Abstract
Purpose
To determine the effect of body mass index (BMI) on level of agreement between six previously established prediction equations for three commonly used accelerometers to predict summary measures of energy expenditure (EE) in youth.
Methods
One hundred thirty-one youth between the ages of 10–17 years and BMI from 15 to 44 kg/m2 were outfitted with hip-worn ActiGraph GT1M, Actical, and RT3 accelerometers and spent approximately 24 hours in a whole-room indirect calorimeter while performing structured and self-selected activities. Five commonly used regression and one propriety equations for each device were used to predict the minute-to-minute EE (normalized to metabolic equivalents, METs), daily physical activity level (PAL), and time spent in sedentary, light, moderate, and vigorous physical activity intensity categories. The calculated values were compared with criterion measurements obtained from the room calorimeter.
Results
All predictive equations, except RT3, significantly over- or under-predicted daily PAL (p < 0.001), with large discrepancies observed in the estimate of sedentary and light activity. Discrepancies between actual and estimated PAL ranged from 0.05 to 0.68. In addition, BMI represented a modifier for two ActiGraph predictive equations (AG1 and AG2), affecting the accuracy of physical activity-related EE (PAEE) predictions.
Conclusion
ActiGraph (AG3) and the RT3 closely predicted overall PAL (within 4.2 and 6.8%, respectively) as a group. When adjusting for age, sex, and ethnicity, Actical (AC1 and AC2) and ActiGraph (AG3) were not influenced by BMI. However, a gap between some hip-worn accelerometer predictive and regression equations was demonstrated compared to both criterion measurement and each other, which poses a potential difficulty for inter-study (e.g. different accelerometers) and intra-study (e.g., BMI, adiposity) comparisons.
Keywords: Energy prediction, Adiposity, Actical, ActiGraph, RT3
INTRODUCTION
An estimated 17% of children and adolescents in the United States are currently obese (7) and a sedentary lifestyle with diminished physical activity (PA) is considered one of the major contributors to this epidemic(22). Several health organizations and government agencies currently recommend 60 minutes of moderate-to-vigorous exercise daily for children and adolescents, but even by self-reports, the majority of youth do not achieve these criteria (5, 11). Thus, accurate measurement of PA and PA-related energy expenditure (PAEE) is imperative to assess the association of PA and health in both clinical and epidemiological studies.
In recent years, accelerometers have emerged as the monitors of choice for measuring free-living PAEE because of their objectivity, reliability, minimal participant burden, versatility, and relative cost efficiency (20, 29, 41). Accelerometry is particularly appealing to measure PA in youth due to the inherent limitations of collecting self-report data within this population (2, 13). However, the accurate characterization of the relationship between accelerometer data output and EE has been challenging (9, 23). Predictive equations for youth have been developed for specific accelerometer devices based on a variety of activities at different levels of intensity (e.g., ambulatory activities and some forms of exercise) in relatively homogenous populations(34). However, results from studies with adults suggest varying accuracy of predictive equations in overweight and obese subjects (16). Validating the accuracy of these equations across a wide BMI range in predicting PAEE during both normal daily activities and structured bouts of PA is integral to determining their utility as a measurement tool (3).
Accelerometers can be used to measure the rate and intensity of body movements in up to three planes (12). Collected data, in the form of counts per time period termed epoch (set by the investigator), is the most commonly used method to represent dynamic PA levels. The data can also be incorporated into predictive equations to estimate gross EE or metabolic equivalents (METs) during studies performed in both, standardized laboratory-based and free -living conditions. Recent studies in adults and children have found that some equations systematically under- or over-predicted EE at different levels of PA intensity (9, 26, 31). These errors are hypothesized to be a result of the different EE conditions under which the particular predictive equations were developed and validated (26), including variability in the actual activities monitored. This point was further highlighted in a recent study be Trost et al., in which intensity-related accelerometer cut points were assessed in children (39). They demonstrated a wide range of classification accuracy of the five independently developed cut points evaluated.
The objective of this study was to build upon these previous studies by examining the validity of PAEE estimates for a set of commercially available accelerometers (ActiGraph, Actical, and RT3) in a large heterogeneous health youth study population with the gold-standard reference of a whole-room indirect calorimeter. We compared the validity of commonly utilized monitor-specific equations in predicting PAEE and PA intensity distribution across a wide BMI range based on both structured bouts of PA and self-selected activities. In addition, we examined the effect of BMI, sex, and ethnicity on these predictions.
METHODS
Participants
One hundred and thirty-one youths, between 10–17 years of age (62 males and 69 females) participated in the study, with about half of each group self-describing themselves as African American. All volunteers were healthy as determined by a physical exam by a board-certified pediatrician, did not take any medications known to alter EE, did not have any limitations or difficulties performing exercise, and were non-smokers. Participants were recruited using flyers, e-mail distribution lists, and personal contacts. All participants and their parent or legal guardian signed an informed consent document (participants under the age of 13 sign an informed assent document) approved by the university-affiliated Institutional Review Board. The characteristics of these participants are shown in Table 1.
Table 1.
