Abstract
Background
Depression represents a growing concern among Asian Americans. This study examined whether discrimination and family dynamics are associated with depression in this population.
Methods
Weighted logistic regressions using nationally representative data on Asian American adults (N = 2095) examining associations between discrimination, negative interactions with relatives, family support, and 12-month major depressive disorder (MDD).
Results
Discrimination (odds ratio [OR] = 2.13, 95% confidence interval [CI] = 1.67, 2.71) and negative interactions with relatives (OR = 1.28, 95% CI = 1.03, 1.58) were positively associated with MDD. Family support was associated with lower MDD (OR = 0.73, 95% CI = 0.59, 0.89), and buffered lower levels of discrimination.
Discussion
Results suggest that discrimination may have negative mental health implications, and also point to the importance of family relationships for depression among Asian Americans. Findings suggest that providers may consider stress experienced at multiple ecological levels to address Asian American mental health needs.
Keywords: Asian Americans, major depressive disorder, discrimination, family relationships
INTRODUCTION
Mental health problems among Asian Americans represent an important and growing public health concern [1-5]. Studies conducted using college student samples have found that Asian American young adults have higher levels of psychological distress compared to other racial/ethnic groups [2, 3]. Another recent national study reported that U.S.-born Asian American women have particularly high rates of suicidal behaviors, with 15.9% having exhibited suicidal ideation, 7.1% having had a suicide plan, and 3.8% having attempted suicide [4]. National prevalence estimates of any lifetime and 12-month psychiatric disorder among Asian Americans are 17.3% and 9.2%, respectively; and among those with a psychiatric disorder in the past year, approximately half met criteria for a depressive disorder [5]. Although these overall estimates are lower than those for other racial/ethnic minority groups, surveillance data indicate that psychological problems among Asian Americans are a cause for concern given: (1) the presence of structural barriers against mental health treatment [6, 7]; (2) cultural stigma against mental illness [8]; as well as (3) considerable heterogeneity in the prevalence of clinically significant psychiatric disorders within the Asian American population, which are particularly high for some subgroups [5]. For example, US-born Asian American women have approximately twice the odds of meeting criteria for any lifetime or 12-month depressive disorder compared to those who are foreign-born. Although fewer statistically significant associations have been found among Asian American men, US-born men have also been found to be more likely to meet criteria for lifetime psychiatric disorders, particularly for substance use disorders, compared to those who are foreign-born [5].
Variations in mental health problems among Asian Americans may reflect differences in exposure to sources of social stress, including experiences of discrimination [9-14]. For example, a recent study on Asian Americans found that self-reported experiences of discrimination were associated with significantly higher odds of having a past year depressive disorder [10]. Furthermore, reports suggest that issues around discrimination continue to be salient in the lives of Asian Americans in contemporary contexts, including experiences of discrimination in specific domains, such as in housing and employment, as well as more chronically and routinely in everyday interactions, including instances of being treated with less courtesy or respect [14-16].
Studies have most consistently found evidence for the negative mental health implications of discrimination among racial/ethnic minority populations, including Asian Americans [16, 17]. Experiences of discrimination may impact mental health through various pathways. Discrimination may have indirect effects on well-being by increasing exposure as well as vulnerability to other demands, including those associated with socioeconomic and neighborhood-related stressors [14, 16, 18, 19]. Discrimination may also lead to systematic differences in access to health-protective resources, including mental health treatment. Recent studies on Asian Americans have found that higher levels of perceived discrimination are associated with lower mental health service use as well as lower levels of satisfaction with care [20, 21]. Discrimination may also have direct effects on mental health via the internalization of negative socio-cultural perceptions of Asians. Social evaluation and symbolic interaction theories suggest that individuals derive self-concept from the social values attached to their group membership [22, 23]. Individuals who feel that their racial group is considered less worthy may be more likely to evaluate themselves negatively. In this respect, systematic experiences of discrimination may impede positive identity formation and manifest in depressive symptoms. Accordingly, discrimination may itself constitute an additional psychosocial demand leading to poor affect.
Incorporating the Role of Family Context
Another source of psychosocial stress that is relevant to the lives of Asian Americans can occur in family contexts [24-26]. In contrast to discrimination, which is typically experienced outside of family domains, negative interactions with relatives may represent another stressor that is experienced more proximally. Furthermore, the cultural emphasis on quality of relationships in this population suggests that examining family dynamics, in addition to other forms of psychosocial stress, is critical in understanding the mental health needs of this population [27-30]. Norms around interdependence, filial piety, and family obligation are values commonly emphasized in Asian cultures, which are often described as being more collectivistic compared to more individualistic U.S. and other Western values [29-31]. For example, a recent qualitative study found that cultural expectations regarding the care of aging parents may constitute an added source of stress among Asian Americans [32]. In addition, difficulties arising from intergenerational differences in language proficiency, particularly between foreign-born parents and more linguistically assimilated and U.S.-born children, were also cited as barriers to communication within the family and as a source of conflict [32]. Family conflict resulting from competing cultural values may exert a deleterious effect on mental health in both younger as well as older Asian American groups [28-35]. A recent national study found that family conflict was a significant predictor of psychiatric morbidity among Asian Americans older than 60 years of age [34]. Another study found that perceptions of parental expectations and criticisms were strongly correlated with depressive symptoms among Asian American college students [35].
