Abstract
Aim
The technical quality of a root canal treatment is clinically judged by the apical extension and homogeneity of the filling material imaged by periapical radiographs (PA). The aim of this experiment was to evaluate the association between the technical quality of the root canal filling and treatment outcome.
Materials and methods
In 234 teeth (268 roots) that underwent root-canal treatment, the quality of the root canal filling as well as the outcome of the treatment were assessed with both PA and cone-beam computed tomography (CBCT) 2 years after treatment. Satisfactory root filling on PA was defined as 0–2 mm within the radiographic apex without voids; on CBCT scans, the apical end of the canal replaced the radiographic apex. The outcome predictors were analyzed using multivariate logistic regression.
Results
At recall, periapical radiolucent areas were absent in 198 (74%) roots on PA and 164 (61%) roots on CBCT scans. The presence of preoperative periapical radiolucency and the quality of root filling and coronal restoration were identified by both PA and CBCT as outcome predictors (p < 0.01). Complete absence of post-treatment periapical radiolucency was observed in CBCT scans in 81% and 49% of satisfactory and unsatisfactory root fillings, respectively, as compared to 87% and 61% revealed by PA.
Conclusion
Satisfactory root fillings were associated with a favorable outcome, confirmed by both PA and CBCT.
Clinical relevance
The outcome of root canal treatment is improved once the filling is 0–2 mm from the apex, and no voids could be detected. Technical skills and performance of root canal filling procedures should be emphasized, and suitable methods should be developed in order to achieve more compacted filling materials without voids and at the correct length.
Keywords: Cone-beam computed tomography, Outcome, Satisfactory root filling, Unsatisfactory root filling
Introduction
A root canal treatment performed with the highest standards of care will often result in healing of the periapical lesion [1]. Since the treatment is technically judged by periapical radiographs (PA), the quality of the treatment is mainly judged by the apical extent of the filling and presence or absence of voids. Some outcome studies concluded that flush root fillings that end 0–2 mm shorter from the radiographic apex are associated with a significantly higher success rate than short (>2 mm from the radiographic apex) or long (extruded beyond the radiographic apex) root fillings [2]. However, other studies could not verify such an association [3–9]. Similarly, radiographically visible voids along root fillings were associated with a less favorable outcome [3, 10, 11]; however, Sjögren et al. [12] and Heling et al. [8] reported that the homogeneity of root fillings had no significant influence on the outcome. Inadequate instrumentation often leads to short root fillings, whereas over instrumentation results in extruded filling material, which may also include infected matter and dentin chips [13]. Radiographic presence of voids could be due to residual pulp tissue and/or dentinal debris in the canal, which indicates inadequate debridement and persistent infection [14, 15]. Meanwhile, voids could be created by problems during obturation [15]. High standard technical quality in cleaning, shaping, and filling root canals, as represented by flush root fillings without voids, positively influences the outcome.
The commonly used PAs are two dimensional and might not detect relevant information in orthogonal planes [16]. Cone-beam computed tomography (CBCT) allows the tooth to be assessed three-dimensionally and may have higher diagnostic yield as compared to PA when assessing outcome of root canal treatments [17]. The increased accuracy of CBCT may highlight differences in outcome between high and low standard root canal treatments that otherwise could be overlooked by PA. There is thus far one clinical study where the outcome of root canal treatment was associated with the length and homogeneity of the root canal filling on CBCT (18).
The terms “satisfactory” and “unsatisfactory” root filling were previously used in retreatments outcome studies [19–21]. It has been realized that in teeth with flush root filling without voids, the persistent lesion is likely to be caused by extraradicular infection, a true cyst or foreign body reaction unresponsive to the non-surgical root canal treatments [21].
The purpose of this study was to evaluate the association between the quality of root canal fillings and treatment outcome, assessed with both PA and CBCT.
Materials and methods
This retrospective cohort study evaluated the outcome of endodontic treatments carried out between January 2007 and October 2008. A 2-year follow-up period was chosen because 91–95% of periapical lesions heal completely within 2 years [21]. Maxillary molars were not included because radiographic overlap hinders the observation of periapical lesions. A total of 457 patients were consecutively contacted by telephone and letter and invited to participate in the follow-up examination. Of the 457 subjects, 213 (47%) attended the recall; 193 subjects (234 teeth and 268 roots), 80 male and 113 female, with a median age of 48 years, signed informed consent forms for clinical and radiological examination. In 20 subjects, the treated teeth were either extracted or retreated. In the 268 roots included, 125 had preoperative radiographic evidence of apical periodontitis (AP) on PA. The results of the other 143 roots without preoperative AP on PA have been reported separately [18]. This study protocol was approved by the ethics board of Peking University Health Science Center. All of the participants were informed of the aims and radiation dose of the CBCT examination, and their consent was secured.
