Abstract
Objectives
Empirical findings on racial discrimination and hypertension risk have been inconsistent. Some studies have found no association between self-reported experiences of discrimination and cardiovascular health outcomes while others have found moderated or curvilinear relationships. The current cross-sectional study examined whether the association between racial discrimination and hypertension is moderated by implicit racial bias among African American midlife men.
Methods
This study examined data on 91 African American men between 30-50 years of age. Primary variables were self-reported experiences of racial discrimination; and unconscious racial bias as measured by the Black-White Implicit Association Test. Modified Poisson regression models were specified examining hypertension, defined as mean resting systolic ≥ 140 mm Hg or diastolic ≥ 90 mm Hg; or self-reported history of cardiovascular medication use with a physician diagnosis of hypertension.
Results
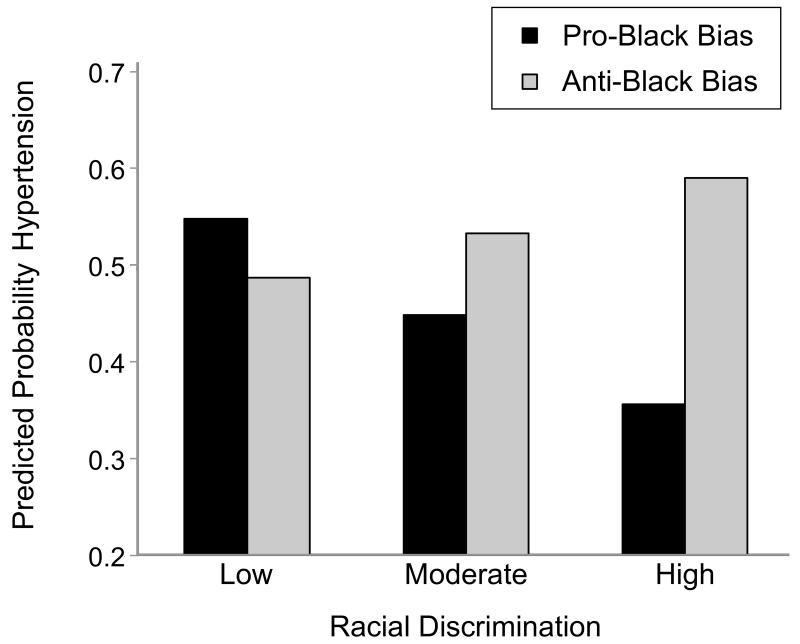
No main effects for discrimination or implicit racial bias were found, but the interaction of the two variables was significantly related to hypertension (χ2 = 4.89, 1 df, p < 0.05). Among participants with an implicit anti-Black bias, more frequent reports of discrimination were associated with a higher probability of hypertension, while among those with an implicit pro-Black bias, it was associated with lower risk.
Conclusions
The combination of experiencing racial discrimination and holding an anti-Black bias may have particularly detrimental consequences for hypertension among African American midlife men, while holding an implicit pro-Black bias may buffer the effects of racial discrimination. Efforts to address both internalized racial bias and racial discrimination may lower cardiovascular risk in this population.
Keywords: African American men, hypertension, racial discrimination, implicit racial bias
Racial disparities in cardiovascular health between African American and White men are well-documented and apparent even in younger adult populations (1-3). There is increasing evidence that social stressors and psychosocial challenges that African American men experience lead to accelerated declines in cardiovascular health (4, 5). Interpersonal experiences of racial discrimination constitute a particularly distinct stressor, which may impact cardiovascular health indirectly through psychological and behavioral responses, as well as directly via effects on biological systems engaged in the stress response (6, 7). Discrimination has been associated with biological markers of stress, including measures of systemic inflammation, and other measures of cardiovascular functioning (8-11). Experimentally manipulated discrimination in particular has been found to be associated with cardiovascular reactivity (11-12).