Characteristics of study participants.
| All participants (n = 131) | Female (n= 69) | Male (n= 62) | |
|---|---|---|---|
| Age (years) | 13.4 ± 2.2 (10 to 17) | 13.3 ± 2.1 (10 to 17) | 13.3 ± 2.4 (10 to 17) |
| Height (m) | 1.60 ± 0.11 (1.06 to 1.95) | 1.58 ± 0.09 (1.06 to 1.77) | 1.62 ± 0.13 (1.37 to 1.95) |
| Weight (kg) | 64.3 ± 19.9 (32.5 to 129.5) | 63.9 ± 18.3 (32.9 to 111.5) | 64.6 ± 21.8 (32.5 to 129.5) |
| BMI(kg/m2) | 24.7 ± 6.1 (15.1 to 44.0) | 25.2 ± 6.3 (15.1 to 40.6) | 24.1 ± 5.9 (15.2 to 44.0) |
| BMI percentile* | 75.5 ± 26.4 (4.0 to 99.0) | 76.5 ± 26.9 (4.0 to 99.0) | 74.3 ± 26.1 (12.0 to 99.0) |
| % Body Fat | 30.8 ± 11.6 (7.5 to 54.6) | 34.4 ± 9.8 (11.2 to 54.6) | 26.7 ± 12.1 (7.5 to 53.2) |
| Ethnicity | |||
| African American | 64 | 37 | 27 |
| White | 64 | 30 | 34 |
| Hispanic | 3 | 2 | 1 |
Values are presented as mean ± standard deviation and (range).
BMI percentile - calculated from CDC BMI-for-age growth charts.
Abbreviations: BMI, body mass index.
During a screening visit conducted by research personnel, details of the study were discussed, and all questions answered. Participants were asked to maintain normal daily routines, but avoid any unusual PA and stress (such as strenuous exercise), on the day before the study was conducted at the Vanderbilt Clinical Research Center. No dietary restrictions were stipulated prior to the study visit.
Anthropometric Measures
Body mass was measured by the research staff to the nearest 0.1 kg with a digital scale (Detecto-Medic, Detecto Scales, Inc, Northbrook, IL) with the participants wearing light clothing and no shoes. Stature was measured using a wall-mounted stadiometer (Perspective Enterprises, Portage, MI) and body composition using dual-energy X-ray absorptiometry (GE Lunar Prodigy, Madison, WI; software enCORE 2007, version 11.40.004). Body mass index (BMI) was calculated as a ratio of weight (kg) to the square of the stature (meters squared). For the purpose of statistical analysis, participants were also categorized to a normal (BMI <85th percentile for sex and age), overweight (BMI ≥85th percentile to <95th percentile for sex and age) or obese (BMI ≥95th percentile for sex and age) BMI category(6).
Study Design and Protocol
All participants completed one overnight stay (~24 hours) in a whole-room indirect calorimeter. The room calorimeter is an airtight room with windows and an airtight pass, and is equipped with a toilet, sink, desk, chair, telephone, multimedia, and exercise equipment. A computerized system with a touch monitor and an audible signal prompts participants to start and finish each standardized physical activity. An intercom system allows research staff to communicate with the person inside the room. The room assures high-precision measurements in a controlled environment and semi-naturalistic conditions (i.e. not wearing a breathing mask), and allows for adjusting the intensity of any PA task to the individual’s capability. Technical details of the indirect calorimeter measurement approach have been reported elsewhere (36). During the stay, participants followed a protocol that included two structured activity sessions, which occurred at set times during the study period (non-randomized). The duration and intensity of activity sessions was predetermined to simulate an average, free-living physical activity profile. The morning session included self-paced ambulatory activities such as walking or jogging. The afternoon session involved sedentary activities such as deskwork. Each structured activity was performed for ten minutes and was followed by a ten-minute rest to allow the EE measurement to reach proximal steady state before the next activity. Previous accelerometer validation studies have similarly utilized structured activity periods lasting less than 10 minutes, based on the short but sustained physical activity episodes that characterize the free-living patterns of children(27, 32). Meals were scheduled at specific times (breakfast, lunch, supper, afternoon snack, evening snack), with participants able to choose from two meal plans (each structured to provide similar caloric, macronutrient, and micronutrient content). Participants were asked to go to bed no later than 10:00 pm. During times when no specific activity was scheduled (~5 h), participants were encouraged to engage in their normal daily PA patterns. During the non-sleeping time, each participant wore the three accelerometers devices mounted on their hip (anterior torso) on the dominant side. The waking period was defined as time from entering the room until going to bed in the evening and confirmed by the room calorimeter.
Energy Expenditure Measures
Measurements of energy expenditure (EE) during rest and performing PA tasks (PAEE) were calculated from measured rates of oxygen (O2) consumption and carbondioxide (CO2) production using Weir’s equation (44). The accuracy and precision of our metabolic chamber for measuring EE as determined by routine alcohol combustion tests was 99.2 ± 0.5% (mean ± SD) over 24 hours and 98.6 ± 2.1% over 30 minutes.
Sleeping EE (SEE, kcal/min)
SEE was calculated as the average EE during sleep between 1:00 am and 4:00 am. Any periods with significant movement recorded by the room calorimeter were removed from the SEE calculations.
Physical Activity-related EE (PAEE)
PAEE during performance of each PA task was calculated as a ratio of EE to SEE (kcal/min), and expressed as metabolic equivalents (METs) (30).
Physical Activity Level (PAL) Categories
For standardized interpretation, cutoff points according to MET values have been established to distinguish between levels of intensity that correspond with levels of activity used in making public health predictions. These categories (termed physical activity levels) include sedentary (1–1.5 METs), light (1.5 – 3 MET), moderate (3–6 METs) and intense/vigorous (>6 METs) (8).0
Accelerometers
Commercially available accelerometers, frequently utilized in studies with adults and youth, including the ActiGraph GT1M (Pensacola, FL), the Actical (MiniMiter/Respironics, Bend, OR), and the RT3 (StayHealthy, Monrovia, CA) were used. Both the ActiGraph and Actical are primarily sensitive to motion in one plane (vertical). The RT3 is a tri-axial accelerometer, which reports activity in three orthogonal directions and the vector magnitude of the three measurements. Technical specifications for each type of monitor have been previously reported (1, 14, 32, 42). The ActiGraph GT1M, which was used without a signal filter, is no longer commercially available; however, it remains utilized in research and has been demonstrated to have similar vertical axis output in comparison to its successors, the ActiGraph GT3X and GT3X+ (33). The monitors report activity counts, a device-specific output that represents the average intensity of acceleration events occurring over a user-defined measurement epoch. For this study, all monitors were attached to a belt secured at the waist with monitors positioned on the hip (dominant side), and data from each monitor were acquired in 1-min epochs to facilitate 24-hour data recording. After data were downloaded, each dataset was time-synchronized with the minute-to-minute data from the room calorimeter.
