Although cigarette smoking is associated with insulin resistance and an increased risk for type 2 diabetes (1), few studies have examined the metabolic and molecular effects of smoking cessation in humans. Epidemiological data from the Atherosclerosis Risk in Communities study in middle-aged men and women offer several insights into the relationship between smoking cessation and diabetes. This study suggests that individuals who quit smoking are at increased risk of type 2 diabetes and that this risk is highest in the first 2 years after smoking cessation, but that risk declines after this point until no excess risk is observed at 12 years after cessation. The increased risk of type 2 diabetes associated with smoking cessation seems to be partially mediated by weight gain (2,3). In this issue of Diabetes, Bergman et al. (4) examined the metabolic and molecular effects of smoking cessation (for 1–2 weeks) in young, lean, otherwise healthy college students, a population that is increasingly vulnerable to the effects of both cigarette smoking and second-hand smoke exposure. Their results suggest that skeletal muscle insulin resistance in smokers is associated with increased mammalian target of rapamycin (mTOR)/p70S6 K activity and insulin receptor substrate-1 (IRS-1) Ser636 phosphorylation by nicotine, and these effects are reversible with smoking cessation.
Cigarette smoking increases energy expenditure (Fig. 1), and this effect may be mediated in part by the sympathetic nervous system (5). In addition, smoking enhances lipid mobilization. Hellerstein et al. (6) demonstrated that cigarette smoking acutely increased free fatty acid (FFA) and glycerol fluxes as well as circulating FFA concentrations due to nicotine-induced lipolysis. Cigarette smoking increased delivery of FFA to the liver, increased hepatic reesterification of FFA, and enhanced VLDL secretion, thereby promoting the atherogenic effects of smoking. There were no acute effects of smoking on de novo lipogenesis, whole body fat oxidation, adipocyte reesterification of FFA, or basal hepatic glucose production. Finally, cessation of smoking for a period of only 1 week (while on an isocaloric diet) was not associated with a rebound reduction in fat mobilization, suggesting the absence of a metabolic predisposition to gain weight, assuming there is no increase in caloric intake. However, chronic nicotine withdrawal increases appetite and food intake. Nicotine directly activates the brain melanocortin system in rodents via hypothalamic α3β4-nicotinic acetylcholine receptors, and the weight gain associated with cessation of smoking is due to reduced activity of melanocortin 4 receptors (7,8). More recently, nicotine has been shown to inhibit hypothalamic AMP-activated protein kinase and enhance brown adipose tissue activation, likely via the sympathetic nervous system. On the other hand, nicotine withdrawal restores energy balance by normalizing feeding, thermogenesis, and lipid mobilization via normalization of AMP-activated protein kinase activity (9).
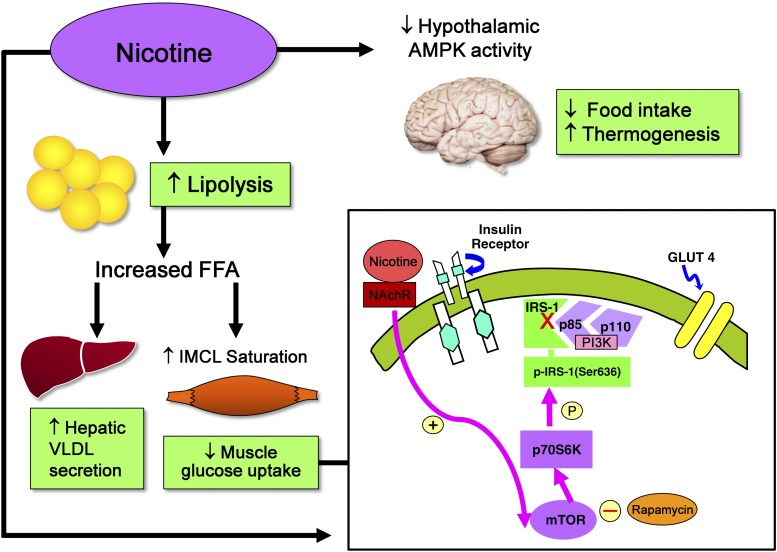
FIG. 1.