However, findings on hypertension and self-reports of racial discrimination have been inconsistent, with some studies finding no association; and still others finding inverse or U-shaped relationships in some subgroups, with those reporting no racial discrimination having the highest risk (13-15). To explain these counterintuitive findings researchers have drawn from racial identity frameworks, which suggest that racial self-concept impacts whether negative experiences are interpreted as being racially motivated (15, 16). Attributions to group-based discrimination may in fact be protective by deflecting self-blame or via the minimization of personal attributes as causes of negative experiences; and may also reflect a greater awareness of the systematic nature of racism (17). Furthermore, racial discrimination may have particularly detrimental consequences among those holding negative beliefs about their own racial group, while having more positive in-group racial attitudes may serve as a potential buffer against race-related stressors (15, 18-20). Along these lines, the relationship between racial discrimination and hypertension may depend on whether individuals have internalized negative perceptions of their own racial group.
This study explores the role of implicit in-group racial bias, measured using the Black-White Implicit Association Test (IAT), in moderating the association between racial discrimination and hypertension among African American midlife men. The IAT is an experimental technique that measures the speed with which participants match images of African American and White faces; and positively (“good”) and negatively (“bad”) valenced words with their respective categories (21). Faster categorizations under different conditions are considered to be more closely associated with representations in memory, which is posited to reflect unconscious racial bias. National studies have found that 70% of people in the U.S. display an implicit anti-Black bias, including almost half of African Americans, making on average faster categorizations of faces and words when mapping the “African American/Bad” or “White/Good” condition in comparison to the “African American/Good” or “White/Bad” condition (22, 23). Among African Americans, holding an implicit anti-Black bias may represent the internalization of broader negative societal attitudes about Blacks (24). The IAT may be a more valid measure of in-group racial bias compared to explicit reports of racial group evaluation given that it is not susceptible to environmental or other extraneous factors; and because performance is not influenced by the provision of socially desirable responses (22, 23).
We hypothesized a significant interaction between racial discrimination and implicit racial bias in relation to hypertension, with the greatest risk of hypertension among those reporting high racial discrimination and exhibiting an implicit anti-Black bias, in comparison to those reporting low racial discrimination and/or holding an implicit pro-Black bias.
Methods
Study Design and Procedures
Data are from the Bay Area Heart Health Study (BAHHS), a cross-sectional observational study of African American midlife men. Ninety-five African American men between 30-50 years of age in the San Francisco Bay Area were recruited between February 2010 and May 2010. Eligibility criteria included: (1) self-identification as an African American man between 30-50 years of age; (2) U.S. nativity and parental U.S. nativity; (3) absence of serious illness (e.g., cancer, HIV/AIDS, tuberculosis, hepatitis); and (4) ability to read, write, and understand English.
Participants were a convenience sample recruited from socioeconomically diverse neighborhoods and at venues where the population was most accessible, including churches, barbershops, and community events; through self-referral from posted advertisements; and via word-of-mouth. Data were collected by trained lay research staff in a non-clinical setting (university or church room). Study procedures were: (1) interviewer-administered questionnaire assessing basic demographic characteristics; (2) minimally invasive physical exam during which time blood pressure and anthropometric data were collected; and (3) computer-assisted self-administered questionnaire including psychological, socioeconomic, and behavioral measures. Participants were compensated with a $70 gift card. All study protocols were approved by the University of California, San Francisco Committee on Human Research.
Measures
Hypertension
Hypertension was defined as mean resting systolic ≥ 140 mm Hg or diastolic ≥ 90 mm Hg; or self-reported history of cardiovascular medication use with a physician diagnosis of hypertension (25). Four consecutive measures of resting blood pressure using an automated blood pressure device were obtained; the first reading was discarded, and the average of the subsequent three readings was used to derive mean systolic and diastolic blood pressure. Several steps were taken to improve the fidelity of blood pressure measurements: (1) discarding the first blood pressure reading and having a lay research assistant measure blood pressure in a non-clinical setting to diminish “white-coat” and “isolated office” hypertension; (2) using the appropriate cuff size based on size of the upper arm; and (3) training of the research assistant on consistent positioning of the participant (upright seating with the lower arm rested on a table), and proper cuff placement (26). Blood pressure measurements were taken subsequent to providing the study description, obtaining informed consent, and administering the non-sensitive demographic questionnaire (approximately 15 minutes) in order to increase familiarity with the research assistant and the study setting to decrease cardiovascular reactivity.
