Abstract
The largest investments in AIDS prevention targeted to the general population are being made in interventions where the evidence for large-scale impact is uncertain.
Several decades into the AIDS pandemic, HIV transmission in most of the world remains firmly concentrated among sex workers, men who have sex with men (MSM), and/or injecting drug users (IDUs), and their sexual partners (1). In some parts of Africa, where over two-thirds of infections occur globally, HIV has expanded outside these high-risk groups, creating generalized, predominantly heterosexual epidemics. In nine southern African countries, more than 10% of adults are infected with HIV. Such devastating epidemics have frequently been attributed to poverty, limited health services, illiteracy, war, and gender inequity. Although these grave problems demand an effective response in their own right, they do not appear to be the immediate causes of generalized epidemics (2).
Some assumptions that drive current HIV prevention strategies are unsupported by rigorous evidence. The presumption, for example, that poverty increases vulnerability to HIV infection is challenged by studies such as an analysis of recent Demographic and Health Surveys (DHSs) from Africa, which show a strong positive correlation between HIV prevalence and wealth in eight countries examined (3, 4). [see supporting online material (SOM)]. Among Kenyan women, HIV prevalence is 3.9% in the lowest economic quintile and 12% in the highest. A study of serodiscordant couples found that, across 12 African nations, the woman was the HIV-infected partner in 34 to 62% of these couples, which suggests that many infections are not, as is commonly assumed, brought into the relationship by the man (4, 5). African regions suffering from conflict, genocide, and rape, such as Rwanda, Congo, and Angola, are much less affected by AIDS than peaceful, wealthier, and more literate countries such as Botswana or Swaziland, which have the world’s highest HIV prevalence (6).
Where multiple sexual partnerships, especially concurrent ones, are uncommon, and particularly where male circumcision (MC) is common, HIV infection has remained concentrated in high-risk populations (7). Niger, a Muslim country where sexual behavior is relatively restrained and MC is universal, has an adult HIV prevalence of 1.1%, despite being the lowest ranking country in the Human Development Index Botswana, the second wealthiest country in Sub-Saharan Africa has high levels of multiple concurrent partnerships among both sexes and lack of MC (8), with an HIV prevalence of 25% (1) (see SOM).
Several current prevention approaches have value, and the search for new, more effective interventions must continue. However, especially given the severe human resource constraints in Africa, we are arguing for a shift in prevention priorities.
Weaker Evidence for Effectiveness
For generalized epidemics, most emphasis has been placed on the three “established” pillars of HIV prevention: condom promotion and distribution, voluntary counseling and testing (VCT), and treatment of other sexually transmitted infections (STIs) (4). Recently, the USA’s global AIDS program has also promoted abstinence. However, although it can be difficult to assess exactly why HIV prevalence has fallen in some generalized epidemics, two other factors stand out as important: the epidemic’s natural progression, as the most susceptible populations become infected and die (9), and behavior change, particularly declines in multiple sexual partnerships (2, 4, 7, 9-11).
Condom use
Condom promotion is effective in epidemics spread mainly through sex work, as in Thailand (7, 10, 11), and also to some extent among other high-risk groups such as MSM. Although condom use has also likely contributed to HIV decline in some generalized epidemics, there is no evidence of a primary role (2, 4, 10, 11). This is probably because consistent condom use has not reached a sufficiently high level, even after many years of widespread and often aggressive promotion, to produce a measurable slowing of new infections in the generalized epidemics of Sub-Saharan Africa. When most transmission occurs within more regular and, typically, concurrent sexual partnerships, consistent condom use is exceedingly difficult to maintain (2, 4, 7, 10)
HIV testing
Unfortunately, reviews of many studies have shown no consistent reduction in risk for those who test HIV-negative, although risk reductions in some who test positive have been reported (4, 12, 13). Several HIV and STI incidence studies in Africa have found no population-level impact of VCT (12-14). Although a critical link to life-prolonging treatment, HIV testing is therefore unlikely to substantially alter the epidemic’s course [the potential for domestic violence against women who test positive must also be considered (15)].
