Abstract
Purpose
The purpose of this study is to report a novel case of a Klebsiella oxytoca-associated infectious crystalline keratopathy
Methods
This is a case report study.
Results
An 80-year-old woman presented with complaint of noticing a white spot in the left eye for 2 to 3 days, as well as mild soreness and discharge. Past ocular history was notable for a failed left corneal transplant for which she was taking prednisolone acetate 1 % twice per day. On slit-lamp examination, there was an extensive stromal ulcer and infiltrate in the inferior half of the transplant. Extending superiorly in the graft were branching, needle-like deep stromal opacities, characteristic of infectious crystalline keratopathy. Diagnostic scrapings revealed Gram-negative bacilli, subsequently identified on culture as K. oxytoca. There was also light growth of Staphylococcus species. The patient was placed on double topical antibiotic therapy with moxifloxacin and fortified tobramycin. After 2 months of treatment there was gradual resolution of the infection.
Conclusions
K. oxytoca is a microorganism which can be associated with clinical infectious crystalline keratopathy, presenting as a mixed infection along with Staphylococcus species.
Keywords: Infectious crystalline keratopathy, ICK, Klebsiella oxytoca, Staphylococcus, Keratitis
Introduction
Infectious crystalline keratopathy (ick) is a slowly progressing corneal infection characterized by branching, grayish-white, needle-like opacities within the corneal stroma, with a paucity of corneal and anterior segment inflammation [1, 2]. The crystalline deposits are composed of bacteria aggregating and spreading within the corneal stromal lamellae. The bacteria are enveloped in a biofilm composed of an exopolysaccharide glycocalyx. This biofilm isolates the infectious organisms from the immune system, as well as conferring resistance to antimicrobial penetration [3]. Risk factors for infectious crystalline keratopathy include previous corneal surgery, long-term topical corticosteroid use, prior corneal disease, and systemic immunocompromise [2]. It has been reported after cataract extraction, penetrating keratoplasty, corneal refractive surgery, and glaucoma filtering surgery. Many microbial pathogens have been reported to cause infectious crystalline keratopathy (ICK), especially Gram-positive cocci, and streptococci in particular [4]. In this report, we present the first case of a patient with infectious crystalline keratopathy associated with Klebsiella oxytoca.
Case report
An 80-year-old woman presented with complaint of noticing a white spot in her left eye for 2 to 3 days. There was mild soreness and discharge. The patient had a complicated past ocular history involving that eye, beginning with significant myopic degeneration. Nineteen years prior, she had undergone left eye cataract surgery. Eleven years later she sustained a ruptured left globe. Despite emergent repair, she developed corneal blood staining and corneal decompensation, requiring penetrating keratoplasty. The graft ultimately failed, and was not repeated due to limited visual potential. At the time of presentation, she was being maintained on prednisolone acetate 1 %, twice per day.
On examination, visual acuity was hand motion in the left eye. Slit-lamp examination revealed minimal conjunctival injection. There was an extensive stromal infiltrate in the transplant involving much of its inferior and central aspects, bordered by the graft edge. Extending upward into the superonasal graft were deep branching, needle-like stromal opacities (Fig. 1).
Fig. 1.
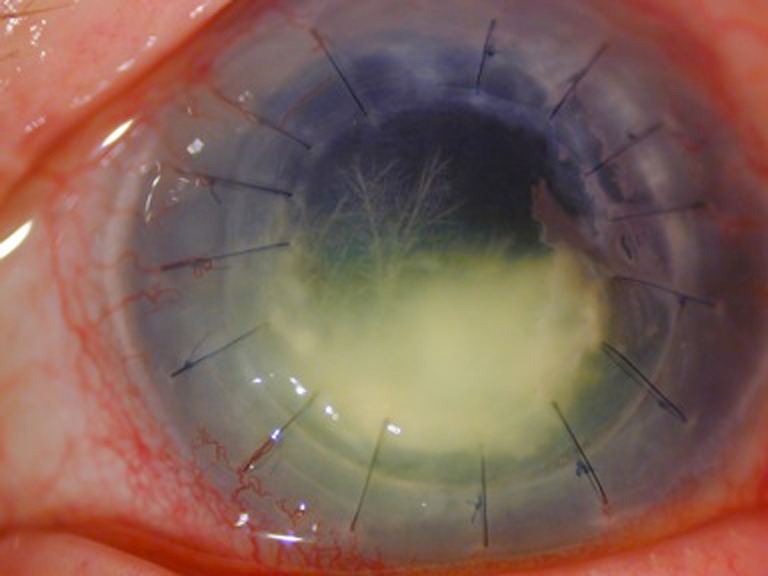
Slit-lamp photograph of infectious infiltrate in the graft. There are branching needle-like stromal opacities extending upwards characteristic of infectious crystalline keratopathy
Based on the clinical picture, the patient was diagnosed with an infectious keratitis, manifesting as infectious crystalline keratopathy. diagnostic corneal scrapings were performed; sutures within the infiltrate were removed and cultured as well. Gram staining revealed Gram-negative bacilli. The organism was identified as K. oxytoca on culture. There was also a minor growth of Staphylococcus species. The patient was placed on intensive topical antibiotic therapy utilizing moxifloxacin 0.3 % and fortified tobramycin 15 mg/ml. After 2 months of treatment, there was gradual resolution of the infection, with healing of the ulcer and scarring-in of the infiltrate.
