Abstract
Hospital physicians care for most seriously ill patients in the United States. We employed dimensional analysis to describe communication about death and dying in audio-recorded admission encounters between seriously ill patients and hospitalists. Acknowledging or not acknowledging the possibility of dying emerged as a key process. Acknowledgment was rare, and depended on synergistic communication behaviors between patient and physician. Facilitators included patients cuing for information and disclosing emotional distress, and physicians exploring the patient’s understanding of his or her illness and emotional distress. When hospitalists focused on acute issues, stated that they were awaiting test results, and deferred to other physicians, discussion moved away from acknowledgment. Meaningful discussion of end-of-life issues, including goals and values, fears about death and dying, prognosis, and options for palliative care followed open acknowledgment. This acknowledgment process can serve as a guide for providers to sensitively and honestly discuss essential end-of-life issues.
Keywords: communication, medical, death and dying, dimensional analysis, end-of-life issues, health care, acute / critical, illness and disease, life-threatening / terminal, medicine
Decades of research and policy highlight the importance of patient–provider communication about serious illness to patients’ end-of-life experiences (Connors et al., 1995; Field & Cassel, 1997; Glaser & Strauss, 1965). Seriously ill patients desire honest, sensitive communication about end-of-life issues (Clayton, Butow, Arnold, & Tattersall, 2005; Wenrich et al., 2001). However, providers often do not convey that an illness is incurable (Tattersall, Gattellari, Voigt, & Butow, 2002), and do not address patients’ concerns (Butow, Brown, Cogar, Tattersall, & Dunn, 2002). Discussions of life-sustaining therapies seldom include realistic information about risks, benefits, and outcomes, or incorporate patients’ overall prognosis and goals (Anderson, Chase, Pantilat, Tulsky, & Auerbach, 2011; Kaldjian et al., 2009). Experts recommend techniques to honestly and sensitively discuss death and dying (von Gunten, Ferris, & Emanuel, 2000), yet it is not clear what such exchanges look like in practice.
Globally, many patients die in hospitals; even more are hospitalized in the months before death (Cohen et al., 2008; Dartmouth Atlas of Health Care, 2011). Patients often present to the hospital without having discussed their prognosis or preferences for care near the end of life (Dow et al., 2010). Hospital providers are often unaware of patients’ preferences, and patients receive unwanted interventions (Connors, et al., 1995; Kaldjian et al., 2009). Thus, experts recommend using hospitalization as an opportunity to discuss goals for the end of life (Kass-Bartelmes & Hughes, 2003).
In the 1990s, the hospitalist model emerged as a key factor shaping the physician–patient relationship in hospitals. At that time, managed care’s emphasis on efficiency exerted dual pressures: for hospitals to minimize resource use, and for outpatient physicians to remain in the clinic and not round on their hospitalized patients (Wachter & Goldman, 1996). In response, hospitals employed generalist physicians, usually trained in internal medicine, to care for inpatients and hand care back to outpatient providers at discharge. Hospitalists now number 30,000 in the United States, and self-define as delivering comprehensive care to hospitalized patients while improving care at the system level (Society of Hospital Medicine, 2010). Multiple specialties and countries now employ the model (Hock Lee, Yang, Soong Yang, Chi Ong, & Seong Ng, 2011; Maa, Carter, Gosnell, Wachter, & Harris, 2007; Mussman & Conway, 2011). Positive outcomes include increased patient satisfaction, reduced lengths of stay, reduced costs, and improved medical education (Fulton, Drevs, Ayala, & Malott, 2011; Wachter & Goldman, 2002).
Hospitalists care for an increasing number of patients with serious illness (Kuo, Sharma, Freeman, & Goodwin, 2009) and view end-of-life care as a core responsibility (Plauth, Pantilat, Wachter, & Fenton, 2001). However, few researchers have examined hospitalists’ provision of end-of-life care (Auerbach & Pantilat, 2004); none have described how hospitalists communicate with patients about death and dying. We aimed to describe initial communications about serious illness between hospitalists and patients, and to identify patterns that led to sensitive and honest discussions of death and dying, even at a first meeting.
Methods
Design
We used a grounded theory approach to analyze communication about death and dying in audio-recorded admission encounters between hospitalist physicians and seriously ill patients. We chose admission encounters, during which the hospitalist first assesses the patient and the two discuss the treatment plan, because they set patterns for future communication and are often longer and more substantive than daily encounters.
Study Setting
We collected data between August 2008 and March 2009 in two hospitals comprising the medical service at an academic medical center in the western United States. The service annually admits approximately 5,500 patients, including those with cancer and other serious illnesses, for tertiary referral and primary hospital care. High-acuity patients receive care in multiple units of a 400-bed hospital on the main medical center campus. A 26-bed medical-surgical unit at a nearby 89-bed satellite campus cares for those with lower acuity. Hospitalists direct the care of patients admitted to the service, seeing them on admission and then at least once daily on subsequent hospital days. Individual hospitalists rotate on and off service at varying intervals, from as little as one shift to as long as a month. Medical students and residents rotate on the service at the larger, but not the smaller campus.
Participants
We recruited all hospitalists attending on the service, and asked those participating to identify patients being admitted to their care—either to the hospital or in transfer from another service—whose death or intensive care unit admission in the next year would not surprise them (Pollak et al., 2007). We excluded patients who could not communicate verbally in English or give informed consent. A research assistant approached patients in the emergency room or their hospital rooms for screening and enrollment. To avoid interfering with patient care, physicians could decline participation on certain days or with certain patients. The University of California, San Francisco, Institutional Review Board approved the study. All participants gave written informed consent. So as not to inadvertently disclose their prognosis, we blinded patient participants to the physicians’ prognostic assessments and the study focus on communication about death and dying.
