Abstract
Background.
Physical activity can positively influence health for older adults. Primary care is a good setting for physical activity promotion.
Objective.
To assess the feasibility of a pedometer-based walking programme in combination with physical activity consultations.
Methods.
Design: Two-arm (intervention/control) 12-week randomized controlled trial with a 12-week follow-up for the intervention group. Setting: One general practice in Glasgow, UK. Participants: Participants were aged ≥65 years. The intervention group received two 30-minute physical activity consultations from a trained practice nurse, a pedometer and a walking programme. The control group continued as normal for 12 weeks and then received the intervention. Both groups were followed up at 12 and 24 weeks. Outcome measures: Step counts were measured by sealed pedometers and an activPALTM monitor. Psychosocial variables were assessed and focus groups conducted.
Results.
The response rate was 66% (187/284), and 90% of those randomized (37/41) completed the study. Qualitative data suggested that the pedometer and nurse were helpful to the intervention. Step counts (activPAL) showed a significant increase from baseline to week 12 for the intervention group, while the control group showed no change. Between weeks 12 and 24, step counts were maintained in the intervention group, and increased for the control group after receiving the intervention. The intervention was associated with improved quality of life and reduced sedentary time.
Conclusions.
It is feasible to recruit and retain older adults from primary care and help them increase walking. A larger trial is necessary to confirm findings and consider cost-effectiveness.
Keywords. Ageing, patient education, physical activity, prevention, primary care, quality of life
Introduction
The Toronto Charter for physical activity 1 reports that physical activity (PA) is key for prevention of non-communicable disease, with physical inactivity the fourth leading cause of mortality globally. In most countries, older adults are less active. There is a growing interest in the health consequences of sedentary behaviour (time spent sitting/lying); even if an individual achieves recommended PA levels, his/her health may still be at risk if sedentary for many hours. 2 UK guidelines recommend older adults achieve a minimum of 150 minutes of moderate intensity PA per week, minimize sedentary time and partake in activities that improve strength and balance. 3 The most recent Scottish Health Survey showed that 83% of men and 88% of women in Scotland aged 65 years and over failed to meet the PA recommendation. 4 Low levels of activity (fewer than 30 minutes of moderate or vigorous activity per week) increases markedly with age (from 46% of men aged 65–69 to 84% of those aged 85 and over, and from 44% to 91%, respectively, among older women). It is widely recognized that promoting PA to older adults is challenging. 5 In a companion document 6 to the Toronto Charter, seven ‘investments that work’ in relation to PA promotion are noted. One such investment is to integrate PA promotion into primary care.
A common method of PA promotion in primary care is an exercise referral scheme. Here, patients are referred to a third party (often a sports centre or leisure facility), which then prescribes an exercise programme tailored to individual needs. In the UK, over 600 schemes are thought to be in operation. However, a recent review found only modest increases in PA levels from such schemes. 7
An alternative model for PA promotion is for primary care staff to provide advice. Ninety-seven percent of the Scottish population are registered with a general practice 8 and 84% of patients made at least one visit in 2008/2009. 9 General practitioner (GP) consultation rates increase as adults get older. 10 Thus, general practices are convenient locations to reach older adults. Non-physician delivery models are important, given time constraints of GPs. 11 Appropriately trained nurses can produce similarly high quality care and outcomes as GPs in some situations. 12
Walking is a low cost and accessible mode of activity, and pedometers, used with walking programmes that make use of evidenced-based behaviour change techniques, have been successful in increasing activity levels for adults in the community. 13 The aim of this study was to assess the feasibility of a pedometer-based walking programme in combination with PA consultations in Scottish adults aged 65 years and above in a primary care setting. We planned to provide information on recruitment and retention, the intervention process and outcome measures that could be useful in designing a larger trial.
Methods
Methods are outlined here and described in more detail elsewhere. 14 Written informed consent was obtained from all participants.
Setting
One general practice in Glasgow, Scotland (UK).
Participants
The practice had 461 patients (190 male and 271 female) aged ≥65 years. Inclusion criteria were living independently and not meeting current PA recommendations. Exclusion criteria were refusals, unable to walk outside independently, unable to understand the rationale behind the trial, and exclusion for medical reasons by GP.
Recruitment
Data were collected between July 2010 and February 2011. Medical records were screened by a GP for contraindications to PA. Recruitment was via letter sent by the GP, with reminder letters sent after 2 weeks to non-responders. An open-ended question was included to determine reasons for non-participation. Positive responders were contacted by a researcher to schedule the first appointment.