While family conflict has been found to be a strong determinant of mental well-being among Asian Americans, positive interactions with family members and other relatives can be a source of social and emotional support. Studies have found that supportive relationships may not only be beneficial for mental health, but also buffer the impact of other forms of social stress [28, 35, 36, 37]. For example, higher levels of perceived family cohesion were found to be associated with lower levels of psychological distress in a national study of Asian Americans [37]. Other studies on adolescent and young adult Asian American groups have found that greater family cohesion and parental support buffered the negative mental health effects of various forms of stress, including experiences of discrimination [28, 35]. Accordingly, more positive interactions in family contexts may serve as a source of support and be protective against social stressors.
Conceptual Framework
In this study, we examine whether discrimination more commonly experienced in broader social contexts, as well as stress experienced within the family in the form of negative interactions with relatives, are associated with major depression among Asian Americans. Based on Pearlin and colleagues’ Process of Social Stress Theory [38, 39], we posit that the mental health implications of discrimination, as a source of psychosocial stress, may be exacerbated by the presence of additional forms of stress, such as negative interactions with relatives. Furthermore, the effects of psychosocial stressors such as discrimination and family conflict on depression are dependent on the degree of available resources that may remain intact, such as support from other relatives. Accordingly, we hypothesized that both discrimination and negative interactions with relatives would be associated with greater risk of major depression, and that family support would be associated with lower risk of major depression. We also hypothesized that negative interactions with relatives would exacerbate the association between discrimination and major depression; and that support from relatives would attenuate associations between major depression and both discrimination and negative interactions with relatives.
METHODS
Sample and Procedures
The NLAAS sample has been previously described in detail [40-42]. Briefly, the NLAAS recruited a nationally representative sample of the Asian and Latino adult household population in the US. Participants were recruited using three methods: (1) core sampling using a multistage stratified area probability design; (2) high-density sampling in which Census block groups where target ethnic ancestry groups represented at least 5% of total households were oversampled (target Asian ancestry groups were: Chinese, Filipino, and Vietnamese); and (3) second-respondent sampling where another participant was selected from the household where an eligible participant was already selected. Sampling weights were constructed taking into account joint probabilities of selection into the different sampling components of the NLAAS. Participants were interviewed face-to-face or via telephone by a trained lay interviewer, and were compensated for their time. The study instrument was available in English, Cantonese, Mandarin, Spanish, Tagalog, and Vietnamese. All procedures and protocols were approved by the institutional review boards of the University of Washington, Cambridge Health Alliance, and Harvard University.
The current study is restricted to the Asian American sample of the NLAAS. A total of 2095 Asian American participants were recruited between May 2002 and November 2003. A weighted response rate of 65.3% was achieved.
Measures
12-month major depression
Presence of major depression during the past year was assessed using the Major Depression battery of a modified version of the World Mental Health Survey Initiative version of the World Health Organization Composite International Diagnostic Interview (WMH-CIDI) [43]. The WMH-CIDI is a fully structured interview that is designed to detect psychiatric disorders using Diagnostic and Statistical Manual, Version 4 (DSM-IV) criteria. Symptoms of major depression include affective, cognitive, behavioral, and somatic symptoms, including depressed mood, difficulty concentrating, and changes in sleep, appetite, and weight. Studies using earlier versions of the CIDI have reported evidence for its validity in assessing clinically significant psychiatric disorders [44, 45]. In the modified version used in the NLAAS, stem items for all DSM-IV disorders assessed in the questionnaire were asked in the beginning of the psychiatric battery in order to reduce false negative and non-response.
Discrimination
Experiences of discrimination were assessed using nine items from the Everyday Discrimination scale developed by Williams, Yu, Jackson, and Anderson [46]. The nine items assessed frequency of experiencing routine forms of unfair treatment in one’s “day-to-day life”, including experiences of being harassed or insulted, being treated with less courtesy or respect, receiving poorer service, and being perceived as dishonest or inferior. Each item ranged in response values of 0 (“never”) to 5 (“almost every day”). In the current study, we examined the mean scores of the nine items, which ranged from 0 to 5, with higher scores reflecting greater experiences of discrimination.
Family relationship variables
Support from relatives was measured as the mean of two items asking participants how much they could rely on relatives (excluding spouses, partners and those who live with them) for help when experiencing a serious problem or to talk to about worries. Responses values were 0 (not at all), 1 (a little), 2 (some), and 3 (a lot).
Negative interactions with relatives was measured as the mean of two items asking participants how often relatives or children make too many demands on them; and how often they argue with family or relatives. Response levels were 0 (never), 1 (rarely), 2 (sometimes), and 3 (often).
Socio-demographic variables
Socio-demographic variables examined in the current study included self-reported measures of: age; gender; ethnic ancestry (Chinese, Filipino, Vietnamese, or Other Asian); nativity (US- or foreign-born); marital status (married, never married, widowed, separated, or divorced); poverty level based on ratio of household income to Census 2000 poverty thresholds taking into account household composition (poor, < 1.00; near-poor, 1.00-1.99; non-poor, 2.00-3.99; and non-poor, 4.00+) [47, 48]; years of education using cut-points relevant to markers of credentials (< 12 years or less than high school; 12 years or high school; 13-15 years or some college; and 16+ years or college or more); insurance (private, public, uninsured, or other insurance); and region of residence (Northeast, Midwest, South, and West). Social desirability bias was also measured as the sum of ten items from the Marlowe and Crowne Social Desirability Scale (e.g., I have always told the truth; I never get bored) [49]. Each item is endorsed as false, with a value of zero, or true, with a value of one. Higher scores represent the presence of personality characteristics that may bias responses to sensitive questions.