Discussion
Diagnosis of ICK is primarily established by clinical appearance on slit-lamp examination. Isolation of the infectious organism can often be difficult since the infiltrate may often lie deep within the corneal stroma, inaccessible to superficial scrapings. Needling of the crystals, culturing involved sutures, or corneal biopsy may be required [5]. At times, a specific pathogen has only been identified after therapeutic corneal transplantation [6]. Polymerase chain reaction has also been demonstrated to be a useful diagnostic tool [7].
Many microorganisms have been identified as causative agents for ICK. Gram-positive alpha-hemolytic streptococci, typically of the Viridans group, are the most common pathogens encountered [2, 4]. Additional Gram-positive bacteria that have been isolated include enterococci, Staphylococcus aureus, and other staphylococcal species, Gemella haemolysans, and anaerobes such as proprionobacterium acne [2, 4, 5]. Non-bacterial organisms have also been implicated in ICK, like filamentous fungi and yeasts including Candida [2, 4, 8], and in mixed infections associated with Acanthamoeba [2, 9]. A few case reports have highlighted the occurrence of ICK after LASIK surgery, caused by microbes such as nontuberculous mycobacteria [10] and Alternaria species [8]. Gram-negative bacteria likewise have not escaped notice, with Serratia marcescens, various species of Pseudomonas and Hemophilus, and even the spirochete Borrelia garinii having been described [2, 4, 6, 7, 11, 12].
To the best of our knowledge, this is the first actual clinical report of infectious crystalline keratopathy associated with K. oxytoca. A typical Gram-negative keratitis of this size would usually present acutely with severe pain, deep injection, purulent discharge, keratolysis, and hypopyon. We believe that the patient's subacute and pauci-inflammatory clinical presentation indicates that the klebsiella was a true and integral contributor to the ICK infection itself. K. oxytoca is a Gram-negative rod, in the enterobacteriaceae family. It is a common cause of antibiotic-associated, Clostridium difficile-negative, hemorrhagic colitis in immunocompetent individuals [13]. It is also an infectious agent involved in meningitis, adrenal hemorrhage and septic shock in immunocompromised patients. An in vitro model of ICK has been created by inoculating K. oxytoca onto corneal buttons [14].
The exact role of the Staphylococcus species that was cultured concomitantly in our patient is unclear. It was thought to be a possible contaminant because of lighter growth, but that it may have been a co-infectious agent is also possible. We do know that there have been several descriptions of polymicrobial ICK [4, 9, 11]. In these instances, one of the isolates may be considered as the primary [4]. We would propose that the infectious milieu of a polymicrobial keratitis is one of those settings that can promote ICK. Tu and colleagues touch on this concept with their suggestion of possible “endosymbiosis” between co-infectious agents, in their report of acanthamoeba keratitis complicated by concomitant ICK from different Gram-positive cocci [9].
Medical treatment of ICK is often difficult, and involves extended use of antibiotics targeted against the etiologic organism. The Nd:YAG laser, intrastomal antibiotic injection, and even the act of corneal biopsy have been found to be useful adjunctive therapy, presumably in part by disrupting the microbial biofilm [3, 5, 15]. Therapeutic penetrating keratoplasty may be required in up to 50 % of cases [2]. Double antibiotic therapy targeted toward the cultured pathogen was effective in resolving our patient's infection. More study may be required to determine if this approach results in faster resolution than monotherapy, or reduces the need for surgical intervention.