Root canal treatment
All treatment data were recorded in the original charts by the treatment providers, endodontists in the Department of Cariology and Endodontology of the Peking University School and Hospital of Stomatology, Beijing, China. During preparation, a crown-down technique with ProTaper (Dentsply Maillefer, Ballaigues, Switzerland) or Hero Shaper (Micro-Mega, Besancon, France) instruments was performed. Each canal was irrigated with 2.5% sodium hypochlorite (NaOCl) solution. The working length (WL) was established with the aid of an apex locator, Root ZX (J. Morita Corp.,Kyoto, Japan), and a WL of 0–2 mm from the apex was confirmed with PA. When a second visit was required, a calcium hydroxide dressing was used as an inter-appointment dressing. All of the canals were filled with gutta-percha cones (Dentsply Maillefer) and a zinc-oxide-based sealer Cortisomol (Pierre Rolland Acteon Inc., Merignac Cedex, France) using a cold lateral compaction technique. A master gutta-percha cone (Dentsply Maillefer) was lightly coated with sealer and placed into the canal to the full WL. Lateral compaction was achieved using accessory gutta-percha cones (size 25) and a size-B endodontic finger spreader (Dentsply Maillefer) that initially approached to within 2 mm of the full WL. A permanent composite filling or core build-up was placed within 2 weeks on all treated teeth.
Recall
At the follow-up examination pain, swelling, tenderness to percussion, presence of a sinus tract, and the quality of the coronal restoration were recorded.
Two radiographic methods, PA and CBCT, were used to detect post-treatment periapical lesions. Straight projection intraoral PA were obtained with the digital imaging system Digora Optime (Soredex, Helsinki, Finland) using a parallel technique. Exposures of 0.16–0.25 s were obtained with a MinRay dental X-ray unit (Soredex) operating at 60 kV and 7 mA. The digital PAs were obtained by immediately scanning the proprietary storage phosphor plates after exposure using the proprietary software (Dfw v.2.5., Soredex). The selected scanning resolution was 400 dpi. The raw data images were then processed with the proprietary default-processing algorithm and saved as 8-bit images.
CBCT scans of the patients were acquired with a 3DX-Accuitomo CBCT scanner (J. Morita MFG. CORP, Kyoto, Japan), with a 4- × 4-cm field of view (FoV) selection and operating conditions of 80 kVp, 4–5 mA, and an exposure time of 17.5 s. The CBCT data was reconstructed using the system’s proprietary software.
Two pre-calibrated examiners, an endodontist and a radiologist independently assessed the images. In case of disagreement, a discussion followed until a consensus was reached. The absence of periapical lesions was defined as radiolucency no more than twice the width of the periodontal ligament in a non-involved area [22].
Clinical factors assessed
The following clinical factors were checked.
Preoperative factors
Preoperative AP
Presence or absence of preoperative periapical radiolucency was determined.
Gender
Gender was also noted
Tooth type
Treatments performed in the anterior teeth, premolars, and mandibular molars were included.
Canal curvature
Schneider’s method [23] was used to measure the root-canal curvature. All of the roots were divided into three categories depending on the curvature: <10°, 10–25°, and >25°.
Intraoperative factors
Quality of root filling
Satisfactory root filling was defined as 0–2 mm within the radiographic apex (flush) without voids. Unsatisfactory root filling was defined as either short (>2 mm short of radiographic apex) or long (extruded beyond the radiographic apex) with or without voids or flush root fillings with voids.
These definitions are similar to previous studies [2]. With CBCT images, the apical end of the root canal was used as the landmark instead of the radiographic apex; short root filling was diagnosed only when the root filling was short in all dimensions (coronal, sagittal, and axial); long filling was diagnosed when the root filling extended beyond the apical end of the canal in at least one section. When two canals were visible in one single root, satisfactory root filling was diagnosed when both root fillings were flush and without voids; unsatisfactory root fillings were diagnosed when the quality of at least one root filling was unsatisfactory.
