0.456 |
| Caregiver network support on child mental health need | 1.764 [−4.31, 7.83] | 0.041 |
| Caregiver network support on child service utilization | 0.215 [−0.083, 0.51] | 0.10 |
| Caregiver mental health need on child mental health need | 0.693 [0.58, 0.81] | 0.571 |
| Caregiver mental health need on child service utilization | −0.002 [−0.0079, 0.004] | −0.039 |
| Child mental health need on child service utilization | 0.017 [0.011, 0.023] | 0.344 |
3.3.3. Indirect associations among latent constructs with child mental health service utilization
There were also several significant indirect effects of interest in the model. Lower caregiver network support was indirectly associated with increased child mental health service utilization through caregiver mental health problems and child need for mental health services(b = −0.192, 95% CI = 0.096–0.288, β = −0.0.89, p<0.001). Further, higher caregiver mental health problems were indirectly associated with increased child service utilization through its association with increased child need for mental health services (b = 0.012, CI = 0.00432–0.01968, β = 0.196, p<0.001). Race was significantly indirectly associated with caregiver mental health problems through its association with caregiver social support (b = 3.820, CI = 2.29–5.35, β = 0.222, p<0.001). This effect indicates that, overall, African American caregivers report less network support, which is associated with increases in their mental health problems.
4. Discussion
This study examined caregiver factors (network support and mental health problems) in relation to child need for mental health services and child service use among maltreated children and children at-risk for maltreatment. We first sought to verify that the factor structures for this set of variables were equivalent between maltreated children and children at-risk for maltreatment. Our multiple group analyses indicated that the factor structures were invariant. This suggested that two separate models comparing maltreated children versus children at-risk for maltreatment on factors that influenced the child’s service use for mental health problems were not distinguishable, statistically. Conceptually, this finding indicates that regardless of maltreatment status caregiver mental health is associated with child mental health need and service utilization. This finding is consistent with previous research that shows caregiver mental health status is associated with child outcomes (Beardslee et al., 1998; Hammen & Brennan, 2003; Kim et al., 2003; Lindsey et al., 2008). Given this finding, we proceeded to examine the relationships among latent constructs for caregiver network support, caregiver mental health problems, child need for mental health services on child mental health service utilization. We also explored indirect relationships between caregiver network support on child service use, after accounting for caregiver and child mental health needs, and the association between caregiver mental health problems and child mental health service utilization through child need for mental health services.
We found partial support for both of our hypothesized effects. First, lower caregiver network support was associated with increases in both caregiver mental health problems and child need for mental health services, but only the relationship between caregiver network support and caregiver mental health problems was significant. Second, higher levels of caregiver mental health problems were associated with increased child need for mental health services. These findings are consistent with prior research studies indicating that lower levels of familial support may characterize the social environment of maltreated youth, and affect the mental health outcomes of both caregivers and their children (Ellis et al., 1997; Farmer et al., 2001; Flisher et al., 1997; Thompson et al., 2007). Additionally, the strong effects between caregiver mental health problems and child need for mental health services could be due, in part, to genetic factors (Goodman & Gotlib, 1999; Lavoie & Hodgins, 1994).
We did not find a direct relationship between caregiver network support and child mental health service use as we initially believed would be the case. We did find, however, that lower caregiver network support was indirectly associated with increased child mental health service use through related increases in caregiver mental health problems and child need for mental health services. Closer examination of the association between caregiver network support and caregiver mental health problems may clarify these findings. That is, given their negative relationship (decreases in caregivers’ support associated with more mental health problems for caregivers), it appears that mental health need factors (caregiver and child) are associated with increased child mental health service use by virtue of the limited support received by caregivers. We also observed a significant indirect relationship of caregiver mental health problems on child mental health service utilization through child need for mental health services. Thus, consistent with previous data by Farmer et al. (1999), our results indicate caregiver mental health problems increase the likelihood that children will receive services. Our findings add to this literature, particularly the Costello model, however, by showing that the association between low caregiver network support and increased caregiver mental health problems may be the precipitant to child need for mental health services and actual service use. Strategies to increase child mental health service use may need to account for caregiver network support and caregiver mental health problems in the context of child mental health needs.
