Abstract
Objectives
To determine the test-retest reliability over 2 separate days for weight-bearing ability during standing tasks in individuals with chronic stroke and to compare the weight-bearing ability among five standing tasks for the paretic and non-paretic limbs.
Design
Prospective study using a convenient sample.
Setting
Free-standing tertiary rehabilitation center.
Participants
15 community-dwelling stroke individuals with moderate motor deficits; volunteer sample.
Interventions
Not applicable.
Main Outcome Measures
Weight-bearing ability as measured by the vertical ground reaction force during 5 standing tasks (rising from a chair, quiet standing, weight-shifting forward, backward, laterally).
Results
The weight-bearing ability was less for the paretic limb compared with the nonparetic limb, but the intraclass correlation coefficients were high (0.95–0.99) for both limbs between the 2 sessions for all 5 tasks. The forward weight-shifting ability was particularly low in magnitude on the paretic side compared with the other weight-shifting tasks. In addition, the forward weight-shift ability of the nonparetic limb was also impaired but to a lesser extent. Large asymmetry was evident when rising from a chair, with the paretic limb bearing a mean 296N and the nonparetic side bearing a mean 458N. The weight-bearing ability during all 5 tasks correlated with one another (r range, 0.56–0.94).
Conclusions
Weight-bearing ability can be reliably measured and may serve as a useful outcome measure in individuals with stroke. We suggest that impairments of the hemiparetic side during forward weight shifting and sit-to-stand tasks presents a challenge to the motor systems of individuals with stroke, which may account for the poor balance that is often observed in these individuals.
Keywords: Cerebrovascular Accident, Reproducibility of Results, Rehabilitation, Weight-Bearing
INTRODUCTION
The transfer of weight onto a limb is essential for functional mobility, and is a requirement for rising from a chair, transfers, walking, turning and stair climbing. Reduced ability to weight-bear on the paretic limb is recognized as a common impairment following a cerebrovascular accident. In fact, it has been reported that the majority of individuals (79 to 87%) with stroke bear less weight on the paretic limb (25 to 43% of body weight) during the static task of quiet standing.1–6 Possible causes of this reduced ability following a stroke include pain, spasticity, impaired balance, sensory loss, neglect, muscle weakness, and perceptual deficits.
Reduced ability to weight-bear on the paretic limb is not limited to static standing tasks. Weight-bearing during dynamic tasks such as rising from a chair7–9 or voluntarily weight-shifting to one limb while standing10–13 is also compromised following a stroke. Asymmetrical weight-bearing has been reported when rising from a chair, with the paretic limb accepting between 25 to 38% of body weight.7–9,14 In addition, it has been reported that individuals with stroke can only shift approximately 55% of their body weight onto the paretic limb while standing in the forward direction in a step stance posture and 65% in the lateral direction with feet parallel.13 In contrast, healthy elderly individuals have demonstrated the ability to voluntarily shift 95% of their body weight onto a single limb in both the forward and lateral directions.13
Weight-bearing ability correlates with functional performance in individuals with stroke. The degree of weight-bearing asymmetry during quiet standing has been correlated to motor function, level of self-care independence as well as length of hospital stay following stroke.4,15 The ability to transfer body weight laterally or forward onto the paretic limb while standing has been shown to be indicative of walking performance.13,14,16 Cheng et al.14 suggested that the asymmetrical body weight distribution during a rise from a chair might be a contributing factor to the cause of falls in individuals with stroke. In addition, increased weight-bearing abilities have been shown to improve the ability to rise from a chair and bilateral symmetry.6,17
Although a major focus of rehabilitation is to increase the tolerance and ability to bear weight on the paretic limb during various functional tasks,18,19 there has been no study that has examined the test-retest reliability of weight-bearing ability across sessions in individuals with stroke. Goldie et al.13 reported high within session reliability (consecutive trials) for forward and lateral weight-shifting while standing for individuals with stroke, however, the day-to-day variability is not known. Reliability is the degree to which measurements are free from error20 and is a pre-requisite prior to use as an outcome measure. More specifically, the test-retest reliability is important to evaluate for rehabilitation since outcome measures are generally evaluated over time to assess the effectiveness of treatment interventions. It is imperative that clinicians know how much of a measurement change can be attributed to random variation and how much is due to true change. Therefore, the first purpose of this study was to determine whether the weight-bearing ability during functional tasks measured across two separate days as quantified by the vertical ground reaction force is reliable for the paretic and non-paretic limbs in individuals with stroke.
Weight-bearing activities are often assessed or practiced in various standing postures (e.g., step stance versus feet parallel), into different directions (lateral, forward, backward) and under static and dynamic conditions. There is little information as to how the particular task, direction or posture affects the magnitude of weight-bearing or how the weight-bearing performance among different tasks relates to one another. Thus, the second purpose of this study was to a) compare the magnitude of weight-bearing ability among five functional standing tasks (quiet standing, rising from a chair, weight-shifting in a forward, lateral and backward direction), and b) measure the relationship (i.e., correlation) of the weight-bearing ability among the five tasks.
