Abstract
Objective:
To detail the presentation of two elite female soccer players with right thigh pain that occurred during training. This article will outline the investigation, diagnosis and management of their cases.
Clinical Features:
The patients presented with anterior thigh pain following injuries incurred during training camp. Both were diagnosed with acute muscular strain and associated muscular hematomas. The plans of management included rest and removal from sport, cryotherapy, and interferential current. Treatment progressed to soft tissue therapy and rehabilitative exercises. The patient in the first case received additional treatment from another practitioner that involved aggressive soft tissue therapy and a strengthening program in the initial stages of recovery.
Outcome Measures:
For both athletes, outcome measures included return to play and re-injury.
Summary:
Two female elite soccer players presented with acute muscle strain and hematoma. These case reports attempt to highlight the differences in treatment options in female soccer players.
Keywords: soccer, athlete, injury
Abstract
Objectif :
Exposer en détail la douleur à la cuisse droite présentée par deux joueuses élites de soccer, qui est survenue au cours de leur entraînement. Cet article souligne l’enquête, le diagnostic et le traitement de ces cas.
Caractéristiques cliniques :
Les patientes ont présenté des douleurs au côté antérieur de la cuisse résultant de blessures encourues durant un camp d’entraînement. Les deux patientes ont reçu le diagnostic de claquage musculaire aigu et d’hématomes musculaires associés. Les plans de traitement comportaient des périodes de repos et d’arrêt de l’activité sportive, de la cryothérapie et de l’électrothérapie à courants interférentiels. Le traitement a progressé vers une thérapie des tissus mous et des exercices de réadaptation. Dans le premier cas, la patiente a reçu des traitements supplémentaires d’un deuxième praticien, qui comportaient une thérapie des tissus mous énergique ainsi qu’un programme de renforcement durant les premiers stades du rétablissement.
Critères d’évaluation :
Les critères ayant servi à l’évaluation des deux athlètes comprenaient notamment le retour à l’activité sportive et l’apparition de nouvelles blessures.
Résumé :
Deux joueuses de soccer élites se sont présentées avec des claquages musculaires aigus et des hématomes. Ces études de cas tentent de mettre en évidence les différences entre les options de traitements s’offrant aux joueuses de soccer.
Keywords: soccer, athlète, blessure
Introduction:
Soccer is the most popular amateur sport in Canada. Over 873,032 players were registered in 2008.1 In 2008, more than 375,000 females played soccer in Canada comprising 43% of total players.1 Although there is growing female participation, there is limited epidemiologic research reporting injuries in these athletes.
Injury rates in female soccer players have ranged from 1.2–24 per 1000 exposure hours, depending on age, level and time in season.2 In a prospective cohort study over eight seasons, Le Gall et al. examined injuries in young elite female soccer players in France.2 They found that over an eight-season period, the rate of injury was 6.4 per 1000 exposure hours (95% CI, 5.9–6.9).2 In total, 110 of the 119 players sustained a documented injury in training or competition.2 In the United States, Leininger et al. studied the epidemiology of pediatric soccer-related injuries presenting emergency departments over a 13-year period and reported an estimated 1,597,528 injuries over this time.3
In general, muscle injuries (including strains and contusions) are the most commonly reported injuries in sport.4 This trend was clearly demonstrated in the study by Leininger et al. as sprain/strain injuries were the most common (35.9%), followed by contusions and abrasions (24.1%).3 Further, this study demonstrated the lower extremity was the most commonly injured area.3
Given the relative paucity of literature regarding injuries in elite, adolescent female soccer players, the objective of these case reports is to detail the presentation of two national under-17 soccer players who sustained right thigh injuries during a training camp. Further, it will outline the investigation, diagnosis and treatment of their cases to assist practitioners in their management of similar cases.
Case Reports:
Case 1
This case report involved a 16-year-old female soccer player with right anterior thigh pain following the National Under-17 (U17) training camp one-week prior due to repeated kicking. She was initially assessed during the camp, but presented to the health care facility at the Provincial and National Soccer Training Centre – Ontario (PNSTC-o), under the direction of a Fellow of the Royal College of Chiropractic Sports Sciences (Canada) (RCCSS(C)) for follow-up in January 2010. At the time of presentation, the intensity of her pain was rated as 7/10 on a written numeric pain rating scale (NPRS), with extension and kicking reported as the most aggravating activities. She had been treated with soft tissue therapy involving movement and instrument-assisted soft tissue therapy while at the camp, and was cleared to practice, with the provision she warmed up prior and stretched and iced following. She had not undergone diagnostic imaging or taken any medication for her complaint.
