Abstract
Objective
Prompted by anecdotal evidence of a higher rate of Type 2 diabetes, we set out to investigate the prevalence of diabetes, its risk factors, and co-morbidities among immigrant Guyanese patients being treated in a family medicine health center.
Methods
Patients were ascertained from a registration database of all patients ≥ 30 years old who were treated from 2004 to 2006. We then conducted a detailed retrospective chart review of all Guyanese, Caucasian, African-American, and Hispanic patients with diabetes and randomly selected non-diabetic controls.
Results
Of 222 Guyanese patients, 67 (30.2%) had a diagnosis of diabetes, compared with 47/219 (21.5%) of Hispanics, 132/777 (17.0%) of African-Americans, and 442/2834 (15.6%) of Caucasians (p <0.0001). Compared with the other racial and ethnic groups, the Guyanese diabetic patients were significantly leaner and more likely to be male.
Conclusion
In the population studied, there is a very high prevalence of Type 2 diabetes among Guyanese patients, with unique characteristics when compared with other ethnic and racial groups. These findings have alerted local clinicians to intensify diabetes screening among Guyanese patients. Furthermore, in response to these findings, a broad coalition including public health, clinical, and community groups has been established with the goal of developing culturally appropriate strategies to prevent and control diabetes among Guyanese residents.
Keywords: Guyanese, Guyana, Type 2 diabetes, minorities
INTRODUCTION
Guyana, the third smallest country in South America, is nestled in the north of the continent between Suriname and Venezuela and bordering the Atlantic Ocean. Originally a Dutch colony in the 17th century, Guyana came under British rule in 1815. The abolition of slavery led to black settlement of urban areas and importation of indentured servants from India to work on the sugar plantations.1 According to the 2002 census, the ancestry of the population is 44% East-Indian, 30% African, 17% mixed, and 9% Amerindian. The population is predominantly young with a median age of 23.9 years. Only 4.8% of Guyanese are older than 65 years. Life expectancy is 71.4 years for females and 63.6 years for males. As of July 2011, the population of Guyana was estimated to be 741,908 people.1, 2 According to the Guyanese Ministry of Health, diabetes is ranked as the fourth leading cause of death in the country and the second most prevalent cause of chronic non-communicable disease among individuals above the age of 45 years. 3
Over the past four decades, it is estimated that more than 500,000 people have emigrated from Guyana to North America, with approximately 50,000 people immigrating annually.4 Most of the Guyanese immigrants reside in the Northeastern United States and Canada. In 2006, the Guyanese community was ranked the 5th most populous recent immigrant group in New York City, amounting to a population of 142,946.5
It is estimated that approximately 6,000–10,000 Guyanese have immigrated to Schenectady NY since 2000, Since they are not captured in official census data, absolute statistics are lacking. Spurred by a continuing decline in population (according to census figures, the population of Schenectady dropped 33% from 92,000 in 1950 to 62,000 in 2000), with associated abandoned housing, shuttered store fronts, rising crime rate and a shrinking tax base, the incumbent mayor set out to recruit a new population for the city. 6 Initially, he recruited Guyanese living in Richmond Hills, Queens, NY and later directly from Guyana. These industrious, English-speaking South Americans, largely of Indian heritage (Indo-Guyanese) were offered low cost housing and improved job prospects. The recruitment effort was successful and according to the 2010 census, Schenectady experienced a 7% population increase from 2000 to 2010, thought to be primarily affected by the influx of Guyanese into the city.7
As Guyanese immigrants began to seek medical care in Schenectady, community physicians noted that many had Type 2 diabetes mellitus. Furthermore, diabetes appeared to be more common in younger and leaner men and women than was normally seen among other non-Guyanese patients. These observations led us to conduct an initial retrospective chart review of 140 Guyanese adults seen in our family health center. This initial study revealed an unusually high prevalence of Type 2 diabetes (32.6%), afflicting relatively young (mean age 40.2 years) and lean (66% with BMI <30) Guyanese patients. 8 Medline literature and Google internet searches yielded no reports about diabetes among Guyanese, either in Guyana or in expatriate communities. The absence of information in the medical literature and the results of our initial study prompted us to undertake this study, setting out to characterize diabetes among the Guyanese patients compared to patients of other racial and ethnic groups seen in our primary care health center.