There is also growing evidence that motor function is not normal on the non-paretic side in individuals with stroke, as evident by the presence of muscle weakness21–22 and altered motor coordination23 on this side. Goldie et al.13 reported that individuals with stroke could not weight-shift in a lateral or forward direction onto their non-paretic limb as well as healthy elderly subjects. Thus, the non-paretic, in addition to the paretic limb was evaluated in this study.
METHODS
Subject information
A convenient sample of chronic stroke survivors was used in this study. Subject characteristics of the study population are listed in Table 1. Ethics approval was acquired from the local university and hospital review boards. In accordance with the university and hospital policy and to protect the rights of the subjects, informed consent was received from all subjects prior to participation in this study. Inclusion criteria were:
Table 1.
Subject Characteristics (N=15)
| Mean | Standard Deviation | Range | |
|---|---|---|---|
| Gender (M/F) | 8/7 | ||
| Hemiparetic Side (L/R) | 6/9 | ||
| AHASFC* I/II/III | 8/6/1 | ||
| Age (years) | 58 | 11.8 | 31–78 |
| Time Since Stroke (years) | 3.8 | 3.8 | 1–10 |
| Mass (kg) | 71.5 | 13.5 | 52.3–98.3 |
| Height (cm) | 163.1 | 11.7 | 141–184 |
Abbreviations: AHASFC (American Heart Association Stroke Functional Classification Level)36
be a minimum of one year post-stroke
present with hemiparesis secondary to first cerebrovascular accident
able to provide informed consent
able to rise from a chair and stand independently for one minute
follow one and two step commands
have an activity tolerance of 30 minutes with rest intervals
Exclusion criteria
musculoskeletal or neurological conditions in addition to the stroke
Protocol
For each test session, the subject completed the following tasks in random order: 1) rise from a chair, 2) stand quietly, 3) shift body weight laterally to the right/left limb, 4) shift body weight forward to the right/left limb in a step stance posture, 5) shift body weight backward to the right/left limb in a step stance posture. Tasks 1 and 2 were bilateral weight-bearing tasks in that subjects could potentially use both limbs while tasks 3 to 5 were single limb weight-bearing tasks as the goal was to shift as much weight to one limb as possible. The instructions for the corresponding tasks were provided by the same person and were 1) rise from a chair as you would usually do except without using your arms, 2) stand as you usually do, 3) shift as much weight as possible sideways onto your right/left leg, 4) shift as much weight as possible forward onto your right/left leg, and 5) shift as much weight as possible backward onto your right/left leg. For the weight-shifting tasks (tasks 3,4,5), subjects were instructed to shift as much weight onto the one limb without lifting the other foot off the ground and to hold the final position for two seconds.
Five trials of each task were collected, with exception of the quiet standing task in which only two trials were collected. To minimize learning effects from the first to last trial, single trials of each task were performed with the tasks being presented in different sequences. Rests were provided as required by the subject.
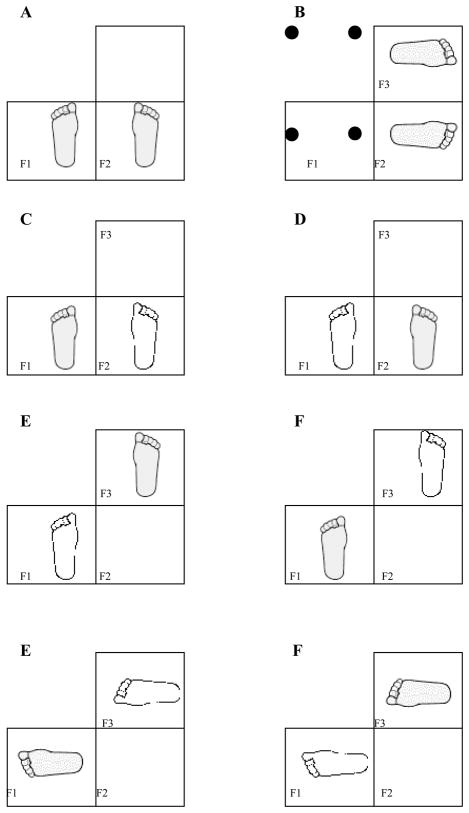
Subjects performed the tasks in bare feet. Three strain gauge force plates (Bertec)a embedded in the floor were used to measure limb loading. The subject placed his/her feet at a comfortable width on two of the force plates. The foot width was then held constant for all subsequent sessions and tasks for that subject (generally 15–20 cm between the feet). The foot position relative to the forceplates is shown in Figure 1. When rising from a chair, the third force plate was positioned under the subject’s chair in order to determine the time of lift-off of the subject’s buttocks from the chair. The same chair was used for each test session and for each subject. The amount of thigh support on the chair was measured from the first test session and kept constant across subsequent sessions for that individual. For the forward and backward weight-shift task, the heel of the front foot was aligned with the toe of the rear foot using the same foot width as in the other tasks (Figure 1).