On physical exam, no divot or defect was observed. The patient was unable to perform a squat due to pain. She reported pain with active extension and passive flexion of the right knee, while all other lower limb ranges of motion were within normal limits. During palpation, pain and tenderness was localized to the distal right vastus lateralis and rectus femoris. Lower limb neurological and peripheral vascular examinations were within normal limits.
The patient was diagnosed with a strain of the right vastus lateralis and rectus femoris, and was referred for an immediate diagnostic ultrasound to determine the extent of her injury. Her plan of management included cryotherapy to the area of chief complaint (10 minutes ice on/10 minutes ice off/10 minutes ice on (10/10/10) protocol), interferential current (IFC) (80 – 120 Hz for 10 min followed by 0–20 Hz for 10 minutes), cold laser therapy (Class I infrared) for six visits (three times per week for two weeks), with removal from sport-specific and lower-body training.
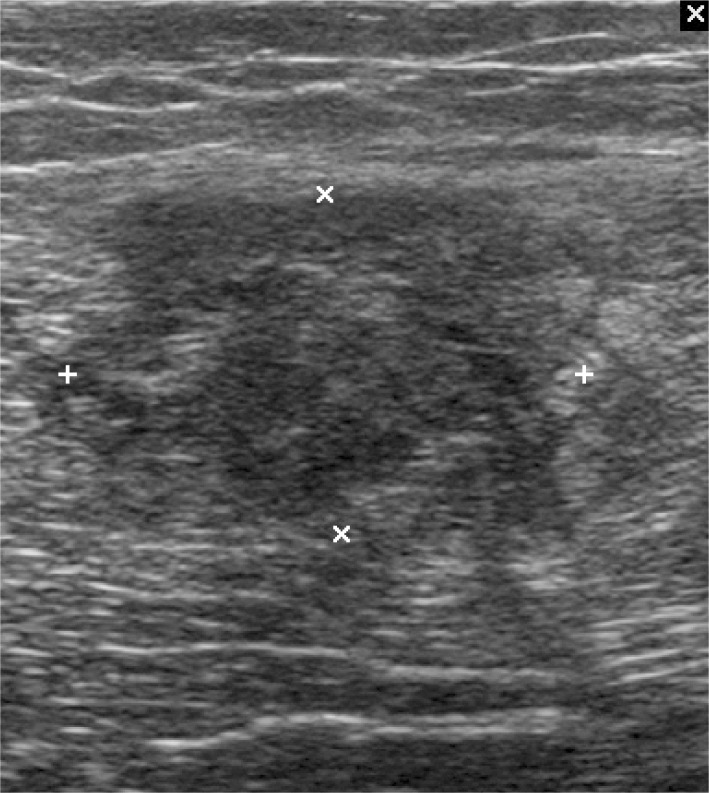
The initial diagnostic ultrasound revealed a hematoma in the right rectus femoris measuring 5.8cmx1.7cmx2.5cm likely related to a partial tear of the muscle (Figure 1). She returned home following this appointment. She received additional treatment from her personal therapists (personal trainer and Certified Athletic Therapist), which had not been recommended originally. This treatment consisted of aggressive manual soft tissue therapy and an active care program of right hip and knee strengthening and assisted stretching.
Figure 1:
Initial diagnostic ultrasound: case one, right rectus femoris. Measures 5.8cmx1.7cmx2.5cm (outline indicated by white markers).
On February 13, 2010 she returned to the Provincial and National Training Centre with decreased pain and increased range of motion (ROM), but had not yet been able to resume training. Effusion and tenderness had decreased, however, palpation of the muscles continued to elicit pain. Cryotherapy and IFC were again provided for pain control, but the athlete was still unable to return to training.