Racial discrimination
Racial discrimination was assessed using the Everyday Discrimination Scale, a widely used and validated instrument (27, 28). Instructions were modified to assess experiences of discrimination specifically attributed to “race, ethnicity, or color”. The scale consists of 10 items about frequency of routine experiences of discrimination in their “day-to-day life”, such as being treated with less courtesy or respect, receiving poorer service, being perceived as less smart, dishonest, or not as good as others. Response options ranged from 0 (never) to 5 (almost everyday). We calculated the mean across items, with higher values representing greater experiences of discrimination. (α = 0.91).
Implicit racial bias
The IAT was administered on computer via Inquisit software (21-23). Values range from −1 to +1 with scores less than 0 reflecting a pro-Black bias, and those greater than 0 reflecting an anti-Black bias. We dichotomized the IAT and classified participants as having an implicit anti-Black or pro-Black bias given its bimodal distribution centered at 0.
Sociodemographic characteristics
We examined several sociodemographic variables: continuous measures of age in years, ratio of household income to the poverty threshold based on family size, and social desirability response bias measured using the short version of the Marlowe-Crowne Social Desirability Scale (29); and categorical measures of relationship status (married or unmarried), education (high school or less vs. more than high school), employment status (employed or unemployed), and health insurance (any vs. none). We also examined several behavioral and physical health factors as potential covariates, including: waist-to-hip ratio calculated as waist divided by hip circumference in inches; smoking status (ever, former, and never smoker); and the number of other health conditions modified from a checklist of common diseases (e.g., diabetes, cancer, renal disease) (30).
Data Analysis
For 15 participants missing data on one of the items measuring racial discrimination, we used the within-subject mean of the remaining nine items to substitute missing values. Mean substitution for multi-item scales with less than 20% missing data has little effect on the validity of statistical inferences (31). Four participants with missing data on poverty and education were excluded from analyses. Analyses using multiple imputation methods to handle missing values for poverty and education did not lead to substantively different results.
Modified Poisson regression models using robust error variances were used to estimate risk ratios and 95% confidence intervals (32). The use of this technique has been recommended in modeling common binary outcomes as a more appropriate approximation of relative risk (33). Logistic regression analyses did not result in substantively different conclusions regarding the significance of variables.
We included conceptually important covariates as well as those significantly associated with hypertension or that showed evidence of confounding. Our final model consisted of the following covariates: age, relationship status, poverty ratio, health insurance status, waist-hip ratio, and chronic conditions. Multivariable models were specified with racial discrimination, implicit racial bias, and the interaction between racial discrimination and implicit racial bias as the primary variables. Analyses were conducted using SAS Version 9.3 statistical software.
Results
Forty-two participants representing 46% of our sample were classified as having hypertension. Additional sociodemographic characteristics in the total sample and by current hypertension status are presented in Table 1.
Table 1.
Characteristics of African American men in the Bay Area Heart Health Study (n = 91).
