Abstract
Purpose
Guidelines recommend bone density screening with dual-energy x-ray absorptiometry (DXA) in women 65 years or older, but <30% of eligible women undergo DXA testing. There is a need to identify a systematic, effective, and generalizable way to improve osteoporosis screening.
Methods
Group randomized, controlled trial of women ≥65 years old with no DXA in the past 4 years, randomized to receive intervention materials (patient osteoporosis brochure and a letter explaining how to self-schedule a DXA scan) vs. usual care (control). Outcome of interest was DXA completion.
Results
Of 2997 women meeting inclusion criteria, 977 were randomized to the intervention group. A total of 17.3% of women in the intervention group completed a DXA, compared to 5.2% in the control group (12.1% difference, p<0.0001). When including only those medically appropriate, we found a difference of 19% between the two groups (p<0.0001). DXA receipt was greater in main clinic patients compared to satellite clinic patients (20.9% main clinic vs. 10.1% satellite clinic). The cost to print and mail the intervention was $0.79 per patient, per mailing. The number of women to whom intervention needed to be mailed to yield one extra DXA performed was 9, at a cost of $7.11.
Conclusions
DXA scan completion was significantly improved through use of a mailed osteoporosis brochure and the availability for patients to self-schedule. This simple approach may be an effective component of a multi-faceted quality improvement program to increase rates of osteoporosis screening.
Keywords: osteoporosis, screening, DXA, randomized controlled trial
Introduction
The link between low bone mineral density (BMD) and increased fracture risk in women and men is well established [1, 2]. While the occurrence of a fragility fracture (e.g. hip fracture) is indicative of low BMD and a clinical diagnosis of osteoporosis made, osteoporosis can be identified in asymptomatic patients using dual energy x-ray absorptiometry (DXA). United States (U.S.) guidelines recommend screening bone density tests using central DXA in all women 65 years or older [3–5]. However, fewer than one-third of eligible U.S. women age 65 and older undergo DXA testing [6]. Achieving greater rates of osteoporosis screening might be facilitated by identifying a systematic, effective, and generalizable way for healthcare providers and patients to schedule DXA results.
Given that national guidelines recommend DXA screening for all older women [5, 7, 8], the reasons a majority of women do not receive DXA testing are likely multifactorial. Patients and their health care providers may be unaware of preventative screening recommendations and the reasons for these recommendations. Screening tests that are required relatively infrequently (i.e. less than once a year) may be difficult for patients and physicians to remember if there are few triggers (e.g. seasonality as a trigger to motivate influenza vaccination). Additionally, primary care providers (PCPs) are responsible for managing a large number of comorbidities and acute care needs and may be unable to stay current with all preventative care needs during increasingly short clinic visits [9, 10].
Mechanisms to improve screening procedures have been implemented with varying degrees of success. Electronic reminders to physicians are beneficial in some facilities with electronic medical records. A more generalizable method has been used since the 1990’s for breast cancer screening, which allows patients to self-schedule annual mammography directly without physician involvement [11].
We hypothesized that the rate of DXA testing would improve if patients were provided osteoporosis education materials, simple instructions, and capacity to self-schedule a DXA scan.
Materials and Methods
Study setting
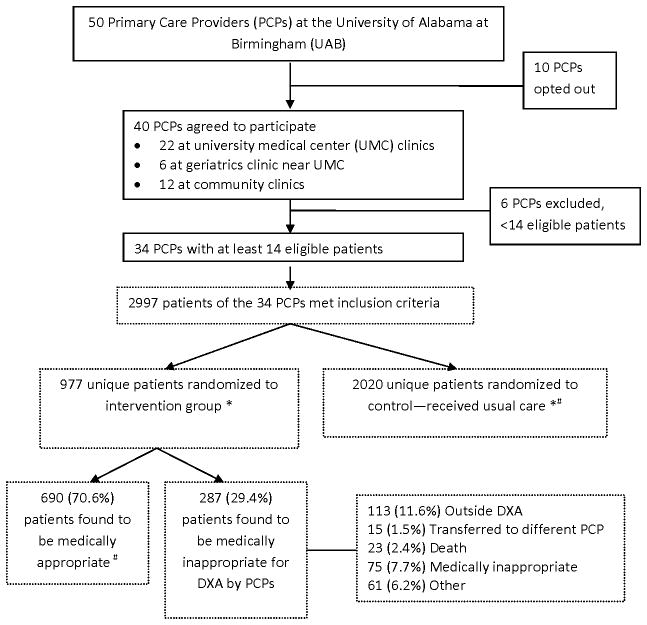
The study protocol was approved by the local Institutional Review Board. We initiated a group randomized, controlled trial involving PCPs at the University of Alabama at Birmingham (UAB). PCPs were contacted about the study and provided the opportunity to opt out via e-mail or fax response. Of a total of 50 PCPs contacted in the university medical center, 40 (80%) PCPs agreed to participate. Of these, 22 physicians were located at four internal medicine clinics at a large multi-specialty outpatient clinic affiliated with the university medical center where the DXA scans are completed; 6 physicians were located at a geriatrics clinic close to the clinic university medical center and the DXA facility; and, 12 physicians practiced at four community clinics located between 8.8 – 16.7 miles from the university medical center (Figure 1).