Intervention
The processes used are detailed in the trial intervention manual (available from the first author). Briefly, two 30-minute PA consultations were delivered individually to each participant by a practice nurse who had been trained in these procedures. The consultations followed recommended guidelines 15 , were based on the social cognitive model of behaviour change, and have been shown to successfully increase PA participation in adults. 13 16 17 The initial consultation aimed to increase walking participation. A 12-week individualized graduated walking programme in the form of a specially designed booklet and pedometer was given to participants. We did not use a universal goal (e.g. 10 000 steps) but encouraged steps to be added to each person’s own baseline. A walking group was an option for participants. The practice nurse informed participants of the walking group meeting point and times prior to the beginning of the intervention. Walking group location and times were also provided in the walking booklet as well as example walking routes in the local area. The walking group met twice weekly regardless of the number of participants attending and was led by a researcher trained in leading walking groups. The second consultation (12 weeks after the first) aimed to maintain walking behaviour and prevent relapse.
Study design
The study was a two-arm 12-week randomized controlled trial with a follow-up at 24 weeks. The intervention group began the walking intervention immediately. The control group was asked to continue normal PA for the first 12 weeks of the study and then received the same 12-week intervention and the second consultation. However, the control group did not have a further follow-up.
Procedures
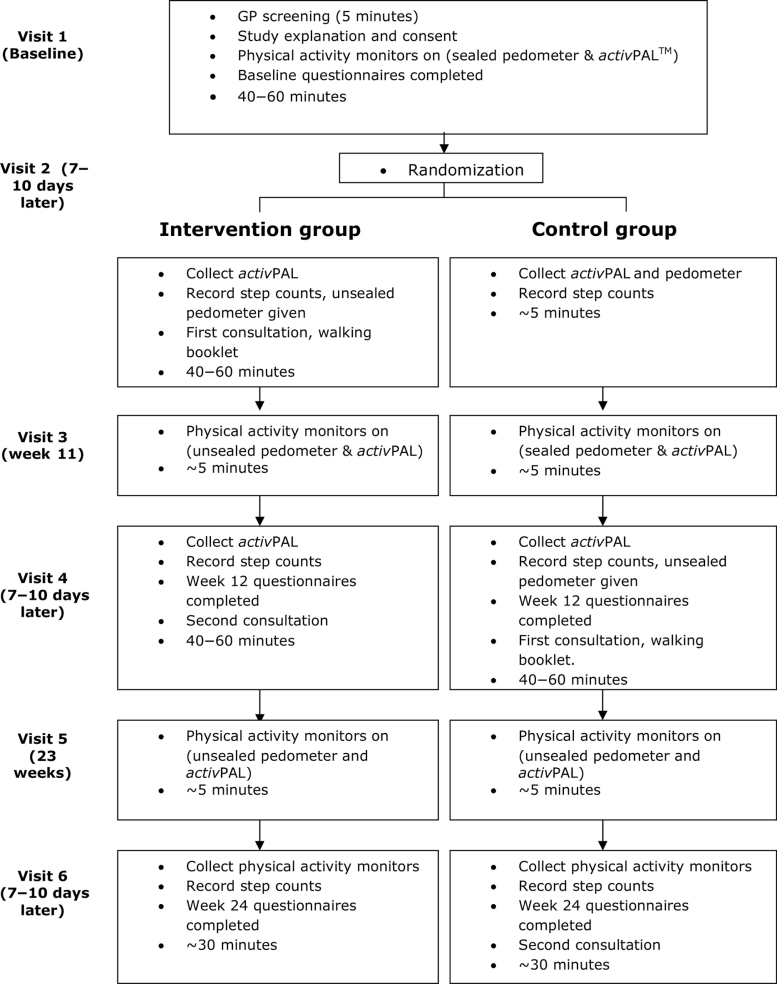
Participants were invited to attend six visits over 24 weeks (Fig. 1). Randomization was performed using an ordered set of sealed envelopes containing group allocations. Allocations were made by an independent member of the research team and inserted into envelopes in a random order. The nurse and a research assistant were not blinded to group allocation but all other researchers were. Full details of the procedures followed on each of the study visits are described elsewhere. 14 Briefly, at visit 1, participants met with the practice nurse to go over the study protocol, discussed their present health with the GP, completed informed consent and questionnaires and were fitted with a sealed pedometer (so that participants were unaware of their step counts before being given the intervention) and an activPAL. All participants were instructed to continue with their normal PA patterns.
Figure 1.