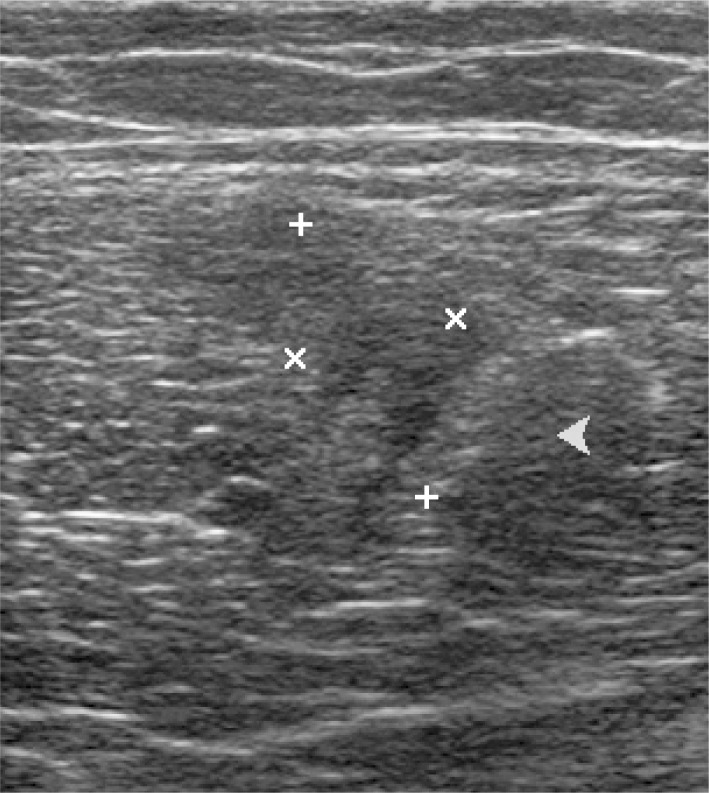
As the complaint had yet to resolve upon re-evaluation (two weeks from initial presentation), the athlete was sent for follow-up diagnostic ultrasound which revealed a decrease in the size of the hematoma (3.4cmx1.2cmx0.29cm), but incomplete healing of a partial thickness tear of the right rectus femoris. A third diagnostic ultrasound performed one week later demonstrated heterogeneity of the rectus femoris (consistent with a residual scar), indicating that the previously described tearing was continuing to heal but not healed (Figure 2).
Figure 2:
Follow up diagnostic ultrasound: case one, right rectus femoris two weeks later. Measures 3.4cmx1.2cmx0.29cm (indicated by white markers).
Following a week of treatment at the Provincial and National Training Centre, the athlete eventually received clearance to return to play in February 2010 and was authorized to compete in the U17 World Cup tournament. Unfortunately, she re-aggravated her condition during pre-competition training and could not compete during the World Cup.
Case 2
This case report involved a different 16-year-old female soccer player who presented to PNSTC-O, under the direction of a RCCSS(C) Fellow in January 2010 with right groin pain. The injury occurred following the following repetitive kicking drills at the National U17 training camp. She recalled bruising at the time of pain onset and reported mild swelling in the area of chief complaint at the time of presentation. At that time, the intensity of her pain was rated as 7/10 on a written NPRS. The pain was localized to the right groin without radiation or referral. Kicking was the only aggravating activity reported. She had not undergone diagnostic imaging or taken any medication for her complaint.
On physical exam, the mild swelling was observed. Active, passive and resisted hip ranges of motion were full, however, resisted adduction recreated pain in the right groin. During palpation, tenderness was localized to the right adductor longus. Lower limb neurological and peripheral vascular examinations were within normal limits.
Differential diagnoses of right adductor longus or pectineus strains were considered, and the athlete was referred for diagnostic ultrasound to identify the structures involved. Her plan of management included cryotherapy to the area of chief complaint (10/10/10 protocol), IFC (10 min of 80 – 120 Hz and then 10 min of 0 – 20 Hz), with progression to soft tissue therapy, proprioceptive neuromuscular facilitation (PNF) over twelve visits (three times a week for 4 weeks), and removal from sport-specific and lower-body training. Treatment was provided by the RCCSS(C) Fellow at the PNSTC-O.