Figure 1.
Figures A-H depict a top-down schematic view of the feet placement with respect to the forceplate location during the five tasks. The shaded foot represents the direction of maximal weight shifting during the unilateral tasks of lateral, forward, and backwards weight shifting. For the bilateral tasks, quiet standing and rising from a chair, both feet are shaded grey, as the task requires the individual to bear weight through both feet as equally as possible. The following figures depict the task and corresponding foot orientation: a) Quiet Standing, b) rising from a chair (4 legs of the chair are represented as black filled circles with subject’s feet on F2 and F3), c) lateral weight shift to the left foot, d) lateral weight shift to the right foot, e) forward weight shift to the right foot, f) backwards weight shift to the left foot, g) forwards weight shift to the left foot, and h) backwards weight shift to the right foot.
Data collection and reduction
Force plate data was sampled at 600 Hz for all trials and tasks. Thirty sec trials were collected for the quiet standing task and 6 sec trials for all other tasks using an analog-digital system (National Instruments)b. A Matlab software package (Mathworks, Inc)c was used to filter (second order, 50 Hz low pass filter), calibrate the vertical force plate data, identify frame ranges and force values, and calculate mean vertical forces over specified frame ranges. One person with no previous experience was trained to identify the appropriate window of data. The force plate under the chair was used to determine the time of lift-off when rising from the chair and the corresponding vertical force under the limb was determined. For the quiet standing and weight-shifting tasks, the most stable one sec duration of the vertical ground reaction force was windowed and averaged.
Statistical Analysis
Coefficients of variation (standard deviation/mean X 100)24 were calculated for the five trials for each subject for each condition as a measure of intrasubject trial variability. To assess the relative reliability between the two test sessions, mean vertical force values were input into a repeated measures analysis of variance (ANOVA) for each task and limb and the results were then used to calculate the intraclass correlation coefficients (ICCs, [1,1]).25 The ICC provides a measure of the relative position of the measurements within a group on repeated measurements.20 The absolute reliability was tested with 10 repeated measures ANOVAs (5 tasks X 2 limbs) to assess whether a significant difference existed between the means of the first and second test sessions26 and the standard error of the measurement (SEM) in Newtons provided a measure of the absolute reliability20 in the units of the instrument tool.
The single limb tasks (i.e., weight-shifting tasks) were also expressed as a percentage of body weight while the bilateral tasks (rising from a chair and quiet standing) were expressed as a percentage of one-half body weight. An ANOVA blocked for subject was used to assess differences for the absolute weight-bearing ability among the five tasks. This ANOVA was performed twice, once for the paretic and once for the non-paretic limb. Post-hoc tests were performed using the Tukey test.
Correlations were performed to determine the relationship between the weight-bearing ability among the five tasks using the Pearson Moment Product Correlation. All statistical analyses were performed with SPSS 8.0 for Windows (SPSS Inc.)d using an alpha value of 0.05.
RESULTS
The coefficients of variation (i.e., representing the within subject trial variability of the weight-bearing ability of each test session) were 5.2% ± 2.0 (mean ± one standard deviation) across all the conditions for the paretic limb (15 subjects, 5 tasks, 2 test session) and 3.4% ± 0.6 across all the conditions for the non-paretic limb. ICCs for the weight-bearing ability between the two test sessions were high for all five tasks for the paretic (0.93–0.99) and non-paretic limbs (0.95–0.99) (Table 2), which suggested that relative reliability was high and similar between the two limbs and across the different tasks. None of the F-tests for the repeated measures ANOVA comparing the means of the first and second test sessions were significant (p > 0.2), which established the absolute reliability of the data with the SEM ranging from 8.0 to 19.0 N for bilateral leg tasks (rising from a chair and quiet standing), and from 13.1 to 33.9 N for weight-shifting tasks. Thus, we can conclude that 68% of the time, a repeated measurement of weight-bearing ability would be within one standard deviation of the mean20, which is 2.2–4.6% of the original measurement for the non-paretic limb and 2.7 to 6.2% for the paretic limb. Given the excellent test-retest reliability of the data, further analyses involved data from only the first session.
Table 2.