Treatment of other STIs
Six randomized controlled trials (RCTs) to measure the impact of STI treatment on HIV transmission have been published. Although the first study, in Mwanza, Tanzania, found a nearly 40% reduction in HIV when STIs were treated through syndromic management, subsequent trials found no effect on HIV (16). Two recent RCTs to prevent HIV acquisition by treating genital herpes have been similarly discouraging (17). Although STI treatment remains critical for broader public health programs, the population-level evidence for impact on HIV transmission, especially in generalized epidemics, appears minimal.
Vaccines and microbicides
Work on vaccine development has been sadly disappointing. In 2007, large-scale efficacy trials had to be stopped prematurely owing to lack of impact or possibly even harm (17). Attempts to develop a female-controlled method of deterring HIV infection have been similarly discouraging; several microbicide candidates (and the cervical diaphragm) have failed (16). Microbicides would have considerably lower biological effectiveness than condoms, and even an effective microbicide might be unlikely to be used consistently enough, especially in longer-term partnerships, to slow a generalized epidemic.
Abstinence
Abstinence completely prevents sexual transmission, and young people should be encouraged to delay sexual debut (18). However, most HIV infections occur among people in their 20s or older, when most are sexually active, and thus, abstinence is unlikely to have a major epidemiological impact (4, 11).
Interventions such as blood screening and preventing maternal-to-child transmission (PMTCT) are clearly effective, but only address a relatively small proportion of total HIV transmission.
What Works
Male circumcision (MC)
Over 45 observational, biological, and other studies from the last 20 years have shown that MC significantly reduces the risk of heterosexual HIV infection (2, 7 19, 20). The population-level effect of widespread MC is observed in west Africa, where HIV has been present for many decades, yet prevalence remains relatively low (1, 7 19, 20). All three recent RCTs of MC in Africa were stopped early for ethical reasons when initial findings demonstrated at least 60% reduction in HIV risk (19, 20). The population-level impact, taking into account “herd immunity,” could be even greater if a large proportion of men become circumcised (19, 20). Unlike most other interventions, MC is a one-time procedure that confers lifelong protection. Modeling suggests that MC could avert up to 5.7 million new HIV infections and 3 million deaths over the next 20 years in Sub-Saharan Africa, many of these among women (21).
A dozen acceptability studies and on-the-ground experience in many high-HIV-prevalence African countries demonstrate that the majority of uncircumcised men and their female partners accept and want MC services (typically for reasons of hygiene and sexual pleasure) (22). In Swaziland, men almost rioted because circumcision services were not available (20). Studies suggest that up to 80% in high HIV-prevalence countries like Botswana and Swaziland would seek MC if it were safe and inexpensive (22).
Donor agencies have the opportunity to be proactive, but African governments and civil society must take the lead, as has begun to occur in several countries (19). MC must be combined with behavior change, especially promotion of partner reduction and consistent condom use (1, 2, 19). Over time MC, which has been called a “surgical vaccine,” would probably protect more women, albeit indirectly, than nearly any other achievable HIV prevention strategy (19-21).
Reducing multiple sexual partnerships
Another preventive measure that has had a powerful impact and that could have even greater effect, if it were more widely and assertively promoted, is partner reduction (2, 4, 7, 11, 18, 23-25). After the extensive “Zero Grazing” campaign initiated in Uganda in 1987, WHO surveys conducted in 1989 and 1995 found a >50% reduction in the number of people reporting multiple and casual partners (23-25). In Kenya, partner reduction and fidelity appear to have been the main behavioral change responsible for the recent HIV decline (2, 4, 7). Similar behavior change has been reported in DHS surveys in Zimbabwe, where HIV has also fallen (1, 2, 7, 26), along with Ethiopia (7, 11), Côte d’Ivoire, and urban Malawi (see SOM). In Swaziland, the number of people reporting two or more partners in the past month was halved after an aggressive 2006 campaign focusing on the danger of having a “secret lover” (7).