Metabolic and molecular effects of smoking (4–11). Nicotine inhibits hypothalamic AMP-activated protein kinase (AMPK) activity, decreases food intake, and increases thermogenesis. Nicotine enhances lipolysis and increases the delivery of FFA to the liver and skeletal muscle. These effects of nicotine are associated with increased hepatic VLDL secretion and intramyocellular lipid (IMCL) saturation as well as peripheral insulin resistance. Nicotine increases mTOR/p70S6 K activity in cultured L6 myotubes in association with increased IRS-1 Ser 636 phosphorylation and reduced insulin-stimulated glucose uptake, and mTOR inhibitor rapamycin blocks these effects of nicotine. NAchR, nicotinic acetylcholine α1 receptors; P, phosphorylation.
In rodents, nicotine treatment is associated with enhanced lipolysis, decreased adipose tissue lipoprotein lipase activity, and increased muscle lipoprotein lipase activity (10). Given these findings, Bergman et al. (11) previously examined the effects of smoking on insulin sensitivity and skeletal muscle lipid metabolism. It is noteworthy that there were no differences in skeletal muscle triglyceride (IMTG) or diacylglycerol (DAG) concentration between smokers and nonsmokers in this work despite the presence of nicotine-induced insulin resistance. IMTG fractional synthesis rates were also similar between smokers and nonsmokers. However, Bergman et al. reported increased saturation of both IMTG and DAG in smokers. The only intracellular mediator of nicotine-induced skeletal muscle insulin resistance that the investigators identified in smokers was increased basal IRS-1 Ser636 phosphorylation in skeletal muscle. Interestingly, the effects of smoking on skeletal muscle long-chain fatty acyl-CoA and ceramide, two other lipid metabolites associated with skeletal muscle insulin resistance (12,13), have not been studied.
As a logical extension of their previous work, Bergman et al. now report the effects of smoking cessation for 1–2 weeks on insulin sensitivity, skeletal muscle insulin signaling, and lipid metabolism in young smokers and compare these results to a control group of healthy nonsmokers. They also explore the role of IRS-1 Ser636 phosphorylation as a mediator of nicotine-induced skeletal muscle insulin resistance. Bergman et al. report that smoking cessation is associated with an improvement in insulin sensitivity in the absence of changes in adiposity or body weight. Consistent with previous studies, the rate of appearance of palmitate was significantly higher in smokers versus nonsmokers and did not change after smoking cessation. As expected, the rate of glucose appearance, whole body fat oxidation, rate of oxidation of palmitate, skeletal muscle IMTG and DAG concentrations as well as IMTG fractional synthesis rates were similar in smokers and nonsmokers and did not change significantly after the intervention. Interestingly, the increase in IMTG and DAG saturation in smokers persisted following smoking cessation. Basal IRS-1 Ser636 phosphorylation was elevated in smokers but decreased significantly following smoking cessation. In cultured L6 myotubes, nicotine exposure significantly increased IRS-1 Ser636 phosphorylation. Since IRS-1 Ser636 phosphorylation is increased by mTOR activation, the investigators proceeded to demonstrate that nicotine acutely increases mTOR activation in cultured myotubes. These effects on IRS-1 Ser636 phosphorylation were blocked by rapamycin. Consistent with these results, nicotine reduced insulin-stimulated glucose uptake in L6 myotubes, and insulin sensitivity was restored by rapamycin.