Figure 1.
Flow diagram
* Intent-to-Treat
# Per-Protocol
Eligible patients
Women, age 65 years or older, with at least one visit with a UAB PCP in the past 12 months and no identifiable DXA scan completed at UAB in the past 4 years were eligible to participate. Recognizing that the optimal interval for DXA testing is uncertain [12], especially if a prior DXA done was normal, 4 years was felt to be sufficient time to constitute a window for which re-testing might be clinically reasonable. Eligibility criteria were identified using administrative billing data and not an electronic medical record. All women meeting eligibility criteria were identified for each PCP that agreed to participate. Physicians were required to have a minimum of 14 eligible patients in order to participate. Random sampling of patients was performed within the practice of each participating PCP’s eligible patients. To minimize physician burden to receiving and needing to review many new DXA results concurrently, it was determined that a maximum of 20 patients per physician would be randomized to the intervention group for each cohort. Thus, for each PCP, 50% of their eligible patients, were randomized to the intervention; the remainder of each physician’s patients comprised the control group (received no mailing). After 6 months, the process was repeated, and up to 20 more women were randomly selected for each physician from the first group of control patients who had not received a DXA. Patients making up the first group of intervention and control patients were designated cohort 1 (518 intervention patients, 2,479 control patients) and the second groups formed 6 months later were designated cohort 2 (459 intervention patients, 1,683 control patients). For each of the two cohorts, the PCPs were provided a list of patients selected and were given the opportunity to decline intervention materials being sent to one or more specific patients. The university compliance department required this ‘opt-out’ process to confirm the medical necessity of the DXA test for each patient. Use of the self-scheduling mechanism in this study was tracked at the time of DXA scheduling and completion.
Intervention Materials
The intervention materials were created based on feedback from four focus groups consisting of women aged 65 years or older at risk for osteoporosis or with a history of a fracture. Focus group participants were asked about their understanding of osteoporosis, perceived risk of fracture, and experiences with fractures. A glossy educational brochure was created using components of the Health Belief Model [13–15] and feedback from the focus groups. The brochure was accompanied by a cover letter sent from two of the study investigators (JC, AW), which told the women that their PCP was aware of and in agreement with the study, and offered the recipients the opportunity to call the university medical center DXA scheduling department and directly schedule a DXA scan. The intervention materials were sent randomly without regard to timing of recent or upcoming clinic visits with the patients’ PCPs.
Pilot testing of the study materials was completed through one-to-one interviews with women at risk of osteoporosis to ensure readability and to check content. Additional piloting of the materials and the randomization process was completed and included the mailing of letters to five eligible patients from a PCP from each clinic. We then conducted telephone interviews with these patients to obtain feedback on the intervention materials and the DXA scheduling process. After completion of pilot testing, the study began. For each cohort, the intervention materials were mailed two times, 90 days apart. The cost to print and mail the intervention materials was $0.79 per patient, per mailing.
Statistical analysis
As the primary endpoint, we compared the proportion of women in the intervention and control groups who underwent a DXA scan within 90 days. Generalized estimating equations (GEE) were used to account for the clustering of patients within physicians and to pool results across the two cohorts. Any unbalanced covariates were adjusted for in the final GEE modeling. For the secondary endpoint of the trial, the observation window was extended to 180 days to include the 2nd mailing. As part of a sensitivity analysis, we included in the intervention group only the women whose doctor deemed them medically appropriate to receive a DXA in the intervention group. Stratified analyses were completed to evaluate the effect of the intervention for patients treated at the university medical center clinics vs. the satellite clinic patients. All analyses were performed using SAS 9.2 (SAS Institute, Cary, NC).