Yet, there are still few demonstrated replicable approaches to reducing multiple sexual partnerships on a large scale. Nonetheless, mass mobilization of the community, as occurred with gay men in the United States and among heterosexuals in Uganda, can effectively encourage behavior change (18, 23, 25). And the Ugandan experience suggests that both partner reduction and combating stigma can be successfully achieved (24, 25).
What Can be Done Now?
Currently, the largest donor investments are being made in interventions for which evidence of large-scale impact is increasingly weak, whereas much lower priority is given to interventions for which the evidence of potential impact is greatest (see figure, page XXX). About 1% of total requested funding is for MC, and probably only a fraction of "community mobilization and mass media" efforts would be focused on reducing multiple and concurrent sexual partnerships. This balance needs to be reassessed.
Fig. 1.
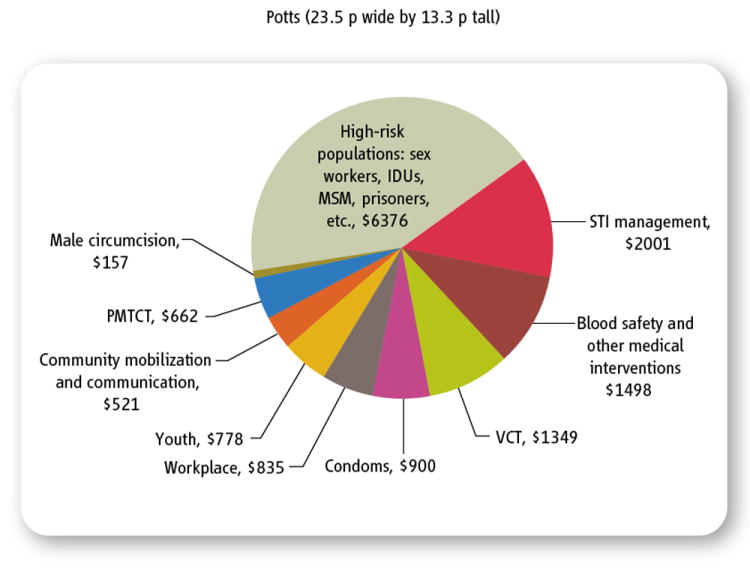
UNAIDS resource allocation estimates to achieve “universal access” to HIV prevention by 2010 (in millions of U.S. dollars). Although interventions for high-risk populations are crucial, resource allocation recommended by UNAIDS is too small for those approaches likely to have a major impact on generalized heterosexual epidemics. (And much of the funding for categories such as “high-risk populations” would actually go for interventions like condom promotion.)
Supplementary Material
Acknowledgments
This paper emerged from an HIV prevention experts’ meeting sponsored by the Bixby Center, University of California at Berkeley, and Harvard University in May 2007. We also thank A. Herling, H. Epstein, P. Kilmarx, H. Kinlaw, T. Mah, J. Chin, M. Hanley, and R. Bailey.
Footnotes
Supporting Online Material
References and Notes
- 1.UNAIDS. AIDS Epidemic Update (UNAIDS Publ UNAIDS/07.27E/JC1322E. UNAIDS; Geneva: 2007. the Joint United Nations Programme on HIV/AIDS. www.unaids.org/en/KnowledgeCentre/HIVData/EpiUpdate/EpiUpdArchive/2007/default.asp. [Google Scholar]
- 2.Southern African Development Community (SDAC) Expert Think Tank Meeting on HIV Prevention in High-Prevalence Countries in Southern Africa: Report; Maseru, Lesotho. 10 to 12 May 2006; Botswana: SADC; 2006. www.sadc.int/downloads/news/SADCPrevReport.pdf. [Google Scholar]
- 3.Mishra V, et al. AIDS. 2007;21(suppl. 7):S17. doi: 10.1097/01.aids.0000300532.51860.2a. [DOI] [PubMed] [Google Scholar]
- 4.Shelton JD. Lancet. 2007;370:1809. doi: 10.1016/S0140-6736(07)61755-3. [DOI] [PubMed] [Google Scholar]
- 5.Economist. 2007 Jun 28;:x. www.economist.com/science/displaystory.cfm?story_id=9401560.