Study visits
Outcome measures
The primary outcome was the average daily step count over 1 week, recorded with a sealed pedometer (NL-1000, New Lifestyles Inc., Lee’s Summit, Missouri). The activPALTM monitor (PAL Technologies Ltd, Glasgow, Scotland) was also used to record step counts and quantify activity patterns. The activPAL is a small (5 × 3.5 × 0.7cm), light (20g) unit, attached to the anterior surface of the thigh and worn continuously throughout the monitoring period. It has been validated for use in older populations, 18 and allows the measurement of posture in addition to step counts but has no visible display. The pedometer and activPAL were fitted by the practice nurse who had been appropriately trained by the research team.
Psychosocial variables were assessed by self-report questionnaires: the Short-Form 36 Health Survey version 2 (SF-36v2) to assess quality of life 19 , the Positive and Negative Affect Schedule (PANAS) to assess mood 20 , the Perceived Motor-Efficacy Scale for Older Adults (PMES-OA) to assess functional ability 21 , and the UCLA Loneliness Scale (version 3) 22 as a measure of emotional and social loneliness. The psychosocial measures were collected on visit 1 (baseline), visit 4 (12 weeks) and visit 6 (24 weeks) for both groups.
To gain insight into participants’ experiences of the walking intervention, two focus groups were conducted; one with each study group (intervention and control) on completion of the 12-week programme. The focus group schedule explored the perceived benefits of increased walking, views on the pedometer and PA consultation, barriers encountered and future recommendations. There was also an opportunity (at the end of the discussion) for feedback on topics of importance to participants that were not covered elsewhere. All participants were asked if they would be interested in participating in a group discussion by the practice nurse during visit 1. Those who were interested provided consent to be contacted and were then invited to attend. Each group consisted of 7–9 participants and lasted for approximately 1 hour. All focus groups took place in a private room and were facilitated by two of the research team. Focus groups were audio-recorded and transcribed verbatim (and anonymized). The feasibility of rolling out the intervention in a community setting was explored using short semi-structured interviews with five key members of the project team and the manager of the general practice in which the trial was conducted.
Data analysis
Quantitative analyses were performed using R for Windows v2.11.1 on an intention to treat basis, i.e. according to randomized group, regardless of adherence to the intervention. For all outcome measures, a mixed-effects (repeated measures) regression model was applied. All available data were used. Models included random participant effects, and fixed effects for study group (intervention or control), time point (baseline, week 12 or week 24, as a categorical variable) and their interaction. A general covariance structure for model residuals over time was assumed.
Intervention effects are reported in terms of mean changes in outcomes over time within each group, and differences between study groups in the within-group changes over time. Between-groups, the main comparison was the difference between the intervention and control groups in the change from baseline to week 12; this represents the randomized intervention effect and is the principal analysis for each outcome.
For each outcome, a fixed-effects regression model, with terms for intervention, time and their interaction, was fitted to estimate the residual standard deviation (SD) of the outcome. Intervention effect estimates were standardized by dividing by the corresponding residual SD estimate (similar to Cohen’s d).
Qualitative data were thematically analysed by two members of the research team independently. The process of thematic analysis involves ‘identifying, analysing and reporting patterns (themes) within data’.23 A qualitative data indexing package (NVivo) was used to facilitate coding and retrieval of the data. First, initial codes were identified, based on careful reading and re-reading of the data. These codes were then sorted into potential themes. Direct quotes from the data were grouped under thematic headings, providing a clear illustration of each theme and also some indication of the frequency with which each theme was addressed. Finally, the themes were refined through comparison across the data set. A summary of the data is presented (rather than the main themes, such as ‘support’ and ‘practical issues’) as this article presents the findings from the feasibility study as a whole. Quotations have been chosen to illustrate particular points and are identified in the text by an anonymized code (indicating respondent number and the focus group discussion they participated in; intervention or control or the project team ID number for semi-structured interviews).