Results
For the 40 PCPs that agreed to participate, 34 had at least 14 eligible patients and were included in the randomization. In total, 2,997 patients of these 34 physicians were identified as meeting inclusion criteria based on age and lack of a DXA in the past 4 years. The average age for eligible women was 77 (Standard Deviation {SD} 7.7) years. Within this group, 977 women were randomized to the intervention group (518 in Cohort 1 and 459 in Cohort 2) (Tables 1a and 1b). Cohort 2 was smaller because three PCPs declined to participate after Cohort 1 (Figure 1). Women in the intervention groups were more likely to be younger, have had a mammogram in the past 12 months, and have more physician visits in the past 12 months when compared to the control group women, in both cohorts (Tables 1a and 1b).
Table 1a.
Baseline Characteristics of Patients in Cohort 1
| Intervention Subjects | Control Subjects | p-value | |
|---|---|---|---|
| N | 518 | 2476 | |
| Age (%) | 0.0038 | ||
| 65–69 | 23.9 | 19.6 | |
| 70–74 | 23.0 | 21.7 | |
| 75–79 | 21.8 | 20.5 | |
| 80–84 | 14.7 | 18.9 | |
| 85+ | 16.6 | 19.3 | |
| Race (%) | <0.0001 | ||
| Black | 53.9 | 34.9 | |
| White | 45.6 | 63.3 | |
| Other | 0.5 | 1.8 | |
| Mammogram in past 12 months (%) | 41.1 | 31.0 | <0.0001 |
| Number of Outpatient Visits in past 12 months (%) | 7.6±7.6 | 6.6±7.6 | 0.0047 |
| History of Fracture* (%) | 4.1 | 4.3 | 0.8197 |
| Other Co-Morbidities† (%) | |||
| COPD | 5.8 | 6.8 | 0.4116 |
| Diabetes Mellitus | 36.7 | 26.5 | <0.0001 |
| Rheumatoid Arthritis | 0.8 | 1.5 | 0.1993 |
Identified during the 12 months prior to randomization using ICD-9 Codes 733.1x, 800.x – 829.x
Identified during the 12 months prior to randomization using the respective ICD-9 codes
Table 1b.
Baseline Characteristics of Patients in Cohort 2
| Intervention Subjects | Control Subjects | p-value | |
|---|---|---|---|
| N | 459 | 1683 | |
| Age (%) | <0.0001 | ||
| 65–69 | 23.1 | 20.8 | |
| 70–74 | 19.8 | 22.9 | |
| 75–79 | 23.1 | 19.3 | |
| 80–84 | 14.8 | 19.7 | |
| 85+ | 19.2 | 18.3 | |
| Race (%) | 0.4236 | ||
| Black | 45.5 | 31.3 | |
| White | 53.6 | 66.4 | |
| Other | 0.9 | 2.3 | |
| Mammogram in past 12 months (%) | 37.9 | 24.48 | <0.0001 |
| Number of Outpatient Visits in past 12 months (%) | 6.7±7.1 | 5.8±7.3 | 0.0123 |
| History of Fracture* (%) | 6.3 | 3.0 | 0.5232 |
| Other Co-Morbidities† (%) | |||
| COPD | 6.8 | 4.8 | 0.9721 |
| Diabetes Mellitus | 25.9 | 22.6 | 0.7560 |
| Rheumatoid Arthritis | 1.5 | 1.2 | 0.8322 |
Identified during the 12 months prior to randomization using ICD-9 Codes 733.1x, 800.x – 829.x
Identified during the 12 months prior to randomization using the respective ICD-9 codes
Women were only excluded after PCPs reviewed the women selected to receive intervention materials. After review of a list of patients selected to receive intervention materials, 287 (133 in Cohort 1; 154 in Cohort 2) were determined to be medically inappropriate for the study by their PCPs. These patients were included in the primary, intent-to-treat analysis but were excluded in the per-protocol analysis. The reasons the PCPs gave for the women being medically inappropriate to participate included a known DXA scan completed at an outside facility, transfer to a different PCP, death of the patient since randomization, and concurrent medical condition (e.g. end-stage renal disease) for which the PCP felt DXA was not necessary (Figure 1). Therefore, 385 women received intervention materials in Cohort 1 and 305 women received materials in Cohort 2. PCP review of the control patients was not completed given the burdensomeness of this to the PCPs.
