Abstract
This analysis investigates changes in spatial access to safety-net primary care in a sample of US public housing residents relocating via the HOPE VI initiative from public housing complexes to voucher-subsidized rental units; substance misusers were oversampled. We used gravity-based models to measure spatial access to care, and used mixed models to assess pre-/post-relocation changes in access. Half the sample experienced declines in spatial access of ≥79.83%; declines did not vary by substance misuse status. Results suggest that future public housing relocation initiatives should partner with relocaters, particularly those in poor health, to help them find housing near safety-net clinics.
Keywords: Public housing, HOPE VI, spatial access to health care, geospatial measures, safety net primary care
There is resurging interest in the ways that features of urban environments influence the health and well-being of urban populations. (Diez Roux, 2007) With notable exception (e.g., Fauth et al., 2004;Wallace, 1990), however, this research typically treats these features as static and ignores population mobility. Social policies and other urban processes (e.g., urban renewal initiatives, gentrification) can transform urban environments and precipitate mass migration, particularly of impoverished and minority households. (Massey and Denton, 1993;Rae, 2003) In the USA, the “Housing Opportunities for People Everywhere” (HOPE) VI initiative is one such policy. HOPE VI demolishes public housing complexes, a prominent feature of many urban environments, and catalyzes mass migrations of public housing residents. At issue in this short report is whether and how HOPE VI affects relocaters’ spatial access to safety-net primary care.
HOPE VI
The USA is experiencing a paradigm shift in public housing policy.(Goetz, 2003) After decades of pursuing policies that spatially concentrated public housing units into high-rises and campuses, the US Department of Housing and Urban Development (HUD) and local public housing authorities now seek to dismantle these complexes and disperse residents to other neighborhoods.(Goetz, 2003) This shift was precipitated by concerns that concentrated poverty was detrimental to public housing residents and to their neighbors, and impeded urban development. (Department of Housing and Urban Development, 2008;Popkin et al., 2002)
HOPE VI has been the primary policy driving this urban transformation. Enacted in 1992, HOPE VI funds the relocation of all residents of “severely distressed” complexes to voucher-subsidized rental units in the private market; the demolition of distressed complexes; and the revitalization of sites where complexes were located.(Popkin et al., 2004) “Severely distressed” complexes have high rates of crime or poverty; contribute to local socioeconomic decline; or are in extreme disrepair.(Popkin et al., 2004)
HOPE VI relocaters tend to move to voucher-subsidized rental units that are located in neighborhoods with lower rates of poverty and violent crime and less drug activity than their original neighborhood.(Popkin et al., 2004) The extent of these improvements, however, is not experienced uniformly across relocaters. Residents in poor health, including those who misuse substances, are HIV infected, or have chronic diseases, experience more modest improvements in post-relocation neighborhood conditions.(Popkin et al., 2004) This unevenness is significant because high proportions of public housing residents are in poor health. (Popkin et al., 2004) For example, Simning et al. (2011) found that the 12-month prevalence of substance use disorders was more than twice as high among African-American public housing residents than it was among other African-American urban residents, controlling for sociodemographic characteristics.
Spatial Access to Safety Net Primary Care
Primary care is the foundation of an effective and responsive healthcare system: it provides primary prevention, enhances opportunities for early disease detection, and improves the efficiency of the healthcare system as a whole. (Committee on the Future of Primary Care, 1996) Primary care is particularly important for active substance misusers, who have high rates of physical and mental health problems (e.g., sexually-transmitted infections, depression).(Weisner et al., 2001) Notably, spatial access to primary care clinics influences service use.(Arcury et al., 2005;Continelli et al., 2010;Nemet and Bailey, 2000) Spatial access to safety-net primary care clinics may be particularly important for linking impoverished individuals to care; the Institute of Medicine (IOM) defines safety-net care clinics as “providers that organize and deliver a significant level of health care and other health-related services to uninsured, Medicaid, and other vulnerable patients”.(p. 3, Committee on the Changing Market, 2000)
In the present analyses, we tested the hypothesis that HOPE VI relocaters in Atlanta, GA (USA) experienced declines in spatial access to safety-net primary care clinics after they moved. A move to a less impoverished neighborhood may also be a move to an area with fewer resources for poor families, including safety-net care. We also investigated whether the magnitude of changes in spatial access to safety-net care varied by relocaters’ baseline substance misuse status, and by other baseline health status indicators.