| Hypertension | ||||
|---|---|---|---|---|
| Total | No | Yes | ||
|
|
||||
| Hypertension, n (%) | No | 49 (53.9) | ||
| Yes | 42 (46.2) | |||
| Racial Discrimination | Mean (SD) | 2.0 (1.2) | 2.1 (1.2) | 2.0 (1.2) |
| Implicit Racial Bias, n (%) | Pro-Black | 57 (62.6) | 33 (57.9) | 24 (42.1) |
| Anti-Black | 34 (37.4) | 16 (47.1) | 18 (52.9) | |
| Age | Mean (SD) | 43.9 (5.8) | 43.4 (5.7) | 44.5 (5.8) |
| Relationship Status, n (%) * | Married | 22 (24.2) | 17 (77.3) | 5 (22.7) |
| Unmarried | 69 (75.8) | 32 (46.4) | 37 (53.6) | |
| Poverty Ratio *** | Mean (SD) | 2.0 (2.3) | 2.8 (2.8) | 1.2 (1.0) |
| Health Insurance, n (%) | Insured | 49 (53.8) | 30 (61.2) | 19 (38.8) |
| Uninsured | 42 (46.2) | 19 (45.2) | 23 (54.8) | |
| Waist-Hip Ratio | Mean (SD) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) |
| Chronic Conditions | Mean (SD) | 0.9 (1.4) | 0.7 (0.9) | 1.1 (1.8) |
Note:
p < 0.05
p < 0.01
p < 0.001
In multivariable regression models (Table 2), there were no main associations between racial discrimination, implicit racial bias, and hypertension. Our main hypothesis was that the association between racial discrimination and hypertension would be significantly different between those with a pro-Black vs. anti-Black bias. This was tested by entering the corresponding interaction term, which was significant at the p = 0.027 level (χ2 = 4.89, 1 df).
Table 2.
Relative risk (RR) estimated by Poisson regression with robust error variances examining hypertension among African American men in the Bay Area Heart Health Study (n = 91).
| Model 1 RR (95% CI) |
Model 2 RR (95% CI) |
Model 3 RR (95% CI) |
|
|---|---|---|---|
|
|
|||
| Racial Discrimination | 0.84 (0.69, 1.02) | 0.85 (0.70, 1.04) | 0.92 (0.75, 1.13) |
| Anti-Black Bias vs. Pro- Black Bias | 1.21 (0.85, 1.74) | 0.55 (0.26, 1.16) | |
| Discrimination × Racial Bias | 1.51 (1.05, 2.19) | ||
| Age | 1.00 (0.96, 1.04) | 1.00 (0.96, 1.04) | 1.00 (0.96, 1.04) |
| Unmarried vs. Married | 2.58 (1.35, 4.92) | 2.65 (1.42, 4.95) | 2.66 (1.42, 4.97) |
| Poverty Ratio | 0.71 (0.60, 0.84) | 0.71 (0.60, 0.84) | 0.69 (0.58, 0.81) |
| Uninsured vs. Insured | 1.03 (0.70, 1.51) | 1.03 (0.71, 1.51) | 0.98 (0.68, 1.43) |
| Waist-Hip Ratio × 10 | 1.67 (1.25, 2.24) | 1.66 (1.24, 2.21) | 1.60 (1.21, 213) |
| Chronic Conditions | 1.05 (0.92, 1.19) | 1.05 (0.93, 1.18) | 1.08 (0.96, 1.23) |
Note: Waist-hip ratio was multiplied by a factor of 10 so that results are interpreted as the change in risk of hypertension per 0.10 increase.
We calculated predicted probabilities from the model with the interaction between racial discrimination and implicit racial bias, choosing values of one standard deviation below the mean, the mean value, and one standard deviation above the mean value for racial discrimination to represent “low”, “moderate”, and “high” levels of racial discrimination, respectively. We set mean values of all covariates in order to demonstrate relationships for the average participant (34). There was a positive relationship between racial discrimination and hypertension risk among participants with an implicit anti-Black bias, but a negative relationship among those with an implicit pro-Black bias.
Discussion
This is the first study incorporating the role of implicit racial bias in examining the relationship between racial discrimination and hypertension. We found the highest risk of hypertension among African American midlife men with an implicit anti-Black bias and who reported higher levels of racial discrimination.