Results
Recruitment and retention
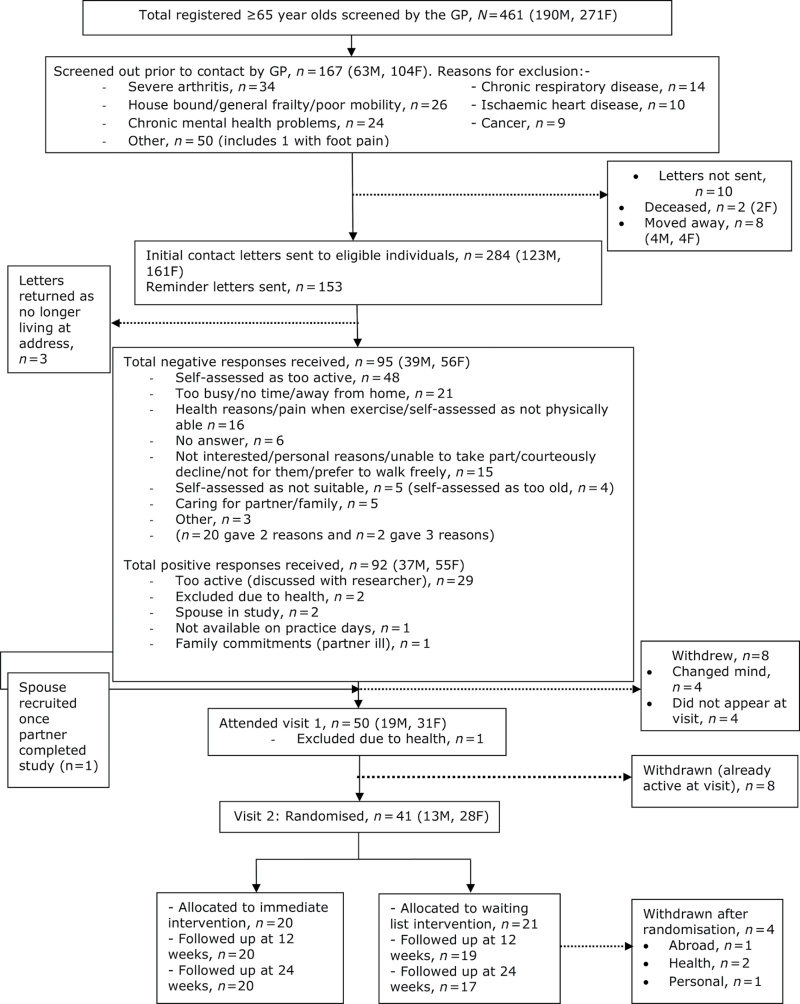
Figure 2 shows participant flow through the trial. From an initial pool of potential participants (N = 461), a total of 177 were ineligible due to (i) excluded by GP (ii) moved away or (iii) deceased. We note in Figure 2 the reasons why individuals were screened out by the GP. The main three contraindications to PA were severe arthritis (n = 34), being house bound, general frailty or poor mobility (n = 26), and chronic mental health problems (n = 24).
Figure 2.
Recruitment and participant flow through the trial
A final sample of eligible participants (n = 284) was invited to join the study. The invitation to participate in the walking project resulted in a 65.8% response rate (187/284). Of the eligible participants, 32.4% (n = 92) responded positively and 33.4% (n = 95) declined to take part. The remaining 34.2% (n = 97) did not respond. Of the 92 participants who responded positively, 44.6% (n = 41) participated in study visits. The Scottish Index of Multiple Deprivation (SIMD) was used to allocate each participant by their postcode to a category of socioeconomic status. Of those who participated in the study, 46% (19/41) were in the least deprived SIMD category and 59% (24/41) were in the youngest age category of 65–69 years. However, no significant differences were found between those who responded positively and those who responded negatively to the study invite in the distributions of SIMD (P = 0.91) or gender (P = 0.15). Baseline characteristics of study participants are shown in Table 1. There were no significant differences in demographic variables between study groups. The predominance of women in the trial (68%) is reflective of the study population. The retention rate (number of participants completing the study, as a proportion of those randomized) was 90% (37/41).
Table 1.
Baseline characteristics of study participants by group (Observations made [OBS] Missing data [MISS])
| Control | Intervention | |||
| Age | N OBS (NMISS) | 21 (0) | 20 (0) | |
| Mean (SD) | 70.0 (4.3) | 71.6 (6.0) | ||
| [Range] | [65.0, 83.0] | [65.0, 83.0] | ||
| Gender | N OBS (NMISS) | 21 (0 | 20 (0) | |
| Male | N (%) | 6 (29%) | 7 (35%) | |
| Female | N (%) | 15 (71%) | 13 (65%) | |
| SIMD | N OBS (N MISS) | 21 (0) | 20 (0) | |
| 1—most deprived | N (%) | 0 (0%) | 1 (5%) | |
| 2 | N (%) | 3 (14%) | 1 (5%) | |
| 3 | N (%) | 6 (29%) | 2 (10%) | |
| 4 | N (%) | 3 (14%) | 6 (30%) | |
| 5—least deprived | N (%) | 9 (43%) | 10 (50%) | |
| Ethnicity | N OBS (N MISS) | 21 (0) | 19 (1) | |
| White Scottish | N (%) | 14 (67%) | 12 (63%) | |
| White British | N (%) | 6 (29%) | 6 (32%) | |
| Other | N (%) | 1 ( 5%) | 1 ( 5%) | |
| Education | N OBS (N MISS) | 21 (0) | 20 (0) | |
| Some secondary school | N (%) | 3 (14%) | 1 ( 5%) | |
| Completed secondary school | N (%) | 2 (10%) | 5 (25%) | |
| College/University | N (%) | 2 (10%) | 5 (25%) | |
| Completed college/University | N (%) | 10 (48%) | 4 (20%) | |
| Postgraduate | N (%) | 4 (19%) | 5 (25%) | |
| Homeowner status | N OBS (N MISS) | 21 (0) | 20 (0) | |
| Own/buying | N (%) | 20 (95%) | 18 (90%) | |
| Rent/private | N (%) | 0 ( 0%) | 1 ( 5%) | |
| Rent/council | N (%) | 1 ( 5%) | 1 ( 5%) | |
| Marital status | N OBS (N MISS) | 21 (0) | 20 (0) | |
| Single | N (%) | 4 (19%) | 4 (20%) | |
| Cohabiting | N (%) | 0 ( 0%) | 0 ( 0%) | |
| Married and living together | N (%) | 8 (38%) | 8 (40%) | |
| Separated | N (%) | 1 ( 5%) | 0 ( 0%) | |
| Divorced | N (%) | 4 (19%) | 4 (20%) | |
| Widowed | N (%) | 4 (19%) | 4 (20%) |
Figure 2 also summarizes the reasons that negative responders gave for declining participation. The most common (51%; 48/95) was that the individual self-assessed as already physically active. Of the positive responders, 54% (50/92) attended the first study visit and 45% (41/92) were randomized into the study. The most common reason for positive responders not being randomized was that they were already active (baseline step count >70 000 steps/week). No participants objected to randomization.