Analysis
Missing data on all variables except for those measuring support and negative interactions with relatives were handled by NLAAS investigators using hot-deck imputation. Fourteen participants had missing data on support and 7 participants had missing data on negative interaction. We used multiple imputation to handle missing data on these variables, in which five imputations for missing data were generated using a Markov chain Monte Carlo (MCMC) technique assuming an arbitrary missing data pattern [50, 51]. Imputed values were truncated to fit the bounds of possible values [52, 53]. Multiple imputation takes into account the uncertainty inherent in missing values and has been shown to lead to valid statistical inferences [54]. Using only complete data in analyses did not result in substantively different conclusions.
Descriptive analyses were conducted to examine the distribution of socio-demographic characteristics in the overall sample and by presence of 12-month MDD. Logistic regression models were specified to examine the main effects of discrimination and family relationship variables on 12-month MDD. We also examined whether associations between discrimination and 12-month MDD significantly varied by family relationship variables by including the interaction between discrimination and negative interactions with relatives and the interaction between discrimination and support from relatives. In addition, we tested whether relative support might buffer negative interactions with relatives by including the corresponding interaction term.
All analyses were conducted using SAS-callable SUDAAN taking into account complex sampling design variables and weights using the PROC CROSSTAB and PROC RLOGIST procedures and MI_COUNT option to arrive at summary statistics across multiple imputations [55].
RESULTS
The weighted distribution of characteristics of participants in the NLAAS by presence of 12-month MDD is presented in Table 1. Overall, approximately 75% of participants reported experiencing any discrimination, and discrimination was more prevalent among those with 12-month MDD compared to those without. Among those with 12-month MDD, 21% of participants reported high levels of racial discrimination, compared to only 4.2% among those without 12-month MDD. We found a similar pattern for negative interactions with relatives, with higher levels of negative interaction being found among those with 12-month MDD compared to those without. In contrast, those without 12-month MDD reported higher levels of support from relatives compared to those with 12-month MDD.
Table 1.
Weighted distribution of socio-demographic characteristics of Asian Americans (N = 2095) in the National Latino and Asian American Study (NLAAS; 2002-2003) by presence of 12-month major depression.
| 12-Month MDD No |
12-Month MDD Yes |
Total | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| 12-Month Major Depression | |||
| No | 1998 (95.3) | ||
| Yes | 97 (4.7) | ||
| Discrimination | |||
| None | 541 (25.5) | 12 (7.7) | 553 (24.6) |
| Low (0.01-1.00) | 835 (43.2) | 34 (28.2) | 869 (42.5) |
| Moderate (1.01-2.00) | 547 (27.2) | 36 (43.1) | 583 (27.9) |
| High (2.01+) | 75 (4.2) | 15 (21.0) | 90 (4.9) |
| Relative Support | |||
| Low (0.00-1.00) | 598 (27.2) | 36 (32.4) | 634 (27.4) |
| Moderate (1.01-2.00) | 630 (32.7) | 29 (36.4) | 659 (32.9) |
| High (2.01+) | 770 (40.1) | 32 (31.2) | 802 (39.7) |
| Negative Relative Interaction | |||
| Low (0.00-1.00) | 1418 (69.9) | 54 (52.1) | 1472 (69.1) |
| Moderate (1.01-2.00) | 524 (26.5) | 34 (37.8) | 558 (27.0) |
| High (2.01+) | 56 (3.6) | 9 (10.1) | 65 (3.9) |
| Age | |||
| 18-34 years | 741 (38.4) | 58 (60.4) | 799 (39.5) |
| 35-49 years | 690 (32.4) | 26 (28.4) | 716 (32.2) |
| 50-64 years | 408 (18.6) | 8 (5.5) | 416 (18.0) |
| 65+ years | 159 (10.5) | 5 (5.7) | 164 (10.3) |
| Gender | |||
| Men | 956 (47.6) | 42 (45.4) | 998 (47.5) |
| Women | 1042 (52.4) | 55 (54.6) | 1097 (52.5) |
| Ethnicity | |||
| Vietnamese | 499 (13.0) | 21 (11.6) | 520 (12.9) |
| Filipino | 485 (21.7) | 23 (19.4) | 508 (21.6) |
| Chinese | 567 (28.7) | 33 (28.3) | 600 (28.7) |
| Other | 447 (36.6) | 20 (40.8) | 467 (36.8) |
| Nativity | |||