Findings from our study suggest the need to jointly consider both interpersonal experiences of racial discrimination and in-group racial bias as factors associated with hypertension in this population. Those with an implicit bias against their own racial group may be more likely to attribute negative experiences to internal or personal causes, and may also be particularly vulnerable to the impact of stigmatizing experiences (19, 35). Self-blame associated with having an anti-Black bias could exacerbate stress responses to racial discrimination and have detrimental consequences for cardiovascular health among African American midlife men (18). In contrast, recognizing and reporting racial discrimination may be protective among those having a pro-Black bias and buffer against the negative impact of racial discrimination (13). Some research has also posited that attributing negative life experiences to external causes, such as racial discrimination may be protective (17), which may be particularly the case among those with a pro-Black bias.
The cross-sectional nature of our data precludes inferences regarding the causal direction of these associations; and the convenience sampling of midlife African American men also limits the generalizability of our findings to this population as well as other groups. Furthermore, there are limitations with respect to the measurement of hypertension, which was based on blood pressure assessed at a single point and retrospective self-reported history (26). Despite these caveats, our findings suggest that racial discrimination in tandem with holding an unconscious anti-Black bias may have particularly detrimental consequences for hypertension among African American midlife men. Our results provide a plausible explanation for previous null or inverse findings, and also point to directions for future research on the health effects of implicit racial bias and racial discrimination.
Figure 1.
Predicted probabilities of hypertension by racial discrimination and implicit racial bias among African American men in the Bay Area Heart Health Study (n = 91).
Note: Controlling for age, relationship status, poverty ratio, health insurance, waist-hip ratio, and number of chronic conditions.
Interaction between racial discrimination and implicit racial bias: χ2 = 4.89, 1 df, p = 0.027.
Acknowledgments
This study was funded by the University of California, Berkeley Population Center, the University of California, San Francisco Health Disparities Group, and the Emory University Race and Difference Initiative.
Acronyms
- BAHHS
Bay Area Heart Health Study
- CI
confidence interval
- IAT
Implicit Association Test
- RR
Risk Ratio
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
David H. Chae, Emory University, Rollins School of Public Health Department of Behavioral Sciences and Health Education
Amani M. Nuru-Jeter, University of California, Berkeley, School of Public Health Departments of Community Health and Human Development and Epidemiology
Nancy E. Adler, University of California, San Francisco Department of Psychiatry and Center for Health and Community
References
- 1.National Center for Health Statistics . Health, United States, 2007 With Chartbook on Trends in the Health of Americans. Hyattsville, MD: 2007. [PubMed] [Google Scholar]
- 2.Heffernan KS, Jae SY, Wilund KR, Woods JA, Fernhall B. Racial differences in central blood pressure and vascular function in young men. Am J Physiol Heart Circ Physiol. 2008;295(6):H2380–7. doi: 10.1152/ajpheart.00902.2008. [DOI] [PubMed] [Google Scholar]
- 3.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360(12):1179–90. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Ann Behav Med. 2003;25(1):55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- 5.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrell JP, Hall S, Taliaferro J. Physiologic responses to racism and discrimination: an assessment of the evidence. Am J Public Health. 2003;93(2):243–8. doi: 10.2105/ajph.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayotte BJ, Hausmann LR, Whittle J, Kressin NR. The relationship between perceived discrimination and coronary artery obstruction. Am Heart J. 2012;163(4):677–83. doi: 10.1016/j.ahj.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Cooper DC, Mills PJ, Bardwell WA, Ziegler MG, Dimsdale JE. The effects of ethnic discrimination and socioeconomic status on endothelin-1 among blacks and whites. Am J Hypertens. 2009;22(7):698–704. doi: 10.1038/ajh.2009.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis TT, Aiella AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behav Immun. 2010;24(3):438–43. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smart Richman L, Pek J, Pascoe E, Bauer DJ. The effects of perceived discrimination on ambulatory blood pressue and affective responses to interpersonal stress modeled over 24 hours. Health Psychol. 2010;29(4):403–11. doi: 10.1037/a0019045. [DOI] [PubMed] [Google Scholar]