Appropriateness of the intervention for this target group and for the primary care setting
Nine participants from the intervention group and seven from the control group attended focus group discussions. The findings from these suggest that the pedometer was easy to use and was an important motivational tool for many. For example, one participant said ‘I think when you’ve got your meter on, you try to get a wee bit better … I feel it’s like a challenge’ (P107, control when receiving intervention). Using the pedometer for feedback in conjunction with goal setting and recording via the booklet appeared helpful. For instance, one participant noted: ‘When you’re out you’re so aware “I’ve got to get this steps going,” … walk round a longer route or do something … I found writing it down, it made me, do more. I did say 7000 today; tomorrow I’ll do 8’ (P123, intervention). However, some participants spoke of not always wearing the pedometer: ‘I probably could have accomplished the steps much more easily if I’d just worn it all the time as suggested. I didn’t, I tended to wait until I was actually going to do something’ (P125, intervention). The nurse-led consultation did not raise any concerns from participants and can therefore be seen as a feasible mechanism for delivering a walking intervention in primary care. Participants noted that it was helpful to have a person to phone if needed (the nurse)—‘You can lift the phone … you’re at the end of a phone I can ask something’ (P107, control).
Six adverse events were noted through the trial. Three were attributable to the intervention or research monitoring: one participant withdrew because of knee pain brought on by walking, one participant experienced temporary low back pain and one participant reported skin irritation due to activPAL wear. The latter two participants continued walking. Walking therefore appears to be a safe mode of activity to promote to older adults. However, the walking group was poorly attended (only nine participants attended but not regularly).
Project team members with an academic background were positive about rolling this intervention out in primary care as they saw it as a good way to access and recruit older adults. However, those from a primary care background were less certain; their main concerns were about time and routine care rather than research. For example, they said that screening for PA contraindications for this age group was time consuming: ‘This is a particular issue about physical activity. You’re not screening to see if the person’s alive or you’re not screening to see if they’re on a particular drug, you’re screening their whole life circumstances to see if physical activity is going to be okay and not contraindicated for them’ (101). Those from primary care acknowledged that a research project is different from routine practice. One said: ‘The project needs to be moved out of [the] research umbrella, it needs to be part of the primary care prevention and it needs to become embedded in the fabric of the way the primary care functions’ (104).
Outcome measures
Step count data collected by pedometer and activPAL are shown in Table 2. At least some pedometer step count data were available for all participants at each time point. The activPAL did not return any data on only five occasions (four at baseline), due to technical failures. Nevertheless, the activPAL appears to have been used more consistently than the pedometer during the assessment periods. There were 52 days of recorded step counts with <1000 steps from the pedometers, compared with only 2 from the activPAL monitors. These values were not considered feasible, possibly due to the monitors not being worn at all times, and were excluded from calculations of the average daily step count. In addition, further analysis of these data has shown that pedometers underreport the values obtained from the continuously used activPAL monitor by around 2000 steps per day. 24
Table 2.