| US-born | 419 (22.6) | 35 (31.4) | 454 (23.0) |
| Foreign-born | 1579 (77.4) | 62 (68.6) | 1641 (77.0) |
| Marital Status | |||
| Married | 1347 (67.1) | 29 (29.4) | 1376 (65.3) |
| Never Married | 457 (23.3) | 55 (59.8) | 512 (25.0) |
| Widowed/Separated/Divorced | 194 (9.6) | 13 (10.8) | 207 (9.7) |
| Poverty Ratio | |||
| Poor (< 1.00) | 331 (17.0) | 26 (29.3) | 357 (17.6) |
| Near-Poor (1.00-1.99) | 198 (9.2) | 9 (8.6) | 207 (9.2) |
| Non-Poor (2.00-3.99) | 392 (19.1) | 18 (21.1) | 410 (19.2) |
| Non-Poor (4.00+) | 1077 (54.8) | 44 (41.1) | 1121 (54.1) |
| Education | |||
| Less than 12 years | 306 (15.5) | 10 (8.2) | 316 (15.1) |
| 12 years | 348 (17.2) | 24 (27.2) | 372 (17.7) |
| 13-15 years | 509 (25.4) | 20 (21.6) | 529 (25.3) |
| 16+ years | 835 (41.9) | 43 (43.0) | 878 (42.0) |
| Employment Status | |||
| Employed | 1325 (63.8) | 55 (62.8) | 1380 (63.7) |
| Unemployed | 551 (30.7) | 28 (21.2) | 579 (30.3) |
| Out of Labor Force | 122 (5.5) | 14 (16.0) | 136 (6.0) |
| Insurance | |||
| Private Insurance | 1330 (66.2) | 53 (49.6) | 1383 (65.5) |
| Public Insurance | 315 (16.5) | 17 (11.8) | 332 (16.2) |
| Uninsured | 269 (12.3) | 23 (32.7) | 292 (13.2) |
| Other | 84 (5.0) | 4 (5.9) | 88 (5.1) |
| Region | |||
| Northeast | 143 (15.3) | 9 (23.7) | 152 (15.7) |
| Midwest | 88 (9.1) | 3 (4.7) | 91 (8.9) |
| South | 141 (8.0) | 4 (5.0) | 145 (7.8) |
| West | 1626 (67.7) | 81 (66.6) | 1707 (67.6) |
| Social Desirability Bias | |||
| 0 | 408 (21.5) | 27 (30.6) | 435 (21.9) |
| 1 | 478 (22.0) | 26 (25.5) | 504 (22.1) |
| 2 | 388 (19.5) | 18 (23.0) | 406 (19.6) |
| 3+ | 724 (37.0) | 26 (21.0) | 750 (36.3) |
Weighted Logistic Regressions Predicting 12-Month MDD
Results from weighted logistic regression analyses predicting 12-month MDD are presented in Table 2. Controlling for socio-demographic characteristics, we found evidence for a significant main effect of discrimination on 12-month MDD (Model 1). Greater levels of self-reported discrimination were associated with higher odds of having 12-month MDD (OR = 2.30, 95% CI = 1.82, 2.91).
Table 2.
Weighted logistic regressions predicting 12-month major depression among Asian Americans (N = 2095) in the National Latino and Asian American Study (NLAAS; 2002-2003).
| 12-Month MDD OR (95% CI) Model 1 |
12-Month MDD OR (95% CI) Model 2 |
12-Month MDD OR (95% CI) Model 3 |
|
|---|---|---|---|
| Discrimination | 2.30 (1.82, 2.91) | 2.13 (1.67, 2.71) | 1.45 (0.89, 2.38) |
| Relative Support | 0.73 (0.59, 0.89) | 2.53 (1.32, 4.82) | |
| Negative Relative Interaction | 1.28 (1.03, 1.58) | 0.49 (0.30, 0.81) | |
| Discrimination*Relative Support | 1.54 (1.27, 1.86) | ||
| Discrimination*Negative Interaction | 0.77 (0.57, 1.05) | ||
| Negative Interaction*Support | 0.84 (0.62, 1.14) | ||
| Age | 1.00 (0.96, 1.03) | 1.00 (0.96, 1.03) | 1.00 (0.96, 1.03) |
| Gender: Women vs. Men | 1.62 (0.73, 3.57) | 1.63 (0.75, 3.56) | 1.73 (0.84, 3.58) |
| Ethnicity (Ref: Chinese) | |||
| Vietnamese | 0.87 (0.24, 3.08) | 0.81 (0.22, 2.93) | 0.82 (0.25, 2.62) |
| Filipino | 0.68 (0.37, 1.27) | 0.72 (0.39, 1.32) | 0.73 (0.39, 1.37) |
| Other | 0.83 (0.39, 1.75) | 0.90 (0.42, 1.93) | 0.90 (0.42, 1.91) |
| Nativity: Foreign- vs. US-born | 1.14 (0.62, 2.10) | 1.04 (0.55, 1.95) | 1.14 (0.59, 2.19) |
| Marital Status (Ref: Married) | |||
| Never Married | 3.21 (1.32, 7.81) | 3.32 (1.41, 7.83) | 3.35 (1.44, 7.80) |
| Widowed, Separated, Divorced | 2.81 (1.10, 7.18) | 2.80 (1.14, 6.86) | 2.86 (1.16, 7.03) |
| Poverty Level (Ref: Poor, < 1.00) | |||
| Near Poor (1.00-1.99) | 0.91 (0.33, 2.51) | 0.85 (0.31, 2.29) | 0.79 (0.29, 2.19) |
| Non-Poor (2.00-3.99) | 1.25 (0.61, 2.55) | 1.21 (0.58, 2.53) | 1.16 (0.57, 2.34) |
| Non-Poor (4.00+) | 0.76 (0.37, 1.53) | 0.80 (0.41, 1.60) | 0.72 (0.36, 1.46) |
| Education (ref: < 12 years) | |||
| 12 years | 1.70 (0.59, 4.89) | 1.64 (0.53, 5.09) | 2.07 (0.73, 5.90) |
| 13-15 years | 0.83 (0.23, 3.00) | 0.79 (0.20, 3.12) | 0.86 (0.23, 3.23) |
| 16+ years | 1.32 (0.46, 3.74) | 1.28 (0.42, 3.93) | 1.43 (0.47, 4.30) |
| Employment (Ref: Employed) | |||
| Unemployed | 0.62 (0.29, 1.33) | 0.61 (0.28, 1.34) | 0.69 (0.33, 1.42) |
| Out of Labor Force | 2.19 (1.04, 4.59) | 2.14 (1.03, 4.44) | 2.03 (0.93, 4.43) |
| Insurance (Ref: Private Insurance) | |||