Data Collection
Audio recordings of admission encounters that occurred in patients’ hospital rooms comprised the primary study data. Encounter content was completely open ended and based on the physicians’ standard practices. Because our goal was to describe usual communication, we designed our protocol to minimize participants’ awareness of being observed. Before the physician entered the room, a research assistant placed an audio-recorder at the bedside and began the recording. The assistant then left the room, waiting outside until the physician completed the encounter and exited. The assistant then reentered to collect the audio recorder. Recordings were professionally transcribed for analysis. Brief patient surveys assessed patient demographics and self-evaluated health (Prigerson, 1992). Brief physician surveys assessed physician demographics as well as the patients’ admission diagnoses and life-limiting diagnoses.
Analytic Procedures
We used dimensional analysis, a method for generating grounded theory, to describe and explain communication about serious illness between patients and physicians in the admission encounters (Bowers & Schatzman, 2009; Kools, McCarthy, Durham, & Robrecht, 1996; Schatzman, 1991). In the data-expansion phase of this method, called dimensionalizing, the analyst identifies dimensions of data. Then, in the data-limitation phase, called differentiation, salient dimensions are selected and configured in relation to one another within an explanatory matrix, a predetermined structure based on symbolic interactionism. The analyst configures the matrix from a perspective, the dimension found to have the most explanatory power in the overall description of the data. Other dimensions are then designated as context, which encompass the setting or environment of the data; conditions, which shape actions; processes, which arise from the conditions; and consequences, the outcomes of the actions. Iterative configuration of dimensions within the prespecified categories ensures the best description of the data and explanation of relationships between elements.
In dimensionalizing, we sought to identify all aspects of physician–patient communication in the encounters without determining their importance, function, or relation to one another (Schatzman, 1991). The first author coded the entire transcript of a subset of encounters; peers in an analysis group and the second author reviewed these coded transcripts. We identified a number of dimensions through this process, including rapport building, pain and symptom management, treatment of the acute medical condition, and prognosis. After reviewing eight transcripts, acknowledgment of the possibility that the patient could die from his or her illness emerged as a key dimension, and we noted redundancy in identified dimensions, suggesting a level of saturation.
We began differentiation by selecting from this robust preliminary set of dimensions those that related to communication about the possibility of dying, and configured these in a preliminary explanatory matrix. The first author coded the remaining transcripts to identify additional dimensions related to communication about the possibility of dying, and to verify and refine the configuration of the matrix to best fit all of the encounters. Throughout this process, the first author wrote analytic memos describing context, conditions, processes, and consequences, which peers and the coauthors reviewed. The first author also maintained reflexive notes and memos regarding the analysis.
We configured the matrix from the perspective of “dancing around death,” a central process found in the analysis, because of this dimension’s salience and ability to integrate other data into an explanatory story (Kools et al., 1996). Theoretical saturation was reached when we identified no new conditions, processes, or consequences, and the relationships established between the elements of the matrix held. To assess our ability to achieve a reasonable level of data saturation within the analyzed sample, we counted the number of encounters that achieved varying degrees of acknowledgment. We selected data exemplars to illustrate the dimensions and their relationships within the final matrix.
We took several steps to ensure theoretical and methodological rigor and credibility of the findings (Charmaz, 2006). The coauthors, as well as a group of qualitative researchers, regularly reviewed coding, conceptual memos, explanatory matrix configuration, and final theoretical integration to ensure rigor and grounding of findings in data. These reviews included direct exploration of reflexivity to minimize bias. A sample of hospitalist participants provided member checking in a focus group at which they described their experiences and practices of discussing serious illness with patients. This group verified the centrality of the process of acknowledgment and the conditions leading to and consequences of it. Patient participants did not provide member checks, because all had been discharged and many were quite ill or had died before we completed the analysis.
Results
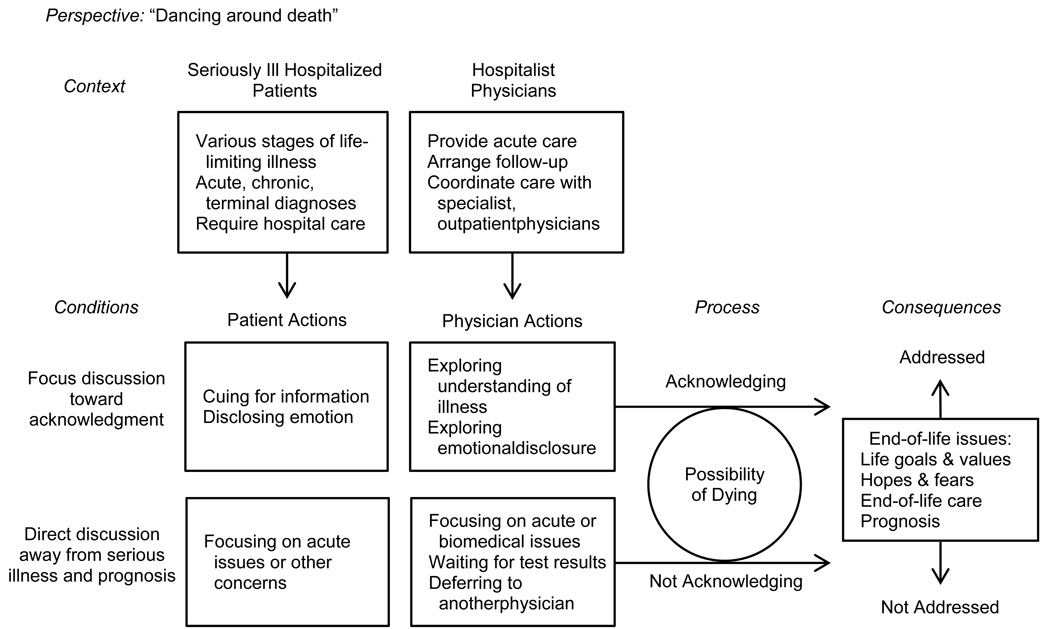
We analyzed audio recordings of 39 patients’ (consent rate 66%) admission encounters with 23 physicians (consent rate 91%). Communication in the encounters about the possibility of dying varied along a continuum, with a minority reaching open acknowledgment that the patient could die of his or her illness. Following open acknowledgment, the tenor of the encounters changed from building to released tension, and the physician and patient explored end-of-life topics with a depth and meaning that we did not observe in the absence of open acknowledgment. In Figure 1 we have diagrammed our explanatory matrix, configured from the perspective of “dancing around death.” We chose the dancing metaphor to describe our perspective because it captured many salient aspects of the interaction: the intricate dyadic interplay; the presence of the possibility of dying but reluctance to acknowledge it; the often interchanging roles of leading and following; the multiple, delicate steps which gradually built toward open acknowledgment when it occurred; and finally resolution, in which the meaning of the acknowledgment was explored. Below we describe each matrix component.