METHODS
Ellis Hospital (formerly St. Clare’s Hospital) is a 300 bed community hospital with a Family Medicine residency program, located in Schenectady, NY. The residency program operates the Family Health Center (FHC), a primary care clinic that serves a diverse urban population. Study patients were ascertained by reviewing an electronic billing database of all patients ≥ 30 years old who were treated at the FHC between May 1, 2004 and April 30, 2006. Elements abstracted from the database included race/ethnicity, age, sex, and ICD-9 diagnosis of diabetes (250.*).
We then conducted a detailed review of paper charts for patients with diabetes and randomly selected non-diabetic controls. The chart review included all Guyanese, African-American, and Hispanic patients with diabetes and a random sample of Caucasian patients with diabetes (chosen to equal the number of diabetic African- American cases). Two controls for each case, matched on race/ethnicity, were randomly selected from the non-diabetic patients of the FHC. Elements abstracted from the charts of all patients included height, weight, calculated body mass index (weight/height2), co-morbid diagnoses of hypertension and hyperlipidemia, and tobacco use. Charts of patients with diabetes were reviewed for accuracy of diabetes diagnosis, HgbA1c levels, and diagnosis of end-organ complications.
Data were compiled using Microsoft Excel spreadsheets & analyzed using EpiInfo™ version 3.5.1 (CDC) software9. Test statistics were chi square, F test from analysis of variance (ANOVA) or Kruskal-Wallace test, where appropriate. For the case control analysis, odds ratios with 95% confidence intervals were computed to compare correlates of diabetes across the racial and ethnic groups. The study was approved by the St. Clare’s Hospital Institutional Review Board.
RESULTS
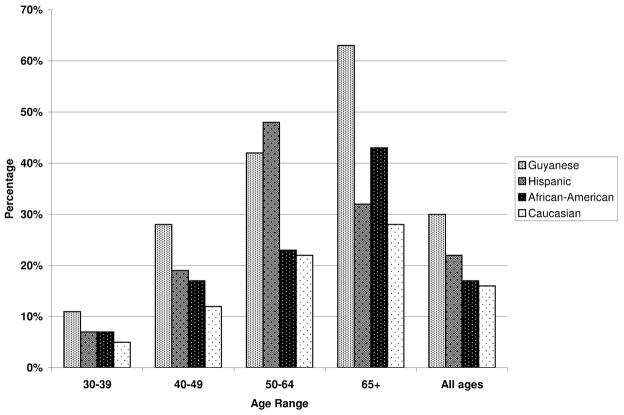
A total of 4,285 patients ≥ 30 years old were seen in the FHC during the study period, including 2,834 (66.1%) Caucasian, 777 (18.1%) African-American, 222 (5.2%) Guyanese, 219 (5.1%) Hispanic, and 233 (5.4%) other. Of the 222 Guyanese patients, 67 (30.2%) had been diagnosed with diabetes, compared with 47/219 (21.5%) of Hispanics, 132/777 (17.0%) of African-Americans, and 442/2834 (15.6%) of Caucasians (p <0.0001). Adjusting for age, using the age distribution of the entire FHC patient population, the rank ordering of prevalence was similar (31.6% among Guyanese, 24.4% among Hispanics, 19.2% among African-Americans, and 14.5% among Caucasians). The probability of being diagnosed with diabetes increased with age (Figure 1). By age 50, over 65% of the Guyanese males and 38% of the females seen in the FHC had been diagnosed with diabetes.
Figure 1.