| Public Insurance | 1.14 (0.45, 2.89) | 1.08 (0.45, 2.61) | 1.18 (0.51, 2.75) |
| Uninsured | 2.24 (1.23, 4.10) | 2.29 (1.31, 3.99) | 2.24 (1.23, 2.08) |
| Other Insurance | 0.87 (0.28, 2.76) | 0.87 (0.26, 2.92) | 0.81 (0.23, 2.93) |
| Region (Ref: Northeast) | |||
| Midwest | 0.48 (0.16, 1.45) | 0.45 (0.14, 1.44) | 0.50 (0.15, 1.62) |
| South | 0.46 (0.11, 1.96) | 0.49 (0.11, 2.14) | 0.44 (0.12, 1.68) |
| West | 0.77 (0.32, 1.85) | 0.81 (0.33, 2.01) | 0.82 (0.36, 1.89) |
| Social Desirability Bias | 0.88 (0.75, 1.04) | 0.88 (0.74, 1.04) | 0.89 (0.74, 1.06) |
In Model 2, we added relative support and negative interactions with relatives to the model. Greater support from relatives was associated with significantly lower odds of 12-month MDD (OR = 0.73, 95% CI = 0.59, 0.89). In addition, higher levels of negative interactions with relatives was associated with significantly higher odds of 12-month MDD (OR = 1.28, 95% CI = 1.03, 1.58). Self-reported racial discrimination continued to significantly predict 12-month MDD in this model.
We examined whether relative support might serve as a buffer against discrimination and if negative interaction may exacerbate the negative effects of discrimination on 12-month MDD by adding the corresponding interaction terms to the model. We concurrently examined whether relative support might buffer negative interactions with relatives. We added these three interaction terms to the model as a single block (Model 3). Adding interaction terms individually did not lead to substantively different results.
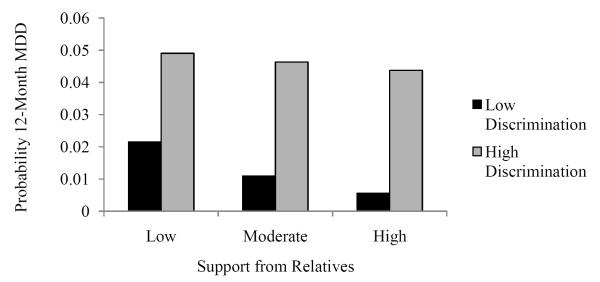
We found evidence for a significant interaction between discrimination and relative support (F = 21.7; 1 df, p < 0.001). To illustrate this relationship, we constructed predicted probabilities of 12-month MDD by discrimination and relative support (Figure 1) [56]. We chose values of 0.50 and 2.50 to represent low and high discrimination, respectively (reflecting the midpoints in experiencing each of the nine items measuring discrimination between “none” and “less than once a year”; and between “a few times a year” and “a few times a month”); and chose mid-points of a priori defined categories of low and high emotional support. Choosing alternative values for discrimination and relative support did not significantly alter the shape of plots. Mean values of all remaining covariates were chosen in order to illustrate relationships between racial discrimination and emotional support for the average participant.
Figure 1.
Predicted probability of 12-month major depression by racial discrimination and relative support among Asian Americans (N = 2095) in the National Latino and Asian American Study (NLAAS; 2002-2003).
Results indicated that higher levels of support were associated with lower probabilities of 12-month MDD among those who reported lower levels of discrimination. However, among those who reported higher levels of discrimination, relative support had little association with the probability of 12-month MDD.
DISCUSSION
Results from analyses are consistent with those of prior studies suggesting that discrimination is associated with worse mental health outcomes among Asian Americans [9-11, 37]. We extend previous research in this area by examining the role that potential stressors and protective factors experienced more proximally in the family context may have in moderating the association between discrimination and 12-month MDD.
We found that along with self-reported discrimination, higher levels of negative interactions with relatives were associated with greater odds of 12-month MDD. These negative interactions may arise from competing cultural demands and expectations, which have been found to negatively impact mental health [29-31, 57, 58]. Although we did not find that negative interactions with relatives exacerbated the effect of discrimination, we did find an additive effect, with higher levels of discrimination and negative relative interactions concurrently being associated with higher risk of 12-month MDD. Our findings suggest that self-reports of discrimination in tandem with high levels of family conflict may be associated with greater risk of 12-month MDD.