Methods
Sample and Recruitment
To be eligible to take part in the study, individuals had to live in one of the seven Atlanta Housing Authority (AHA) complexes targeted for relocation and demolition by HOPE VI in 2008–2009; be an African-American adult (≥18 years old); have been sexually active in the past year; and not live with a current study participant. Given the project’s overarching interest in investigating the impact of relocations on substance misusers’ health, we used quota sampling to create a cohort that was diverse with regard to substance misuse at baseline. Specifically, we sought to create a sample in which 25% of participants met screening criteria for alcohol or drug dependence; 50% misused substances but were not dependent; and 25% did not misuse substances at baseline. Because data collection began after relocations had started, we could not use random sampling or respondent-driven sampling to create the cohort. The sample was created using a variety of recruitment methods, including consistent staff presence within each of the seven complexes targeted by HOPE VI; peer recruitment; and partnering with community-based organizations near each complex that served substance misusers. Interested individuals were screened for eligibility.
We report here on data collected at baseline (i.e., pre-relocation) and Wave 2. Baseline data were gathered in 2009, and Wave 2 data collection occurred approximately 9 months later. 172 participants completed baseline interviews; 163 of these individuals completed Wave 2 interviews. These analyses pertain to the 160 participants who completed Wave 2 interviews and lived in the Atlanta metropolitan area at Wave 2.
Measures
We assessed potential spatial access to safety-net primary care clinics at baseline and Wave 2 using gravity-based models (GBMs). GBMs measure spatial access as:
where Cijl is the travel distance between participant i ’s residence and clinic j at wave l; b is a distance decay formula that allows access to decline as distance increases; and Wjl is the service capacity at clinic j at wave l (Iacono et al., 2008) We calculated Cijl in three stages:
Stage 1: At each wave, we geocoded each participant’s home address to its longitude/latitude.
Stage 2: We created inventories of all safety-net primary care clinics operating in the Atlanta metro area at baseline and Wave 2 by reviewing federal, state, and local rosters of public clinics and consulting with local experts. We called each clinic to verify that it met the IOM definition of a “safety-net clinic”. That is., it (1) accepted Medicaid for all patients, and (2) either provided free services or had a sliding scale for the uninsured or for costs not covered by insurance. We created inventories of safety-net clinics for baseline and Wave 2, and geocoded their addresses.
Stage 3: We calculated Cijl for all residence/clinic pairs that were within a “reasonable travel distance” of one another. We calculated two versions of “reasonable travel distance”, one assuming that people drove to care and the other assuming that they took public transportation. To calculate these two variants of “reasonable travel distance” we analyzed participant responses to baseline questions about travel time and mode of transportation to their usual source of care. The mean travel time was 38 minutes for people who drove to care. We translated travel time to distance by calculating the distance one could travel in 38 minutes on the local road network at the local speed limit from each participant’s home. The mean travel time was 23 minutes for people who took public transportation. The average distance one could travel on the public transportation network is 2.44 miles, as determined by multiple trials on Hopstop™ from eight randomly-selected participants’ homes.
Service capacity (Wjl ) can be operationalized as the number of providers delivering healthcare services at each site. The high number of volunteer and part-time providers at each clinic, however, prevented clinics from estimating the number of providers, and so we set Wjl to 1.00. Based on Schuurman et al. (2010) we used two values of b, 1.5 and 2.0; lower values of b generate lower access values to sites that are farther away. We therefore calculated four GBM-based estimates of spatial access for each participant at each wave, reflecting the two possible modes of transportation and two possible b s. Higher GBM values indicate better access.
GBMs produce unitless results and so are difficult to interpret intuitively. We therefore complemented these GBM-based measures with access measures that simply captured the distance between each residence and the closest clinic at each wave of data collection.
Individual sociodemographic characteristics and health status were ascertained at baseline using surveys. Substance dependence was assessed using the TCU Drug Screen II. (TCU Institute of Behavioral Research, 2006) A global measure of self-rated health from the SF-12 was used to assess general health status.(Ware et al., 1996) HIV serostatus was ascertained via self report.
Analysis
We calculated measures of central tendency and dispersion for each of the spatial access measures at baseline and at Wave 2, and for the percent change in each of these measures over time. We used mixed models that included random coefficients for the intercept and time to test whether changes in access differed from zero, and whether changes in access varied by baseline health status.