Interestingly, while African American caregivers in our sample reported lower levels of mental health problems, they also had lower levels of network support than Caucasian caregivers did. Considering the strong association between caregiver network support and caregiver mental health problems, however, we found that lower levels of caregiver network support were associated with increased caregiver mental health problems for African American caregivers. Our findings suggest that the families and children most vulnerable to poor mental health outcomes may be African Americans who experience limited support from their network. This is particularly concerning given the overwhelming evidence indicating that African American children with mental health needs in the child welfare system have the lowest rates of formal mental health service use (Horwitz et al., 2010; Staudt, 2003). However, Bussing et al. (2003) found that higher levels of instrumental support experienced by African American caregivers were associated with lower child mental health service utilization rates. Future research is necessary to resolve whether social networks of African American caregivers prohibit service use by virtue of the support they provide to caregivers of children with mental health needs, or whether the lack of supportive networks increases the chance that African American families might receive services.
Finally, our finding regarding the lower use of mental health services among females is consistent with those of Farmer et al. (2010) who also examined mental health service use patterns among maltreated youth. Gender differences in service use is often reflected in type of mental health problem exhibited, and previous research (c.f. Thompson & May, 2006) has demonstrated that boys exhibiting behavioral problems were most likely to receive mental health services. Farmer et al. (2010) also examined child mental health service use by sector, and found that boys were more likely to receive mental health services via the juvenile justice and the general medical setting. While our data does not differentiate service use by sector, future research might examine the associations between gender and child mental health service use to discern factors that differentially effect service use for boys versus girls.
4.1. Limitations
Our findings must be considered in light of several limitations. First, CBCL internalizing and externalizing subscales indicated our latent construct for child mental health need, and the CBCL is not a diagnostic measure of mental health. Thus, we were only able to determine problem behaviors that warrant concern. Additionally, our report of child mental health need relied upon the caregiver’s report of internalizing and externalizing child behavioral problems. Previous literature found that caregivers who are dealing with their own mental and physical health concerns report higher problem behavior scores on the CBCL (Lau, Valeri, McCarty, & Weisz, 2006). Thus, some caregivers in our sample might have overestimated their child’s problems. Among the adult measures of mental health need, the BSI subscales confirm only symptoms of mental health problems and not diagnostic indications of caregivers’ mental health need (Derogatis, 1993).
Second, because this is a secondary data analysis of cross-sectional data, causality cannot be determined. In fact, it may be the case that child behavioral problems lead to elevated caregiver mental health needs at which point networks are activated. The true relationship between caregiver and child mental health need might have best been understood in a longitudinal analysis; however, SEM offers some similarities to a longitudinal advantage insofar as it provides an opportunity to look at paths and associations among study variables, both directly and indirectly. Given this relatively understudied area, our findings build on previous caregiver social network and child mental health services literature by examining multiple indicators of caregiver network support and caregiver mental health factors that affect child outcomes for maltreated children (Bussing et al., 2003; Martinez & Lau, 2011).
Third, we did not assess the extent of out-of-home services in which children and families in the study may have been involved. If maltreated children in our sample were involved with out-of-home child welfare services, the “onset hypothesis” may explain their mental health service use. This hypothesis suggests that entry into the child welfare system may be associated with increase child mental health service use (Landsverk, Hurlburt, Leslie, Rolls, & Zhang, 2010). Landsverk et al. further note the greatest access to mental health services may require the highest levels of child welfare involvement, even when accounting for child mental health needs. Thus, a confluence of factors related to child welfare involvement may be associated with our findings regarding child mental health service use for which we did not account.
Fourth, our model of child mental health service utilization included a limited number of measured factors that influence service use. For example, while caregiver’s service use may influence child service use, other caregiver factors we did not measure (e.g. substance abuse) may additionally influence children’s use of mental health services. It was not possible in this study to include all the possible caregiver factors that might affect child service use. Thus, we chose to focus on available factors pertaining to caregiver social networks that have been previously found to be associated with child mental health service use (Bussing et al., 2003; Martinez & Lau, 2011). There may also be unmeasured social network factors (e.g., the nature and quality of family relations within a child’s home or the social network’s attitudes and beliefs about mental health services) that are associated with a child’s mental health service use for which our data does not account.