Number of treatment visits
The treatment was completed in either one or two visits.
Postoperative factors
Coronal restoration
The quality of the coronal restoration was examined both clinically and radiographically. A satisfactory restoration was defined as having no evidence of discrepancy, discoloration or recurrent caries at the restoration margin, along with an absence of a history of decementation [9]. CBCT scans were not used for this evaluation because metal crowns create noise that hinders the observation [24].
The use as abutment for prosthesis
The influence of the use as abutment for prosthesis on treatment outcome was calculated.
Statistics
The differences between quality assessments done by PA and those done with CBCT were analyzed using a chi-square test. Multivariate logistic regression analysis was performed on the data from both PA and CBCT to identify the outcome predictors. The level of significance was set at α = 0.05. Statistics were calculated using SPSS v17.0 from Windows (SPSS Inc, Chicago, IL, USA).
Results
An assessment of CBCT scans and PA revealed an inter-examiner agreement (Cohen’s kappa) of 0.75 and 0.65, respectively.
At recall, 12 (4.5%) teeth were symptomatic, with pain, swelling, sinus tract, or tenderness to percussion.
In 72 (26.9%) roots, there was a disagreement between PA and CBCT with regard to the apical extent of root filling (Table 1; Figs. 1 and 2); in 96 (35.8%) roots, there was a disagreement between PA and CBCT with regard to the homogeneity of the root filling (Table 2); and in 110 (41%) roots, there was a disagreement between PA and CBCT with regard to the quality of the root filing (Table 3). The difference in the diagnosis between PA and CBCT was statistically significant (p < 0.01). Overall, 29 of the 38 (76.3%) short root fillings on PA appeared as flush fillings on CBCT (Fig. 2); 25 of the 153 (16.3%) PA-determined flush fillings were diagnosed as long fillings by CBCT (Fig. 1); 82 of the 234 (35%) root fillings without voids on PA appeared as root fillings with voids on CBCT (Fig. 3); 70 of the 132 (53%) satisfactory root fillings diagnosed by PA appeared unsatisfactory on CBCT; and 40 of the 136 (29%) unsatisfactory root fillings diagnosed by PA appeared satisfactory on CBCT. On PA, the apical extent of all root fillings was within 3.5 mm of the radiographic apex; on CBCT images, it was within 3.0 mm of the apical end of the root canal. The 166 unsatisfactory root fillings on CBCT included 88 overextended root fillings and 10 short root fillings with or without voids, as well as 68 flush fillings with voids. Complete absence of periapical radiolucency on PA was observed in 73.9% of the 268 treated roots 2-year after treatment as compared to 61.2% by CBCT (Tables 4, 5). Complete absence of radiolucency was achieved in 87.1% of roots with satisfactory root fillings on PA as compared to 81.4% on CBCT.
Table 1.
Apical extension of root fillings determined with PA and CBCT
| PA | Total | ||||
|---|---|---|---|---|---|
| Flush | Long | Short | |||
| CBCT | Flush | 126 | 15 | 29 | 170 |
| Long | 25 | 62 | 1 | 88 | |
| Short | 2 | 0 | 8 | 10 | |
| Total | 153 | 77 | 38 | 268 | |
Fig. 1.
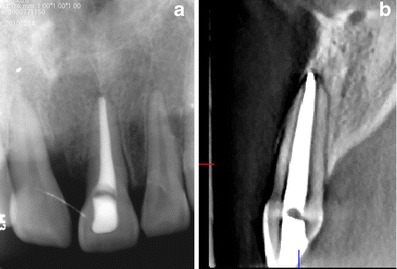
a A radiograph of tooth 21 shows a flush root filling. b A sagittal view on CBCT (note the extruted root filling)
Fig. 2.
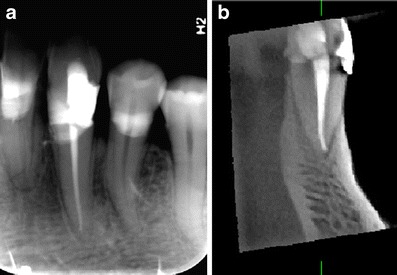
a A radiograph shows a short root filling in tooth 33 that is 2.5 mm short of the radiographic apex. b A sagittal CBCT view. Note the flush filling
Table 2.
