Abstract
A combination of inspiratory and expiratory three-dimensional computed tomographic volumetry provides useful information on pulmonary function and lung volume. We previously reported an early outcome of a patient undergoing living-donor lobar lung transplantation with sparing of the bilateral native upper lobes. Long-term follow-up on such patients had not been reported, and therefore we herein, for the first time, reported the 2-year follow-up of the previously reported case. According to the inspiratory and expiratory three-dimensional computed tomographic volumetric data, we demonstrated that transplanted lower lobe grafts had been working efficiently and spared bilateral native upper lobes had not provided any adverse effects.
Keywords: Living-donor, Lung transplantation, Size mismatch, Native lung sparing, Three-dimensional computed tomographic volumetry
We reported a successful case of living-donor lobar lung transplantation (LDLLT) with sparing of the bilateral native upper lobes [1]. It was the first reported case of a successful LDLLT in which a very large size mismatch between donor lungs and recipient chest cavity was solved by sparing the bilateral native upper lobes. As we have reported [1], the early postoperative outcome was satisfactory, but intermediate to long-term follow-up has not been reported in such native lung-sparing LDLLTs to date.
Three-dimensional (3D) computed tomographic (CT) volumetry has been introduced as a method of size matching into the field of lung transplantation [2, 3]. In addition, a combination of inspiratory and expiratory 3D-CT volumetry provides a useful data on pulmonary function and lung volume in individual lung lobes. We herein reported an additional report on our initial experience of bilateral native lobe-sparing LDLLT with the long-term follow-up. We also evaluated the pulmonary function both in the transplanted grafts and in the native lobes, using a combination of inspiratory and expiratory 3D-CT volumetry.
CASE REPORT
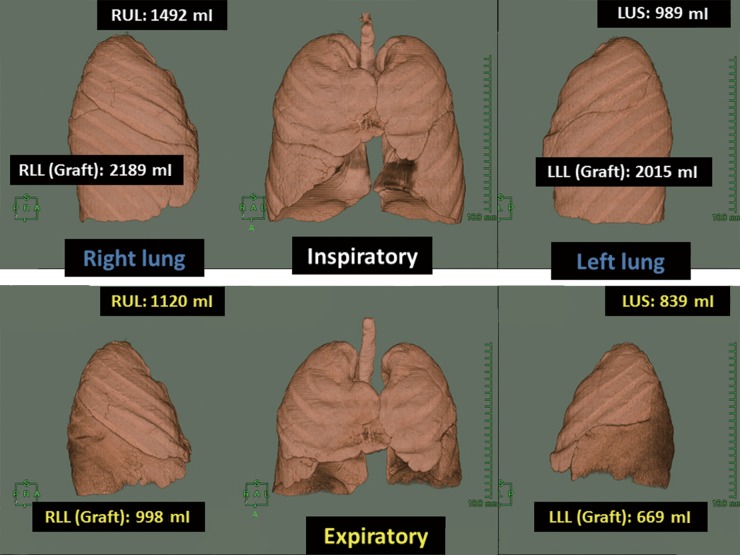
A 44-year old man with acute myelogenous leukaemia received chemotherapy followed by peripheral blood stem cell transplantation from his sister. However, he developed bronchiolitis obliterans and underwent bilateral LDLLT from his sister for the right lower lobe and his wife for the left lower lobe. According to the large size mismatch, native right upper lobe and left upper segment were spared. The postoperative course was uneventful and the patient recovered very well after LDLLT. He did not show any sign of rejection. Follow-up bronchoscopy 6 months after LDLLT showed an excellent bronchial anastomosis. His postoperative pulmonary function also maintained in a good condition and he did not show any limitations during a daily life (Table 1). According to the 3D-CT volumetric data, bilateral upper lobes (native lungs) hardly change their values both in the inspiratory and expiratory phase perioperatively, while bilateral lower lobes (implanted lower lobes) showed a drastic change (Table 1 and Fig. 1). Postoperative ventilation scintigraphy demonstrated that marked air trapping remained in the spared lungs, and ventilation score itself hardly changes anything perioperatively. The postoperative perfusion scintigraphy score also hardly changes anything perioperatively, but perfusion scintigraphy score of the bilateral upper area seemed to decrease at 2 years after LDLLT in comparison with that before LDLLT (Table 1).
Table 1:
Perioperative characteristics including pulmonary function
| Preoperative | Postoperative |
|||
|---|---|---|---|---|
| 6 months | 12 months | 24 months | ||
| Spirometry | ||||
| FVC (ml) | 2790 | 3700 | 4090 | 4210 |
| FVC (%) | 72 | 95 | 106 | 110 |
| FEV1 (ml) | 590 | 2090 | 2110 | 2160 |
| FEV1% (%) | 21 | 57 | 52 | 51 |
| TLC (ml) | 5900 | 5500 | 4820 | 5000 |
| TLC (%) | 99 | 91 | 70 | 73 |
| DLCO (ml/min/mmHg) | 2.48 | 3.97 | 4.56 | 4.38 |
| DLCO/VA (ml/min/mmHg/L) | 48.3 | 77.3 | 89.2 | 86.0 |
| Arterial blood gas (room air) | ||||
| PaO2 (mmHg) | 60.1 | 86.9 | 86.0 | 83.5 |
| PaCO2 (mmHg) | 57.0 | 36.4 | 36.8 | 35.1 |
| Six-minute walk (m) | 75 | 603 | 640 | 695 |
| 3D-CT volumetry | ||||
| Inspiratory (expiratory) | ||||
| Right lung | ||||
| Upper lobe (ml) | 1517 (1275) | 1536 (1193) | 1508 (1180) | 1492 (1120) |
| Lower lobe (ml) | 2444 (2029)a | 2120 (1106) | 2169 (1139) | 2189 (998) |
| Left lung | ||||
| Upper segment (ml) | 1049 (906) | 1059 (922) | 980 (882) | 989 (839) |
| Lower lobe (ml) | 2381 (1965)b | 1898 (791) | 2017 (822) | 2015 (669) |
| Ventilation scintigraphy (%) | ||||
| Right (U/M/L) | 13/22/19 | 13/24/19 | 15/25/18 | 12/24/22 |
| Left (U/M/L) | 8/20/18 | 8/18/18 | 8/17/17 | 7/16/19 |
| Perfusion scintigraphy (%) | ||||
| Right (U/M/L) | 14/20/16 | 12/26/21 | 14/26/20 | 11/25/25 |
| Left (U/M/L) | 10/21/19 | 6/17/18 | 6/15/19 | 5/14/20 |
DLCO: diffusion capacity for carbon monoxide; DLCO/VA: diffusion capacity for carbon monoxide/alveolar volume; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; TLC: total lung capacity; U/M/L: upper area/middle area/lower area.