Intraclass Correlations and standard error of the measurement (SEM)* in Newtons for standing tasks (N=15).
| Task | Paretic limb | Non-paretic limb |
|---|---|---|
| Rising from a chair | 0.99 (8.0) | 0.97 (16.2) |
| Quiet standing | 0.95 (19.0) | 0.95 (18.8) |
| Weight-shift Laterally | 0.93 (30.8) | 0.99 (13.1) |
| Weight-shift Forward | 0.96 (33.9) | 0.98 (20.2) |
| Weight-shift Backwards | 0.97 (18.0) | 0.98 (15.8) |
SEM in parentheses
As expected, the absolute weight-bearing ability was lower for the paretic limb compared to the non-paretic limb for all five tasks (Table 3). Asymmetry was particularly evident during the bilateral task of rising from a chair with the paretic limb bearing 296 N, which is equal to 83% of the expected weight through a single limb. This is in contrast to the non-paretic side which bore 458 N or 130% of the expected weight through a single limb. During bilateral tasks, the expected body weight through a single limb would be 50% of the total body weight. In contrast, the observed differences in weight bearing abilities between the paretic and non-paretic sides were not as pronounced for the remaining 4 tasks (differences between paretic and non-paretic limbs ranging between 7 to 30%, Table 3).
Table 3.
Absolute weight-bearing in Newtons (mean ± 1 standard deviation)* and corresponding normalized values (percent means ± 1 standard deviation)* for the standing tasks for test session one (N=15)
| Task | Paretic limb Absolute | Paretic limb Normalized | Non-paretic limb Absolute | Non-paretic limb Normalized | Difference† |
|---|---|---|---|---|---|
| Rising from a chair‡|| | 296.0 (95.5) | 83 (18) | 457.7 (85.6) | 130 (16) | 47 |
| Quiet standing‡ | 325.6 (79.7) | 85 (14) | 405.5 (78.2) | 115 (14) | 30 |
| Weight-shift Laterally | 521.8 (122.3)¶ | 72 (12)¶ | 602.6 (125.9) | 84 (6) | 12 |
| Weight-shift Forward | 445.7 (87.3) | 65 (11) | 520.5 (109.9)** | 72 (7)** | 7 |
| Weight-shift Backwards | 483.1 (104.2) | 68 (12) | 579.9 (109.7) | 81 (6) | 13 |
standard deviations represented in parentheses
Difference between paretic and non-paretic normalized values (i.e., asymmetry)
to normalize for differences in weight-bearing demands between single leg and bilateral limb, weight-bearing values for the single leg tasks were normalized by dividing by total body weight while values for the bilateral tasks (rising from a chair and quiet standing) were normalized by dividing by ½ of body weight
the sum of the paretic and non-paretic limb when rising from a chair is not necessarily the same as the quiet standing due to a small acceleration effect
significantly greater than weight-shift backwards and forwards for that limb, Tukey’s test, p < 0.05
significantly less than weight-shift backwards and lateral for that limb, Tukey’s test, p < 0.05
For both the paretic and non-paretic limbs, there was a significant task effect on weight-bearing ability (paretic: F(4,75)= 6.4, p< 0.001, ; non-paretic: F(4,75)=78.3, p< 0.001) and a discussion of the post-hoc results follows. The absolute weight measured for the bilateral limb tasks (rising from a chair and quiet standing) was significantly less than that recorded for the weight-shifting tasks since bilateral tasks demand the transfer of only one-half of body weight to each limb, while the weight-shifting tasks require the whole body weight to be transferred to a single limb. Thus, one might have expected the weight measured through a limb during the weight-shifting tasks to be close to double (200%) that of the bilateral tasks. However, the values between the bilateral and single limb tasks were not as dissimilar as one might have expected given the different task requirements. For example, on the paretic limb, the values during the forward weight-shift (mean 445.7 N) measured only 137% (not 200% as one might have expected) of the quiet standing values (mean 325.6 N). The weight bearing ability between the two bilateral tasks was significantly different from each other with the paretic limb bearing less weight when rising from a chair (mean 296.0 N) compared to quiet standing (mean 325.6 N). For the weight-shifting tasks, the greatest magnitude of weight was measured in the lateral, followed by backwards, and then forwards direction for both the paretic and non-paretic limbs. However, not all means were significantly different from each other. On the paretic limb, the post-hoc analyses demonstrated that the weight-bearing ability was significantly greater in the lateral direction compared to the backwards and forwards directions. For the non-paretic limb, the weight-bearing ability in the forwards direction was significantly lower compared to the backwards and lateral directions (Table 3).
The normalized values for the weight-shifting tasks (lateral, forward, backward) on the non-paretic limb did not reach the same magnitude as reported in healthy elderly subjects, i.e., 95% of body weight.13 In fact, in the forward direction the weight-shifting ability on the non-paretic limb (72% of body weight) was only slightly greater than that on the paretic limb (65% of body weight).
All the weight-bearing tasks were significantly related to each other (r=0.56 to 0.94, p < 0.001) (Table 3). Nine of the ten correlations were greater for the non-paretic limb compared to the paretic limb. Of interest, the lowest correlations involved the forward weight-shift task for the paretic limb.