Results
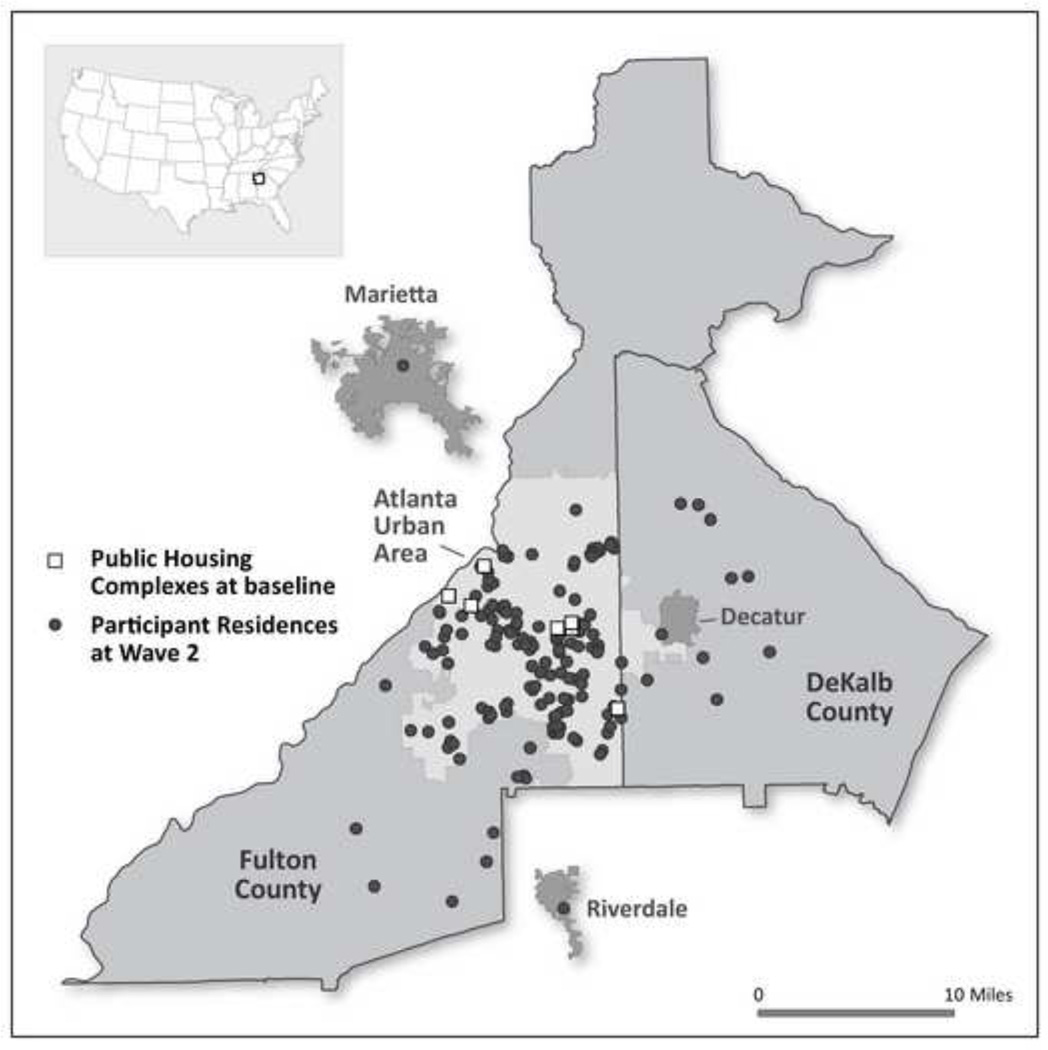
Fifty-seven percent of participants were women and the median annual income in the sample was $7,500 (Table 1). At baseline approximately 20% of participants were substance dependent, 30% reported that they were in poor to fair health, and 9% reported that they were HIV-positive. Almost all participants moved to homes within the city of Atlanta (Figure 1); the median distance between each participant’s housing complexes and his/her new home was 5 miles.
Table 1.