Figure 1. Explanatory matrix describing physician–patient communication about serious illness.
Context: A Seriously Ill Patient’s Hospital Admission
The structure of the admission encounter, the characteristics of the patients’ illnesses, and the physicians’ roles as hospitalists formed the boundaries of our inquiry and the environment in which the dimensions in our explanatory matrix occurred (see Figure 1). Varying encounter lengths (median 21, range 4 to 68 minutes) signified differences in illness medical complexity, and the degree to which patients had been previously evaluated. Activities common to encounters were history taking, eliciting and answering patient questions, and discussing treatment plans. Encounters typically began with the physician asking what had brought the patient to the hospital, and concluded with the plan for the day or hospital stay.
Seriously ill hospitalized patients
Participating patients represented the hospital demographics (see Table 1), with heterogeneous life-limiting and admission diagnoses, acuity, and self-rated health. We observed three broad types of life-limiting diagnoses: (a) terminal, progressive illnesses, such as metastatic cancer, from which the patient would die despite treatment; (b) chronic illness, such as diabetes, from which the patient might eventually die, but which could be controlled long term; and (c) acute illness, such as pulmonary embolism. Some patients’ illnesses fell along the continuum between chronic and terminal, such as end-stage renal disease or HIV—manageable for some time, but ultimately likely to be terminal. Most patients were admitted through the emergency room because of an acute event or symptom, often related to the life-limiting diagnosis; others came under the care of a physician in transfer from another service within the medical center; a few were admitted for scheduled inpatient chemotherapy.
Table 1.
Characteristics of Patient and Physician Study Participants
| Characteristics | Patientsa n (%) |
Physiciansb n (%) |
|---|---|---|
| Age in years [mean (SD)] | 59 (16) | 34 (4) |
| Men | 20 (51%) | 9 (39%) |
| Ethnicity, Hispanic | 1 (3%) | 0 |
| Race | ||
| White | 29 (74%) | 14 (61%) |
| Asian | 4 (10%) | 7 (30%) |
| Black/African American | 4 (10%) | 0 |
| Other | 2 (5%) | 2 (9%) |
| Life-limiting diagnosis | ||
| Cancer | 21 (54%) | |
| Chronic illness (e.g., diabetes, heart disease) | 5 (13%) | |
| Posttransplant | 4 (10%) | |
| End-stage renal disease | ||
| End-stage liver disease | 3 (8%) | |
| HIV | 2 (5%) | |
| Other | 2 (5%) | |
| Patient health, self-evaluated | ||
| Relatively healthy | 8 (21%) | |
| Seriously but not terminally | 22 (56%) | |
| Ill | 9 (23%) | |
| Seriously and terminally ill |
n = 39
n = 23
Acuity of illness varied: some patients might be expected to die during the studied hospitalization, whereas others might live for weeks, months, or longer. Though we screened patients who were admitted to intensive care units, all were excluded because they could not provide informed consent. By survey before the encounter, most patients evaluated their health as “seriously but not terminally ill” (see Table 1). The type of life-limiting illness, acuity, relationship to admission diagnosis, and patient evaluation of health influenced whether and how acknowledgment occurred.
Hospitalist physicians
The physicians’ demographics typified those of the practice from which we recruited. In the encounters, they described their role as providing acute hospital care and arranging appropriate follow-up. Physicians told their patients that they would be under their care for a limited time—for the duration of the hospitalization, or sometimes only for one shift. When explicating their role in coordinating with primary care and subspecialty physicians, such as oncologists, hospitalists explained that these other providers often directed the treatment of life-limiting diagnoses, as illustrated in the following excerpt:
I’m a hospitalist. I’m the internal medicine doctor. I’m not an oncologist or a surgeon, and certainly not versed in neuroendocrine tumors beyond what I learned in medical school. My job is to help with the hypercalcemia, and hopefully come up with a sustainable strategy for you, as you leave here.... And also to coordinate your care with these other subspecialties who will be advising us.
The way the hospitalists presented the limited nature of their relationships with the patients, and their roles as generalists, at times directed discussion away from acknowledgment.