Finally, our conceptual model (Costello et al., 1998) for this study suggests the role of schools as a provider of mental health services and the support offered by schools to caregivers in terms of identifying the child’s problems as mental health-related and offering feedback on next steps to address the concern. Our analyses, however, do not account for this possible role. This certainly warrants further investigation to determine the extent of the school’s role as a network influence on child mental health service use among maltreated children.
Limitations notwithstanding, our findings add to the extant literature regarding social network support characteristics associated with both mental health need and service use among maltreated children and children at-risk for maltreatment. Importantly, previous studies have found maltreatment to be associated with lower treatment engagement and participation (Burns et al., 2004). These findings suggest that detrimental aspects of caregivers’ support networks (or the lower use of social network support), and caregiver mental health needs are related to children’s use of mental health services. Our findings suggest that mental health and child welfare practitioners working with this population should pay attention to the assessment of the caregiver’s support network, as well as their mental health to determine their unique associations with the child’s well-being. If children who need mental health services have parents with significant mental health problems, the factors associated with caregivers’ service utilization and mental health outcomes should be assessed to determine whether those factors are likely to also inhibit child mental health service use and/or benefit. If so, this knowledge may suggest ways to overcome these obstacles in order to increase the chance that the child will get the services he/she needs and have the best chance possible of benefitting from them. Future research might also examine, via a longitudinal design, at which point(s) in the mental health problem cycle social networks are activated, to untangle the issue of whether caregiver networks in these troubled families tend to buttress or negatively impact caregiver and child emotional/psychological well-being.
Acknowledgments
Dr. Lindsey was supported for his time in preparation of this manuscript by the University of Maryland Multidisciplinary Research Career Development Program MCRDP (NIH K12RR023250; PI: Alan R. Shuldiner). Dr. Lindsey was awarded a personal competitive 5-year K12 scholar career development award as allocated under the institutional MCRDP K12 grant awarded to the University of Maryland.
References
- Achenbach TM. Manual for child behavior checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- Barlow M, Wildman BG, Stancin T. Mothers’ help-seeking for pediatric psychosocial problems. Clinical Pediatrics. 2005;44(2):161–167. doi: 10.1177/000992280504400208. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(11):1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Berkowitz Improving access to health care: Case management for vulnerable children. Social Work in Health Care. 1992;17(1):101–123. doi: 10.1300/j010v17n01_07. [DOI] [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA, Foster EM. The role of caregiver strain and other family variables in determining children’s use of mental health services. Journal of Emotional and Behavioral Disorders. 2003;11(2):78–92. [Google Scholar]
- Burns BJ, Mustillo SA, Farmer EMZ, Kolko DJ, McCrae J, Libby AM, et al. Caregiver depression, mental health service use, and child outcomes. In: Webb MB, Dowd K, Harden BJ, Landsverk J, Testa MF, editors. Child welfare and child well-being – New perspectives from the National Survey of Child and Adolescent Well-being. New York, NY: Oxford University Press; 2010. pp. 351–379. [Google Scholar]
- Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, et al. Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Gary FA, Mason DM, Leon CE, Sinha K, et al. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(7):842–850. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- Cauce AM, DomenechRodriguez M, Paradise M, Cochran BN, Shea JM, Srebnik D, et al. Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology. 2002;70(1):44–55. doi: 10.1037//0022-006x.70.1.44. [DOI] [PubMed] [Google Scholar]