Sociodemographic characteristics, baseline health status, and distance migrated in a sample of African-American adults (n=160) relocating via HOPE VI in Atlanta, GA (USA)
| Characteristic | % (N) or median (25th
percentile, 75thpercentile) |
|---|---|
| Woman | 56.88% (91) |
| Age (years) | 46 (30,54) |
| Annual household income | $7,500 ($2,500, $12,500) |
| Dependent on alcohol or other drugs | 20.63% (33) |
| Health Status (self-rated) | |
| Excellent/Very Good | 35.00% (56) |
| Good | 34.38% (55) |
| Fair/Poor | 30.00% (48) |
| HIV positive (self-report) | 9.38% (15) |
| Distance between public housing complex and new home (miles) | 5.17 (2.78, 8.12) |
| Public housing complex at baseline | |
| Bankhead | 13.13% (21) |
| Thomasville | 15.00% (24) |
| Bowen Homes | 9.38% (15) |
| Hollywood Court | 11.25% (18) |
| Herndon Homes | 13.13% (21) |
| Palmer House | 21.88% (35) |
| Roosevelt House | 16.25% (26) |
Figure 1.
Spatial distributions of the public housing complexes where participants (n=160) lived at Wave 1 and of their homes after they relocated.1
1The locations of the Wave 2 addresses were jittered to preserve participant anonymity.
Participants experienced sharp declines in spatial access to safety-net primary care after relocating, regardless of how access was measured (Table 2). When access was measured as distance to the closest safety-net primary care clinic, our results suggest that at baseline half the sample lived <0.5 miles from such a clinic; at Wave 2, half the sample lived <2.00 miles from such a clinic. When we used GBM-based measures and set b =1.50, half of the participants taking public transportation to care experienced declines in access of ≥79.83%; people who drove to care experienced slightly steeper declines. Access estimates were higher when b =2.00, and declines in access were more modest. Mixed models indicate that the absolute decline in access differed significantly from zero (Table 3; results were similar across access measures, and so we present only results for public transportation when b =1.5; results of other models are available upon request to the first author). Regardless of the access measure used, mixed models also suggest that pre-/post-relocation changes in access did not vary according to baseline substance dependence or by self-rated health; we could not test the relationship between HIV status and change in access because so few people self-reported HIV-positive serostatus.
Table 2.
Changes in spatial access to safety net primary care in a cohort of adults (N=160) relocating from public housing in Atlanta, GA via the HOPE VI initiative, as measured using five different methods of measuring spatial access
| Gravity-based measure: Driving to care, beta=1.5 Median (25th, 75thpercentile) |
Gravity-based measure: Public transportation to care, beta=1.5 Median (25th, 75thpercentile) |
Gravity-based measure: Driving to care, beta=2.0 Median (25th, 75thpercentile) |
Gravity-based measure: Public transportation to care, beta=2.0 Median (25th, 75thpercentile) |
Distance Measure (miles): Median (25th , 75thpercentile) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 | Wave 2 | % change | Wave 1 | Wave 2 | % change | Wave 1 | Wave 2 | % change | Wave 1 | Wave 2 | % change | Wave 1 | Wave 2 | % change | |
| Total Sample | 0.73 (0.62, 0.99) |
0.12 (0.00, 0.35) |
−86.22 (−100.0, −55.71) |
0.80 (0.63, 1.03) |