Conditions: Patient and Physician Actions
As shown in Figure 1, physicians’ and patients’ combined communication behaviors were the conditions that focused the discussion toward or away from acknowledgment; within the dancing metaphor, these behaviors constituted the opening steps. In encounters in which acknowledgment occurred, the physician sometimes started the dance, but thereafter followed the patient’s lead by responding to and exploring the patient’s statements. When acknowledgment did not occur, we observed either an absence of physician and patient facilitative behaviors or a presence of behaviors that diverted discussion from the patient’s serious illness and prognosis.
Conditions facilitating acknowledgment of the possibility of dying
Both cognitive and emotional aspects of conversation around serious illness synergistically built the conditions for acknowledgment to occur. Cognitive behaviors included physician exploration of patient understanding of illness and patient cuing for information. Physicians explored patients’ understanding using open-ended questions such as, “What do you understand about the status of your illness?” This type of question began the conversation, encouraging the patient to disclose his or her understanding. These questions also encouraged patients to disclose gaps in their understanding of their illness, in the form of cues for information. For encounters to reach acknowledgment, physicians had to engage in the dance by responding to patient’s cues.
In response to a hospitalist’s questions about the overall status of his illness and whether he would want cardio-pulmonary resuscitation, a 60-year-old man with metastatic cancer admitted to the hospital with failure to thrive said,
Somewhere there’s a judgment call before—I mean—in other words, what is the state of—if you’re gonna do something aggressive—I’m not that old. Right? I’m not that unhealthy. I mean, well, except I—and [the oncology physicians] really haven’t talked about how—they haven’t provided much information on prognosis.
The physician continued to explore the patient’s understanding of his illness, asking what would help him to understand it better. This led the patient to acknowledge that he was not going to be “magically cured” of his cancer, thence to a plan for the oncologist to discuss a specific prognosis with the patient.
Emotional behaviors facilitating acknowledgment included patient disclosures of emotional distress and physician empathy and exploration of distress. For the patient, these disclosures often centered on illness or treatment challenges. As with information cues, whether acknowledgment resulted from these disclosures depended on how physicians responded. Patients’ initial disclosures did not directly reference death, but in some encounters, the possibility of dying emerged when the physician explored the disclosure. When asked to describe his understanding of his illness, a 59-year-old man with a history of rectal cancer related his concern that his cancer might have recurred. He expressed distress about the toll his past therapy had exacted and his inability to tolerate the treatment again: “More radiation—I can’t do it again. It almost killed me, it was so painful.” The physician responded with empathy and explored the patient’s distress: “What was it, in particular, that bothered you with your last round of therapy?” As the conversation continued, the physician agreed that the cancer had likely recurred. After discussion of work-up and treatment options, the patient disclosed that he believed he was dying.
Conditions directing the conversation away from serious illness and prognosis
In some encounters, the patient focused on acute issues or other concerns, such as the immediate management of his or her condition or social concerns. A physician asked a 62-year-old woman with thyroid cancer, admitted for urgent treatment of brain metastases, “What do you understand about where things stand now and where things are heading?” The patient described her discussions with a neurologist about gamma-knife therapy, then introduced a concern about her husband’s death and estate. When the physician responded with empathy, the patient described how she reassured herself: “God's watching over you. This is all [part] of a big plan. You’re all right. You're not going to die today.” When the physician asked what she had planned, the patient mentioned an advance directive, but segued back to her concerns about her husband’s estate. Despite the physician’s facilitative actions, the patient repeatedly directed conversation away from discussion of the overall status of her illness.
In other encounters, despite patient-facilitative actions, the physician directed discussion away from serious illness and prognosis by focusing on biomedical or acute issues. A 66-year-old man with metastatic prostate cancer admitted with pneumonia expressed anxiety about feeling weak and not being able to care for his family: “So, the whole thing is just real scary and I’m hoping that, in partnership, we’re going to be able to turn it around.” The physician’s explanation that the patient might be discharged the next day prompted additional anxiety:
I have to say the thought of going home is scary.... Because I’m feeling so vulnerable and that’s new for me. You know, I’ve never been a vulnerable guy. I just want to have some—I need to have some strength back. I need to have some capability to make my own way. By that, I mean walk and you know, carry a couple [of] small things.
The physician expressed understanding: “Sure. So you have to be able to take care of yourself, basically.” However, instead of exploring the patient’s concern about weakness and vulnerability, the physician then focused on discharge planning:
If it seems that what you need most is some time to get back on your feet, get stronger, then there’s places to go between here and home, to get tuned up, get rehab [rehabilitation], like a skilled nursing facility or an acute rehab facility.
Focusing on these clinically appropriate logistics directed the discussion away from the patient’s emotional experience. Neither the patient nor the physician mentioned the patient’s prostate cancer.
Physicians also directed discussion away from acknowledgment by deferring patients’ information cues or emotional disclosures to another provider or waiting for test results. A physician explained to a 71-year-old man with liver cancer, fever, and back pain that his symptoms could be caused by bone infection or cancer metastasis. The patient repeatedly cued for information about his serious illness: Which type of outpatient specialist should he follow-up with? What treatment would be required, surgery or radiation therapy? Which did the physician recommend? The physician deferred these questions, emphasizing that, as the hospitalist, he would not determine which therapy the patient received: “Well, I think we need to definitely talk to the surgeons and radiation oncologist in order to answer that question.” Moreover, a decision could not be made until the diagnosis was confirmed: “Let's first figure out what this is and then we can determine which route to go. Because until we figure out what it is, nobody’s going to do any surgery or radiation.” Absent exploration of the patient’s concerns, these clinically accurate statements shifted discussion of all issues related to the patient’s serious illness to another provider at another time.