The homogeneity of root filling determined with PA and CBCT (n = 268)
| PA | Total | |||
|---|---|---|---|---|
| With voids | Without voids | |||
| CBCT | With voids | 20 | 82 | 102 |
| Without voids | 14 | 152 | 166 | |
| Total | 34 | 234 | 268 | |
Table 3.
The quality of root filling determined with PA and CBCT
| PA | Total | |||
|---|---|---|---|---|
| Satisfactory | Unsatisfactory | |||
| CBCT | Satisfactory | 62 | 40 | 102 |
| Unsatisfactory | 70 | 96 | 166 | |
| Total | 132 | 136 | 268 | |
Fig. 3.
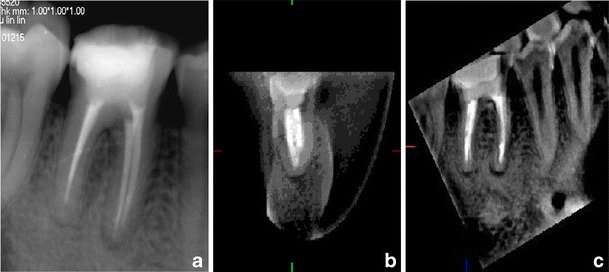
a A periapical radiograph of tooth 46. No void was observed in the distal root filling, but in the coronal and sagittal CBCT views (b, c), void was diagnosed
Table 4.
The outcome of 268 endodontically treated roots as determined by CBCT
| Factors | Number of treated roots | Number (%) of roots without AP at recall | p value |
|---|---|---|---|
| Preoperative AP | |||
| Without | 143 (53.4) | 106 (74.1) | <0.001 |
| With | 125 (46.6) | 58 (46.4) | |
| Gender | |||
| Male | 126 (47.0) | 85 (67.5) | 0.674 |
| Female | 142 (53.0) | 79 (55.6) | |
| Tooth type | |||
| Anterior teeth | 109 (40.1) | 64 (58.7) | 0.856 |
| Premolars | 61 (22.8) | 40 (65.6) | |
| Molars | 98 (36.6) | 60 (61.2) | |
| Curvature | |||
| <10° | 144 (53.7) | 86 (63.6) | 0.298 |
| 10–25° | 96 (35.8) | 61 (72.5) | |
| >25° | 28 (10.4) | 17 (65.2) | |
| Quality of root filling | |||
| Satisfactorya | 102 (38.1) | 83 (81.4) | 0.006 |
| Unsatisfactory | 166 (61.9) | 81 (48.8) | |
| Treatment visits | |||
| Single | 157 (58.6) | 108 (68.8) | 0.112 |
| Two | 111 (41.4) | 56 (50.5) | |
| Coronal restoration | |||
| Satisfactory | 219 (81.7) | 146 (66.7) | <0.001 |
| Unsatisfactory | 49 (18.3) | 18 (36.7) | |
| Use as abutment | |||
| No | 235 (87.7) | 146 (62.1) | 0.133 |
| Yes | 33 (12.3) | 18 (54.5) | |
| Total | 268 (100) | 164 (61.2) | |
aExtending to within 2 mm of the apical end of the root canal and absence of voids
Table 5.
The outcome of 268 endodontically treated roots as determined by PA
| Factors | Number (%) of treated roots | Number (%) of roots without AP at recall | p value |
|---|---|---|---|
| Preoperative AP | |||
| Without | 143 (53.4) | 125 (87.4) | <0.001 |
| With | 125 (46.6) | 73 (58.4) | |
| Gender | |||
| Male | 126 (47.0) | 97 (77.0) | 0.692 |
| Female | 142 (53.0) | 101 (71.1) | |
| Tooth type | |||
| Anterior teeth | 109 (40.1) | 72 (66.1) | 0.798 |
| Premolars | 61 (22.8) | 50 (82.0) | |
| Molars | 98 (36.6) | 76 (77.6) | |
| Curvature | |||
| <10° | 154 (57.5) | 106 (68.8) | 0.446 |
| 10-25° | 91 (34.0) | 77 (84.6) | |
| >25° | 23 (8.6) | 15 (65.2) | |
| Quality of root filling | |||
| Satisfactorya | 132 (49.3) | 115 (87.1) | <0.001 |
| Unsatisfactory | 136 (50.7) | 83 (61.0) | |
| Treatment visits | |||
| Single | 157 (58.6) | 126 (80.3) | 0.165 |
| Two | 111 (41.4) | 72 (64.9) | |
| Coronal restoration | |||
| Satisfactory | 219 (81.7) | 170 (77.6) | <0.001 |
| Unsatisfactory | 49 (18.3) | 28 (57.1) | |
| Use as abutment | |||
| No | 235 (87.7) | 173 (73.6) | 0.127 |
| Yes | 33 (12.3) | 25 (75.8) | |
| Total | 268 (100) | 198 (73.9) | |
aExtending to within 2 mm of the radiographic apex and absence of voids
The outcome associated with satisfactory and unsatisfactory root fillings in cases with and without preoperative AP are presented in Tables 6 and 7 separately.