aIncluding middle lobe.
bIncluding lingular segment.
Figure 1:
Three-dimensional computed tomographic volumetry 2 years after LDLLT. The volumes of individual lung lobes are shown in the inspiratory and expiratory phase. LLL: left lower lobe, LUS: left upper segment, RLL: right lower lobe, RUL: right upper lobe.
DISCUSSION
Size matching is the most critical issue in LDLLT since the recipient usually receives at most two lower lobes from two donors [1, 4]. When grafts are too small, a limited amount of vascular bed and intrathoracic remaining dead space could cause severe complications. Hyperinflation of the grafted lungs might also result in insufficient respiratory dynamics or haemodynamic collapse after LDLLT [5]. It is often difficult for large patients to find two donors who can donate enough lung volume, and native lung-sparing LDLLT might be an option for such patients. Because of the scarcity of such surgical procedures, reliable evidences have not been accumulated. Therefore, we reported an intermediate follow-up of bilateral native upper lobe-sparing LDLLT with favourable results.
We demonstrated that a combination of inspiratory and expiratory 3D-CT volumetry provided the useful data on pulmonary function and lung volume in individual lung lobes. As shown in Fig. 1, 3D-CT volumetry apparently visualized the data that transplanted lower lobe grafts worked efficiently and that the native bilateral upper lobes neither changed in size nor affected the total lung function. According to perfusion/ventilation scintigraphy and 3D-CT volumetry, native spared lungs showed marked air trapping and received very little blood flow. In contrast, the implanted small grafts received a majority of blood flow and provided sufficient lung function. Furthermore, the blood flow in the native spared lungs slightly decreased 2 years after LDLLT, which is usually seen in the single cadaveric lung transplantation. This would be reflected by the fact that the vascular resistance of the healthy implanted lobes was lower than that of the native lobes, although the change was small in the present case because the patient did not show pulmonary hypertension preoperatively. Although the perfusion of the bilateral native upper lobes decreased to some extent with time, there was a possibility that at least the right native upper lobe worked not only as a space saver but also as an additional vascular bed soon after LDLLT. In addition, the fact that the ventilation score did not change before and after LDLLT implied that the severity of the bronchiolitis obliterans did not develop since the patient received more immunosuppressants after LDLLT and the obstructive lesion itself was already at end stage before LDLLT. However, it should be kept in mind that this surgical technique potentially has the limitation when the spared native lungs become emphysematous with time.
In conclusion, we reported the intermediate follow-up of bilateral native upper lobe-sparing LDLLT with favourable results. We also confirmed that a combination of inspiratory and expiratory 3D-CT volumetry was effective since it provided useful information on pulmonary function and lung volume. We believe that this novel technique of a combination of inspiratory and expiratory 3D-CT volumetry would be widely utilized to assess the local lung function in the future.
Conflict of interest: none declared.
REFERENCES
- 1.Fujinaga T, Bando T, Nakajima D, Sakamoto J, Chen F, Shoji T, et al. Living-donor lobar lung transplantation with sparing of bilateral native upper lobes: a novel strategy. J Heart Lung Transplant. 2011;30:351–3. doi: 10.1016/j.healun.2010.10.006. doi:10.1016/j.healun.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Chen F, Fujinaga T, Shoji T, Yamada T, Nakajima D, Sakamoto J, et al. Perioperative assessment of oversized lobar graft downsizing in living-donor lobar lung transplantation using three-dimensional computed tomographic volumetry. Transpl Int. 2010;23:e41–4. doi: 10.1111/j.1432-2277.2010.01123.x. [DOI] [PubMed] [Google Scholar]
- 3.Chen F, Kubo T, Shoji T, Fujinaga T, Bando T, Date H. Comparison of pulmonary function test and computed tomography volumetry in living lung donors. J Heart Lung Transplant. 2011;30:572–5. doi: 10.1016/j.healun.2010.11.019. doi:10.1016/j.healun.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Date H, Aoe M, Sano Y, Nagahiro I, Miyaji K, Goto K, et al. Improved survival after living-donor lobar lung transplantation. J Thorac Cardiovasc Surg. 2004;128:933–40. doi: 10.1016/j.jtcvs.2004.07.032. [DOI] [PubMed] [Google Scholar]
- 5.Haddy SM, Bremner RM, Moore-Jefferies EW, Thangathurai D, Schenkel FA, Barr ML, et al. Hyperinflation resulting in hemodynamic collapse following living donor lobar transplantation. Anesthesiology. 2002;97:1315–7. doi: 10.1097/00000542-200211000-00042. doi:10.1097/00000542-200211000-00042. [DOI] [PubMed] [Google Scholar]