In the preceding example, deferral to other physicians was explicit. Physicians also implicitly deferred discussion of the serious illness. A 53-year-old man with HIV was admitted with nausea, vertigo, and hyperparathyroidism. When the patient mentioned his HIV, the physician verified that the patient had a primary care physician who followed the HIV. The patient’s HIV was not discussed again.
Process: Continuum of Acknowledging the Possibility of Dying
The patient and physician actions created an acknowledgment continuum, ranging from not discussing the serious illness to open acknowledgment. As shown in Figure 1, the way the patient and physician interacted around the possibility of dying influenced the degree to which they addressed end-of-life issues.
Acknowledging the possibility of dying
In acknowledging, both the physician and patient openly stated their understanding that the patient could die from his or her illness. Although most patients rated their health as seriously ill, acknowledgment occurred in only six of the encounters. In all cases of acknowledgment, the patient disclosed his or her understanding of this possibility first and the physician confirmed it. In no encounters did the physician disclose the possibility of dying to an unsuspecting patient. Patients’ self-evaluated health, assessed by survey, substantiated this finding: we only observed acknowledgment in patients who described their health as “seriously but not terminally ill” or “seriously and terminally ill”; no patient who described his or her health as “relatively healthy” acknowledged the possibility of dying.
In some cases, patients described knowing that they were dying before the interaction with the hospitalist. In others, they disclosed their suspicion and received confirmation from the hospitalist. For example, the 59-year-old man with rectal cancer volunteered that he felt he was dying after the physician confirmed that his cancer had likely recurred:
If your suspicion is correct and your intuition and your experience tells you that that’s what it is, then I don’t see the point in taking a biopsy of this and, you know, I can live with that.... I’ve been dealing with it for the last couple months. I knew that it probably wasn’t good—the end. And, you know, if I’m emotional talking about it, I don’t get emotional when I think about it. It’s just, “Okay, put your things in order.”
The way acknowledgment occurred varied by the type of life-limiting diagnosis. Patients with terminal illness acknowledged death indirectly. Instead of voicing the words death or dying, they used euphemisms such as “the end.” Patients with acute or chronic life-limiting diagnoses acknowledged death more directly. A 58-year-old woman admitted with a pulmonary embolism said of her condition, “They say they thought I was dying.”
Not acknowledging the possibility of dying
In the encounters in which open acknowledgment did not occur, we observed a range in how the patient and physician discussed the serious illness. Some physicians (n = 12) did not mention the patient’s life-limiting illness at all, as in the case of the 66-year-old man admitted with pneumonia, whose metastatic prostate cancer was not discussed; others (n = 11) discussed the life-limiting illness, but only in terms of its immediate management. For example, discussions with patients admitted for inpatient chemotherapy focused on the treatment logistics, not the larger picture of their illness.
Still other encounters (n = 10) addressed the status of the life-limiting illness but did not connect this status to whether the patient could die from it, as in the case of a 45-year-old man with a neuroendocrine tumor and recurrent hypercalcemia. When his physician elicited his “understanding of (a) prognosis and (b) treatment options for your cancer,” the patient described medical and surgical treatment options, and his understanding that the cancer could not be completely removed:
I know they can’t get the full tumor out right now, but at least ablate or freeze what you can and that’s always been, you know, a positive outcome, as far as stopping the symptoms, which with me is excess calcium.
However, because neither the physician nor the patient pursued the implications of this disease status for the patient’s survival, acknowledgment was not reached.
Consequences: Addressing End-of-Life Issues
As indicated by the arrows in Figure 1, the degree to which end-of-life issues were meaningfully addressed in the encounter varied by the degree to which acknowledgment occurred. The consequences of acknowledgment also varied by type of life-limiting diagnosis. For patients with acute or chronic illness, discussion focused narrowly on medical interventions. After acknowledgment, the physician and the 58-year-old woman admitted with a pulmonary embolism talked about how treatment with anticoagulation could prevent her death. A 69-year-old woman with end-stage renal disease talked about how she could have died during an episode of volume overload. She and the hospitalist reviewed how hemodialysis averted her death, but neither mentioned her poor overall prognosis.
For patients with terminal illness, open acknowledgment resulted in the physician and patient talking explicitly about end-of-life issues. These included the patient’s goals and values for the time remaining. A 72-year-old man with metastatic bladder cancer described that he most valued being outdoors hunting and fishing. His goals for his remaining time were to leave the hospital, get home, and be as active as possible. Acknowledgment also allowed patients to voice their hopes and fears about death and dying. The 59-year-old man with rectal cancer articulated the importance of maintaining peace of mind, and fear of being in pain. Clarification of goals, values, hopes, and fears allowed physicians to present options for care in terms of patients’ specific needs. The physician responded to the hopes and fears of the above patient with rectal cancer by describing palliative care: “We have a lot of things that we can do. There’s a whole specialty [that] we call palliative care.... And what we do is focus on all those things that are important for you.”
Acknowledgment also led patients to request a specific prognosis for the time they might have left. Patients noted that these estimates were important for life planning and deciding about medical treatments. The 59-year-old man with rectal cancer questioned the benefit of cancer treatment, wondering how much time it would gain him. The 60-year-old man with metastatic cancer and failure to thrive felt it was critical to understand his prognosis so that he could make informed decisions about his preferences for life-sustaining therapies, and not die like a “vegetable” on a ventilator. Hospitalists deferred these requests for specific time estimates, citing inability to predict a how long a patient might live. When patients persisted, hospitalists facilitated discussions between patients and their specialists. One physician explained:
It’s difficult for me to have a conversation about it with you, because I’m not an oncologist. I fully agree with your need for more information. I’m going to see if [oncologist] can come and have the conversation with you.