Table 6.
The outcome of 125 roots with preoperative apical periodontitis (AP) associated with satisfactory and unsatisfactory root fillings, as determined by CBCT
| Root filling | Post-treatment AP | Total | |
|---|---|---|---|
| Absence (%) | Presence (%) | ||
| Satisfactory | 31 (69) | 14 (31) | 45 |
| Unsatisfactory | 27 (34) | 53 (66) | 80 |
| 125 | |||
Table 7.
The outcome of 143 roots without preoperative apical periodontitis (AP) associated with satisfactory and unsatisfactory root fillings, as determined by CBCT
| Root filling | Post-treatment AP | Total | |
|---|---|---|---|
| Absence (%) | Presence (%) | ||
| Satisfactory | 52 (91) | 5 (9) | 57 |
| Unsatisfactory | 54 (63) | 32 (37) | 86 |
| 143 | |||
The assessed factors and their effects on treatment outcome are presented in Tables 4 and 5. The multivariate logistic regression analysis revealed that the preoperative apical status, the quality of the root filling, and coronal restoration were risk factors affecting the treatment outcome (p < 0.01). The other factors did not significantly influence the outcome (p > 0.05).
Discussion
Methodology
In the current retrospective clinical outcome study, the presence of preoperative AP and the quality of both root filling and coronal restoration significantly influenced the treatment outcome, as revealed by multivariate logistic regression. Our findings are in line with previous outcome studies [2].
Only 47% of the 457 treated subjects attended their follow-up appointment because of the high dropout rate over the 2-year recall period given the population mobility in Beijing, a city with rapidly growing economic activities. With a low recall rate, the reported success rate could be under- or overestimated [25, 26]. The root rather than the whole tooth was used as the entity for measurements in this study and several previous outcome studies [2, 12], which has a tendency to over-estimate success rates [27, 28]. However, the use of a whole tooth would render investigation of some variables (density and apical extent of root filling) problematic, as they could be independent for different roots in the same tooth. Two visit treatments were performed in 41% of cases (Table 5) due to insufficient chair time at the first visit or the personal preference of some of the dentists to use calcium hydroxide between appointments [7, 12, 28]. The success rate for two visit was 18% lower than that of single visit treatments (Table 4), but the difference was not statistically significant (p = 0.112). Furthermore, a prednisolone containing sealer that may influence the periapical healing [2] was used. Importantly, the purpose of the present study was not to report success rates but to explore the association between the quality of root fillings and the treatment outcome. Although in this study maxillary molars were excluded, 34 teeth had two roots, and in some roots of premolars and mandibular molars, two canals could have existed. Radiographic overlap could disturb the assessment of both the periapical lesion of each root and the quality of each root filling. This may partly explain the differences in quality and outcome determined by PA and CBCT (Tables 1, 2, 3, 6, and 7). As preoperative CBCT scans were not available in this retrospective study, the number of roots with preoperative AP in Table 4 and 5 might be underestimated and the number of roots without preoperative AP overestimated [16, 17]. Reliable success rates for teeth with or without preoperative AP should be recorded in future studies where CBCT scans are performed both pretreatment and recall.
Association between the quality and outcome
In this study, satisfactory root fillings (flush fillings without voids) were observed in 132 of the 268 (49%) roots on PA or 102 of the 268 (38%) roots on CBCT (Table 3).
Complete resolution of the periapical lesion was observed in 87% of roots with satisfactory root fillings on PA, as compared to 81% on CBCT (Tables 4 and 5). Although there was a difference of 6% between the two radiographic techniques, they both revealed that satisfactory root fillings were associated with an optimum root-canal treatment outcome.