Prevalence of diabetes by race/ethnicity and age range
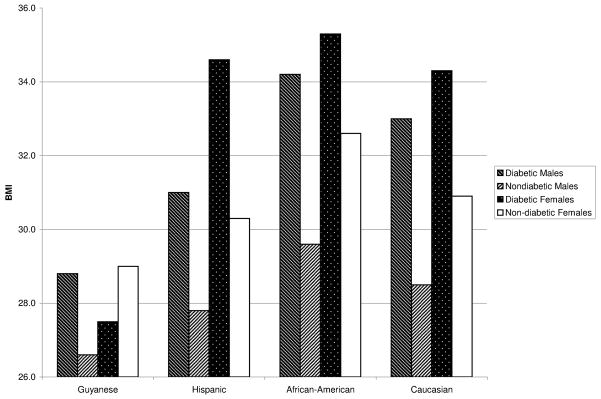
Case-control data on the association of diabetes with sex, age, weight, and BMI are summarized in Table 1. Within the FHC patient population, the increased prevalence of diabetes among men in the Guyanese (OR=2.8) was not observed in Hispanics, African-Americans, or Caucasians (OR=0.9, 1.2, and 1.4, respectively). In contrast, the age of patients and age difference between cases and controls were fairly consistent across race and ethnicity. The analysis of weight and BMI revealed unique features of the Guyanese patients (Table 1, Figure 2). Compared with the other three racial and ethnic groups, the Guyanese patients were leaner and the case-control difference in BMI seen in Hispanics, African-Americans, and Caucasians was smaller among the Guyanese men and reversed in direction for Guyanese women.
Table 1.
Characteristics of diabetic cases and non-diabetic controls, by racial and ethnic group, FHC, 2004–2006
| Characteristic | Guyanese
|
Hispanics
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diabetics | Non-diabetics | OR | 95% CI | p-value | Diabetics | Non-diabetics | OR | 95% CI | p-value | |
| Total n | 67 | 132 | 47 | 94 | ||||||
| Sex | ||||||||||
| Males | 39 (58%) | 44 (33%) | 2.8 | 1.5,5.1 | <0.001 | 18 (38%) | 38 (40%) | 0.9 | 0.5,1.9 | 0.48 |
| Females | 28 (42%) | 88 (67%) | 29 (62%) | 56 (60%) | ||||||
| Mean age (+/−SD) | ||||||||||
| Males | 52.5+/−12.2 | 43.0+/−10.5 | <0.001 | 51.9+/−18.1 | 45.9+/−13.3 | 0.16 | ||||
| Females | 57.4+/−14.4 | 43.8+/−12.1 | <0.001 | 55.8+/−11.9 | 42.9+/−14.0 | <0.001 | ||||
| Mean BMI (+/−SD) | ||||||||||
| Males | 28.6+/−5.0 | 26.4+/−5.2 | 0.04 | 31.0+/−5.6 | 27.9+/−5.2 | 0.04 | ||||
| Females | 27.5+/−4.8 | 29.0+/−5.6 | 0.24 | 34.6+/−7.6 | 30.8+/−6.6 | 0.03 | ||||
| Mean Weight(Kg +/−SD) | ||||||||||
| Males | 81.7+/−14.3 | 75.8+/−16.0 | 0.08 | 93.0+/−21.0 | 83.1+/−14.1 | 0.04 | ||||
| Females | 69.9+/−14.6 | 71.9+/−15.7 | 0.55 | 83.4+/−21.5 | 79.1+/−18.8 | 0.35 | ||||
| Characteristic | African-Americans
|
Caucasians
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diabetics | Non-diabetics | OR | 95% CI | p-value | Diabetics | Non-diabetics | OR | 95% CI | p-value | |
| Total n | 126 | 252 | 126 | 252 | ||||||
| Sex | ||||||||||
| Males | 48 (38%) | 85 (34%) | 1.2 | 0.8,1.9 | 0.23 | 64 (51%) | 105 (42%) | 1.4 | 0.9,2.2 | 0.06 |
| Females | 78 (62%) | 167 (66%) | 62 (49%) | 147 (58%) | ||||||
| Mean age (+/−SD) | ||||||||||
| Males | 48.6+/−10.6 | 43.5+/−9.4 | <0.001 | 57.8+/−12.1 | 47.0+/−12.8 | <0.001 | ||||
| Females | 56.4+/−14.9 | 45.6+/−11.4 | <0.001 | 62.1+/−11.7 | 47.6+/−15.0 | <0.001 | ||||
| Mean BMI (+/− SD) | ||||||||||
| Males | 34.2+/−6.7 | 29.7+/−8.3 | 0.002 | 33.0+/−8.1 | 28.5+/−6.2 | <0.001 | ||||
| Females | 35.3+/−9.1 | 32.6+/−9.1 | 0.04 | 34.4+/−8.2 | 30.9+/−−0.0 | 0.02 | ||||
| Mean Weight(Kg +/−SD) | ||||||||||
| Males | 109.8+/−27.0 | 95.2+/−27.0 | 0.003 | 101.7+/−25.7 | 88.8+/−21.0 | <0.001 | ||||
| Females | 95.7+/−25.4 | 87.4+/−26.6 | 0.02 | 89.4+/−23.0 | 82.2+/−27.7 | 0.07 | ||||
Figure 2.