Discussion
In our dimensional analysis of 39 seriously ill patients’ admission encounters with 23 hospitalist physicians, acknowledging the possibility of dying emerged as a key process in communication about serious illness. Although all physicians and most patients rated the respective patient’s health as seriously ill, they infrequently acknowledged that the patient could die from his or her illness. Furthermore, discussions of end-of-life issues—goals, values, hopes, fears, options for end-of-life care, and prognosis—required open acknowledgment of this possibility in the encounter. These findings support the importance of communication about serious illness in hospitals. Many patients do not have primary care and subspecialty physicians, and even those with excellent outpatient care present with unmet needs. Some prefer to discuss end-of-life issues with inpatient physicians (Dow et al., 2010). Hospitalization for progression of life-limiting illness provides an opportunity to readdress goals of care (Kass-Bartelmes & Hughes, 2003; Pardon et al., 2012; Wagner, Riopelle, Steckart, Lorenz, & Rosenfeld, 2010).
Our results indicate that Glaser and Strauss’s (1965) awareness contexts of dying persist, despite changes to the health care system and the decades since their seminal work. The process we describe as acknowledgment mirrors their concept of open awareness, in which the provider and patient both realize that the patient could die and choose to acknowledge the possibility in their interaction. Encounters in which the patient and physician knew that the patient could die (based on their survey responses), but did not acknowledge it in the encounter, illustrate Glaser and Strauss’s concept of mutual pretense. Finally, encounters involving patients who reported lack of awareness of life-limiting illness in their survey responses correspond to closed awareness. A few encounters captured transitions from suspicion to open awareness as patients articulated their worry about dying and received confirmation from the physicians.
Our findings support and augment other work emphasizing the importance of prognostic communication to substantive discussions of end of life. Surgical intensive care unit decisions to withdraw life-sustaining therapies required consensus on the patient’s status as terminal (Aldridge & Barton, 2007). Cancer patients who discuss end-of-life issues with their physicians and more accurately understand their respective prognosiss receive life-sustaining therapies less frequently and have better quality of life near the end of life (Weeks et al., 1998; Wright et al., 2008). In advance care planning discussions, frail elders must accept dying as a likely outcome to discuss end-of-life preferences (Piers et al., 2011). We found that discussing end-of-life issues did not require specific time prognoses. Furthermore, patients did not have to accept with certainty that they would die from their illness to meaningfully discuss end-of-life issues. This provides empiric support for the communication approach, “hope for the best, prepare for the worst,” in which clinicians encourage patients to plan for the possibility of dying while maintaining hope for improvement (Back, Arnold, & Quill, 2003).
Our results provide concrete examples of how physicians can communicate sensitively about death and dying, and can be used as a model for provider training. Even in a first meeting, specific behaviors—exploring patients’ understanding of disease status and emotional disclosures—permitted hospitalists to open and facilitate, but not force, a discussion of end of life. Open-ended questions such as, “What is your understanding of your illness?” allowed hospitalists to safely broach this sensitive topic while individualizing discussions to accommodate varying preferences for prognostic information (Ahalt et al., 2011). Following patients’ informational and emotional cues created tailored, patient-centered discussions (Broom & Adams, 2010). The young age of hospitalists in our study, typical of this new field, suggests limited experience as a cause of infrequent acknowledgment. Alternatively, young age might facilitate acknowledgment, because younger physicians more frequently respond empathically to patient emotional expressions (Pollak et al., 2007).
Our study had several limitations. First, our dataset was limited to the patients’ admission conversations with their attending hospitalists and did not include discussions at other times or with other providers. We did not know what the patients understood from previous discussions, aside from what they revealed in the encounters. Second, all cases of acknowledgment depended on the patient’s knowledge or suspicion that he or she could die from the serious illness. Discussions with patients who do not suspect the possibility would follow a different pattern. Third, family members, who play a key role in end-of-life communication, were rarely present during these largely workday encounters. Finally, we studied interactions at hospitals in a single, U.S. academic center, limiting generalizability.
In summary, our findings highlight the importance of communication about serious illness in the hospital, and demonstrate the central role that hospitalists play in addressing unmet communication needs of seriously ill patients. Acknowledging the possibility of dying led to outcomes that made real differences in patients’ end-of-life experiences. Emotional support decreases distress (Fogarty, Curbow, Wingard, McDonnell, & Somerfield, 1999; Heaven & Maguire, 1998). Discussing prognosis, goals, and values improves quality of life at the end of life by matching treatments to patients’ goals (Weeks et al., 1998; Wright et al., 2008). Referral to palliative care improves the quality of life for patients and families, and even lengthens life (Higginson et al., 2002; Temel et al., 2010). Future research should investigate how acknowledging the possibility of death influences care during hospitalization, on discharge, and after hospitalization.
Acknowledgments
We thank the patients and physicians who generously donated their time to participate, and Amy J. Markowitz for editing the manuscript.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Anderson was funded by the National Palliative Care Research Center. Drs. Anderson and Lyndon were funded by the University of California, San Francisco, Clinical and Translational Science Institute Career Development Program, supported by National Institutes of Health grant number 5 KL2 RR024130-04.