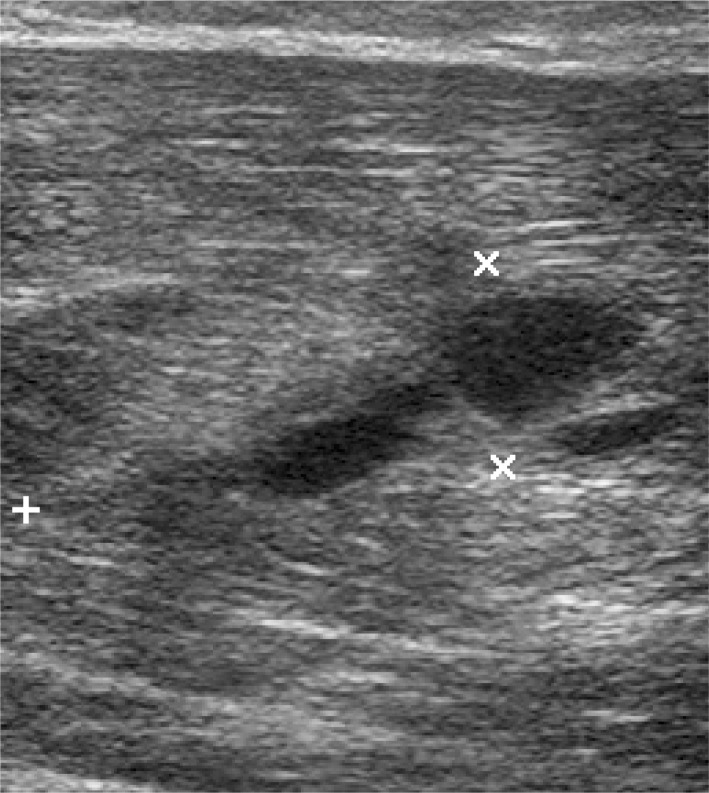
The initial diagnostic ultrasound revealed a 3.4x1.3cm defect in the mid-belly of the adductor longus with an associated hematoma, indicating a partial intrasubstance tear of the muscle (Figure 3).
Figure 3:
Initial diagnostic ultrasound: case two, right adductor longus. Measures 3.4x1.3cm (indicated by white markers).
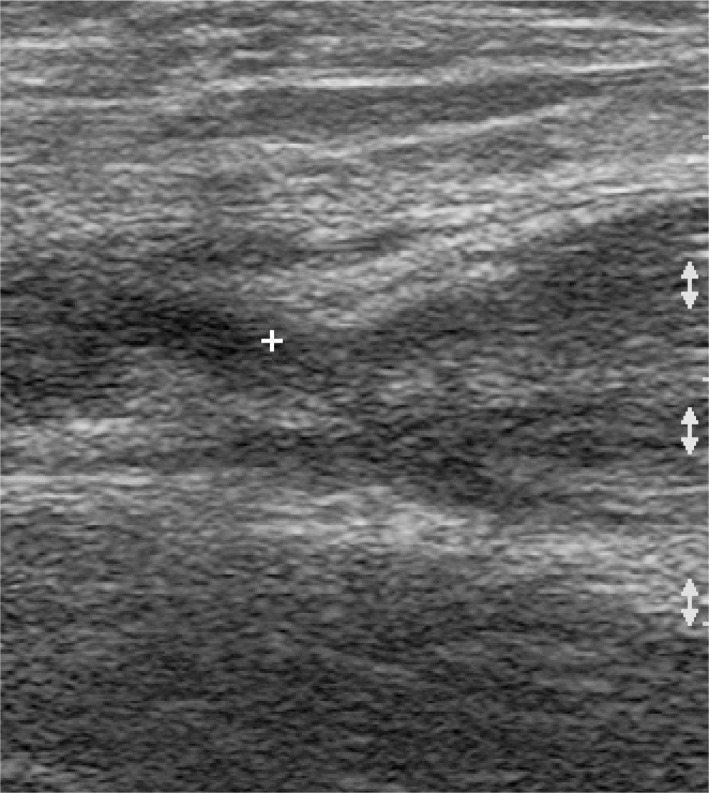
Over the course of the initial treatment plan, the athlete’s pain and swelling progressively decreased, and function returned. She was able to begin using a pneumatic isokinetic device to strengthen her adductors after eight treatments (nine days). After 10 treatments (two weeks), follow-up imaging was performed and revealed a healing scar indicating that the tear in adductor longus has healed (Figure 4). The athlete was then cleared to resume field training and practicing with the national team. She was able to compete in the U17 World Cup tournament.
Figure 4:
Follow up diagnostic ultrasound: case two, right adductor longus, two weeks later. Healed scar indicated by white marker.
Discussion:
With increasing participation in soccer, it is likely that injury rates from participation may increase proportionately, and it is certainly possible that these athletes may present to a chiropractic practice. According to the 2010 National Board of Chiropractic Examiners – Practice Analysis of Chiropractic, lower extremity injuries comprise 8.8% of chief complaints seen by chiropractors. Further, sport, exercise and recreation injuries make up 12.0% of the etiology of patient conditions.5 Given their prevalence in practice, clinicians should be familiar with the presentation of muscular injuries in the thigh related to the forceful eccentric contractions of these muscles during kicking.6 Additionally, chiropractors should be able to understand the pathomechanics of these soft tissue injuries.