DISCUSSION
Reliability of the weight-bearing ability
Although it has been well documented that weight-bearing abilities on the paretic limb are compromised, there has been a paucity of studies that examine the test-retest reliability of this measure across sessions in individuals with stroke. Studies have reported high within session reliability (consecutive trials) for forward and lateral weight- shifting in persons with stroke,13 good within session reliability (consecutive trials) for the body centre of mass displacement when transferring weight laterally into a single leg posture in persons with stroke,27 and good test-retest reliability measured over two separate days for the vertical ground reaction force for healthy adults when rising from a chair.8
Our study is the first to assess the reliability of weight-bearing abilities over different days in persons with chronic stroke. In addition, we established the reliability of weight-bearing in different postures and directions. We found that the within subject trial variability was low for a single test session as measured by the coefficients of variation, however, there was higher variability for the paretic limb compared to the non-paretic limb. The test-retest protocol performed over different days accounts for variability of 1) the forceplate instrumentation, 2) performance of the subject which could potentially be influenced by factors such as fatigue, motivation, selected posture, movement strategy and comprehension of the instructions and 3) performance of the evaluator to identify the appropriate window of data. The results of this study demonstrate that weight-bearing ability can be attained reliably over separate days in individuals with chronic stroke for both the paretic and non-paretic limbs. Weight-bearing reliability was high and similar for both limbs, despite the lower weight measured through the paretic limb. A well-defined clinical protocol which standardized the instructions, foot positioning, and thigh placement (when rising from a chair) may have promoted high reliability in these individuals who have had a stroke. The absolute and relative reliability of this data, coupled with the established validity from the literature15,16,28 suggest that this measure may be a useful outcome measure in individuals with stroke.
Effect of task on weight-bearing ability
Functional mobility requires weight-bearing in a variety of postures and directions. Thus, a major focus of rehabilitation is to increase the tolerance and ability to bear weight on the paretic limb during various functional tasks.18,19 The results from our study indicate that the magnitude of weight bearing ability measured through a single limb while standing is dependent on the specific task.
Bilateral weight-bearing versus single-limb weight-shifting tasks
Interestingly, although subjects can shift well over one-half their body weight onto the paretic limb during a voluntary weight-shift in any direction, they bear under one-half their body weight through the paretic limb during the static task of standing or dynamic task of rising from a chair. Unlike the voluntary weight-shift where there is a concerted effort to load the paretic limb, the subject can compensate with the non-paretic limb and reduce the load of the paretic limb when rising from a chair and quiet standing. When given this choice it appears that subjects do not bear the weight that they are capable of. This trend has been observed in acute,1–4,6 subacute,5 and now chronic stroke survivors, although the degree of asymmetry during bilateral tasks appear to be greater in the acute stroke population. In addition, our observation is consistent with the findings that individuals with stroke can distribute their weight more symmetrically when requested to rise from a chair with their body weight distributed evenly on both feet8 and provides further support for the undertaking of interventions to improve symmetry during functional tasks.6,7
Weight-bearing on bilateral limbs
Why was the ability to weight-bear through the paretic limb when rising from a chair more impaired than that of quiet standing? Engardt and Olsson8 reported that the degree of sensory function did not influence the symmetry of weight-bearing of individuals with stroke when rising from a chair. However, large demands are placed on the knee musculature when rising from a chair where up to 87% of available knee strength is used in older adults.29,30 The poor weight-bearing ability when rising from a chair may be a result of the important concentric knee muscle component specific to this task, coupled with the very weak paretic knee musculature which has been reported previously in individuals with stroke.31 In addition, rising from a chair is a dynamic task which requires that force be generated quickly which may be challenging as a reduced rate of force generation has been documented with the paretic muscles in individuals with stroke.32 The lower than expected weight measured through the paretic limb when rising from a chair is cause for concern as this asymmetry may contribute to falls. Cheng et al.14 found that body weight distribution was more asymmetrical for individuals with stroke with a history of falling than those who did not, although the difference did not reach statistically significant levels.
Weight-shifting to a single-limb
The weight-shifting ability was particularly low for the paretic limb in the forward direction. We observed that subjects generally flexed the front knee during the forward weight-shift which would require eccentric knee control and could be challenging for individuals with stroke. However, given that both the paretic and non-paretic limbs could shift the most weight in the lateral, followed by backward and then forward direction, it also suggests that each task poses different challenges. During the lateral weight-shift subjects may rely partly on the passive hip and knee structures, in addition to the inherent stiffness of the trunk and sacroiliac structures in this plane.33 The forward and backward weight shift may be more challenging as there is more motion available in the hip and trunk in the sagittal plane, which requires greater control of the top heavy body mass. In addition, the forward and backward weight-shift tasks involve more than one plane of motion as the step stance posture will require control of a lateral shift to the weight-bearing limb in addition to the sagittal motion.