Prediction equations
Activity count data for each monitor were collected using 1-minute epochs and converted to measures of PA intensity (EE, PAEE or METs) using both published (ActiGraph, Actical) and proprietary (RT3) equations (14, 28, 29, 34, 40). All models were then treated equally to result in individually-normalized PAEE in METs on a minute-by-minute basis. Three regression equations were tested for the ActiGraph and two equations for the Actical in youth, and one equation for the RT3 (Table 2). The regression equation for the RT3 monitor is proprietary, and consequently the exact structure is not reported. Acquired data were analyzed using both MET-based categorical predictions and daily PAL, which was computed as the average of the minute-by-minute MET predictions during the study interval.
Table 2.
Selected regression equations for AG, AC and RT3 accelerometers
| Equation Number | Developer | Activity Monitor | Age Range (years) | Regression Equation |
|---|---|---|---|---|
| AC1 | Puyau et al.(29) | Actical | 7 – 18 | AEE (kcal/kg/min) = 0.00423 + 0.00031 × (ct/min) 0.653 |
| AC2 | Heil(14) | Actical | 8 – 17 | AEE (kcal/kg/min) = 0.01667 + 0.00005103 × (ct/min) if ct/min < 1650 AEE (kcal/kg/min) = 0.03534 + 0.00001135 × (ct/min) if ct/min ≥ 1650 |
| AG1 | Puyau et al. (28) | Actigraph | 6 – 16 | EE (kcal/kg/min) = 0.0654 − 0.00197 × age(years) + 0.000010 × (ct/min) |
| AG2 | Schmitz et al.(34) | Actigraph | 13 – 14 | EE (kJ/min) = 7.6628 + 0.1462 × [((ct/min)−3000)/100] + 0.2371 × weight(kg) − 0.00216 × [((ct/min)− 3000)/100]2 + 0.004007 × [((ct/min)− 3000)/100] × weight(kg) |
| AG3 | Trost et al.(40) | Actigraph | 10 – 13 | EE (kcal/min) = −2.23 + 0.0008 × (ct/min) + 0.08 × weight(kg) |
| RT3 | StayHealthy | RT3 | Proprietary |
Abbreviations: AC, Actical; AEE, activity energy expenditure; EE, energy expenditures; AG, ActiGraph; METs, metabolic equivalents; ct, activity counts.
PAL represents the ratio of mean EE and SEE, and is an important outcome measure because it reflects the cumulative duration and intensity of PA episodes in each day(19). In the present study, the average PAL during waking was by design similar to averages found in previous population studies (21, 25) to mimic a free-living PA pattern, in which 90% of the day is engaged in “sedentary” and “light” activity (40% and 50%, respectively), 8% in “moderate” activity and only 2% in “vigorous” activity. Given the objective of categorizing daily PAL and time spent in PA categories, data from time sleeping in the whole-room indirect calorimeter were excluded from analysis. However, a 24-hour study was important to collect stable SEE in individuals.
As in previous reports (31), the equation-predicted EE were expressed in METs, which was the PAEE normalized to individual measured REE (35). This approach is consider more accurate than using a constant factor of 3.5 mL oxygen per of body mass per minute (4) proposed by Jette et al. (17).
Statistical analysis
Descriptive statistics were calculated as the mean with standard deviation and the total range or median with interquartile range (IQR) for continuous variables. For categorical variables, percentage (N) was presented. Predicted PAL and the time spent in the four PA intensity ranges (specified in METs) calculated from all the equations were compared to measured values by the room calorimeter. All analyses included wear time for all waking hours. As the standard criteria, the calorimetry MET values were calculated on a minute-by-minute basis as the ratio of measured EE to SEE. The Kruskal-Wallis test was used to compare PAL data among normal, overweight, and obese. The Wilcoxon signed rank test was used to compare the predicted PAL with the actual PAL for each device and each equation. The predicted and actual time spent in each intensity category was compared using Wilcoxon signed rank test. The PAL difference for sex, ethnicity, and obesity status were compared using the Mann-Whitney U test. To account for multiple testing, a type I error rate of p<0.001 was used for statistical significance. We analyzed the association of BMI with PAL difference (equation minus calorimeter) for each device/equation using ordinary least squares (OLS), adjusting for age, ethnicity, and sex. We used restricted cubic splines to model the nonlinear effect of BMI and age. Interaction between age and BMI, sex and BMI were also included to account for the BMI effect differences at different ages and between male and female. Residual plot and q-q (quantile-quantile) plot were used to check the model assumptions. All statistical analyses were performed using open source R statistical software (version 2.13.0, Vienna, Austria).