Body Mass Index (BMI), by race/ethnicity and sex
Data by race and ethnicity and co-morbidities and sequelae often linked with diabetes are summarized in Table 2. Hypertension was strongly associated with prevalence of diabetes in each racial and ethnic group (Odds ratio ranging from 4.6 to 6.5). Hyperlipidemia also was associated with prevalence of diabetes, but more strongly in African-American and Caucasian patients (OR=7.4 and 9.4 respectively) than in Guyanese and Hispanic patients (OR=2.5). Smoking had little association with diabetes among FHC patients, and the prevalence of smoking was markedly low among both diabetic and non-diabetic Guyanese patients.
Table 2.
Co-morbidities, sequelae, and HbgA1c, by racial and ethnic group, FHC, 2004–2006
| Characteristic | Guyanese
|
Hispanics
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diabetics | Non-diabetics | OR | 95% CI | p-value | Diabetics | Non-diabetics | OR | 95% CI | p-value | |
| Total n | 67 | 132 | 47 | 94 | ||||||
| Hypertension | 39 (64%) | 26 (21%) | 5.8 | 3.0,11.3 | <0.001 | 26 (55%) | 15 (16%) | 6.5 | 2.9,14.5 | <0.001 |
| Hyperlipidemia | 41 (68%) | 26 (46%) | 2.5 | 1.2,5.3 | 0.01 | 16 (34%) | 16 (17%) | 2.5 | 1.1,5.6 | 0.02 |
| Current Smoking | 3 (4.6%) | 10 (9.3%) | 0.5 | 0.1,1.8 | 0.25 | 12 (25.5%) | 29 (31.2%) | 0.8 | 0.5,1.8 | 0.49 |
| Mean HgbA1c | 8.3+/−1.8 | 7.9+/−1.9 | ||||||||
| End-organ disease | 24 (35.8%) | 13 (28.9%) | ||||||||
| Characteristic | African-Americans
|
Caucasians
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diabetics | Non-diabetics | OR | 95% CI | p-value | Diabetics | Non-diabetics | OR | 95% CI | p-value | |
| Total n | 126 | 252 | 126 | 252 | ||||||
| Hypertension | 90 (71%) | 89 (35%) | 4.6 | 2.9,7.3 | <0.001 | 80 (64%) | 61 (24%) | 5.4 | 2.9,7.3 | <0.001 |
| Hyperlipidemia | 62 (50%) | 30 (12%) | 7.4 | 4.4,12.4 | <0.001 | 86 (68%) | 47 (19%) | 9.3 | 5.7,15.3 | <0.001 |
| Current Smoking | 57 (45.2%) | 111 (44%) | 1.0 | 0.7,1.6 | 0.83 | 43 (34.1%) | 101 (40.1%) | 0.8 | 0.5,1.2 | 0.26 |
| Mean HgbA1c | 7.6+/−2.1 | 7.8+/−2.0 | ||||||||
| End-organ disease | 32 (26.2%) | 33 (26.4%) | ||||||||
Although not statistically different than the patients from the other ethnic and racial groups, Guyanese patients with diabetes who were seen in the FHC generally had poorly controlled diabetes, with a mean (most recent) HgbA1c of 8.3% (SD 1.9). During the study period, twenty four patients (36%) already had exhibited end-organ damage, having been diagnosed with coronary artery, cerebrovascular, peripheral vascular, renal, and/or ophthalmic disease. Twelve patients (17%) (data not shown) had experienced a myocardial infarction and/or coronary artery bypass surgery, 4 patients (6%) had undergone amputations, 7 patients (10%) had nephropathy, 4 (6%) had suffered a stroke, and 3 (%) were blind in at least one eye. Although the incidence of end-organ disease increased with age, 7 Guyanese patients (23%) under the age of 50 already manifested at least 1 complication.