Why was the weight-shift more difficult in the forward, as opposed to backward direction? Goldie et al.12 reported that weight-shifting ability was more difficult in the backward, as opposed to forward direction when the feet were in a parallel, side-by-side position. In this foot position, the short moment arm between the ankle joint and the posterior heel would make it difficult to bear weight in the backward direction. In the step stance posture, the eccentric knee control required to maintain the observed flexed knee posture of the leading limb may result in a more difficult task compared to the backwards weight-shift, where subjects were observed to extend both the hip and knee of the weight-bearing limb and possibly rely more on passive structures (e.g., posterior capsule of the knee and posterior hip ligaments). The difficulties in weight-shifting forward could also be due to differences in ability (both perceived and actual ability) to control the forward trunk motion compared to a backward motion.
Non-paretic weight-bearing ability
As expected, the non-paretic limb demonstrated greater weight-bearing ability for all five tasks, especially when rising from a chair and quiet standing where the non-paretic limb must compensate for the paretic limb. These results concur with previous studies which have reported significantly higher weight bearing abilities of the non-paretic limb compared to the paretic limb during these tasks.13,21 However, values for the non-paretic limb during the weight-shifting tasks were not close to that of healthy elderly, particularly for the forward weight-shift.13 Goldie et al.13 reported that healthy elderly individuals were able to weight-shift 95% of their body weight in all directions (i.e. forward, backwards, laterally) for both legs. In contrast, individuals with stroke were only able to weight-bear 85% and 80% of their total body weight in the lateral and forwards directions, respectively, on their non-paretic limb. These values are similar to what was observed in the present study. Given this information, the performance of the non-paretic side should not be used as the criterion against which the paretic side is evaluated because this would underestimate the deficit on the paretic side.
What might be the cause of the deficits on the non-paretic limb? Adams et al.34 suggested that motor deficits on the non-paretic side might reflect the loss of effective ipsilateral corticofugal projections to the lower limb muscle. This hypothesis is supported by reports that weakness is bilateral following stroke.21,22,34 However, other factors such as reduced physical activity, fear of falling, and impaired postural control likely play a role as well. These results suggest that function of the non-paretic limb should not be overlooked.
Relationship of weight-bearing tasks
Although the magnitude of weight-bearing is significantly different among the tasks, the relationship among the tasks is positive and moderate to strong in all cases. Thus, subjects with low weight-bearing ability in one task had low weight-bearing ability in another task. This is reasonable since all the tasks required postural stability in an upright position (i.e., controlling the body’s centre of mass within the base of support)35 and muscle strength, particularly of the antigravity muscles to load the limb. The lowest correlations involved forward weight-shifting on the paretic limb and suggest that this task may have components (e.g., eccentric knee control) which are not related to the other tasks. Given the strong relationship among the tasks, it is not surprising that others have found that improvements in weight-bearing abilities in one task result in improvements to other weight-bearing tasks. For example, Dean and Shephard17 reported that loading the paretic limb, which accompanies the practice of a forward reach task while sitting, resulted in improved ability to rise from a chair in individuals with stroke. Winstein et al.6 found that weight-shifting exercises resulted in better weight-bearing symmetry while standing.
Limitation and clinical significance of the study
We provided instructions which allowed subjects to perform the movement as they felt comfortable, rather than constrain the task with more specific instructions. We felt that further standardization of the posture may reduce the generalizability of the outcome measures to natural behavior. For example, some subjects needed to rock back and forth several times to gain momentum to stand up from the chair, while some subjects used substantial knee flexion of the leading limb during the forward weight shift. Thus, although the results are reliable in that each subject replicated their performance, it does not imply that all subjects used the same movement strategies to perform the task. Since the forceplate measures the whole body acceleration, one cannot determine the actions of individual segments. On the other hand, the vertical ground reaction force provides a continuous measure of weight-bearing ability and whole body postural stability without any attachment of cables or markers to the subject and thus subject preparation and inconvenience are minimal.
Given the major focus of rehabilitation to increase the tolerance and ability to bear weight on the paretic limb during various functional tasks,18,19 one can now justifiably use weight-bearing ability as a reliable outcome measure in neurological rehabilitation. Furthermore, clinicians can expect that the magnitude of weight-bearing to differ across tasks due to the posture and direction of weight-bearing, in addition to the interaction of stroke-specific impairments. The strong relationship among the tasks is likely due to the involvement of postural stability and muscle strength in all these tasks. This study only examined weight-bearing ability at one point in time, while outcome measures are generally evaluated over time to assess the change from treatment interventions. Thus, it would be useful for future studies to determine the extent that improvements in weight-bearing ability in one standing task relate to improvements to other standing tasks.
Table 4.