RESULTS
Physical Activity Levels (PAL)
Difference in PAL predicted with each regression equation and the measurement using the calorimeter is represented in Figure 1. The median PAL measured by room calorimeter during waking was 1.92 (IQR 1.80 to 2.01), with a mean testing duration of 13.3 hours (SD = 0.3 hours). All equation estimates significantly differed from the room calorimeter measures at P < 0.001, except RT3 (p = 0.008). PAL was under-predicted by the AC1, AC2, and AG3 equations, and over-predicted by the AG1 and AG2 equations. Discrepancies between actual and estimated PAL ranged from 0.05 to 0.68. The AG1 and AG2 equations over-predicted PAL by 0.58 (95% CI: 0.49–0.68) and 0.32 (95% CI: 0.25–0.39) respectively; whereas the AC2 equation under-predicted PAL by 0.46 (95% CI: 0.42–0.50). The AG3 and RT3 equations were the closest approximations to the calorimeter measurement, under-predicting PAL by 0.10 (95% CI: 0.05–0.19) and 0.14 (95% CI: 0.08–0.20) respectively. The above variations in PAL results were similar between ethnicity (white vs. black) and sex (female vs. male). However, the median differences in estimating PAL by models were consistently higher in the overweight and obese compared to normal BMI youth (Table 3, Supplemental Figure 1).
Figure 1.
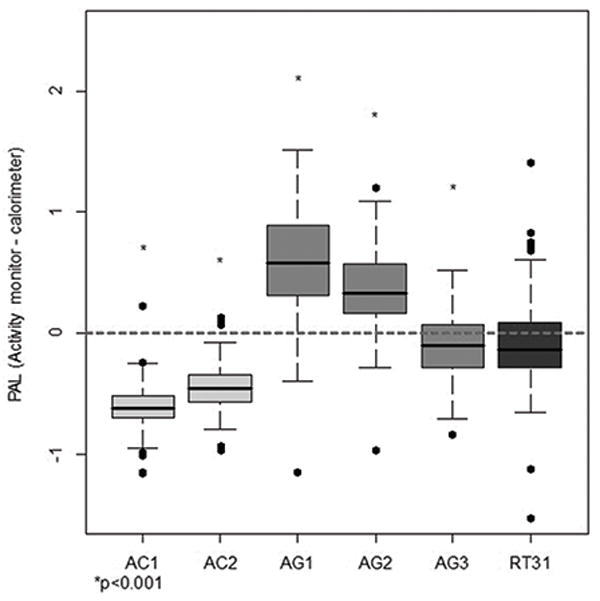
Difference in physical activity level (PAL) predicted with each regression equation and the measurement using the calorimeter. Underpredictions fall below the x-axis (0), while overpredictions are above. The mean PAL measured by the room calorimeter is 1.92. AC -Actical; AG - ActiGraph, RT3 - RT3 accelerometer.
* Significant at P<0.001.
Table 3.
Summary comparison of PAL by obesity status.
| Normal (N=62) | Overweight (N=24) | Obese (N=45) | P-value | |
|---|---|---|---|---|
| IC | 1.91 (1.77 to 1.99) | 1.96 (1.87 to 2.01) | 1.91 (1.80 to 2.02) | 0.230 |
| AC1 | 1.26 (1.21 to 1.34) | 1.35 (1.26 to 1.39) | 1.33 (1.24 to 1.41) | 0.018 |
| AC2 | 1.40 (1.31 to 1.49) | 1.53 (1.41 to 1.61) | 1.47 (1.39 to 1.65) | 0.004 |
| AG1 | 2.23 (2.00 to 2.40) | 2.66 (2.46 to 2.70) | 2.96 (2.67 to 3.13) | <0.001 * |
| AG2 | 2.12 (1.92 to 2.31) | 2.33 (2.17 to 2.3) | 2.51 (2.25 to 2.71) | <0.001 * |
| AG3 | 1.82 (1.53 to 2.02) | 1.94 (1.76 to 2.01) | 1.90 (1.58 to 2.08) | 0.220 |
| RT3 | 1.76 (1.56 to 1.96) | 1.74 (1.70 to 1.96) | 1.90 (1.70 to 2.23) | 0.071 |
Values are presented as median and (interquartile range). P-values represent direct comparison of PAL values.
Abbreviations: IC, indirect calorimetry, AC, Actical; AG, Actigraph.
Significant at P<0.001.
For further investigation of the PAL variations seen between obese, overweight and normal BMI youth, the analysis of PAL difference between calorimeter and individual predictive equation was also investigated using BMI as a continuous variable, while adjusting for age, sex, and ethnicity. Higher BMI was associated with increased PAL difference for AG1 (P<0.001) and AG2 (P<0.001), and neared a significant associated for RT3 (P=0.002) (Figure 2, Supplemental Table 1). A similar pattern was demonstrated when percent body fat was investigated as a continuous variable instead of BMI, except for RT3 (P=0.027) (Supplemental Table 1). However, since the results of these two variables were similar and BMI is much easier to obtain in population studies, it was chosen as the continuous variable for reporting of results.
Figure 2.