Muscle strains are defined as a shearing injury, damaging both the myofibers and the associated endomysial sheaths.4 They are graded from one to three depending on the severity of tissue damage. Grade one strains present with tearing of few myofibers with minor swelling and discomfort and minimal loss of strength or range of motion (ROM).4 Grade two present with a clear loss of strength due to the increased number of myofibers damaged, and grade three tears represent a tear through the entire muscle and mysial sheaths, and result in complete loss of function, often accompanied by a palpable defect.4,6
As demonstrated in these case reports, muscle strains may result in large hematomas due to the associated tearing of intramuscular blood vessels.4 Hematomas are described as intramuscular if the epimysium contains the hematoma, or intermuscular if the fascia is ruptured.4 Although intermuscular hematomas appear dramatic due to the resultant bruising and swelling, intramuscular hematomas are considered a more serious condition as the intact fascia creates an increase in pressure, which compresses the capillary system as the bleed progresses.7 Due to this compression, these bleeds frequently present with greater pain and athletes typically require longer periods of rest before returning to sport.7 The prognosis for intramuscular hematomas is therefore worse than intermuscular hematomas, and expert opinion suggests treating these bleeds more cautiously to avoid the development of further complications, such as the potential for myositis ossificans traumatic.7,8
To assist clinicians in their understanding and management of hematomas, Jackson and Feagin developed a classification system for thigh contusions.9 Mild contusions were classified as those injuries that presented with localized tenderness in the quadriceps, total knee ROM of 90° or greater and no alterations in gait pattern.9 Moderate contusions presented with a swollen, tender mass, knee ROM less that 90°, and altered gait favouring the injured limb.9 Severe contusions presented with marked tenderness, swelling and guarding to palpation combined with less than 45° of motion in the knee.9 The authors of this prospective cohort linked the severity of contusion with disability time, contributing to the understanding of natural history for contusions.9 Although no further studies have examined the application of this classification system in sport, this information may benefit clinicians in their formulation of prognosis by understanding the severity of a contusion. Current recommendations suggest that athletes should be pain-free with at least 120° of total knee ROM and ability to perform functional activities of sport .6,10 Future studies and case reports may effectively use this classification system in grouping athletes by severity and creating return-to-play guidelines.
Clinical presentation
As demonstrated in these cases, patients frequently report a sharp and local pain in the area of injury, commonly associated with decrease in strength or loss of function in the affected muscle.6 Physical exam immediately following the injury is commonly unremarkable, however, follow-up examination 24 hours following the injury may demonstrate swelling, ecchymosis, deformities such as bulging or defects, limitations in range of motion, and weakness.6,10 Given the potential for delay in developing clinical signs and symptoms, it is imperative that practitioners follow-up with athletes in order to make the correct diagnosis and guide management. If more serious injuries, such as avulsion fracture, compartment syndrome, or complete muscular rupture are suspected, appropriate testing and imaging should be considered.
Ultrasonographic imaging (US) was used to confirm the diagnosis of a muscle strain and measure the hematoma in each of the cases presented in this report. US is highly operator dependent, and thus, requires a skilled and experienced technician in order to ensure accurate results, however, it is considered to be an excellent imaging modality to visualize soft tissue anatomy.5,7,11 Further, US imaging has the ability to image muscles dynamically and can also assess for local bleeding and the development of hematoma following injury.6 As demonstrated in these case reports, follow-up US can be used to quantify the extent of healing and assist in guiding return to play decisions in the context of clinical information.
Treatment
Although quadriceps strains and contusions are reported as a common injury, there is little high quality evidence available to guide practitioners in appropriate treatment. 6,12,13 Recent reviews regarding manual treatment for quadriceps contusions and strains have not supported the efficacy of specific treatment approaches.12,13 Ice, heat, compression and combined physical therapy have been suggested as useful treatments; however, this is largely based on the results of animal-model research, expert opinion and empirical observation.13 The most consistent recommendation in the literature has been relative rest to avoid further damage and pain.6,12 Commonly, injury management in the acute phase has been focused on the RICE (rest, ice, compression, elevation) protocol, with varying recommendations for the application and efficacy of this approach.6,13 Cryotherapy (ice) has been advocated as it creates vasoconstriction and may limit the development of extensive hematoma; however, this research has been focused on animal studies.13 Compression has also been found to alter intramuscular blood flow but significant differences in time to recovery have not been demonstrated.13 Elevation has been empirically reported to decrease swelling by altering the pressure gradient to increase drainage from a limb, yet it has not been demonstrated to alter healing or return to play.13
Given that few high quality studies have demonstrated significant differences in treatment approaches, clinicians must rely on practical guidelines, previous experiences and outcome measures in order to formulate an appropriate plan of management. In these case reports, two patients sustained very similar injuries; however, the first patient received aggressive soft tissue therapy and early active care (without relative rest of the injured limb), which may have been related to the delay in her recovery. With the inherent limitations of case studies, no clear conclusion can be drawn from the management of these two patients; however, this case does reflect the trends in the literature regarding the importance of relative rest in acute injury management.