Our findings that the percentage of complete resolution was 32% higher for satisfactory root fillings than unsatisfactory root fillings, as revealed by CBCT (Table 4), demonstrates that elimination of AP is highly quality-sensitive and depends on the adequate root canal debridement and obturation [1]. Root canal treatment should be performed with the highest possible technical standards and observation of the quality of root fillings may serve as surrogate measures of root canal treatment efficacy. In a review by Ng et al. [2], 61% of all root fillings checked in clinical studies (1922–2002) were either short or long. In the present study, overextended and short root fillings with or without voids and flush fillings with voids were observed in 51% of roots as revealed by PA and 62% by CBCT (Table 3). Although steps should be taken to improve the quality, 222 of the 234 (95%) of treated teeth were asymptomatic, indicating that tooth survival is not as quality-sensitive as the elimination of AP [29].
Overextensions
Extruded root fillings were observed on CBCT in 88 of the 268 (33%) roots (Table 1). Byström et al [4] observed a high percentage of extrusions (38%) in teeth with PA probably because of apical resorption that could enlarge the apical diameter.
In 80% of roots, the apical foramen is up to 3.8 mm shorter than the anatomic apex and is located often on the buccal or lingual aspect of the root [30]. This could explain why instruments and fillings often extruded beyond the apical foramen when they were placed within 2 mm of the radiographic apex on PA [31, 32]. Moreover, 16.3% of flush fillings on PA were diagnosed as long fillings on CBCT (Fig. 1) and 76.3% of short fillings on PA appeared as flush fillings on CBCT (Fig. 2). Many short fillings on PA were not short on CBCT also because they were no more than 3.5 mm shorter than the radiographic apex.
Detection of voids in the root canal filling
In the present study, voids were detected on CBCT scans in 102 roots, three times as many as those detected by PA (Table 2). Voids along inadequate root fillings may be invisible on two-dimensional PA because of a superposition of root-filling materials [33, 34]. Meanwhile, the buccolingual dimension of the root filling, which is only available on CBCT scans, is wider than the mesiodistal one, thus, more likely to show voids [35]. Both the superposition of material and the mesiodistal image explain the unreliable imaging of voids by PA (Fig. 3). Fourteen root fillings with voids as diagnosed by PA appeared as root fillings without voids on CBCT. It has been reported that the three-dimensional CBCT may not offer advantages for small void detection because of its low resolution features [36].
ALARA principles
To adhere the as low as reasonably achievable (ALARA) principle, a 4- × 4-cm FoV was used, which improves resolution and minimizes the radiation dose. The effective radiation dose for PA in mandibular molar region is up to 0.01 mSv, the effective radiation dose for an Accuitomo CBCT scan 4- × 4-cm FoV in the same region is 0.043 mSv [37–39]. Although PA generated relatively lower radiation dose as compared to CBCT, they may provide unreliable information [40]. In this study, the length and homogeneity of the root canal filling was misinterpreted by PA (Fig. 1, 2, and 3).
Conclusions
According to the results of this study elimination of AP depends on the high quality of the root canal treatment.