- Caughy MO, O’Campo PJ, Muntaner C. When being alone might be better: Neighborhood poverty, social capital, and child mental health. Social Science & Medicine. 2003;57(2):227–237. doi: 10.1016/s0277-9536(02)00342-8. [DOI] [PubMed] [Google Scholar]
- Coohey C. Social networks, informal child care, and inadequate supervision by mothers. Child Welfare: Journal of Policy, Practice, and Program. 2007;86(6):53–66. [PubMed] [Google Scholar]
- Costello EJ, Pescosolido BA, Angold A, Burns BJ. A family network-based model of access to child mental health services. Research in Community and Mental Health. 1998;9:165–190. [Google Scholar]
- Cutrona CE, Russell D. The provisions of social relationships and adaptation to stress. 1987:37–67. [Google Scholar]
- Davies PT, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;33(4):657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, editor. BSI, brief symptom inventory: Administration, scoring & procedures manual. 4. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- dosReis S, Mychailyszyn MP, Myers M, Riley AW. Coming to terms with ADHD: How urban African–American families come to seek care for their children. Psychiatric Services (Washington, D C) 2007;58(5):636–641. doi: 10.1176/ps.2007.58.5.636. [DOI] [PubMed] [Google Scholar]
- Drewes DW. Subject-centered scalability: The sine qua non of summated ratings. Psychological Methods. 2009;14(3):258–274. doi: 10.1037/a0016621. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Zucker RA, Fitzgerald HE. The role of family influences in development and risk. Alcohol Health and Research World. 1997;21(3):218–226. [PMC free article] [PubMed] [Google Scholar]
- Ezzell CE, Swenson CC, Faldowski RA. Child, family, and case characteristics: Links with service utilization in physically abused children. Journal of Child and Family Studies. 1999;8:271–284. [Google Scholar]
- Farmer E, Burns B, Chapman M, Phillips S, Angold A, Costello E. Use of mental health services by youth in contact with social services. The Social Service Review. 2001;75(4):605. [Google Scholar]
- Farmer EMZ, Mustillo SA, Wagner HR, Burns BJ, Kolko DJ, Barth RP, et al. Service use and multi-sector use for mental health problems by youth in contact with child welfare. Children and Youth Services Review. 2010;32(6):815–821. [Google Scholar]
- Farmer EMZ, Stangl DK, Burns BJ, Costello EJ, Angold A. Use, persistence, and intensity: Patterns of care for children’s mental health across one year. Community Mental Health Journal. 1999;35(1):31–46. doi: 10.1023/a:1018743908617. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Wolak J, Berliner L. Police reporting and professional help seeking for child crime victims: A review. Child Maltreatment. 2001;6(1):17–30. doi: 10.1177/1077559501006001002. [DOI] [PubMed] [Google Scholar]
- Flisher AJ, Kramer RA, Grosser RC, Alegria M, Bird HR, Bourdon KH, et al. Correlates of unmet need for mental health services by children and adolescents. Psychological Medicine. 1997;27(5):1145–1154. doi: 10.1017/s0033291797005412. [DOI] [PubMed] [Google Scholar]
- Ford T, Collishaw S, Meltzer H, Goodman R. A prospective study of childhood psychopathology: Independent predictors of change over three years. Social Psychiatry and Psychiatric Epidemiology. 2007;42(12):953–961. doi: 10.1007/s00127-007-0272-2. [DOI] [PubMed] [Google Scholar]
- Ghuman HS, Weist MD, Shafer ME. Demographic and clinical characteristics of emotionally disturbed children being raised by grandparents. Psychiatric Services. 1999;50(11):1496–1498. doi: 10.1176/ps.50.11.1496. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295X.106.3.458. [DOI] [PubMed] [Google Scholar]
- Graham JW, Cumsille PE, ElekFisk E. Methods for handling missing data. US: John Wiley & Sons Inc; 2003. Retrieved from; pp. 87–114. [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry. 2003;60(3):253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan P, Shih J. Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):994–1002. doi: 10.1097/01.chi.0000127588.57468.f6. [DOI] [PubMed] [Google Scholar]