In general, studies have found that family and other forms of social support are protective against poor mental health [30, 36, 59]. Consistent with these studies, we found that having supportive interactions with relatives was associated with significantly lower risk of 12-month MDD. This finding is in accordance with prior observations that improving family relationships may be particularly important in enhancing the mental health of Asian Americans [27-30, 60]. While studies have found that social support may also buffer the effect of discrimination on poor health [28, 36, 61, 62], we found that support from relatives only mitigated lower levels of discrimination. One explanation for this finding may be that those who report greater levels of discrimination are exposed to a high level of stress that is not necessarily abated by supportive relationships. Accordingly, the buffering effects of support from relatives may be limited to only lower levels of social stress. Another explanation may be that relatives, particularly those in earlier generations who have not experienced racial discrimination in their country of origin, may not recognize discrimination or be able to provide later generations with the support to cope with such stressors.
A novelty of the NLAAS is the nationally representative nature of the data, which potentially increases the generalizability of our findings. However, a caveat to the NLAAS study is that the survey was not available in “other” Asian languages, possibly leading to lower response rates of those belonging to national ancestry groups that were not explicitly targeted; and in particular those with lower levels of English proficiency [63]. Differential patterns in participation by ethnicity may have impacted our effect estimates. Along these lines, an additional limitation to our results is that we did not disaggregate our analyses between specific Asian national origin groups or conduct analyses stratified by gender or nativity due to the relatively small prevalence of 12-month MDD in the population. It is possible that the associations that we reported could be differ between Asian American subgroups.
The cross-sectional nature of the data and retrospective self-report of our measures limit inferences regarding the causal direction of the associations that we found. For example, it is possible that high levels of depression could result in greater frequency of negative interactions or lower levels of perceived support from relatives. Depression may also lead to greater perceptions of being discriminated against. Furthermore, although our measure of MDD is an improvement over lifetime measures of psychiatric morbidity, because presence of MDD was assessed over the past year timeframe, it is uncertain whether participants who were positive on our outcome currently met MDD criteria, Accordingly, causal inferences are limited in using cross-sectional and largely retrospective observational data. However, our findings may inform future longitudinal studies in order to deduce the temporal sequence between our hypothesized exposures and the onset of mental illnesses.
CONCLUSIONS
Despite these limitations, the results of our study are consistent with prior research on the mental health implications of discrimination as well as research on family dynamics among Asian Americans. Our study bridges research in these areas by examining the interactive effects of psychosocial stress experienced in these domains. Results suggest that mental health service providers should be concerned with psychosocial stressors experienced in broader social contexts as well as within the family among Asian Americans. Our findings suggest that routine and chronic forms of discrimination experienced in everyday interactions may have a detrimental impact on psychological well-being in this population. In addition, while having supportive relationships may be protective against mental health problems among Asian Americans, its effectiveness as a buffer for discrimination as well as conflict within the family may be limited. Having an ecological understanding of stress experienced at multiple levels may help mental health providers and public health practitioners appropriately address the mental health needs of Asian Americans.
ACKNOWLEDGMENTS
The National Latino and Asian American Study is funded by the National Institute of Mental Health (NIMH U01 MH62209 and U01 MH62207) with additional support from the Office of Behavioral and Social Science Research and the Substance Abuse and Mental Health Services Administration.
References
- 1.Sue S, Chu JY. The mental health of ethnic minority groups: challenges posed by the Supplement to the Surgeon General’s Report on Mental Health. Cult Med Psychiatry. 2003;27:447–65. doi: 10.1023/b:medi.0000005483.80655.15. [DOI] [PubMed] [Google Scholar]
- 2.Kearney LK, Draper M, Baron A. Counseling utilization by ethnic minority college students. Cultur Divers Ethnic Minor Psychol. 2005;11:272–85. doi: 10.1037/1099-9809.11.3.272. [DOI] [PubMed] [Google Scholar]
- 3.Young CB, Fang DZ, Zisook S. Depression in Asian-American and Caucasian undergraduate students. J Affect Disord. 2010;125:379–82. doi: 10.1016/j.jad.2010.02.124. [DOI] [PubMed] [Google Scholar]