0.15 (0.03, 0.44) |
−79.83 (−97.84, −39.50) |
1.26 (0.78, 1.52) |
0.20 (0.00, 0.55) |
−81.00 (−100.0, −44.14) |
1.44 (0.82, 1.73) |
0.35 (0.08, 0.79) |
−69.11 (−94.36, −22.67) |
0.47 (0.03, 1.07) |
1.94 (1.01, 3.08) |
239.95 (21.61, 1742.55) |
| Alcohol/drug Dependent | 0.73 (0.62, 0.94) |
0.04 (0.00, 0.27) |
−95.07 (−100.0, −63.41) |
0.80 (0.63, 1.01) |
0.08 (0.02, 0.34) |
−82.62 (−98.33, −35.52) |
0.99 (0.78, 1.52) |
0.09 (0.00, 0.49) |
−93.45 (−100.0, −65.91) |
1.16 (0.82, 1.73) |
0.22 (0.07, 0.66) |
−71.86 (−95.30, −11.75) |
1.05 (0.42, 1.07) |
2.41 (1.24, 3.38) |
210.33 (24.29, 886.92) |
| Not alcohol/drug dependent | 0.94 (0.71, 0.99) |
0.12 (0.00, 0.36) |
−84.57 (−100.0, −50.94) |
1.01 (0.74, 1.03) |
0.15 (0.03, 0.45) |
−78.94 (−96.97, −40.52) |
1.26 (0.88, 1.52) |
0.21 (0.00, 0.61) |
−79.00 (−100.0, −40.51) |
1.44 (0.99, 1.73) |
0.35 (0.09, 0.90) |
−64.50 (−94.30, −27.76) |
0.47 (0.03, 1.07) |
1.93 (0.97, 2.92) |
244.80 (18.93, 2619.85) |
| HIV positive (self report) |
0.73 (0.73, 0.94) |
0.06 (0.00, 0.88) |
−94.13 (−100.0, −40.46) |
0.80 (0.80, 1.01) |
0.07 (0.02, 0.95) |
−91.53 (−97.99, −41.53) |
1.26 (1.26, 1.52) |
0.11 (0.00, 1.07) |
−92.53 (−100.0, −30.25) |
1.44 (1.44, 1.73) |
0.16 (0.07, 1.44) |
−88.93 (−95.30, −32.92) |
1.05 (0.47, 1.07) |
2.17 (0.97, 3.31) |
210.33 (24.29, 274.32) |
| HIV negative (self report) |
0.84 (0.62, 0.99) |
0.12 (0.00, 0.35) |
−84.57 (−100.0, −56.15) |
0.91 (0.63, 1.03) |
0.15 (0.03, 0.44) |
−78.94 (−97.04, −39.11) |
0.99 (0.78, 1.52) |
0.21 (0.00, 0.55) |
−80.25 (−100.0, −44.71) |
1.16 (0.82, 1.73) |
0.35 (0.09, 0.79) |
−64.77 (−90.58, −20.98) |
0.47 (0.03, 1.07) |
1.93 (1.01, 3.04) |
258.90 (18.93, 2619.85) |
| Self-rated poor health | 0.94 (0.71, 0.94) |
0.12 (0.00, 0.34) |
−85.22 (−100.0, −63.41) |
1.01 (0.74, 1.01) |
0.17 (0.03, 0.38) |
−79.46 (−96.89, −62.74) |
1.26 (0.88, 1.52) |
0.23 (0.00, 0.52) |
−81.00 (−100.0, −65.91) |
1.44 (0.99, 1.73) |
0.41 (0.09, 0.64) |
−70.21 (−94.24, −55.17) |
1.05 (0.42, 1.07) |
1.92 (1.16, 2.96) |
164.32 (18.14, 472.17) |
| Self-rated excellent/good health | 0.73 (0.62, 0.99) |
0.10 (0.00, 0.39) |
−86.22 (−100.0, −49.33) |
0.80 (0.63, 1.03) |
0.15 (0.03, 0.46) |
−79.83 (−97.89, −33.85) |
0.99 (0.78, 1.52) |
0.20 (0.00, 0.62) |
−80.14 (−100.0, −34.99) |
1.16 (0.82, 1.73) |
0.35 (0.07, 0.89) |
−64.77 (−94.64, −11.75) |
0.47 (0.03, 1.07) |
1.96 (0.98, 3.31) |
299.96 (24.29, 5530.56) |
Table 3.
Results of mixed models regressing post-relocation spatial access to safety net primary care on measures of baseline health status, pre-relocation spatial access to safety net primary care, and time in a sample of HOPE VI relocaters in Atlanta, GA (N=160)
| Model 1Y coefficient (SE) |
Model 2¥ coefficient (SE) |
|
|---|---|---|
| Fixed Effects | ||
| Intercept | 0.82*** | 0.78*** |
| (0.19) | (0.19) | |
| Time | −0.55*** | −0.54*** |
| (0.16) | (0.16) | |
| Alcohol/drug dependence | −0.05 | |
| (0.04) | ||
| Self-rated health | 0.04 | |
| (0.03) | ||
| Variance Components | ||
| Intercept | 0.24* | 0.24* |
| (0.14) | (0.04) | |
| Rate of change | 0.16* | 0.16 |
| (0.10) | (0.10) | |
| Residual | 0.07*** | 0.07*** |
| (0.01) | (0.01) |
In Model 1, post-relocation spatial access to clinics was regressed on baseline access, time, and baseline substance dependence. Spatial access to care is measured assuming that participants took public transportation to care, and that the distance decay was beta =1.5.