- Harrison ME, McKay MM, Bannon WMJ. Community Mental Health Journal. 2004;40(2):119–131. doi: 10.1023/b:comh.0000022732.80714.8b. [DOI] [PubMed] [Google Scholar]
- Hoagwood KE. Family-based services in children’s mental health: A research review and synthesis. Journal of Child Psychology and Psychiatry. 2005;46(7):690–713. doi: 10.1111/j.1469-7610.2005.01451.x. [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Gary L, Briggs-Gowan M, Carter A. Do needs drive services use in young children? Pediatrics. 2003;112(6):1373–1378. doi: 10.1542/peds.112.6.1373. [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Hulburt MS, Zhang J. Patterns and predictors of mental health services use by children in contact with the child welfare system. In: Webb MB, Dowd K, Harden BJ, Landsverk J, Testa MF, editors. Child welfare and child well-being — New perspectives from the National Survey of Child and Adolescent Well-being. New York, NY: Oxford University Press; 2010. pp. 279–329. [Google Scholar]
- Humphreys C. Whatever happened on the way to counseling? Hurdles in the interacency environment. Child Abuse & Neglect. 1995;19:801–809. doi: 10.1016/0145-2134(95)00045-a. [DOI] [PubMed] [Google Scholar]
- Hunter WM, Cox CE, Teagle S, Johnson RM, Mathew R, Knight ED, et al. Measures for assessment of functioning and outcomes in longitudinal research on child abuse. Middle Childhood. 2003;2 [Google Scholar]
- Jreskog KG. LISREL 8 user’s reference guide. Chicago IL: Scientific Software International; 1996. [Google Scholar]
- Kim IJ, Ge X, Brody GH, Conger RD, Gibbons FX, Simons RL. Parenting behaviors and the occurrence and co-occurrence of depressive symptoms and conduct problems among African American children. Journal of Family Psychology. 2003;17(4):571–583. doi: 10.1037/0893-3200.17.4.571. [DOI] [PubMed] [Google Scholar]
- Klem L. Structural equation modeling. In: Grimm LG, Yarnold PR, editors. Reading and understanding more multivariate statistics. Washington, DC: American Psychological Association; 2000. pp. 227–259. [Google Scholar]
- Kolko DJ, Seleyo J, Brown EJ. The treatment histories and service involvement of physically and sexually abusive families: Description, correspondence and clinical correlates. Child Abuse & Neglect. 1999;23:459–476. doi: 10.1016/s0145-2134(99)00022-8. [DOI] [PubMed] [Google Scholar]
- Landsverk J, Hurlburt MS, Leslie L, Rolls J, Zhang J. Exits from out-of-home care and continuity of mental health service use. In: Webb MB, Dowd K, Harden BJ, Landsverk J, Testa MF, editors. Child welfare and child well-being —New perspectives from the National Survey of Child and Adolescent Well-being. New York, NY: Oxford University Press; 2010. pp. 279–329. [Google Scholar]
- Lau AS, Valeri SM, McCarty CA, Weisz JR. Abusive parents’ reports of child behavior problems: Relationship to observed parent–child interactions. Child Abuse & Neglect. 2006;30(6):639–655. doi: 10.1016/j.chiabu.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Lavoie F, Hodgins S. Mental disorders among children with one parent with a lifetime diagnosis of major depression. In: Hodgins S, Lane C, LaRoche C, Lavoie F, Kratzer L, Palmour R, Rubin N, editors. A critical review of the literature on children at-risk for major affective disorders. Ottawa: The Strategic Fund for Children’s Mental Health; 1994. pp. 37–82. [Google Scholar]
- Lewinsohn PM, Olino TM, Klein DN. Psychosocial impairment in offspring of depressed parents. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2005;35(10):1493–1503. doi: 10.1017/S0033291705005350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Browne DC, Thompson R, Hawley KM, Graham JC, Weisbart C, et al. Caregiver mental health, neighborhood, and social network influences on mental health needs among african american children. Social Work Research. 2008;32(2):79–88. [Google Scholar]
- Logan DE, King CA. Parental facilitation of adolescent mental health services utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2001;8(3):319–333. [Google Scholar]
- Lyons JS, Rogers L. The U.S. child welfare system: A de facto public behavioral health care system. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(8):971. doi: 10.1097/01.chi.0000127575.23736.90. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez LM. Neighborhood context and the development of African American children. New York, NY: Garland; 2000. [Google Scholar]