DISCUSSION AND CONCLUSION
This study of Guyanese patients supports our initial impression that diabetes is significantly more prevalent among these newly arrived immigrants to Schenectady than among other racial and ethnic groups at our practice. Furthermore, the Guyanese with diabetes differ from these other groups, being leaner and more likely to be male. Although the incidence of diabetes among Guyanese increases with age, we did not confirm our initial impression that it was more common among younger Guyanese patients than young patients from other racial or ethnic groups. We found BMIs to be lower among Guyanese patients compared with other ethnic groups, a weaker association between BMI and diabetes in men, and no association in women. This finding is markedly different from the strong association between BMI and weight found in the African-American, Caucasian, and Hispanic patients. Diabetes among the Guyanese studied was not well controlled, 2/3 of patients had hypertension and/or hyperlipidemia, and 1/3 of patients had already experienced at least one end-organ complication.
We believe this study to be the first in the medical literature systematically investigating diabetes among immigrants from Guyana. A literature search yielded only three reports regarding diabetes among Guyanese, either in Guyana or North America. The first was a 2006 report from the New York City Department of Health that listed diabetes as the third leading cause of death among Guyanese-born immigrants. By comparison, diabetes was the sixth leading cause of death among North American-born New Yorkers and fifth among all foreign-born New Yorkers.10 The second was the afore-mentioned report published by the Guyanese Ministry of Health in 2008 that ranked diabetes as the second most prevalent cause of chronic non-communicable disease among individuals over the age of 45 years. 3 The third was a recently published study from New York City which reported a higher incidence of three vessel coronary artery disease, diabetes, hypertension, and dyslipidemia among Guyanese, compared with Caucasian patients referred for cardiac catheterization.11
There is a growing literature regarding the high and increasing prevalence of diabetes in migrant South Asians and Indians, the latter of significance since they constitute the genetic ancestry of the Indo-Guyanese. For example, the prevalence of diabetes among South Asians living in the United Kingdom is estimated to be approximately 20%, which is nearly fivefold higher than the indigenous white population. 12 In South India, the Chennai Urban Rural Epidemiology Study (CURES) screened over 26,000 urban Indian adults and found an overall diabetes prevalence of 15.5%. In the span of 14 years, the prevalence of diabetes increased by 72.3%.13 Similar to the Indo-Guyanese in our study, other published reports reveal that Asian Indians with diabetes are leaner than other populations.13–16
Diabetes is clearly influenced by genetic predisposition, with the thrifty genotype and phenotype and the thin-fat phenotype thought to partially explain the increased risk among Indians. 16 The thrifty genotype theory ascribes the increased susceptibility to diabetes to the evolutionary enrichment of thrifty genes, which enhanced the chances of survival in the past when food supplies were scarce and intermittent, but have become detrimental in contemporary conditions of plentiful food and sedentary lifestyles. The thrifty phenotype hypothesis ascribes the increased risk of diabetes to an unfavorable intrauterine environment. The thin-fat phenotype describes the observation that Indians have a higher percentage of body fat and more visceral fat than members of other populations, increasing their risk for insulin resistance when exposed to increased food and decreased exercise. 16 Irrespective of the underlying etiology and pathogenesis, it is clear that diabetes is increasing in both urban and rural areas in association with improvement in living conditions, and changes in exercise and diet.13, 15–17 We believe that these multiple combined factors help explain the high prevalence of diabetes among the Guyanese immigrants in North America as well.