Step counts, recorded using pedometer and activPAL
| Pedometer | activPAL | |||||
| Intervention | Control | Intervention | Control | |||
| Number of participants providing data, number of outliers removed and mean (SD) daily average step counts | ||||||
| Baseline | N Participants | 20 | 21 | 19b | 18b | |
| N Outliersa | 8 | 11 | 0 | 0 | ||
| Mean (SD) | 6743 (2282) | 5671 (1900) | 7469 (2312) | 7351 (2360) | ||
| Week 12 | N Participants | 20 | 19 | 20 | 19 | |
| N Outliers | 3 | 14 | 0 | 2 | ||
| Mean (SD) | 7347 (1766) | 5935 (2226) | 9351 (2017) | 7138 (2169) | ||
| Week 24 | N Participants | 20 | 17 | 19b | 17 | |
| N Outliers | 11 | 5 | 0 | 0 | ||
| Mean (SD) | 7543 (2804) | 7683 (2824) | 9161 (2631) | 9100 (3175) | ||
| Within-group changesc | ||||||
| W12– BL | Estimate | 604 | 266 | 1907 | –213 | |
| (95% CI) | (–320, 1528) | (–672, 1205) | (1070, 2743) | (–1104, 679) | ||
| P-value | P = 0.20 | P = 0.57 | P < 0.001 | P = 0.64 | ||
| W24 – W12 | Estimate | 196 | 1672 | –206 | 1908 | |
| (95% CI) | (–867, 1260) | 538, 2806) | (–1100, 688) | (972, 2844) | ||
| P-value | P = 0.71 | P = 0.004 | P = 0.65 | P < 0.001 | ||
| Between-group difference (Intervention – Control)c | ||||||
| W12 – BL | Estimate | 338 | 2119 | |||
| (95% CI) | (–979, 1654) | (897, 3342) | ||||
| P-value | P = 0.61 | P = 0.001 | ||||
| W24 – W12 | Estimate | –1476 | –2114 | |||
| (95% CI) | (-3030, 79) | (–3408, –820) | ||||
| P-value | P = 0.062 | P = 0.002 | ||||
a Any daily step count <1000 steps was assumed to be due to a device malfunction or failure to wear the device for the whole day. Such values were excluded from the calculation of daily average step counts.
bData processing errors resulted in loss of activPAL data for four participants (one intervention, three controls) at baseline and for one participant (intervention) at week 24.
c Models not adjusted for baseline covariates.
There was no evidence of changes in pedometer step counts in either group during the first 12 weeks of the study, and no difference between groups over this period. Between weeks 12 and 24, the control group increased their average daily walking by 1672 pedometer steps.
There was strong evidence of an intervention effect with activPAL step counts, based on the between-group comparison of changes over the first 12 weeks of the study (2119 steps/day, P = 0.001). During the walking intervention, both study groups showed similar step count increases (1907 for intervention and 1908 for control when they received the intervention; standardized effect = 0.78). The increase in steps observed from baseline appears to have been maintained in the intervention group (mean step count week 12: 9351, week 24: 9161, P = 0.65). These results are illustrated in Figure 3.
Figure 3.
ActivPAL step counts
Table 3 shows changes over time and between-group differences for selected secondary outcomes. Both groups showed increases in objectively measured walking time and decreases in objectively measured sedentary time during the periods when they received the walking intervention. While a pattern of improvement was seen across all subscales of the SF-36, the physical health dimension score was most sensitive to change during the intervention. Neither PANAS (both positive and negative) scores, the UCLA Loneliness Scale nor PMES-OA scores showed any evidence of within- or between-group effects during the study (full data available on request). A cost-utility analysis suggested that the intervention would cost around 100 pounds sterling per patient (full report available on request).
Table 3.
Selected secondary outcomesa
| Within-group changes | Between-group difference (Intervention – Control) | ||
| Intervention | Control | ||
| Sedentary Time (activPAL minutes/day) | |||
| W12 – BL | –47.9 (–70.2, –25.6 | 19.6 (–4.2, 43.4) | -67.5 –100.1, –34.9), P < 0.001 |
| W24 – W12 | 6.9 (–21.2 , 34.9) | –27.5 (–56.5 , 1.5) | 34.3 –6.0, 74.7), P = 0.094 |
| Walking time (activPAL minutes/day) | |||
| W12 – BL | 22 (13, 30) | –3 (–12, 6) | 25 (13, 37), P < 0.001 |
| W24 – W12 | –2 (–12, 7) | 21 (10, 31) | –23 (-37, -9), P = 0.002 |
| SF-36 Mental Health Dimension Score | |||
| W12 – BL | 5.6 (–4.1, 15.3) | –8.8 (–20.7, 3.2) | 14.4 (–1.0, 29.8), P = 0.067 |
| W24 – W12 | –0.2 (–10.4, 9.9) | 5.3 (–7.4, 17.9) | –5.5 (–21.7, 10.7), P = 0.50 |
| SF-36 Physical Health Dimension Score | |||
| W12 – BL | 4.9 (–3.8, 13.6) | –11.0 (–21.8, –0.2) | 15.9 (2.0, 29.8), P = 0.025 |
| W24 – W12 | –0.2 (–8.2, 7.8) | 13.1 (2.9, 23.4) | –13.3 (–26.3, –0.3), P = 0.045 |
Discussion
We have shown that it is feasible to recruit and retain older adults from primary care into a walking study. The intervention was well received and no major issues arose with attendance at appointments, wearing the monitoring equipment, or use of pedometers to provide feedback towards step count goals. Participants reported that having a contact person helped them. The walking group that we provided was not well attended and is therefore not a critical aspect of the intervention, although the people who did attend appreciated it.