Correlational analysis for standing tasks for test session one (N=15)
| Standing Balance | Weight-shift Laterally | Weight-shift Forward | Weight-shift Backward | |
|---|---|---|---|---|
| PARETIC LIMB | ||||
|
| ||||
| Rising from a chair | 0.739 | 0.783 | 0.665 | 0.626 |
| Quiet standing | 0.893 | 0.556 | 0.692 | |
| Weight-shift Laterally | 0.709 | 0.817 | ||
| Weight-shift Forward | 0.688 | |||
|
| ||||
| NON-PARETIC LIMB | ||||
|
| ||||
| Rising from a chair | 0.745 | 0.814 | 0.877 | 0.773 |
| Quiet standing | 0.746 | 0.744 | 0.778 | |
| Weight-shift Laterally | 0.888 | 0.939 | ||
| Weight-shift Forwards | 0.833 | |||
All correlations significant at p < 0.001
Acknowledgments
Financial Support: BC Health Research Foundation, Grant-in-Aid from the Heart and Stroke Foundation of BC and Yukon and the Canadian Institute of Health Research (operating grant # 57862).
Footnotes
Bertec Corporation, 6185 Huntley Rd, Columbus, OH, 43229
National Instruments Corporation, 11500 N Mopac Expwy, Austin, TX, 78759-3504
MathWorks Inc., 3 Apple Hill Drive, Natick, MA, 01760-2098
SPSS Inc., 233 S. Wacker Dr., Chicago, IL, 60606
References
- 1.Dickstein R, Nissan M, Pillar T, Scheer D. Foot-ground pressure pattern of standing hemiplegic patients: Major characteristics and patterns of improvement. Phys Ther. 1984;64:19–23. doi: 10.1093/ptj/64.1.19. [DOI] [PubMed] [Google Scholar]
- 2.Laufer Y, Dickstein R, Resnik S, Marcovitz E. Weight-bearing shifts of hemiparetic and healthy adults upon stepping on stairs of various heights. Clin Rehabil. 2000;14:125–129. doi: 10.1191/026921500674231381. [DOI] [PubMed] [Google Scholar]
- 3.Mizrahi J, Solzi P, Ring H, Nisell R. Postural stability in stroke patients: Vectorial expression of asymmetry, sway activity and relative sequence of reactive forces. Med & Biol Eng & Comput. 1989;27:181–190. doi: 10.1007/BF02446228. [DOI] [PubMed] [Google Scholar]
- 4.Sackley CM. The relationships between weight-bearing asymmetry after stroke, motor function and activities of daily living. Physiother Theory Prac. 1990;6:179–185. [Google Scholar]
- 5.Shumway-Cook A, Anson D, Haller S. Postural sway biofeedback: Its effect on reestablishing stance stability in hemiplegic patients. Arch Phys Med Rehabil. 1988;69:395–400. [PubMed] [Google Scholar]
- 6.Winstein CJ, Gardner ER, McNeal DR, Barto PS, Nicholson DE. Standing balance training: Effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil. 1989;70:755–762. [PubMed] [Google Scholar]
- 7.Engardt M. Rising and sitting down in stroke patients. Auditory feedback and dynamic strength training to enhance symmetrical body weight distribution. Scand J Rehabil Med. 1994;31 (Suppl 1):3–54. [PubMed] [Google Scholar]
- 8.Engardt M, Olsson E. Body weight-bearing while rising and sitting down in patients with stroke. Scand J Rehabil Med. 1992;24:67–74. [PubMed] [Google Scholar]
- 9.Hesse S, Schauer M, Petersen M, Jahnke M. Sit-to-stand manoevre in hemiparetic patients before and after a 4-week rehabilitation programme. Scand J Rehabil Med. 1998;30:81–86. doi: 10.1080/003655098444174. [DOI] [PubMed] [Google Scholar]
- 10.Bohannon R, Larkin P. Lower extremity weightbearing under various standing conditions in independently ambulatory patients with hemiparesis. Phys Ther. 1985;65:1323–5. doi: 10.1093/ptj/65.9.1323. [DOI] [PubMed] [Google Scholar]
- 11.Dickstein R, Dvir Z, Jehosua EB, Rois M, Pillar T. Automatic and voluntary lateral weight shifts in rehabilitation of hemiparetic patients. Clin Rehabil. 1994;8:91–99. [Google Scholar]
- 12.Goldie PA, Evans O, Matyas TA. Performance in the stability limits test during rehabilitation. Gait & Posture. 1996;4:315–322. [Google Scholar]
- 13.Goldie PA, Matyas TA, Evans OM, Galea M, Bach TM. Maximum voluntary weight-bearing by the affected and unaffected legs in standing following stroke. Clin Biomech. 1996;11:333–342. doi: 10.1016/0268-0033(96)00014-9. [DOI] [PubMed] [Google Scholar]