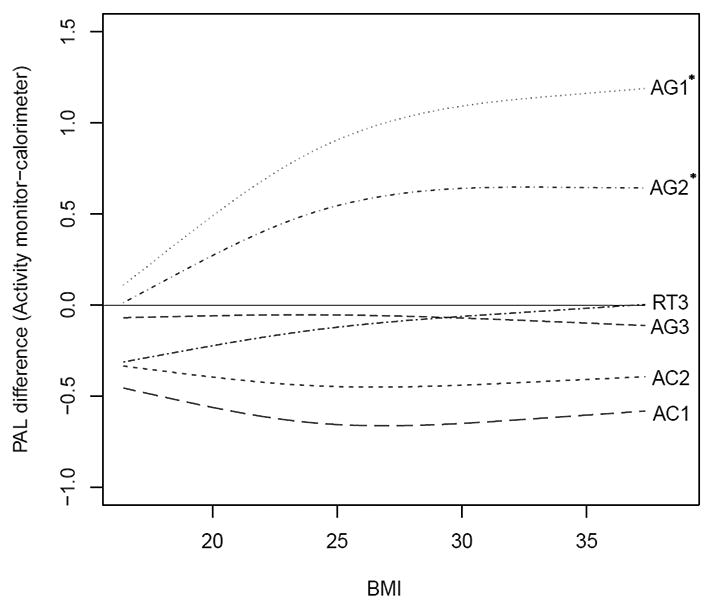
Nonparametric regression (loess) estimates calculated for the relationship between BMI and differences in PAL predicted with each equation and the measurement using the calorimeter, adjusted for age, sex, and ethnicity. Solid line (0.0) represents reference PAL measured by room calorimeter. Underpredictions fall below the reference line (AC1, AC2, AG3, and RT3), while overpredictions are above (AG1 and AG2). AC, Actical; AG, ActiGraph; PAL, physical activity level; BMI, body mass index (kg/m2).
* Significant at P<0.001.
Time spent in PA intensity categories
During the awake periods in the calorimeter, participants spent approximately 40% of their time in sedentary activities (1 – 1.5 METs), 50% in light (1.5 –3 METs), 8% in moderate (3–6 METs), and 2% in vigorous (>6 METs) PAL categories. There were significant differences between the calorimeter measurements and most accelerometer predictions for the sedentary and light categories (p < 0.001). AC1 and AC2 over-predicted and AG1 and AG2 under-predicted the time spent in sedentary behaviors by 35% or more. Only 2 equations fell within 35% of the calorimeter measure of time spent in sedentary behavior, AG3 (7% under-estimated) and RT3 (18% over-estimated). Similar differences were observed for light activities, with the AG3 equation over-predicted the calorimeter measure by 12% and the RT3 under-predicted it by 20%. The remaining five equations under- or over-predicted the calorimeter reading for time spent in the light PAL category by 34% or more. Most equation predictions differed from the calorimeter estimate of time spent in moderate and vigorous PA categories, ranging from 1% over-estimation to 5% under-estimation for moderate PA and from −1% to 1% for vigorous PA (Figure 3).
Figure 3.
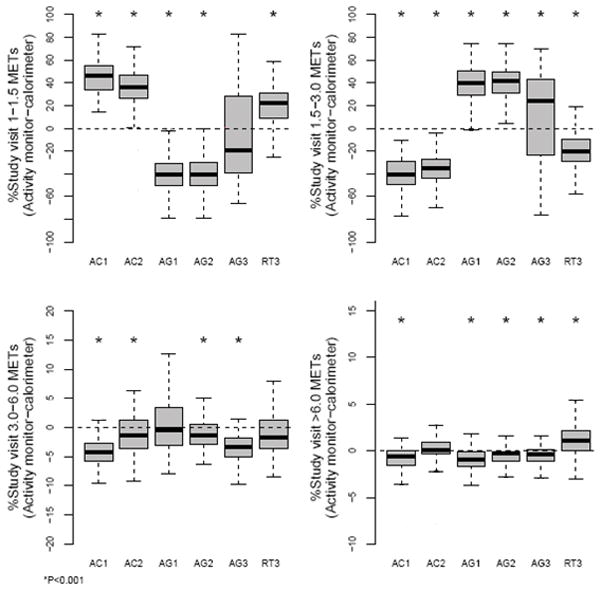
Percent of study spent in four intensity categories represented for each equation as the difference from the room calorimeter. Underpredictions fall below the x-axis (0), while overpredictions are above. AC, Actical; AG, ActiGraph; METs, metabolic equivalents.
* Significant at P<0.001.
DISCUSSION
Our study was designed to quantify the accuracy of one day of PAEE predicted from three commonly used accelerometers in a large group of heterogeneous youth using the gold-standard reference of a room calorimeter. Using simple regression algorithms, we found the ActiGraph (AG3) and the RT3 closely predicted overall PAL (within 4.2 and 6.8%, respectively) as a group. When adjusting for age, sex, and ethnicity, Actical (AC1 and AC2) and ActiGraph (AG3) were not influenced by BMI. However, we also demonstrated a gap between some hip-worn accelerometer predictive and regression equations compared to both criterion measurement and each other, which poses a potential difficulty for inter-study (e.g. accelerometers) and intra-study (e.g., adiposity) comparisons.
The predictive equations utilized in this present study included commonly used regressions validated in children and adolescents (15, 43), with variable inclusion or exclusion of several components (weight, age, stature). However, the development of these equations was largely achieved with small cohorts comprised of limited numbers of obese youth. For the five predictive equations with published methods and results (the StayHealthy RT3 proprietary equation being excluded), only one study had a cohort size greater than 35 (the AG2 equation was derived from a study involving 74 adolescent females)(14, 28, 29, 34, 40). In addition, at least one equation (AG1) was derived from a cohort that did not include any obese youth(28). The variability in cohort composition (ethnicity, age, and sex) and testing methods (different activities and exercise intensities) between studies likely also present variables that would contribute to the variances observed among predictive equations. Our present study is strengthened by a relatively large sample size of 131 youth with a heterogeneous composition according to age, ethnicity, sex, and BMI. In addition, approximately 13 hours of continuous waking energy expenditure data per subject measured by reference standard room calorimeter(37) were collected on each individual for comparison to accelerometer predicted EE.