Conclusions
K. oxytoca is a microorganism that can be associated with infectious crystalline keratopathy. It may be present in the form of a mixed microbial keratitis along with Staphylococcus species. Treatment may be prolonged, but double topical antimicrobial therapy can be effective in eradicating the infection.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Gorovoy MS, Stern GA, Hood CI, Allen C. Intrastromal noninflammatory bacterial colonization of a corneal graft. Arch Ophthalmol. 1983;101:1749–1752. doi: 10.1001/archopht.1983.01040020751018. [DOI] [PubMed] [Google Scholar]
- 2.Sharma N, Vajpayee RB, Pushker N, Vajpayee M. Infectious crystalline keratopathy. CLAO J. 2000;26:40–43. [PubMed] [Google Scholar]
- 3.Masselos K, Tsang HH, Ooi JL, Sharma NS, Coroneo MT. Laser corneal biofilm disruption for infectious crystalline keratopathy. Clin Experiment Ophthalmol. 2009;37:177–180. doi: 10.1111/j.1442-9071.2008.01912.x. [DOI] [PubMed] [Google Scholar]
- 4.Khater TT, Jones DB, Wilhelmus KR. Infectious crystalline keratopathy caused by gram-negative bacteria. Am J Ophthalmol. 1997;124:19–23. doi: 10.1016/s0002-9394(14)71638-1. [DOI] [PubMed] [Google Scholar]
- 5.Kailasanathan A, Anderson DF. Infectious crystalline keratopathy caused by Gemella haemolysans. Cornea. 2007;26:643–644. doi: 10.1097/ICO.0b013e3180439c0c. [DOI] [PubMed] [Google Scholar]
- 6.Chen CL, Tai MC, Chen JT, Chen CH, Lu DW. Infectious crystalline keratopathy caused by Serratia marcescens. Cornea. 2007;26:1011–1013. doi: 10.1097/ICO.0b013e3180de4928. [DOI] [PubMed] [Google Scholar]
- 7.Dietrich T, Geidorfer W, Schlotzer-Schrehardt U, Holbach L, Schoemer C, Seitz B. Borrelia-associated crystalline keratopathy with intracorneal detection of Borrelia garinii by electron microscopy and polymerase chain reaction. Cornea. 2008;27:498–500. doi: 10.1097/ICO.0b013e318162a8f5. [DOI] [PubMed] [Google Scholar]
- 8.Verma K, Vajpayee RB, Titiyal JS, Sharma N, Nayak N. Post-LASIK infectious crystalline keratopathy caused by Alternaria. Cornea. 2005;24:1018–1020. doi: 10.1097/01.ico.0000159735.83295.1c. [DOI] [PubMed] [Google Scholar]
- 9.Tu EY, Joslin CE, Nijm LM, Feder RS, Jain S, Shoff ME. Polymicrobial keratitis: Acanthamoeba and infectious crystalline keratopathy. Am J Ophthalmol. 2009;148:13–19. doi: 10.1016/j.ajo.2009.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvarenga L, Freitas D, Hofling-Liima AL, Belfort R, Jr, Sampaio J, Sousa L, Yu M, Mannis M. Infectious post-LASIK crystalline keratopathy caused by nontuberculous mycobacteria. Cornea. 2002;21:426–429. doi: 10.1097/00003226-200205000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Hu FR. Infectious crystalline keratopathy Caused by Mycobacterium fortuitum and Pseudomonas aeruginosa. Am J Ophthalmol. 1990;109:738–739. doi: 10.1016/s0002-9394(14)72451-1. [DOI] [PubMed] [Google Scholar]
- 12.Connell B, Armstrong M, Tullo A. A case of recurrent infectious crystalline keratopathy secondary to Haemophilus influenza. Eye (Lond) 2007;21:427–428. doi: 10.1038/sj.eye.6702614. [DOI] [PubMed] [Google Scholar]
- 13.Högenauer C, Langner C, Beubler E, Lippe IT, Schicho R, Gorkiewicz G, Krause R, Gerstgrasser N, Kreis GJ, Hinterleitner TA. Klebsiella oxytoca as a causative organism of antibiotic-associated hemorrhagic colitis. N Engl J Med. 2006;355:2418–2426. doi: 10.1056/NEJMoa054765. [DOI] [PubMed] [Google Scholar]
- 14.Butler TK, Dua HS, Edwards R, Lowe JS. In vitro model of infectious crystalline keratopathy: Tissue architecture determines pattern of microbial spread. Invest Ophthalmol Vis Sci. 2001;42:1243–1246. [PubMed] [Google Scholar]
- 15.Khan IJ, Hamada S, Rauz S. Infectious crystalline keratopathy treated with intrastromal antibiotics. Cornea. 2010;29:1186–1188. doi: 10.1097/ICO.0b013e3181d403d4. [DOI] [PubMed] [Google Scholar]