We found that the intervention increased step counts by around 2000 steps/day. The effect was not short term, with step counts being maintained in the intervention group at the 24-week follow-up. This suggests that walking is a mode of activity that older adults may be able to sustain over time. The increases in step counts we observed are less than we found in a similar study of working age adults. 13 However, such increases will confer health benefits to these older adults, 25 and the mean post-intervention and week 24 step counts (all over 9000 steps/day) were within the range of daily steps recommended for health benefits for older adults in a recent review. 26
We also showed that objectively monitored sedentary time was reduced by the intervention, suggesting that the participants did not compensate for increased walking by increased sitting. Continuously worn monitors are better than pedometers to provide an outcome measure for this population, although pedometers were useful for motivation. Psychosocial results suggested that the walking intervention has potential to improve quality of life for older adults. The intervention is not expensive.
Strengths and limitations
The strengths of this study were objectively monitored PA and the opportunity to observe other PA patterns from activPAL data. Limitations are those of a pilot study with only one general practice involved and one nurse delivering the intervention.
Implications for future research
A practice nurse could be trained to deliver a walking programme and therefore intervene to improve PA levels of older patients in the primary care setting. Simpler and less time-consuming methods of screening for contraindications to PA are needed to save GP time. However, despite the comment from those working in primary care that this approach needs to become part of routine care, a large scale trial, using more than one practice, is now warranted to confirm findings and to consider cost-effectiveness in more detail. A continuously worn activity monitor such as activPAL is preferred over a pedometer as an outcome measure. The SF-36 could be used in future studies to measure quality of life. There was little indication that other psychosocial measures (mood, loneliness and perceived motor efficacy) were sensitive to change. Finally, refinements to the screening processes are needed since a higher proportion of potential participants than might be expected self-reported that they were already meeting PA guidelines.
Declaration
Funding: Chief Scientist Office [CSO] Scotland (CZH/4/457); NHS Research and Development from Greater Glasgow and Clyde and the Scottish Primary Care Research Network.
Ethical approval: All procedures were approved by appropriate NHS (reference number: 08/S0701/121) and University Ethics Committees (reference number: 080855). Trial registration: ISRCTN70658148
Conflict of interest: The authors declare that they have no competing interests. Professor Malcolm Granat is a director of PAL Technologies Ltd, Glasgow UK. Professor Granat had no involvement in the data collection. There was no financial contribution to this work from PAL Technologies Ltd.
Acknowledgements
The authors thank Karen Black for delivering the intervention, the participants for engaging in the trial, walk leaders for assistance with walking groups, the general practice manager for accommodating recruitment and screening and the Clinical Research Facility for provision of consulting and meeting rooms. Walk Glasgow also provided support in setting up the walking group and Adam Evans coordinated the start of the project. We thank Carol Emslie, Joanne Cummings, Lynsay Matthews, Chloe McAdam and Graham Brennan who assisted with elements of data collection. NM conceived of the study, obtained funding and ethical approval, supervised the project, led the manuscript preparation and is guarantor for the integrity of the data. The order of the other authors is alphabetical. All authors contributed to editing the manuscript. OD and AM carried out statistical analysis and interpretation. CF helped conceive of the study and contributed to study design, obtaining funding and ethical approval, and interpreting the data. M Grant, M Grealy, M Granat, DR and DS were involved in study design and data interpretation. HM was involved in study design and collecting the data. FM was involved in data collection, analysis and interpretation. RS led the qualitative component of the project.
References
- 1. Global Advocacy for Physical Activity (GAPA) the Advocacy Council of the International Society for Physical Activity and Health (ISPAH).2010. Available from: http://www.globalpa.org.uk/charter/ (last accessed 11 July 2012).