Our study is limited by its small sample size and the possibility of selection bias. Since all cases were from one family medicine practice, they may not be representative of the community at large and we may have investigated a population consisting of sicker patients with diabetes seeking care. This potential bias could help explain the higher prevalence of diabetes that we found among Guyanese men, who have been noted to be less likely than women to seek medical care unless ill. Nonetheless, approximately 2/3 of the Guyanese patients with diabetes in the study had no known end-organ disease and many were being seen for routine primary care visits. Furthermore, it is reasonable to expect that selection bias would have had a similar influence on the prevalence of diabetes that we found among African-American and Caucasian patients, who had rates of diabetes which were proportionally similar to those reported from the National Health and Nutrition Examination Survey (NHANES) 18
Schenectady clinicians have responded to these findings with a heightened index of suspicion regarding diabetes among Guyanese patients, leading to increased screening of all Guyanese adults, irrespective of traditional risk factors, such as obesity. 19 Appreciating the necessity and importance of public health initiatives in addition to the clinical interventions already underway, the Schenectady County Public Health Department, with the assistance of a coalition of health care providers and citizen groups, successfully applied for and was awarded a REACH (Racial and Ethnic Approaches to Community Health) grant from the Centers for Disease Control and Prevention (CDC).19,20 Currently, mid-way though the two year grant cycle, the health department, in partnership with the Guyanese and West Indian communities, has formed the West Indian Diabetes Action Coalition (WIDAC) to develop primary, secondary and tertiary public health strategies to prevent, identify, and treat Type 2 diabetes and its consequences. The coalition is developing culturally sensitive solutions to the identified diabetes problem that exists in Schenectady, with the goal of sharing lessons with the entire community as well as the CDC. Drawing upon the availability and popularity of current technology, the coalition has developed a Facebook page in order to disseminate high-quality health related information to a wide audience. 21 Other tools and interventions are underway as well.
We are currently in the midst of a worldwide “diabetes epidemic”, with enormous implications for health care needs and costs over the next century.22 As highlighted by this study, despite many similarities, diabetes epidemiology and presentation differs among racial and ethnic groups, requiring public health and clinical providers to approach diabetes prevention and control within a “culturally competent” framework.23–25 In addition to the public health implications, we believe that studying the lean individuals with diabetes who we identified among our Guyanese patients may ultimately provide key insights into the molecular basis of insulin resistance, paving the way for better control and treatment.
Acknowledgments
D.S.S. and Z.S. were supported by the National Institute on Minority Health and Health Disparities, National Institutes of Health (grant number 1 P20 MD003373).
Footnotes
The authors report no potential conflicts of interest to report.
References
- 1.Central Intelligence Agency. The World Factbook. Guyana; 2010. [Accessed March 4, 2012]. https://www.cia.gov/library/publications/the-world-factbook/geos/gy.html. [Google Scholar]
- 2.Pan-American Health Organization. [Accessed March 4, 2012];Health Situation Analysis & Trends Summary: General Situation & Trends. 2010 http://www.paho.org/English/DD/AIS/cp_328.htm.
- 3.Ministry of Health. Republic of Guyana. [Accessed March 4, 2012];Statistical Bulletin. 2008 http://www.health.gov.gy/pub/moh_stats_bulletin_08.pdf.
- 4.Orozco M. Remitting Back Home and Supporting the Homeland: The Guyanese Community in the U.S. Inter-American Dialogue. [Accessed March 4, 2012];Working Paper commissioned by the US Agency for International Development GEO Project. 2003 2003 https://www.thedialogue.org/PublicationFiles/Remitting%20back%20home%20and%20supporting%20the%20homeland.pdf. [Google Scholar]
- 5.Salvo J, Lobo AP. The Hon Jerome and Helene Berg Public Policy Papers on Government Reform Issue No 6. Published by the Hugh L. Carey Center for Government Reform; Wagner College, Staten Island, NY: 2010. [Accessed March 4, 2012]. Monograph: New Immigrants to New York. http://www.wagner.edu/carey_center/monographs. [Google Scholar]
- 6.Kershaw S. The New York Times. Jul 26, 2002. For Schenectady, A Guyanese Strategy; Mayor Goes All Out to Encourage A Wave of Hardworking Immigrants. [Google Scholar]
- 7.US Census Bureau. [Accessed March 4, 2012];State and County Quick Facts. http://quickfacts.census.gov/qfd/states/36/3665508.html.