Eighty-nine women in the intervention group for cohort 1 and seventy-nine women in cohort 2 completed a DXA (Tables 2a and 2b). Women that completed DXA scans in both cohorts were younger and more likely to have had a mammogram in the past 12 months, when compared to women who did not complete a DXA scan (Tables 2a and 2b). In the intent-to-treat population, results for the intervention groups in Cohorts 1 and 2 were similar and were therefore pooled, using GEE to account for the clustered nature of the data. At the end of the trial at 90 days, women in the intervention group were significantly more likely to schedule and undergo DXA imaging, compared to women receiving DXA in the control group (17.3% versus 5.2% respectively, p<0.0001) (Table 3). When the intervention group was restricted to only those determined to be medically appropriate (n=692), the proportion receiving a DXA was greater; resulting in a significant difference of 19.0% between the two groups (p<0.0001) (Figure 2). Significance remained after adjusting for the baseline use of mammography and age (Table 3). In the sensitivity analysis that extended the observation period to 180 days to assess the benefit of the second mailing, an additional 3.6% (n=35) of women in the intervention group scheduled and underwent DXA imaging, compared to 1.7% (n=63) women receiving DXA in the control group (Figure 2).
Table 2a.
Characteristics of Intervention Patients that had a DXA vs. those that did not receive a DXA Cohort 1
| Completed a DXA | No DXA | p-value | |
|---|---|---|---|
| N | 89 | 429 | |
| Age (%) | 0.0099 | ||
| 65–69 | 29.2 | 22.8 | |
| 70–74 | 27.0 | 22.1 | |
| 75–79 | 24.7 | 21.2 | |
| 80–84 | 10.1 | 15.6 | |
| 85+ | 9.0 | 18.2 | |
| Race (%) | 0.3118 | ||
| Black | 58.4 | 52.9 | |
| White | 40.5 | 46.6 | |
| Other | 1.1 | 0.5 | |
| Mammogram in past 12 months (%) | 66.3 | 35.9 | <0.0001 |
| Number of Outpatient Visits in past 12 months (%) | 6.5±4.5 | 7.8±8.1 | 0.2874 |
| History of Fracture* (%) | 0 | 4.9 | 0.0333 |
| Other Co-Morbidities† (%) | |||
| COPD | 7.9 | 5.4 | 0.3579 |
| Diabetes Mellitus | 37.1 | 36.6 | 0.9317 |
| Rheumatoid Arthritis | 0 | 0.9 | 0.3609 |
Identified during the 12 months prior to randomization using ICD-9 Codes 733.1x, 800.x – 829.x
Identified during the 12 months prior to randomization using the respective ICD-9 codes
Table 2b.
Characteristics of Intervention Patients that had a DXA vs. those that did not receive a DXA Cohort 2
| Completed a DXA | No DXA | p-value | |
|---|---|---|---|
| N | 79 | 380 | |
| Age (%) | 0.0002 | ||
| 65–69 | 36.7 | 20.3 | |
| 70–74 | 22.8 | 19.2 | |
| 75–79 | 21.5 | 23.4 | |
| 80–84 | 8.9 | 16.1 | |
| 85+ | 10.13 | 21.1 | |
| Race (%) | 0.6181 | ||
| Black | 48.1 | 45.0 | |
| White | 50.6 | 54.2 | |
| Other | 1.3 | 0.8 | |
| Mammogram in past 12 months (%) | 60.7 | 33.2 | <0.0001 |
| Number of Outpatient Visits in past 12 months (mean±SD) | 8.0±7.7 | 6.4±7.0 | 0.0957 |
| History of Fracture* (%) | 5.1 | 6.6 | 0.6148 |
| Other Co-Morbidities† (%) | |||
| COPD | 5.1 | 4.7 | 0.9017 |
| Diabetes Mellitus | 30.4 | 25.0 | 0.3213 |
| Rheumatoid Arthritis | 2.5 | 1.3 | 0.4228 |
Identified during the 12 months prior to randomization using ICD-9 Codes 733.1x, 800.x – 829.x
Identified during the 12 months prior to randomization using the respective ICD-9 codes
Table 3.