- 4.Duldulao AA, Takeuchi DT, Hong S. Correlates of suicidal behaviors among Asian Americans. Arch Suicide Res. 2009;13:277–90. doi: 10.1080/13811110903044567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Walton E, Sue S, Alegría M. Immigration-related factors and mental disorders among Asian Americans. Am J Public Health. 2007;97:84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barreto RM, Segal SP. Use of mental health services by Asian Americans. Psychiatr Serv. 2005;56:746–8. doi: 10.1176/appi.ps.56.6.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spencer MS, Chen J, Gee GC, Fabian CG, Takeuchi DT. Discrimination and mental health-related service use in a national study of Asian Americans. Am J Public Health. 2010;100:2410–7. doi: 10.2105/AJPH.2009.176321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Georg Hsu LK, Wan YM, Chang H, Summergrad P, Tsang BY, Chen H. Stigma of depression is more severe in Chinese Americans than Caucasian Americans. Psychiatry. 2009;71:210–8. doi: 10.1521/psyc.2008.71.3.210. [DOI] [PubMed] [Google Scholar]
- 9.Noh S, Kaspar V, Wickrama KA. Overt and subtle racial discrimination and mental health: preliminary findings for Korean immigrants. Am J Public Health. 2007;97:1269–74. doi: 10.2105/AJPH.2005.085316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Soc Sci Med. 2007;64:1984–96. doi: 10.1016/j.socscimed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang WC, Goto S. The impact of perceived racial discrimination on the mental health of Asian American and Latino college Students. Cultur Divers Ethnic Minor Psychol. 2008;14:326–35. doi: 10.1037/1099-9809.14.4.326. [DOI] [PubMed] [Google Scholar]
- 12.Cheng JK, Fancher TL, Ratanasen M, Conner KR, Duberstein PR, Sue S, Takeuchi D. Lifetime suicidal ideation and suicide attempts in Asian Americans. Asian Am J Psychol. 2010;1:18–30. doi: 10.1037/a0018799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juang LP, Alvarez AA. Discrimination and adjustment among Chinese American adolescents: family conflict and family cohesion as vulnerability and protective factors. Am J Public Health. 2010;100:2403–9. doi: 10.2105/AJPH.2009.185959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–23. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sue DW, Bucceri J, Lin AI, Nadal KL, Torino GC. Racial microaggressions and the Asian American experience. Cultur Divers Ethnic Minor Psychol. 2007;13:72–81. doi: 10.1037/1099-9809.13.1.72. [DOI] [PubMed] [Google Scholar]
- 16.Gee GC, Ro A, Shariff-Marco S, Chae D. Discrimination and health among Asian Americans: evidence, assessment, and direction for future research. Epidemiol Rev. 2009;31:130–51. doi: 10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93:215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spencer MS, Chen J. Effect of discrimination on mental health service utilization among Chinese Americas. Am J Public Health. 2004;64:809–14. doi: 10.2105/ajph.94.5.809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang B, Appel H, Ai AL. The effects of discrimination and acculturation to service seeking satisfaction for Latina and Asian American women: implications of mental health professions. Soc Work Public Health. 2011;26:46–59. doi: 10.1080/10911350903341077. [DOI] [PubMed] [Google Scholar]
- 22.Pettigrew TF. Social evaluation theory: convergences and applications. In: Levine D, editor. Nebraska Symposium on Motivation. University of Nebraska Press; Lincoln, NE: 1967. pp. 241–304. [Google Scholar]
- 23.Mead GH. Mind, Self, and Society. University of Chicago Press; Chicago: 1934. [Google Scholar]
- 24.Zhou M. Growing up American: the challenge confronting immigrant children and children of immigrants. Ann Rev Sociol. 1997;23:63–95. [Google Scholar]
- 25.Oyserman D, Sakamoto I. Being Asian American: identity, cultural constructs, and stereotype perception. J App Behav Sci. 1997;33:435–53. [Google Scholar]
- 26.Kwak K. Adolescents and their parents: a review of intergenerational family relations for immigrant and non-immigrant families. Hum Dev. 2003;46:115–36. [Google Scholar]
- 27.Fuligni AJ, Tseng V, Lam M. Attitudes toward family obligations among American adolescents with Asian, Latin American, and European backgrounds. Child Dev. 1999;70:1030–44. [Google Scholar]
- 28.Juang LP, Alvarez AA. Discrimination and adjustment among Chinese American adolescents: family conflict and cohesion as vulnerability and protective factors. Am J Public Health. 2010;100:2403–9. doi: 10.2105/AJPH.2009.185959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juan LP, Syed M, Takagi M. Intergenerational discrepancies of parental control among Chinese American families: links to family conflict and adolescent depressive symptoms. J Adolesc. 2007;30:965–75. doi: 10.1016/j.adolescence.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Kuo BC, Chong V, Joseph J. Depression and its psychosocial correlates among older Asian immigrants in North America: a critical review of two decades’ research. J Aging Health. 2008;20:615–52. doi: 10.1177/0898264308321001. [DOI] [PubMed] [Google Scholar]
- 31.Park IJ, Kim PY, Cheung RY, Kim M. The role of culture, family processes, and anger regulation in Korean American adolescents’ adjustment problems. Am J Orthopsychiatry. 2010;28:258–66. doi: 10.1111/j.1939-0025.2010.01029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hwang WC, Wood JJ. Acculturative family distancing: links with self-reported symptomatology among Asian Americans and Latinos. Child Psychiatry Hum Dev. 2009;40:123–38. doi: 10.1007/s10578-008-0115-8. [DOI] [PubMed] [Google Scholar]