This study provides convincing evidence of a direct and partially reversible effect of nicotine on skeletal muscle insulin resistance by increasing IRS-1 Ser636 phosphorylation. However, it should be noted that the improvement in insulin sensitivity following smoking cessation was partial, and the metabolic and molecular mechanisms responsible for the persistence of residual insulin resistance despite smoking cessation need to be further investigated. Although the bulk of evidence from their work does not suggest a key role for intramyocellular lipid as a mediator of nicotine-induced insulin resistance in smokers, measurements of skeletal muscle ceramide and long-chain fatty acyl-CoA content following smoking cessation need to be performed in future studies. In addition, the precise molecular mechanisms by which activation of the nicotinic acetylcholine α1 receptors in the muscle by nicotine results in mTOR activation need to be investigated. Furthermore, measurement of skeletal muscle IRS-1 Ser636 phosphorylation was performed by these investigators in a basal state, and the effect of insulin stimulation on downstream insulin signaling needs to be examined in smokers. Finally, the chronic effects of smoking cessation on insulin sensitivity and β-cell function, as well as adiposity and fat topography, need to be examined in future studies given the association between smoking cessation and weight gain.
As suggested by the authors, these results are important as they provide the basis for investigating therapeutic agents that oppose skeletal muscle mTOR activation as a strategy for preventing the deleterious metabolic effects of smoking in those who cannot break the habit. Future clinical studies are essential to provide further evidence for the effectiveness of such interventions. However, it must be emphasized that these therapeutic strategies will never replace effective educational programs to prevent smoking among adolescents and young adults.
ACKNOWLEDGMENTS
This work was supported by a Clinical and Translational Research Grant from the American Diabetes Association to M.B. Additional support was from Diabetes and Endocrinology Research Center (NIH P30 DK-079638).
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 3156.
REFERENCES
- 1.Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 2007;298:2654–2664 [DOI] [PubMed] [Google Scholar]
- 2.Yeh HC, Duncan BB, Schmidt MI, Wang NY, Brancati FL. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: a cohort study. Ann Intern Med 2010;152:10–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr 2008;87:801–809 [DOI] [PubMed] [Google Scholar]
- 4.Bergman BC, Perreault L, Hunerdosse D, et al. Novel and reversible mechanisms of smoking-induced insulin resistance in humans. Diabetes 2012;61:3156–3166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hofstetter A, Schutz Y, Jéquier E, Wahren J. Increased 24-hour energy expenditure in cigarette smokers. N Engl J Med 1986;314:79–82 [DOI] [PubMed] [Google Scholar]
- 6.Hellerstein MK, Benowitz NL, Neese RA, et al. Effects of cigarette smoking and its cessation on lipid metabolism and energy expenditure in heavy smokers. J Clin Invest 1994;93:265–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mineur YS, Abizaid A, Rao Y, et al. Nicotine decreases food intake through activation of POMC neurons. Science 2011;332:1330–1332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seeley RJ, Sandoval DA. Neuroscience: weight loss through smoking. Nature 2011;475:176–177 [DOI] [PubMed] [Google Scholar]
- 9.Martínez de Morentin PB, Whittle AJ, Fernø J, et al. Nicotine induces negative energy balance through hypothalamic AMP-activated protein kinase. Diabetes 2012;61:807–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sztalryd C, Hamilton J, Horwitz BA, Johnson P, Kraemer FB. Alterations of lipolysis and lipoprotein lipase in chronically nicotine-treated rats. Am J Physiol 1996;270:E215–E223 [DOI] [PubMed] [Google Scholar]
- 11.Bergman BC, Perreault L, Hunerdosse DM, Koehler MC, Samek AM, Eckel RH. Intramuscular lipid metabolism in the insulin resistance of smoking. Diabetes 2009;58:2220–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bajaj M, Suraamornkul S, Romanelli A, et al. Effect of a sustained reduction in plasma free fatty acid concentration on intramuscular long-chain fatty Acyl-CoAs and insulin action in type 2 diabetic patients. Diabetes 2005;54:3148–3153 [DOI] [PubMed] [Google Scholar]
- 13.Adams JM, 2nd, Pratipanawatr T, Berria R, et al. Ceramide content is increased in skeletal muscle from obese insulin-resistant humans. Diabetes 2004;53:25–31 [DOI] [PubMed] [Google Scholar]