Biographies
Wendy G. Anderson, MD, MS, is an assistant professor in the Department of Medicine, Division of Hospital Medicine and Palliative Care Program, at the University of California, San Francisco, School of Medicine in San Francisco, California, USA.
Susan Kools, RN, PhD, is a professor in the Department of Family Health Care Nursing at the University of California, San Francisco, School of Nursing in San Francisco, California, USA.
Audrey Lyndon, RNC, PhD, CNS, is an assistant professor in the Department of Family Health Care Nursing at the University of California, San Francisco, School of Nursing in San Francisco, California, USA.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ahalt C, Walter LC, Yourman L, Eng C, Perez-Stable EJ, Smith AK. "Knowing is better": Preferences of diverse older adults for discussing prognosis. Journal of General Internal Medicine. 2011 doi: 10.1007/s11606-011-1933-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldridge M, Barton E. Establishing terminal status in end-of-life discussions. Qualitative Health Research. 2007;17:908–918. doi: 10.1177/1049732307299995. [DOI] [PubMed] [Google Scholar]
- Anderson WG, Chase R, Pantilat SZ, Tulsky JA, Auerbach AD. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. Journal of General Internal Medicine. 2011;26(4):359–366. doi: 10.1007/s11606-010-1568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach AD, Pantilat SZ. End-of-life care in a voluntary hospitalist model: Effects on communication, processes of care, and patient symptoms. American Journal of Medicine. 2004;116(10):669–675. [Google Scholar]
- Back AL, Arnold RM, Quill TE. Hope for the best, and prepare for the worst. Annals of Internal Medicine. 2003;138(5):439–443. doi: 10.7326/0003-4819-138-5-200303040-00028. Retrieved from http://www.annals.org/content/138/5/439.full. [DOI] [PubMed] [Google Scholar]
- Bowers B, Schatzman L. Dimensional analysis. In: Morse J, Stern PN, Corbin J, Bowers B, Charmaz K, Clarke A, editors. Developing grounded theory: The second generation. Walnut Creek, CA: Left Coast Press; 2009. pp. 86–126. [Google Scholar]
- Broom A, Adams J. The reconfiguration of expertise in oncology: The practice of prediction and articulation of indeterminacy in medical consultations. Qualitative Health Research. 2010;20:1433–1445. doi: 10.1177/1049732310373042. [DOI] [PubMed] [Google Scholar]
- Butow PN, Brown RF, Cogar S, Tattersall MH, Dunn SM. Oncologists' reactions to cancer patients' verbal cues. Psycho-Oncology. 2002;11(1):47–58. doi: 10.1002/pon.556. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. London: Sage; 2006. [Google Scholar]
- Clayton JM, Butow PN, Arnold RM, Tattersall MH. Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers. Cancer. 2005;103(9):1965–1975. doi: 10.1002/cncr.21011. [DOI] [PubMed] [Google Scholar]
- Cohen J, Bilsen J, Addington-Hall J, Lofmark R, Miccinesi G, Kaasa S, Deliens L. Population-based study of dying in hospital in six European countries. Palliative Medicine. 2008;22(6):702–710. doi: 10.1177/0269216308092285. [DOI] [PubMed] [Google Scholar]
- Connors A, Dawson N, Desbiens N, Fulkerson W, Goldman L, Knaus W, Ransohoff D. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) Journal of the American Medical Association. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- Dartmouth Atlas of Health Care. Percent of Medicare decedents hospitalized at least once during the last six months of life. 2011 Retrieved from http://www.dartmouthatlas.org/data/table.aspx?ind=133.
- Dow LA, Matsuyama RK, Ramakrishnan V, Kuhn L, Lamont EB, Lyckholm L, Smith TJ. Paradoxes in advance care planning: The complex relationship of oncology patients, their physicians, and advance medical directives. Journal of Clinical Oncology. 2010;28(2):299–304. doi: 10.1200/JCO.2009.24.6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field MJ, Cassel CKE. Approaching death: Improving care at the end of life. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? Journal of Clinical Oncology. 1999;17(1):371–379. doi: 10.1200/JCO.1999.17.1.371. Retrieved from http://jco.ascopubs.org/content/17/1/371.long. [DOI] [PubMed] [Google Scholar]
- Fulton BR, Drevs KE, Ayala LJ, Malott DL., Jr Patient satisfaction with hospitalists: Facility-level analyses. American Journal of Medical Quality: The Official Journal of the American College of Medical Quality. 2011;26(2):95–102. doi: 10.1177/1062860610381274. [DOI] [PubMed] [Google Scholar]
- Glaser B, Strauss A. Awareness of dying. Chicago: Aldine; 1965. [Google Scholar]
- Heaven CM, Maguire P. The relationship between patients' concerns and psychological distress in a hospice setting. Psycho-Oncology. 1998;7(6):502–507. doi: 10.1002/(SICI)1099-1611(199811/12)7:6<502::AID-PON336>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- Higginson IJ, Finlay I, Goodwin DM, Cook AM, Hood K, Edwards AG, Norman CE. Do hospital-based palliative teams improve care for patients or families at the end of life? Journal of Pain and Symptom Management. 2002;23(2):96–106. doi: 10.1016/s0885-3924(01)00406-7. Retrieved from http://www.jpsmjournal.com/article/S0885-3924%2801%2900406-7/fulltext. [DOI] [PubMed] [Google Scholar]
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: Outcomes of a family medicine hospitalist model in Singapore. Journal of Hospital Medicine. 2011;6(3):115–121. doi: 10.1002/jhm.821. [DOI] [PubMed] [Google Scholar]
- Kaldjian LC, Erekson ZD, Haberle TH, Curtis AE, Shinkunas LA, Cannon KT, Forman-Hoffman VL. Code status discussions and goals of care among hospitalised adults. Journal of Medical Ethics. 2009;35(6):338–342. doi: 10.1136/jme.2008.027854. [DOI] [PubMed] [Google Scholar]
- Kass-Bartelmes BL, Hughes R. Advance care planning: Preferences for care at the end of life. Agency for Healthcare Research and Quality Research in Action (12) 2003 Retrieved from http://www.ahrq.gov/research/endliferia/endria.htm.