- Martinez JI, Lau AS. Do social networks push families toward or away from youth mental health services?: A national study of families in child welfare. Journal of Emotional and Behavioral Disorders. 2011;19(3):169–181. doi: 10.1177/1063426610377898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCray JS, Barth RP, Guo S. Changes in maltreated children’s emotional–behavioral problems following typically provided mental health services. The American Journal of Orthopsychiatry. 2010;80(3):350–361. doi: 10.1111/j.1939-0025.2010.01039.x. [DOI] [PubMed] [Google Scholar]
- Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born black and latina women from seeking mental health care? Psychiatric Services. 2007;58(12):1547–1554. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- Ohannessian C, Hesselbrock V, Kramer J, Kuperman S, Bucholz K, Schuckit M, et al. The relationship between parental alcoholism and adolescent psychopathology: A systematic examination of parental comorbid psychopathology. Journal of Abnormal Child Psychology. 2004;32(5):519–533. doi: 10.1023/b:jacp.0000037781.49155.a6. [DOI] [PubMed] [Google Scholar]
- Pascoe JM, Ialongo NS, Horn WF, Reinhart MA, Perradatto D. The reliability and validity of the maternal social support index. Family Medicine. 1988;20(4):271–276. [PubMed] [Google Scholar]
- Pescosolido BA. Beyond rational choice: The social dynamics of how people seek help. The American Journal of Sociology. 1992;97(4):1096–1138. [Google Scholar]
- Runyan DK, Hunter WM, Socolar RR, Amaya-Jackson L, English D, Landsverk J, et al. Children who prosper in unfavorable environments: The relationship to social capital. Pediatrics. 1998;101(1):12–18. doi: 10.1542/peds.101.1.12. [DOI] [PubMed] [Google Scholar]
- Schafer J, Graham J. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- Snowden L. Racial, cultural and ethnic disparities in health and mental health: Toward theory and research at community levels. American Journal of Community Psychology. 2005;35(1–2):1–8. doi: 10.1007/s10464-005-1882-z. [DOI] [PubMed] [Google Scholar]
- Staudt MM. Mental health services utilization by maltreated children: Research findings and recommendations. Child Maltreatment. 2003;8(3):195–203. doi: 10.1177/1077559503254138. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Chen YW, Elze D, Dore P, Cheng LC. Adolescents’ and providers’ perspectives on the need for and use of mental health services. Journal of Adolescent Health. 1997;21:335–342. doi: 10.1016/S1054-139X(97)00046-3. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Pescosolido B, Cabassa LJ. Building a model to understand youth service access: The gateway provider model. Mental Health Services Research. 2004;6(4):189–198. doi: 10.1023/b:mhsr.0000044745.09952.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R, Lindsey M, English D, Hawley K, Lambert S, Browne D. The influence of family environment on mental health need and service use among vulnerable children. Child Welfare. 2007;86(5):57–74. [PubMed] [Google Scholar]
- Thompson R, May MA. Caregivers’ perceptions of child mental health needs and service utilization: An urban 8-year old sample. The Journal of Behavioral Health Services & Research. 2006;33(4):474–482. doi: 10.1007/s11414-006-9021-7. [DOI] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, Wester SR, Larson L, Hackler AH. Seeking help from a mental health professional: The influence of one’s social network. Journal of Clinical Psychology. 2007;63(3):233–245. doi: 10.1002/jclp.20345. [DOI] [PubMed] [Google Scholar]
- Walrath CM, Nickerson KJ, Crowel RL, Leaf PJ. Serving children with serious emotional disturbance in a system of care: Do mental health and non-mental health agency referrals look the same? Journal of Emotional and Behavioral Disorders. 1998;6(4):205–213. [Google Scholar]
- Wu P, Hoven CW, Cohen P, Liu X, Moore RE, Tiet Q, et al. Factors associated with use of mental health services for depression by children and adolescents. Psychiatric Services. 2001;52(2):189–195. doi: 10.1176/appi.ps.52.2.189. [DOI] [PubMed] [Google Scholar]