In Model 2, post-relocation spatial access to clinics was regressed on baseline access, time, and baseline self-rated general health status. Spatial access to care is measured assuming that participants took public transportation to care, and that the distance decay was beta =1.5.
p<0.05
p<0.001
p<0.0001
Discussion
Our findings suggest that HOPE VI residents in Atlanta experienced substantial declines in spatial access to safety-net primary care after they relocated. The median distance to the nearest safety net clinic increased from approximately 0.5 miles to 2.00 miles. The median decline in spatial access to care as measured using GBM methods ranged from 69%–86%, depending on the measure. The “severely distressed” public housing complexes targeted by HOPE VI in Atlanta were often located in neighborhoods of entrenched destitution;(Boston, 2005) despite their many hazards, these neighborhoods may have attracted services for deeply impoverished families. Because of intersectoral collaboration, local health departments had located public clinics within or near at least three AHA complexes. HOPE VI relocations tended to take residents to less impoverished neighborhoods that might have had fewer assets for poor families, though they conferred other benefits.(Popkin et al., 2004) These neighborhoods may have had good access to primary care, but not to safety-net primary care clinics. Notably, spatial access to safety-net primary care decreased even among people who relocated to rental units near their public housing complex because several safety-net clinics in and near the complexes closed after the demolitions.Osypuk and Acevedo-Garcia (2010) have written about opportunities and limitations that mobility programs hold for population health; to their discussion of limitations we would add that the neighborhoods to which relocaters move may lack key services for low-income residents.
Diminished spatial access to safety-net primary care for these relocaters is concerning, given their generally poor health and the well-established link between proximity to healthcare and utilization. Prior research with this cohort confirms the importance of spatial access to care for this population: we found a positive relationship at baseline between travel time to care and current infection with a sexually-transmitted infection. (Bonney et al., 2012)
Results from mixed models indicate that declines in spatial access to care were uniform across participants, regardless of baseline substance misuse or other health status. Perhaps finding a home that was near safety-net primary care was not among relocaters’ priorities even when they were in poor health, or perhaps they were unable to find such housing among available voucher-subsidized units.
Our findings should be interpreted in light of their limitations. As is common in studies with substance misusers, our sample was not randomly drawn from the underlying population in each complex and thus the extent to which our findings are generalizable is unknown. Notably, however, comparisons of our sample with a HUD survey of these complexes suggest that our sample’s income and household size were similar to those of the underlying resident population. (Department of Housing and Urban Development, 2000) The sample’s income, marital status, and age structure were also similar to those of a 782-member cohort created by the Urban Institute study of HOPE VI in five cities (Popkin et al., 2002). Additionally, our measure of spatial access for participants who used public transportation did not incorporate bus or train schedules or routes. Our findings were, however, robust across several measures of spatial access.
Our analyses suggest directions for future research and practice. Despite their scope and frequency in the USA, few studies have explored whether and how mass intra-urban migrations alter migrants’ spatial access to care. Future research analyzing data from probability-based samples whenever possible should document these changes, and identify successful strategies to help ensure continuity of care post-relocation. If future studies confirm our findings, relocation initiatives for public housing residents should help relocaters, particularly those in poor health, find housing that is near safety-net primary care.
Highlights.
HOPE VI disperses public housing residents to privately-owned subsidized rental units.
We studied HOPE VI’s impact on relocaters’ spatial access to safety net primary care.
Spatial access to safety net primary care declined substantially post-relocation.
Declines in access to care did not vary by baseline health status.
Acknowledgements
This study was funded by three grants: a CFAR03 grant awarded by the Emory Center for AIDS Research (P30 AI050409); a NIDA grant entitled “Public Housing Relocations: Impact on Healthcare Access, Drug Use & Sexual Health” (R21DA027072); and a NIDA grant entitled “Public Housing Relocations: Impact on HIV and Drug Use” (R01DA029513). We would like to thank our NIDA Project Officer, Dr. Bethany Deeds, for her excellent help with this project; AHA for permitting us to recruit participants on site; study participants for sharing their time and experiences with the study; and Ms. Juliana Clough and Ms. Melanie Wolfgang for helping to create the inventories of spatial access to safety net primary care.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hannah LF Cooper, Email: hcoope3@emory.edu.
Stephanie Wodarski, Email: stephanie.wodarski@gmail.com.
Janet Cummings, Email: jrcummi@emory.edu.
Josalin Hunter-Jones, Email: jjhunte@emory.edu.
Conny Karnes, Email: conny.chen@emory.edu.
Zev Ross, Email: zev@zevross.com.
Ben Druss, Email: bdruss@emory.edu.
Loida E Bonney, Email: lbonney@emory.edu.