Summary:
Two National U-17 female soccer players presented to the Provincial and National Soccer Training Centre – Ontario with strains of thigh muscles and associated hematomas following participation in training camp. Although the plan of management originally prescribed was similar for both athletes, the athlete in case one received additional care in the form of aggressive soft tissue therapy and did not adhere to the recommendation of relative rest of the injured limb. These case reports aimed to highlight the differences in treatment strategies recommended for a muscular strain with associated hematoma in female soccer players and the importance of relative rest and a conservative approach to care with graded return to activity. Future research should investigate the role of conservative care and manual therapy in the management of muscle injuries with subjective and objective outcome measure to guide clinicians in their approach to care and return to play.
Footnotes
Conflicts of Interest: none declared
Sources of Funding: none declared
Patients consent provided. REB approval by CMCC.
References
- 1.Ottawa, ON: c2011. Canada Soccer [homepage on the Internet] [cited 2011 April 24]. Available from: http://canadasoccer.com. [Google Scholar]
- 2.Le Gall F, Carling C, Reilly T. Injuries in young elite female soccer players: An 8-season prospective study. Am J Sports Med. 2008;36:276–284. doi: 10.1177/0363546507307866. [DOI] [PubMed] [Google Scholar]
- 3.Leininger RE, Knox CL, Comstock RD. Epidemiology of 1.6 million pediatric soccer-related injuries presenting to US emergency departments from 1990 to 2003. Am J Sports Med. 2007;35:288–293. doi: 10.1177/0363546506294060. [DOI] [PubMed] [Google Scholar]
- 4.Jarvinen TA, Kaariainen M, Jarvinen M, Kalimo H. Muscle strain injuries. Curr Opin Rheumatol. 2000;12:155–161. doi: 10.1097/00002281-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 5.National Board of Chiropractic Examiners Practice analysis of chiropractic 2010. 2010. Greeley Colorado.
- 6.Kary JM. Diagnosis and management of quadriceps strains and contusions. Curr Rev Musculoskelet Med. 2010;3:26–31. doi: 10.1007/s12178-010-9064-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith C, Kruger MJ, Smith RM, Myburgh KH. The inflammatory response to skeletal muscle injury. Sports Med. 2008;38:947–969. doi: 10.2165/00007256-200838110-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gray SD. Haematoma and myositis ossificans. Aus J Physiother. 1977;23:147–152. doi: 10.1016/S0004-9514(14)60859-X. [DOI] [PubMed] [Google Scholar]
- 9.Jackson DW, Feagin JA. Quadriceps contusions in young athletes: Relation of severity of injury to treatment and prognosis. J Bone Jt Surg (Am) 1973;55:95–105. [PubMed] [Google Scholar]
- 10.Diaz JA, Fischer DA, Rettig AC, Davis TJ, Shelbourne KD. Severe quadriceps muscle contusions in athletes. Am J Sports Med. 2003;31:289–293. doi: 10.1177/03635465030310022201. [DOI] [PubMed] [Google Scholar]
- 11.Bianchi S, Zwaa A, Abdelwahab IF, Banderali A. Diagnosis of tears of the quadriceps tendon of the knee: Value of sonography. Am J Roentgenol. 1994;162:1137–1140. doi: 10.2214/ajr.162.5.8165998. [DOI] [PubMed] [Google Scholar]
- 12.Beiner JM, Jokl P. Muscle contusion injury and myositis ossificans traumatica. Clin Orthop Relat Res. 2002;403S:S110–S119. doi: 10.1097/00003086-200210001-00013. [DOI] [PubMed] [Google Scholar]
- 13.Smith TO, Hunt NJ, Wood SJ. The physiotherapy management of muscle hematomas. Phys Ther Sport. 2006;7:201–209. doi: 10.1016/j.ptsp.2006.06.001. [DOI] [PubMed] [Google Scholar]