Summary statistics for time spent in PA intensity categories is a commonly used measure for assessing whether an individual has met daily PA recommendations (18). Among equations, AG1 and RT3 were the most accurate in estimating moderate activity, while AC2, AG2, and RT3 were the most accurate in estimating vigorous activity (within 2% of the calorimeter data). However, all equations were substantially less accurate in predicting sedentary and light activity. The AG3 equation, which under-estimated sedentary activity by 7% and over-estimated light activity by 12%, was most accurate in estimating mean proportion of time spent in activity intensities. However, this equation also produced the largest degree of individual variability, suggesting low individual accuracy. This can be explained, at least in part, by the lack of a body mass component in the equation. The AG2 equation, with a similar structure, provides lower individual variability. The RT3 equation over-predicted EE of sedentary activity by 18% and under-predicted light activity by 20%. The AG1 equation significantly over-estimated the percentage of time spent in the moderate activity category. Several participants had more than 20% of time categorized as moderate activity, which was significantly higher than measured time. The AG2, AC1, and AC2 equations under- or over-estimated sedentary and light activity similarly (Figure 3).
There are limitations of this study that should be considered. First, due to our relatively large sample size (in regards to both the number of participants and duration of data collection), even small mean differences on an individual’s basis may be detected as statistically significant within the entire study population. This is particularly evident in the data for time spent in moderate and vigorous activities. Despite the small percentage of time spent in either of these activity categories, several differences were statistically significant. We have attempted to address absolute and relative differences between the predictions of each equation and the calorimeter measurements regardless of their statistical significance. However, the translation of these statistically significant findings to clinically significant applicability remains undefined. Even if absolute differences appear minimal, over-prediction of PAL or intensity classification might falsely predict that threshold values have been achieved. Second, our analysis of BMI as a continuous variable was limited by its skewed distribution, which is characteristic for obese children and adolescents. A large percentage of participants were at or near the 99th percentile of BMI adjusted for sex and age, which prompted our use of unadjusted BMI when analyzed as a continuous measure. For categorical measures of BMI (non-obese vs. obese), age- and sex-adjusted BMI percentiles were utilized. However, in both methods the results were similar, with BMI representing a statistically significant modifier for AG2 and AG2 equation PAL estimation. Researchers should use care to consider the clinical significance of the discrepancies reported here within the context of their own work. Lastly, a potential limitation and source of error is the use of >3 METs as the lower cut point for moderate physical activity. Traditionally, this has been the accepted cut point in children and adolescents based on several validation studies (10, 28, 38). However, recent studies have suggested that this lower cut point is not valid in children, and instead should be >4 METs (24, 38).
Results of this study suggest the accelerometers examined were generally limited in their ability to distinguish between sedentary and light activities, but performed reasonably well at detecting moderate and vigorous activities, which was an unexpected finding. Trost et al. recently examined five predictive equations for the ActiGraph monitor (one of which were also utilized in our study) and demonstrated the most consistent accuracy for sedentary behaviors (39). While inclusion of other predictive equations might provide different results, our findings for sedentary and light activities were present regardless of the particular device or predictive equation utilized. Potential etiologies for these findings of sedentary and light activities are the duration of observation and variations in times spent in either sedentary or light activities. According to the indirect calorimetry data, percent sedentary activity time was 41% (IQR 31 % to 51%) and percent light activity time was 50% (IQR 42% to 59%). This wide variation was also demonstrated in the accelerometer data, which resulted in much broader ranges than in data for percent time spent in either moderate or vigorous activities. A practical significance of these findings is that the current standard approach (hip-worn, one-minute epoch, and simple regression) should be used cautiously in clinical trials and intervention studies targeted on sedentary behaviors (e.g. screen time in youth) but might be adequate for measuring compliance with moderate to vigorous PA recommendations. However, researchers should exercise caution when using these equations to characterize an individual’s general PA profile. Based on our results, we suggest that to increase accuracy of PAEE and PA patterns prediction from currently available accelerometers in youth across a wide range of BMI, it is necessary to develop new approaches, equations, or correction factors.
In conclusion, we found that ActiGraph (AG3) and RT3 closely predicted overall PAL (within 4.2 and 6.8%, respectively) as a group. When adjusting for age, sex, and ethnicity, Actical (AC1 and AC2) and ActiGraph (AG3) were not influenced by BMI. The presented data suggest that there is a gap between some hip-worn accelerometer predictive and regression equations compared to both criterion measurement and each other. These differences pose a potential difficulty in both inter-study (e.g. accelerometers) and intra-study (e.g. BMI, adiposity) comparisons.
Supplementary Material
Difference in PAL predicted with each regression equation and the room calorimeter measurement stratified by obesity status (obese, BMI ≥95th percentile; non-obese, BMI <95th percentile). Underpredictions fall below the x-axis (0), while overpredictions are above. AC, Actical; AG, ActiGraph; PAL, physical activity level.
* Significant at P<0.001.
Effect of (a) BMI and (b) percent body fat on the predictive accuracy of PAL selected accelerometer predictive equations.
Acknowledgments
This work was supported by grants from the National Institutes of Health (NIH) RO1HL082988, Vanderbilt CTSA grant UL1 RR024975, and Vanderbilt Diabetes Research and Training Center supported by NIH grant DK20593. We would like to thank Marissa Avolio, Stephane Daphnis, Cindy Dorminy, Kristen Jensevar, Natalie Meade and Elizabeth Provenzano, for their contributions to the acquisition of the data for this study. The results of the present study do not constitute endorsement by the ACSM.
Footnotes
Conflict of Interests: The authors report no conflict of interest.