Conflict of Interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Happasalo M, Shen YA, Ricucci D. Reasons for persistent and emerging post-treatment endodontic disease. Endod Topic. 2011;18:31–50. doi: 10.1111/j.1601-1546.2011.00256.x. [DOI] [Google Scholar]
- 2.Ng Y-L, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature—part 2. Influence of clinical factors. Int Endod J. 2008;41:6–31. doi: 10.1111/j.1365-2591.2008.01484.x. [DOI] [PubMed] [Google Scholar]
- 3.Halse A, Molven O. Overextended gutta-percha and Kloroperka NO root canal fillings. Radiographic findings after 10–17 years. Acta Odont Scand. 1987;45:171–177. doi: 10.3109/00016358709098856. [DOI] [PubMed] [Google Scholar]
- 4.Byström A, Happonen R-P, Sjögren U, Sundqvist G. Healing of periapical lesions of pulpless teeth after endodontic treatment with controlled asepsis. Endod Dent Traumatol. 1987;3:58–63. doi: 10.1111/j.1600-9657.1987.tb00543.x. [DOI] [PubMed] [Google Scholar]
- 5.Peak JD. The success of endodontic treatment in general dental practice: a retrospective clinical and radiographic study. Primary Dent Care. 1994;1:9–13. [PubMed] [Google Scholar]
- 6.Friedman S, Löst C, Zarrabian M, Trope M. Evaluation of success and failure after endodontic therapy using glass–ionomer cement sealer. J Endod. 1995;21:384–390. doi: 10.1016/S0099-2399(06)80976-3. [DOI] [PubMed] [Google Scholar]
- 7.Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997;30:297–306. doi: 10.1111/j.1365-2591.1997.tb00714.x. [DOI] [PubMed] [Google Scholar]
- 8.Heling I, Bialla-Shenkman S, Turetzky A, Horwitz J, Sela J. The outcome of teeth with periapical periodontitis treated with nonsurgical endodontic treatment: a computerized morphometric study. Quintessence Int. 2001;32:397–400. [PubMed] [Google Scholar]
- 9.Hoskinson SE, Ng YL, Hoskinson AE, Moles DR, Gulabivala K. A retrospective comparison of outcome of root canal treatment using two different protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:705–15. doi: 10.1067/moe.2001.122822. [DOI] [PubMed] [Google Scholar]
- 10.Harty FJ, Parkins BJ, Wengraf AM. Success rate in root canal therapy. A retrospective study on conventional cases. Br Dent J. 1970;128:65–70. doi: 10.1038/sj.bdj.4802429. [DOI] [PubMed] [Google Scholar]
- 11.Teo CS, Chan NC, Lim SS. Success rate in endodontic therapy—a retrospective study. Part I. Dent J Malaysia. 1986;9:7–10. [PubMed] [Google Scholar]
- 12.Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16:498–504. doi: 10.1016/S0099-2399(07)80180-4. [DOI] [PubMed] [Google Scholar]
- 13.Yusuf H. The significance of the presence of foreign material periapically as a cause of failure of root treatment. Oral Surg Oral Med Oral Pathol. 1982;54:566–574. doi: 10.1016/0030-4220(82)90196-7. [DOI] [PubMed] [Google Scholar]
- 14.Wu M-K, Wesselink PR. A primary observation on the preparation and obturation of oval canals. Int Endod. 2001;34:137–41. doi: 10.1046/j.1365-2591.2001.00361.x. [DOI] [PubMed] [Google Scholar]
- 15.Gutmann JL, Lovdahl PE (2010) Problem solving in working length determination: problem solving challenges in root canal obturation. In Gutmann JL, Lovdahl PE (eds) Problem solving in endodontics, 5th edn. Elsevier, Mosby, pp. 189–194, 218–240
- 16.Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009;42:507–515. doi: 10.1111/j.1365-2591.2008.01538.x. [DOI] [PubMed] [Google Scholar]
- 17.Paula-Silva FWG, Wu M-K, Leonardo MR, da Silva LAB, Wesselink PR. Accuracy of periapical radiography and cone beam computed tomography in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod. 2009;35:1009–1012. doi: 10.1016/j.joen.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Liang YH, Li G, Wesselink PR, Wu MK. Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod. 2011;37:326–31. doi: 10.1016/j.joen.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 19.Farzaneh M, Abitbol S, Friedman S. treatment outcome in endodontics: the Toronto study. Phase 3 and 4: Orthograde retreatment. J Endod. 2004;30:627–633. doi: 10.1097/01.DON.0000129958.12388.82. [DOI] [PubMed] [Google Scholar]