- 11.Merritt MM, Bennett GG, Williams RB, Edwards CL, Sollers JJ. Perceived racism and cardiovascular reactivity and recovery to personally relevant stress. Health Psychol. 2006;25(3):364–9. doi: 10.1037/0278-6133.25.3.364. [DOI] [PubMed] [Google Scholar]
- 12.Sawyer PJ, Major B, Casad BJ, Townsend SS, Mendes WB. Discrimination and the stress response: psychological and physiological consequences of anticipating prejudice in interethnic interactions. Am J Public Health. 2012;102(5):1020–6. doi: 10.2105/AJPH.2011.300620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. Am J Public Health. 1996;86(10):1370–8. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: the Pitt County Study. Am J Epidemiol. 2008;167(5):624–32. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- 15.Chae DH, Lincoln KD, Adler NE, Syme SL. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Soc Sci Med. 2010;71(6):1182–8. doi: 10.1016/j.socscimed.2010.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. J Pers Soc Psychol. 2003;84(5):1079–92. doi: 10.1037/0022-3514.84.5.1079. [DOI] [PubMed] [Google Scholar]
- 17.Crocker J, Major B. Social stigma and self-esteem: the self-protective propertives of stigma. Psychol Rev. 1989;96(4):608–30. [Google Scholar]
- 18.LaVeist TA, Sellers R, Neighbors HW. Perceived racism and self and system blame attribution: consequences for longevity. Ethn Dis. 2001;11(4):711–21. [PubMed] [Google Scholar]
- 19.Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: implications for group identification and well-being. J Pers Soc Psychol. 1999;77(1):135–49. [Google Scholar]
- 20.Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial identity, racial discrmination, perceived stress, and psychological distress among African American young adults. J Health Soc Behav. 2003;44(3):302–317. [PubMed] [Google Scholar]
- 21.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 22.Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 23.Nosek BA. Understanding and using the Implicit Association Test: II. Method variables and construct validity. Pers Soc Psychol Bull. 2005;31(2):166–80. doi: 10.1177/0146167204271418. [DOI] [PubMed] [Google Scholar]
- 24.Okazaki S. Impact of racism on ethnic minority mental health. Perspect Psychol Sci. 2009;4(1):103–7. doi: 10.1111/j.1745-6924.2009.01099.x. [DOI] [PubMed] [Google Scholar]
- 25.Harlow SD, Linet MS. Agreement between questionnaire data and medical records—the evidence for accuracy of recall. Am J Epidemiol. 1989;123:894–900. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- 26.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 27.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J Health Psychol. 1997;2(3):335–51. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 28.Taylor TR, Kamarck TW, Shiffman S. Validation of the Detroit Area Study Discrimination Scale in a community sample of older African American adults: the Pittsburgh healthy heart project. Int J Behav Med. 2004;11(2):88–94. doi: 10.1207/s15327558ijbm1102_4. [DOI] [PubMed] [Google Scholar]
- 29.Reynolds WM. Development of reliable and valid short forms of the Marlowe-Crowne Social Desirability Scale. J Clin Psychol. 1982;38(1):119–25. [Google Scholar]
- 30.Ewert T, Fuessi M, Cieza A, Andersen C, Chatterji S, Kostanjsek N, Sucki G. Identification of the most common patient problems in patients with chronic conditions using the ICF checklist. J Rehabil Med. 2004;44(Suppl):22–9. doi: 10.1080/16501960410015362. [DOI] [PubMed] [Google Scholar]
- 31.Roth PL, Switzer FS, Switzer DM. Missing data in multiple item scales: a Monte Carlo analysis of missing data techniques. Organ Res Methods. 1999;2(3):211–32. [Google Scholar]
- 32.Spiegelman D. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 33.Zou G. A modified Poisson approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 34.Jaccard J. Interaction effects in logistic regression. Sage Publications; Thousand Oaks, CA: 2001. [Google Scholar]
- 35.Livingston RW. The role of perceived negativity in the moderation of African Americans’ implicit and explicit racial attitudes. J Exp Soc Psychol. 2002;38(4):405–413. [Google Scholar]