References
- 1.ActiGraph. Actisoft Analysis Software 3.2 User’s Manual. For Walton Beach; FL: 2005. [Google Scholar]
- 2.Adamo KB, Prince SA, Tricco AC, Connor-Gorber S, Tremblay M. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: a systematic review. International Journal of Pediatric Obesity. 2009;4(1):2–27. doi: 10.1080/17477160802315010. [DOI] [PubMed] [Google Scholar]
- 3.Bassett DR, Jr, Rowlands A, Trost SG. Calibration and validation of wearable monitors. Medicine and Science in Sports and Exercise. 2012;44(1 Suppl 1):S32–8. doi: 10.1249/MSS.0b013e3182399cf7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. Journal of Applied Physiology. 2005;99(3):1112–9. doi: 10.1152/japplphysiol.00023.2004. [DOI] [PubMed] [Google Scholar]
- 5.CDC. Centers for Disease Control and Prevention: How much physical activity to children need? 2011 [updated March 30, 2011; cited 2011 August 1]. Available from: http://www.cdc.gov/physicalactivity/everyone/guidelines/children.html.
- 6.CDC. Centers for Disease Control and Prevention. Basics about childhood obesity. 2011 [cited 2011 August 9, 2011]. Available from: http;// www.cdc.gov/obesity/childhood/basics.html.
- 7.Centers for Disease Control and Prevention. Childhood Overweight and Obesity. 2010 [March 27, 2010]. Available from: http://www.cdc.gov/obesity/childhood/index.html.
- 8.Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS. Development and validation of a Pregnancy Physical Activity Questionnaire. Medicine and Science in Sports and Exercise. 2004;36(10):1750–60. doi: 10.1249/01.mss.0000142303.49306.0d. [DOI] [PubMed] [Google Scholar]
- 9.Crouter SE, Churilla JR, Bassett DR., Jr Estimating energy expenditure using accelerometers. European Journal of Applied Physiology. 2006;98(6):601–12. doi: 10.1007/s00421-006-0307-5. [DOI] [PubMed] [Google Scholar]
- 10.Freedson P, Pober D, Janz KF. Calibration of accelerometer output for children. Medicine and Science in Sports and Exercise. 2005;37(11 Suppl):S523–30. doi: 10.1249/01.mss.0000185658.28284.ba. [DOI] [PubMed] [Google Scholar]
- 11.Fulton JE. Physical activity levels of high school students --- United States, 2010. MMWR - Morbidity and Mortality Weekly Report. 2011;60(23):773–7. [PubMed] [Google Scholar]
- 12.Godfrey A, Conway R, Meagher D, OLaighin G. Direct measurement of human movement by accelerometry. Medical Engineering & Physics. 2008;30:1364– 86. doi: 10.1016/j.medengphy.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 13.Goran MI. Measurement issues related to studies of childhood obesity: assessment of body composition, body fat distribution, physical activity, and food intake. Pediatrics. 1998;101(3 Pt 2):505–18. [PubMed] [Google Scholar]
- 14.Heil DP. Predicting activity energy expenditure using the Actical activity monitor. Research Quarterly for Exercise and Sport. 2006;77(1):64–80. doi: 10.1080/02701367.2006.10599333. [DOI] [PubMed] [Google Scholar]
- 15.Hussey J, Bennett K, Dwyer JO, Langford S, Bell C, Gormley J. Validation of the RT3 in the measurement of physical activity in children. Journal of Science and Medicine in Sport/Sports Medicine Australia. 2009;12(1):130–3. doi: 10.1016/j.jsams.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 16.Jacobi D, Perrin AE, Grosman N, Dore MF, Normand S, Oppert JM, et al. Physical activity-related energy expenditure with the RT3 and TriTrac accelerometers in overweight adults. Obesity (Silver Spring) 2007;15(4):950–6. doi: 10.1038/oby.2007.605. [DOI] [PubMed] [Google Scholar]
- 17.Jette M, Sidney K, Blumchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clinical Cardiology. 1990;13(8):555–65. doi: 10.1002/clc.4960130809. [DOI] [PubMed] [Google Scholar]
- 18.Kelly EB, Parra-Medina D, Pfeiffer KA, Dowda M, Conway TL, Webber LS, et al. Correlates of physical activity in black, Hispanic, and white middle school girls. J Phys Act Health. 2010;7(2):184–93. doi: 10.1123/jpah.7.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Livingstone MBE, Robson PJ, Wallace JMW, McKinley MC. How active are we? Levels of routine physical activity in children and adults. Proceedings of the Nutrition Society. 2003;62(3):681–701. doi: 10.1079/PNS2003291. [DOI] [PubMed] [Google Scholar]
- 20.Lyden K, Kozey SL, Staudenmeyer JW, Freedson PS. A comprehensive evaluation of commonly used accelerometer energy expenditure and MET prediction equations. European Journal of Applied Physiology. 2011;111(2):187–201. doi: 10.1007/s00421-010-1639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maffeis C, Zaffanello M, Pinelli L, Schutz Y. Total energy expenditure and patterns of activity in 8–10-year-old obese and nonobese children. J Pediatr Gastroenterol Nutr. 1996;23(3):256–61. doi: 10.1097/00005176-199610000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Martinez-Gonzalez MA, Martinez JA, Hu FB, Gibney MJ, Kearney J. Physical inactivity, sedentary lifestyle and obesity in the European Union. Int J Obes Relat Metab Disord. 1999;23(11):1192–201. doi: 10.1038/sj.ijo.0801049. [DOI] [PubMed] [Google Scholar]
- 23.Matthews CE. Calibration of Accelerometer Output for Adults. Medicine and Science in Sports and Exercise. 2005;37(11 Supplement):S512–S22. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 24.Mattocks C, Leary S, Ness A, Deere K, Saunders J, Tilling K, et al. Calibration of an accelerometer during free-living activities in children. Int J Pediatr Obes. 2007;2(4):218–26. doi: 10.1080/17477160701408809. [DOI] [PubMed] [Google Scholar]