References
- Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The Effects of Geography and Spatial Behavior on Health Care Utilization among the Residents of a Rural Region. Health Services Research. 2005;40:135–156. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonney LE, Cooper HL, Caliendo AM, del Rio C, Hunter-Jones J, Swan DE, Rothenberg R, Druss B. Access to Health Services and Sexually Transmitted Infections in a Cohort of Relocating African American Public Housing Residents: An Association Between Travel Time and Infection. Sexually Transmitted Diseases. 2012;39:116–121. doi: 10.1097/OLQ.0b013e318235b673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boston TD. Environment Matters: The effect of mixed-income revitalization on the socioeconomic status of public housing residents: a case study of Atlanta. Atlanta, GA: Georgia Institute of Technology; 2005. p. 96. [Google Scholar]
- Committee on the Changing Market. America's Health Care Safety Net: Intact but Endangered. Washington D.C.: Institute of Medicine; 2000. M.C., and the Future Viability of Safety Net Providers. [Google Scholar]
- Committee on the Future of Primary Care. Primary Care: America's Health in a New Era. Washington, D.C.: Institute of Medicine; 1996. [Google Scholar]
- Continelli T, McGinnis S, Holmes T. The effect of local primary care physician supply on the utilization of preventive health services in the United States. Health & Place. 2010;16:942–951. doi: 10.1016/j.healthplace.2010.05.010. [DOI] [PubMed] [Google Scholar]
- Department of Housing and Urban Development. A Picture of Subsidized Households -- Data Query Tool. Washington, D.C.: HUD; 2000. [Google Scholar]
- Department of Housing and Urban Development. About HOPE VI: Overview. Washington, D.C.: Department of Housing and Urban Development; 2008. [Google Scholar]
- Diez Roux AV. Neighborhoods and health: where are we and were do we go from here? Revue d Epidemiologie et de Sante Publique. 2007;55:13–21. doi: 10.1016/j.respe.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauth RC, Leventhal T, Brooks-Gunn J. Short-term effects of moving from public housing in poor to middle-class neighborhoods on low-income, minority adults' outcomes. Social Science and Medicine. 2004;59:2271–2284. doi: 10.1016/j.socscimed.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Goetz EG. Clearing the way: deconcentrating the poor in urban America. Washington, D.C.: The Urban Institute; 2003. [Google Scholar]
- Iacono M, Krizek K, El-Geneidy A. Estimating Accurate Distance Decay Functions for Multiple Modes and Different Purposes. Minnesota: Minnesota Department of Transportation, St. Paul; 2008. Access to Destinations: How Close is Close Enough? [Google Scholar]
- Massey D, Denton N. American Apartheid: Segregation and the Making of the Underclass. Cambridge, Massachusetts: Harvard University Press; 1993. [Google Scholar]
- Nemet GF, Bailey AJ. Distance and health care utilization among the rural elderly. Social Science & Medicine. 2000;50:1197–1208. doi: 10.1016/s0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health & Place. 2010;16:1113–1123. doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin S, Katz B, Cunningham M, Brown K, Gustafson J, Turner M. A Decade of HOPE VI: Research Findings and Policy Challenges. Wahsington, D.C.: The Urban Institute; 2004. p. 62. [Google Scholar]
- Popkin S, Levy D, Harris LE, Comey J, Cunningham M, Buron L, Woodley W. HOPE VI Panel Study: Baseline Report. Washington, D.C.: Urban Institute; 2002. [Google Scholar]
- Rae DW. City: Urbanism and Its End. New Haven: Yale University Press; 2003. [Google Scholar]
- Schuurman N, Berube M, Crooks VA. Measuring potential spatial access to primary health care physicians using a modified gravity model. The Canadian Geographer. 2010;54:29–45. [Google Scholar]
- Simning A, van Wijngaarden E, Yeates C. The association of African Americans’ perceptions of neighborhood crime and drugs with mental illness. Social Psychiatry and Psychiatric Epidemiologyq. 2011 doi: 10.1007/s00127-011-0426-0. Published online August 24 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TCU Institute of Behavioral Research. TCU Drug Screen IITCU. Texas: Fort Worth; 2006. [Google Scholar]
- Wallace R. Urban desertification, public health and public order:"Planned shrinkage", violent death, substance abuse, and AIDS in the Bronx. Social Science & Medicine. 1990;31:801–813. doi: 10.1016/0277-9536(90)90175-r. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Keller S. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–223. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. Jama. 2001;286:1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]