- Kools S, McCarthy M, Durham R, Robrecht L. Dimensional analysis: Broadening the conception of grounded theory. Qualitative Health Research. 1996;6:312–330. [Google Scholar]
- Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. New England Journal of Medicine. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maa J, Carter JT, Gosnell JE, Wachter R, Harris HW. The surgical hospitalist: A new model for emergency surgical care. Journal of the American College of Surgeons. 2007;205(5):704–711. doi: 10.1016/j.jamcollsurg.2007.05.008. [DOI] [PubMed] [Google Scholar]
- Mussman GM, Conway PH. Pediatric hospitalist systems versus traditional models of care: Effect on quality and cost outcomes. Journal of Hospital Medicine: An Official Publication of the Society of Hospital Medicine. 2011 doi: 10.1002/jhm.951. [DOI] [PubMed] [Google Scholar]
- Pardon K, Deschepper R, Vander Stichele R, Bernheim JL, Mortier F, Bossuyt N, Deliens L. Changing preferences for information and participation in the last phase of life: A longitudinal study among newly diagnosed advanced lung cancer patients. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer. 2012 doi: 10.1007/s00520-011-1369-4. [DOI] [PubMed] [Google Scholar]
- Piers RD, van Eechoud IJ, Van Camp S, Grypdonck M, Deveugele M, Verbeke NC, Van Den Noortgate NJ. Advance care planning in terminally ill and frail older persons. Patient Education and Counseling. 2011 doi: 10.1016/j.pec.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Plauth WH, 3rd, Pantilat SZ, Wachter RM, Fenton CL. Hospitalists' perceptions of their residency training needs: Results of a national survey. American Journal of Medicine. 2001;111(3):247–254. doi: 10.1016/s0002-9343(01)00837-3. [DOI] [PubMed] [Google Scholar]
- Pollak KI, Arnold RM, Jeffreys AS, Alexander SC, Olsen MK, Abernethy AP, Tulsky JA. Oncologist communication about emotion during visits with patients with advanced cancer. Journal of Clinical Oncology. 2007;25(36):5748–5752. doi: 10.1200/JCO.2007.12.4180. [DOI] [PubMed] [Google Scholar]
- Prigerson HG. Socialization to dying: Social determinants of death acknowledgement and treatment among terminally ill geriatric patients. Journal of Health, Society, and Behavior. 1992;33(4):378–395. Retrieved from http://www.jstor.org/stable/2137315. [PubMed] [Google Scholar]
- Schatzman L. Dimensional analysis: Notes on an alternative approach to the grounding of theory in qualitative research. In: Maines D, editor. Social organization and social process: Essays in honor of Anselm Strauss. New York: Aldine de Gruyter; 1991. pp. 303–314. [Google Scholar]
- Society of Hospital Medicine. General information overview. 2010 Retrieved from http://www.hospitalmedicine.org/Content/NavigationMenu/AboutSHM/GeneralInformation/General_Information.htm.
- Tattersall MH, Gattellari M, Voigt K, Butow PN. When the treatment goal is not cure: Are patients informed adequately? Supportive Care in Cancer. 2002;10(4):314–321. doi: 10.1007/s005200100291. [DOI] [PubMed] [Google Scholar]
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Lynch TJ. Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine. 2010;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- von Gunten CF, Ferris FD, Emanuel LL. The patient-physician relationship. Ensuring competency in end-of-life care: Communication and relational skills. Journal of the American Medical Association. 2000;284(23):3051–3057. doi: 10.1001/jama.284.23.3051. [DOI] [PubMed] [Google Scholar]
- Wachter RM, Goldman L. The emerging role of "hospitalists" in the American health care system. New England Journal of Medicine. 1996;335(7):514–517. doi: 10.1056/NEJM199608153350713. [DOI] [PubMed] [Google Scholar]
- Wachter RM, Goldman L. The hospitalist movement 5 years later. Journal of the American Medical Association. 2002;287(4):487–494. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- Wagner GJ, Riopelle D, Steckart J, Lorenz KA, Rosenfeld KE. Provider communication and patient understanding of life-limiting illness and their relationship to patient communication of treatment preferences. Journal of Pain and Symptom Management. 2010;39(3):527–534. doi: 10.1016/j.jpainsymman.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Weeks JC, Cook EF, O'Day SJ, Peterson LM, Wenger N, Reding D, Phillips RS. Relationship between cancer patients' predictions of prognosis and their treatment preferences. Journal of the American Medical Association. 1998;279(21):1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- Wenrich MD, Curtis JR, Shannon SE, Carline JD, Ambrozy DM, Ramsey PG. Communicating with dying patients within the spectrum of medical care from terminal diagnosis to death. Archives of Internal Medicine. 2001;161(6):868–874. doi: 10.1001/archinte.161.6.868. Retrieved from http://archinte.ama-assn.org/cgi/content/full/161/6/868. [DOI] [PubMed] [Google Scholar]
- Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Prigerson HG. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Journal of the American Medical Association. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]