- 8.Bachwani AS, Back EE. Profile of diabetes among immigrants from Guyana in Schenectady County, NY. Southern Medical Association’s 99th Annual Scientific Assembly: Oral Presentation Abstracts of Scientific Papers. Southern Medical Journal. 2005;98(10 supplement):S9–S10. [Google Scholar]
- 9.http://www.cdc.gov/epiinfo/
- 10.Kim M, Kerker B, Thorpe L, Frieden T. The Health of Immigrants in New York City. [Accessed March 4, 2012];A report from the New York City Department of Health and Mental Hygiene. 2006 Jun; http://www.nyc.gov/html/doh/downloads/pdf/episrv/episrv-immigrant-report.pdf.
- 11.Silbiger JJ, Stein R, Trost B, et al. Coronary angiographic findings and conventional artery disease risk factors of Indo-Guyanese immigrants with stable angina pectoris and acute coronary syndromes. Ethn Dis. 2012;22(1):12–14. [PubMed] [Google Scholar]
- 12.Gholap N, Davies M, Patel K, Sattar N, Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Primary Care Diabetes. 2011 Apr;5(1):45–56. doi: 10.1016/j.pcd.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Mohan V, Deepa M, Deepa R, Shanthirani CS, Farooq S, Ganesan A, Datta M. Secular trends in the prevalence of diabetes and impaired glucose tolerance in urban South India—the Chennai Urban Rural Epidemiology Study (CURES-17) Diabetologia. 2006;49(6):1175–1178. doi: 10.1007/s00125-006-0219-2. [DOI] [PubMed] [Google Scholar]
- 14.Mohan V. Why are Indians more prone to diabetes? J Assoc Physicians India. 2004;52(6):468–74. [PubMed] [Google Scholar]
- 15.Chan JCN, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: Epidemiology, Risk Factors, and Pathophysiology. JAMA. 2009;301(20):2129–2140. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- 16.Yaznik CS. Early Life Origins of Insulin Resistance and Type 2 Diabetes in India and Other Asian Countries. J Nutr. 2004;134(1):205–10. doi: 10.1093/jn/134.1.205. [DOI] [PubMed] [Google Scholar]
- 17.Ramachandran A, Snehalatha C, Baskar ADS, Mary S, Sathish Kumar CKS, Selvam S, Catherine S, Vijay V. Temporal changes in prevalence of diabetes and impaired glucose tolerance associated with lifestyle transition occurring in the rural population in India. Diabetologia. 2004;47(5):860–865. doi: 10.1007/s00125-004-1387-6. [DOI] [PubMed] [Google Scholar]
- 18.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. NCHS data brief, no 36. Hyattsville, MD: National Center for Health Statistics; 2010. [Accessed March 4, 2012]. Hypertension, High Serum Total Cholesterol, and Diabetes: Racial and Ethnic Prevalence Differences in U.S. Adults, 1999–2006. http://www.cdc.gov/nchs/data/databriefs/db36.pdf. [PubMed] [Google Scholar]
- 19.Lamendola M. Diabetes initiatives earn praise: State health leader applauds prevention efforts in county. Schenectady Gazette. 2011 Apr 5; [Google Scholar]
- 20.Schenectady County Department of Public Health. [Accessed March 4, 2012];REACH: Racial and Ethnic Approaches to Community Health. 2011 http://www.schenectadycounty.com/FullStory.aspx?m=870&amid=10532.
- 21. [Accessed March 7, 2012];West Indian Diabetes Action Coalition. http://www.facebook.com/WIDACNY.
- 22.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 23.Eged LE, Dagogo-Jack S. Epidemiology of Type 2 diabetes: focus on ethnic minorities. Med Clin N Am. 2005;89(5):949–975. doi: 10.1016/j.mcna.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Julkarni KD. Food, culture, and diabetes in the United States. Clinical diabetes. 2004;22(4):190–192. [Google Scholar]
- 25.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O., II Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;18(4):293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]