- 6.Spiegel PB, et al. Lancet. 2007;369:2187. doi: 10.1016/S0140-6736(07)61015-0. [DOI] [PubMed] [Google Scholar]
- 7.Halperin DT, Epstein H. South African J HIV Med. 2007;26:19. www.harvardaidsprp.org/research/halperin&epstein-why-is-hiv-prevalence-so-severe.pdf. [Google Scholar]
- 8.Carter MW, et al. AIDS Behav. 2007;11:822. doi: 10.1007/s10461-006-9203-6. [DOI] [PubMed] [Google Scholar]
- 9.Shelton JD, Halperin DT, Wilson D. Lancet. 2006;367:1120. doi: 10.1016/S0140-6736(06)68436-5. [DOI] [PubMed] [Google Scholar]
- 10.Hearst N, Chen S. Stud Fam Plann. 2004;35:39. doi: 10.1111/j.1728-4465.2004.00004.x. [DOI] [PubMed] [Google Scholar]
- 11.Shelton JD, et al. BMJ. 2004;328:891. doi: 10.1136/bmj.328.7444.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cassell MM, Surdo A. Lancet Infect Dis. 2007;7:491. doi: 10.1016/S1473-3099(07)70114-7. [DOI] [PubMed] [Google Scholar]
- 13.Denison JA, et al. AIDS Behav. 2008;12:363. doi: 10.1007/s10461-007-9349-x. [DOI] [PubMed] [Google Scholar]
- 14.Corbett EL, et al. AIDS. 2007;21:483. doi: 10.1097/QAD.0b013e3280115402. [DOI] [PubMed] [Google Scholar]
- 15.Maman S, et al. AIDS Behav. 2003;7:373. doi: 10.1023/b:aibe.0000004729.89102.d4. [DOI] [PubMed] [Google Scholar]
- 16.Gray RH, Wawer M. Lancet. 2007;370:200. doi: 10.1016/S0140-6736(07)61058-7. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J. Science. 2008;319:888. doi: 10.1126/science.319.5865.888. [DOI] [PubMed] [Google Scholar]
- 18.Halperin DT, et al. Lancet. 2004;364:1913. doi: 10.1016/S0140-6736(04)17487-4. [DOI] [PubMed] [Google Scholar]
- 19.Weiss HA, et al. AIDS. 2008;22:567. doi: 10.1097/QAD.0b013e3282f3f406. [DOI] [PubMed] [Google Scholar]
- 20.Klausner JD, et al. Future HIV Ther. 2008;2:1. doi: 10.2217/17469600.2.1.1. www.futuremedicine.com/doi/full/10.2217/17469600.2.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams BG, et al. PLoS Med. 2006;3:e262. doi: 10.1371/journal.pmed.0030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Westercamp N, Bailey RC. AIDS Behav. 2007;11:341. doi: 10.1007/s10461-006-9169-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stoneburner RL, Low-Beer D. Science. 2004;304:714. doi: 10.1126/science.1093166. [DOI] [PubMed] [Google Scholar]
- 24.Green EC, Halperin DT, Nantulya V, Hogle JA. AIDS Behav. 2006;10:335. doi: 10.1007/s10461-006-9073-y. www.springerlink.com/content/h00r4n6521805w27/fulltext.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Epstein H. The Invisible Cure: Africa, the West and the Fight Against AIDS. Farrar Straus and Giroux; New York: 2007. [Google Scholar]
- 26.Gregson S, et al. Science. 2006;311:664. doi: 10.1126/science.1121054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