- 20.Chevigny C, Dao TT, Basrani BR, et al. Treatment outcome in endodontics: the Toronto study-phases 3 and 4: orthograde retreatment. J Endod. 2008;34:131–137. doi: 10.1016/j.joen.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Ng Y-L, Mann V, Gulabivala K. A prospective study of the factors affecting outcome of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44:583–609. doi: 10.1111/j.1365-2591.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 22.Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl H-G. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:114–119. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Schneider SW. Comparison of canal preparation in straight and curved root canals. Oral Surg Oral Med Oral Pathol. 1971;32:271–275. doi: 10.1016/0030-4220(71)90230-1. [DOI] [PubMed] [Google Scholar]
- 24.Zhang YB, Zhang LF, Zhu XR, Lee AK, Chambers M, Dong L. Reducing metal artifacts in cone-beam CT images by preprocessing projection data. Int J Radiat Oncol Biol Phys. 2007;67:924–933. doi: 10.1016/j.ijrobp.2006.09.045. [DOI] [PubMed] [Google Scholar]
- 25.Ørstavik D, Qvist V, Stoltze K. A multivariate analysis of the outcome of endodontic treatment. Euro J Oral Sci. 2004;112:224–230. doi: 10.1111/j.1600-0722.2004.00122.x. [DOI] [PubMed] [Google Scholar]
- 26.Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto Study. Phase III: initial treatment. J Endod. 2006;32:299–306. doi: 10.1016/j.joen.2005.10.050. [DOI] [PubMed] [Google Scholar]
- 27.Friedman S. Prognosis of initial endodontic therapy. Endod Topic. 2002;1(2):59–88. doi: 10.1034/j.1601-1546.2002.20105.x. [DOI] [Google Scholar]
- 28.Ricucci D, Russo J, Rutberg M, Burleson JA, Spångberg LS (2011 Dec) A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112(6):825–42 [DOI] [PubMed]
- 29.Tickle M, Milsom K, Qualtrough A, Blinkhorn F, Aggarwal VR (2008) The failure rate of NHS funded molar endodontic treatment delivered in general dental practice. Br Dent J 204(5):E8 (discussion 254–255 [DOI] [PubMed]
- 30.Dummer PMM, Mc Ginn JH, Rees DG. The position and topography of the apical foramen. Int Endod J. 1984;17:192–198. doi: 10.1111/j.1365-2591.1984.tb00404.x. [DOI] [PubMed] [Google Scholar]
- 31.Elayouti A, Weiger R, Löst C. Frequency of overinstrumentation with an acceptable radiographic working length. J Endod. 2001;27:49–52. doi: 10.1097/00004770-200101000-00018. [DOI] [PubMed] [Google Scholar]
- 32.Stein TJ, Corcoran JF. Radiographic ―working length‖ revisited. Oral Surg Oral Med Oral Pathol. 1992;74:796–800. doi: 10.1016/0030-4220(92)90412-J. [DOI] [PubMed] [Google Scholar]
- 33.Kersten HW, Wesselink PR, Thoden van Velzen SK. The diagnostic reliability of the buccal radiograph after root canal filling. Int Endod J. 1987;20:20–24. doi: 10.1111/j.1365-2591.1987.tb00583.x. [DOI] [PubMed] [Google Scholar]
- 34.Van der Sluis LWM, Wu M-K, Wesselink PR. An evaluation of the quality of root fillings in mandibular incisors and maxillary and mandibular canines using different methodologies. J Dent. 2005;33:683–688. doi: 10.1016/j.jdent.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Wu M-K, Bud MG, Wesselink PR. The quality of single cone and laterally compacted gutta-percha fillings in small and curved root canals as evidenced by bidirectional radiographs and fluid transport measurements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:946–951. doi: 10.1016/j.tripleo.2009.07.046. [DOI] [PubMed] [Google Scholar]
- 36.Huybrechts B, Bud M, Bergmans L, Lambrechts P, Jacobs R. Void detection in root fillings using intraoral analogue, intraoral digital and cone beam CT images. Int Endod J. 2009;42:675–685. doi: 10.1111/j.1365-2591.2009.01566.x. [DOI] [PubMed] [Google Scholar]
- 37.Ekestubbe A, Thilander-klang A, Lith A, Gröndahl HG. Effective and organ doses from Sacnography and zonography: a comparison with periapical radiography. Dentomaxillofacial Radiol. 2004;33:87–92. doi: 10.1259/dmfr/24877187. [DOI] [PubMed] [Google Scholar]
- 38.Hirsch E, Wolf U, Heinicke F, Silva MAG. Dosimetry of the cone beam computed tomography Veraviewepocs 3D compared with the 3D Accuitomo in different fields of view. Dentomaxillofacial Radiol. 2008;37:268–273. doi: 10.1259/dmfr/23424132. [DOI] [PubMed] [Google Scholar]
- 39.Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, Cockmartin L, Bosmans H, Jacobs R, Bogaerts R, Horner K; The SEDENTEXCT Project Consortium (2010) Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol (2010 Dec 31 online publication) [DOI] [PubMed]
- 40.Wu M-K, Wesselink PR, Shemesh H, Patel S (2011) Endodontic epidemiologic investigations and clinical outcome studies with cone-beam computed tomography. J Endod (in press)