- 14.Cheng P, Liaw M, Wong M, Tang F, Lee MY, Lin PS. The sit-to-stand movement in stroke patients and its correlation with falling. Arch Phys Med Rehabil. 1998;79:1043–1046. doi: 10.1016/s0003-9993(98)90168-x. [DOI] [PubMed] [Google Scholar]
- 15.Sackley CM. Falls, sway, and symmetry of weight-bearing after stroke. Int Disabil Studies. 1991;13:1–4. doi: 10.3109/03790799109166267. [DOI] [PubMed] [Google Scholar]
- 16.Dettman MA, Linder MT, Sepic SB. Relationships among walking performance, postural stability, and functional assessments of the hemiplegic patient. Am J Phys Med. 1987;66:77–90. [PubMed] [Google Scholar]
- 17.Dean CM, Shephard RB. Task-related training improves performance of seated reaching tasks after stroke. Arch Phys Med Rehabil. 1997;28:722–728. doi: 10.1161/01.str.28.4.722. [DOI] [PubMed] [Google Scholar]
- 18.Carr JH, Shepherd RB. Neurological rehabilitation: optimizing motor performance. Boston: Butterworth-Heinemann; 1998. [Google Scholar]
- 19.Umphred DA. Neurological Rehabilitation. 3. St. Louis: Mosby; 1995. [Google Scholar]
- 20.Domholdt ED. Principles and Applications. Philadelphia: WB Saunders; 2000. Physical Therapy Research. [Google Scholar]
- 21.Bohannon RW, Andrews AW. Limb muscle strength is impaired bilaterally after stroke. J Phys Ther Sci. 1995;7:1–7. [Google Scholar]
- 22.Sjostrom M, Fugl-Meyer AR, Nordin G, Wahlby L. Post-stroke hemiplegia; crural muscle strength and structure. Scand J Rehabil Med. 1980;7:53–67. [PubMed] [Google Scholar]
- 23.Desrosiers J, Bourbonnais D, Bravo G, Roy PM, Guay M. Performance of the ‘unaffected’ upper extremity of elderly stroke patients. Stroke. 1996;27:1564–70. doi: 10.1161/01.str.27.9.1564. [DOI] [PubMed] [Google Scholar]
- 24.Rosner B. Fundamentals of Biostatistics. Pacific Grove: Duxbury Press; 2000. [Google Scholar]
- 25.Strout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 26.Verducci FM. Measurement Concepts in Physical Education. St. Louis: CV Mosby Co; 1980. [Google Scholar]
- 27.Pai Y, Rogers MW, Hedman LD, Hanke TA. Alterations in weight-transfer capabilities in adults with hemiparesis. Phys Ther. 1994;74:647–659. doi: 10.1093/ptj/74.7.647. [DOI] [PubMed] [Google Scholar]
- 28.Bohannon RW. Gait performance of hemiparetic stroke patients: selected variables. Arch Phys Med Rehabil. 1987;68:777–781. [PubMed] [Google Scholar]
- 29.Alexander NB, Schultz AB, Ashton-Miller JA, Gross MM, Giordani B. Muscle strength and rising from a chair in older adults. Muscle & Nerve. 1997;20 (Suppl 5):S56–S59. [PubMed] [Google Scholar]
- 30.Hughes MA, Myers BS, Schenkman ML. The role of strength in rising from a chair in the functionally impaired elderly. J Biomech. 1996;29:1509–1513. [PubMed] [Google Scholar]
- 31.Sunnerhagen KS, Svantesson U, Lonn L, Krotkiewski M, Grimby G. Upper motor neuron lesions: Their effect on muscle performance and appearance in stroke patients with minor motor impairment. Arch Phys Med Rehabil. 1999;80:155–161. doi: 10.1016/s0003-9993(99)90113-2. [DOI] [PubMed] [Google Scholar]
- 32.Canning CG, Ada L, O’Dwyer N. Slowness to develop force contributes to weakness after stroke. Arch Phys Med Rehabil. 1999;80:66–70. doi: 10.1016/s0003-9993(99)90309-x. [DOI] [PubMed] [Google Scholar]
- 33.White AA, Panjabi MM. Clinical biomechanics of the spine. 2. Philadelphia: Lippincott; 1990. [Google Scholar]
- 34.Adams RW, Gandevia SC, Skuse NF. The distribution of muscle weakness in upper motoneuron lesions affecting the lower limb. Brain. 1990;113:1459–1476. doi: 10.1093/brain/113.5.1459. [DOI] [PubMed] [Google Scholar]
- 35.Shumway-Cook A, Woollacott MH. Motor control: Theory and Applications. Baltimore: Williams and Wilkins; 1995. [Google Scholar]
- 36.Kelly-Hayes M, Robertson JT, Broderick JP, Duncan PW, Hershey LA, Roth EJ, Thies WH, Trombly CA. The American Heart Association Stroke Outcome Classification. Stroke. 1998;29:1274–1280. doi: 10.1161/01.str.29.6.1274. [DOI] [PubMed] [Google Scholar]