- 2. Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer Med Sci Sports Exerc 2009; 41: 998 1005 [DOI] [PubMed] [Google Scholar]
- 3. Department of Health, Physical Activity, Health Improvement and Protection. rs London: Crown copyright; 2011. [Google Scholar]
- 4. Scottish Government. Edinburgh: Crown copyright, 2011.. Available from: http://www.scotland.gov.uk/Publications/2011/11/24083430/49 [Google Scholar]
- 5. Horne M, Skelton D, Speed S, Todd C. The influence of primary health care professionals in encouraging exercise and physical activity uptake among White and South Asian older adults: experiences of young older adults Patient Educ Couns 2010; 78: 97 103 [DOI] [PubMed] [Google Scholar]
- 6. Global Advocacy for Physical Activity (GAPA) the Advocacy Council of the International Society for Physical Activity and Health (ISPAH). 2011.. Available from: http://www.globalpa.org.uk/investments/ (last accessed on 11 July 2012).
- 7. Pavey TG, Taylor AH, Fox KR, et al. Exercise referral schemes in primary care: An effective approach to enhancing physical activity and improving health outcomes Br Med J 2011; 343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. NHS Health Scotland. Edinburgh: NHS Health Scotland. 2008.. Available from: http://www.healthscotland.com/uploads/documents/7545-Energising%20Lives.pdf (last accessed on 11 July 2012). [Google Scholar]
- 9. Information & Statistics Division. 2010.. Available from: http://www.isdscotland.org/isd/1044.html
- 10. Wood R, Bain MRS. The Health and Well-being of Older People in Scotland: Insights from National Data Edinburgh: Information & Statistics Division, 2001. [Google Scholar]
- 11. Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research J Fam Pract 2000; 49: 158 68 [PubMed] [Google Scholar]
- 12. Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care Cochrane Database Syst Rev 2005; CD001271 [DOI] [PubMed] [Google Scholar]
- 13. Baker G, Gray SR, Wright A, et al. The effect of a pedometer-based community walking intervention “Walking for Wellbeing in the West” on physical activity levels and health outcomes: a 12-week randomized controlled trial Int J Behav Nutr Phys Act 2008; 5: 44–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Macmillan F, Fitzsimons C, Black K, et al. West End Walkers 65+: a randomised controlled trial of a primary care-based walking intervention for older adults: study rationale and design BMC Public Health 2011; 11: 120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kirk AF, Barnett J, Mutrie N. Physical activity consultation for people with Type 2 diabetes: evidence and guidelines Diabet Med 2007; 24: 809 16 [DOI] [PubMed] [Google Scholar]
- 16. Kirk A, Mutrie N, MacIntyre P, Fisher M. Effects of a 12-month physical activity counselling intervention on glycaemic control and on the status of cardiovascular risk factors in people with Type 2 diabetes Diabetologia 2004; 47: 821 32 [DOI] [PubMed] [Google Scholar]
- 17. Hughes A, Gillies F, Kirk A, et al. Exercise consultation improves exercise adherence in phase IV cardiac rehabilitation J Cardiopulm Rehabil 2002; 22: 421 5 [DOI] [PubMed] [Google Scholar]
- 18. Grant PM, Dall PM, Mitchell SL, Granat MH. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults J Aging Phys Act 2008; 16: 201 14 [DOI] [PubMed] [Google Scholar]
- 19. Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom J Epidemiol Community Health 1999; 53: 46 50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales J Pers Soc Psychol 1988; 54: 1063 70 [DOI] [PubMed] [Google Scholar]
- 21. Potter LM, Grealy MA, O’Connor RC. Healthy ageing, perceived motor-efficacy, and performance on cognitively demanding action tasks Br J Psychol 2009; 100(Pt 1): 49 70 [DOI] [PubMed] [Google Scholar]
- 22. Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure J Pers Assess 1996; 66: 20 40 [DOI] [PubMed] [Google Scholar]
- 23. Braun V, Clarke V. Using thematic analysis in psychology Qual Res Psychol 2006; 3: 77 101 [Google Scholar]
- 24.MacMillan F, Rowe DA, Grant MP, Granat MH, Mutrie N. Are we missing steps? A comparison of pedometer counts and 24-hour motion sensor counts in older adults. Poster Presentation. International Conference on Ambulatory Monitoring of Physical Activity and Movement; Glasgow, UK. 2011. [Google Scholar]
- 25. Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults. Recommendation from the American College of Sports Medicine and the American Heart Association Circulation 2007; 116: 1094 105 [DOI] [PubMed] [Google Scholar]
- 26. Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations Int J Behav Nutr Phys Act 2011; 8: 80 [DOI] [PMC free article] [PubMed] [Google Scholar]