- 33.Lee S, Juon H-S, Martinez G, Hsu CE, Robinson S, Bawa J, Ma GX. Model minority at risk: expressed needs of mental health by Asian American young adults. J Community Health. 2009;34:144–52. doi: 10.1007/s10900-008-9137-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim J, Choi NG. Twelve-month prevalence of DSM-IV mental disorders among older Asian Americans: comparison with younger groups. Aging Ment Health. 2010;14:90–9. doi: 10.1080/13607860903046461. [DOI] [PubMed] [Google Scholar]
- 35.Yoon J, Lau AS. Maladaptive perfectionism and depressive symptoms among Asian American college students: contributions of interdependence and parental relations. Cultur Divers Ethnic Minor Psychol. 2008;14:92–101. doi: 10.1037/1099-9809.14.2.92. [DOI] [PubMed] [Google Scholar]
- 36.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. Am J Public Health. 2003;93:232–8. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yip T, Gee GC, Takuechi DT. Racial discrimination and psychological distress: the impact of ethnic identity and age among immigrant and United States-born Asian adults. Dev Psychol. 2008;44:787–800. doi: 10.1037/0012-1649.44.3.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- 39.Pearlin LI, Mullan JT, Semple SL, Skaff MM. Caregiving and the stress process: an overview of concepts and measures. Gerontologist. 1990;30:583–94. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 40.Pennell BE, Bowers A, Carr D, Chardoul S, Cheung GQ, Dinkelmann K, Gebler N, Hansen SE, Pennell S, Torres M. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. Int J Methods Psychiatr Res. 2004;13:241–69. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) Int J Methods Psychiatr Res. 2004;13:221–40. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng XL, Vega W, Zane N, Vila D, Woo M, Vera M, Guarnaccia P, Aguilar-Gaxiola S, Sue S, Escobar J, Lin KM, Gong F. Considering context, place and culture: the National Latino and Asian American Study. Int J Methods Psychiatr Res. 2004;13:208–20. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jordanova, Wickramesinghe C, Gerada C, Prince M. Validation of two survey diagnostic interview among primary care attendees: a comparison of CIS-R and CIDI with SCAN ICD-10 diagnostic categories. Psychol Med. 2004;34:1013–24. doi: 10.1017/s0033291703001727. [DOI] [PubMed] [Google Scholar]
- 45.Kessler RC, Wittchen H-U, Abelson JM, Mcgonagle K, Schwarz N, Kendler KS, Knäuper B, Zhao S. Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US National Comorbidity Survey (NCS) Int J Methods Psychiatric Res. 1998;7:33–55. [Google Scholar]
- 46.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J Health Psychol. 1997;2:335–31. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 47.US Census Bureau . Poverty in the United States: 2000. US Government Printing Office; Washington, DC: 2001. [Google Scholar]
- 48.National Center for Health Statistics . Health, United States, 1998 with Socioeconomic and Health Chartbook. US Government Printing Office; Hyattsville, MD: 1998. [Google Scholar]
- 49.Marlowe D, Crowne DP. Social desirability and response to perceived situational demands. J Consult Psychol. 1961;25:109–15. doi: 10.1037/h0041627. [DOI] [PubMed] [Google Scholar]
- 50.Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley and Sons; New York: 1987. [Google Scholar]
- 51.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Meth. 2002;7:147–77. [PubMed] [Google Scholar]
- 52.Allison PD. Multiple imputation for missing data—a cautionary tale. Sociol Meth Res. 2000;28:301–9. [Google Scholar]
- 53.Horton NJ, Lipsitz SF, Parzen M. A potential for bias when rounding in multiple imputation. Am Stat. 2003;57:229–32. [Google Scholar]
- 54.Schafer JL. Analysis of Incomplete Multivariate Data. Chapman and Hall; New York: 1997. [Google Scholar]
- 55.RTI International . SUDAAN. version 9.0.0 RTI; Research Triangle Park, NC: 2004. [Google Scholar]
- 56.Jaccard J. Interaction Effects in Logistic Regression. Sage Publication; Thousand Oaks, CA: 2001. [Google Scholar]
- 57.Yeh KH, Bedford O. A test of the dual filial piety model. Asian J Soc Psychol. 2003;6:215–28. [Google Scholar]
- 58.Youn G, Knight BG, Jeong H-S, Benton D. Differences in familism, values, and caregiving outcomes among Korean, Korean American, and White American dementia caregivers. Psychol Aging. 1999;14:355–64. doi: 10.1037//0882-7974.14.3.355. [DOI] [PubMed] [Google Scholar]
- 59.Han H-R, Kim M, Lee H, Pistulk G, Kim KB. Correlates of depression in the Korean American elderly: focusing on personal resources of social support. J Cross Cult Gerontol. 2007;22:115–27. doi: 10.1007/s10823-006-9022-2. [DOI] [PubMed] [Google Scholar]
- 60.Adlwin C, Greenberger E. Cultural differences in predictors of depression. Am J Commun Psychol. 1987;15:789–813. doi: 10.1007/BF00919803. [DOI] [PubMed] [Google Scholar]
- 61.Gee GC, Chen J, Spencer MS, See S, Kuester OA, Tran D, Takeuchi D. Social support as a buffer for perceived unfair treatment among Filipino Americans: differences between San Francisco and Honolulu. Am J Public Health. 2006;96:677–84. doi: 10.2105/AJPH.2004.060442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yoshikawa H, Wilson PA, Chae DH, Cheng JF. Do family and friendship networks protect against the influence of discrimination on mental health and HIV risk among Asian and Pacific Islander gay men? AIDS Educ Prev. 2004;16:84–100. doi: 10.1521/aeap.16.1.84.27719. [DOI] [PubMed] [Google Scholar]
- 63.Chae DH, Gavin AR, Takeuchi DT. Smoking prevalence among Asian Americans: findings from the National Latino and Asian American Study (NLAAS) Public Health Rep. 2006;121:755–63. doi: 10.1177/003335490612100616. [DOI] [PMC free article] [PubMed] [Google Scholar]