- 25.McManus AM, Chu EY, Yu CC, Hu Y. How children move: activity pattern characteristics in lean and obese chinese children. J Obes. 2011;2011:679328. doi: 10.1155/2011/679328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nilsson A, Brage S, Riddoch C, Anderssen SA, Sardinha LB, Wedderkopp N, et al. Comparison of equations for predicting energy expenditure from accelerometer counts in children. Scandinavian Journal of Medicine & Science in Sports. 2008;18(5):643–50. doi: 10.1111/j.1600-0838.2007.00694.x. [DOI] [PubMed] [Google Scholar]
- 27.Pfeiffer KA, McIver KL, Dowda M, Almeida MJ, Pate RR. Validation and calibration of the Actical accelerometer in preschool children. Medicine and Science in Sports and Exercise. 2006;38(1):152–7. doi: 10.1249/01.mss.0000183219.44127.e7. [DOI] [PubMed] [Google Scholar]
- 28.Puyau M, Adolph A, Vohra F, Butte N. Validation and calibration of physical activity monitors in children. Obesity Research. 2002;10:150– 7. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 29.Puyau MR, Adolph AL, Vohra FA, Zakeri I, Butte NF. Prediction of activity energy expenditure using accelerometers in children. Medicine and Science in Sports and Exercise. 2004;36(9):1625–31. [PubMed] [Google Scholar]
- 30.Rothney M, Brychta R, Chen K, Buchowski M. Validation of the ActiGraph Two–Regression Model for Predicting Energy Expenditure. Medicine and Science in Sports and Exercise. 2010;42(9):1785–92. doi: 10.1249/MSS.0b013e3181d5a984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rothney MP, Schaefer EV, Neumann MM, Choi L, Chen KY. Validity of physical activity intensity predictions by ActiGraph, Actical, and RT3 accelerometers. Obesity. 2008;16(8):1946–52. doi: 10.1038/oby.2008.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rowlands A, Thomas P, Eston R, Topping R. Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Medicine and Science in Sports and Exercise. 2004;36:518– 24. doi: 10.1249/01.mss.0000117158.14542.e7. [DOI] [PubMed] [Google Scholar]
- 33.Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. Journal of Science and Medicine in Sport. 2011;14(5):411–6. doi: 10.1016/j.jsams.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 34.Schmitz KH, Treuth M, Hannan P, McMurray R, Ring KB, Catellier D, et al. Predicting energy expenditure from accelerometry counts in adolescent girls. Medicine and Science in Sports and Exercise. 2005;37(1):155–61. doi: 10.1249/01.MSS.0000150084.97823.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schutz Y, Weinsier RL, Hunter GR. Assessment of free-living physical activity in humans: an overview of currently available and proposed new measures. Obesity Research. 2001;9(6):368–79. doi: 10.1038/oby.2001.48. [DOI] [PubMed] [Google Scholar]
- 36.Sun M, Reed G, Hill J. Modification of a whole room indirect calorimeter for measurement of rapid changes in energy expenditure. Journal of Applied Physiology. 1994;98:601– 12. doi: 10.1152/jappl.1994.76.6.2686. [DOI] [PubMed] [Google Scholar]
- 37.Tokuyama K, Ogata H, Katayose Y, Satoh M. Algorithm for transient response of whole body indirect calorimeter: deconvolution with a regularization parameter. Journal of Applied Physiology. 2009;106(2):640–50. doi: 10.1152/japplphysiol.90718.2008. [DOI] [PubMed] [Google Scholar]
- 38.Treuth M, Schmitz K, Catellier D, McMurray R, Murray D, Almeida M, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Medicine and Science in Sports and Exercise. 2004;36:1259– 66. [PMC free article] [PubMed] [Google Scholar]
- 39.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Medicine and Science in Sports and Exercise. 2011;43(7):1360–8. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 40.Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the computer science and applications (CSA) activity monitor in children. Medicine and Science in Sports and Exercise. 1998;30(4):629–33. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- 41.Trost SG, Way R, Okely AD. Predictive validity of three ActiGraph energy expenditure equations for children. Medicine and Science in Sports and Exercise. 2006;38(2):380–7. doi: 10.1249/01.mss.0000183848.25845.e0. [DOI] [PubMed] [Google Scholar]
- 42.Tryon W, Williams R. Fully proportional actigraphy: A new instrument. Behav Res Methods Instrum Comput. 1996;28:392– 403. [Google Scholar]
- 43.Vanhelst J, Beghin L, Rasoamanana P, Theunynck D, Meskini T, Iliescu C, et al. Calibration of the RT3 accelerometer for various patterns of physical activity in children and adolescents. Journal of Sports Sciences. 2010;28(4):381–7. doi: 10.1080/02640410903508821. [DOI] [PubMed] [Google Scholar]
- 44.Weir J. New methods for calculating metabolic rate with special reference to protein metabolism. The Journal of Physiology. 1949;109(1–2):1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Difference in PAL predicted with each regression equation and the room calorimeter measurement stratified by obesity status (obese, BMI ≥95th percentile; non-obese, BMI <95th percentile). Underpredictions fall below the x-axis (0), while overpredictions are above. AC, Actical; AG, ActiGraph; PAL, physical activity level.
* Significant at P<0.001.
Effect of (a) BMI and (b) percent body fat on the predictive accuracy of PAL selected accelerometer predictive equations.