DXA Receipt in Intervention Women Compared to Control Women
| DXA Receipt (95% CI) | Difference Intervention vs. Control | OR (95% CI), Crude | OR (95% CI), Adjusteda | Number Need to Mail for DXA Receiptb | ||
|---|---|---|---|---|---|---|
| Total | Intervention (n=977) | 17.3% (11.5–25.1) | 12.1% | 3.8 (2.4 – 6.1) | 2.9 (1.7 – 4.8) | 9 |
| Controlc (n=4163) | 5.2% (3.9–6.9) | - | ||||
| Per Protocold | Intervention (n=692) | 24.6% (17.5–33.4) | 19.0% | 5.6 (3.6 – 8.2) | 4.2 (2.6 – 6.7) | 6 |
| Controlb (n=4163e) | 5.6% (4.2 –7.5) | - |
Adjusted for baseline use of mammography, age, and number of outpatient visits in past 12 months
Number of women to whom intervention materials were needed to be mailed to yield one ‘extra’ DXA compared to control group
There was partial overlap in the control patients between cohorts 1 and 2, which was accounted for using generalized estimating equations (GEE).
Physician determined that it was medically appropriate for the patient to receive a DXA.
We were not able to exclude patients from the control group that were medically inappropriate
CI = Confidence Intervals; DXA = dual-energy x-ray absorptiometry; OR = Odds Ratio, using generalized estimated equations to account for the clustered nature of the data.
Figure 2.
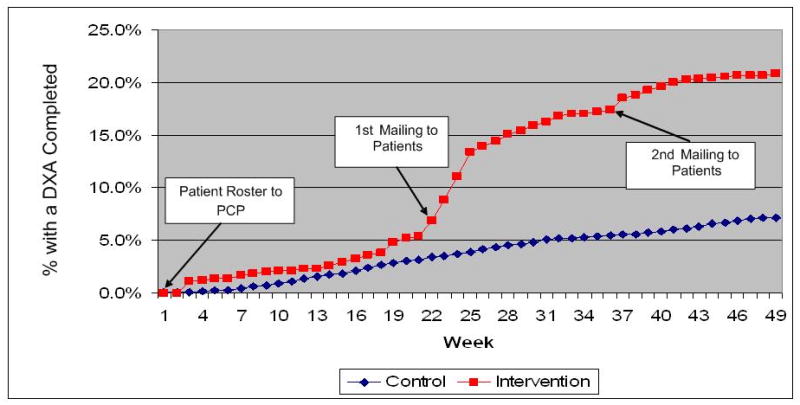
DXAs completed in relation to the timing of the mailed intervention materials (intervention group) and the corresponding time interval (control group)
Receipt of DXA for intervention patients who received their primary care at one of the main university medical center clinics (and proximate to the DXA scanner) was greater compared to patients receiving their primary care from one of the satellite clinics (20.9% vs. 10.1%, respectively). This difference was also observed, albeit smaller, for the control group patients treated at the main university medical center vs. satellite clinics (5.9% vs. 3.3%).
Among the women who completed a DXA scan in the intervention group, 44.4% had T-scores in the osteopenia range (T-score between −1.0 and −2.5) and 18.5% had T-scores in the osteoporosis range (T-score ≤ −2.5). This is compared to 47.6% and 27.7% in the control group, respectively.
The number of women to whom intervention materials needed to be mailed to yield one extra DXA performed was 9 at a mailing cost of $7.11. When the intervention group was restricted to those determined to be medically appropriate by their PCP, only 6 women, at a cost of $4.74, needed to be mailed the intervention materials to yield one extra DXA performed. The number of women to whom intervention materials needed to be mailed to yield one extra DXA performed with a diagnosis of osteoporosis was 77, whereas diagnosis of osteopenia or osteoporosis was 19; with a mailing costs of $60.83 and $15.01, respectively. These cost estimates do not include potential costs incurred from physician involvement.
Discussion
As shown in this group randomized controlled trial, we found that mailing a simple educational osteoporosis brochure and providing an opportunity to self-schedule a DXA scan significantly improved osteoporosis screening for women 65 years or older. There was an approximate 12–19% increase in the rate of DXA screening in women receiving the intervention when compared to the control group, depending on inclusion of all women (intent-to-treat) or only those found to be medically appropriate by their PCP (per protocol). The findings of our study support current efforts at increasing patient-centered activation [16–18], in part through providing the ability to self-schedule a low-risk screening procedure. DXA self-scheduling improved to a similar degree when compared to what was seen in initial evaluations of mammography self-scheduling interventions [11]. In light of a multitude of recommendations for routine health maintenance exams and monitoring [19], increasing the involvement of the patient may lessen the burden on physicians to achieve improved rates of recommended screening tests.
Although the majority of osteoporosis evidence implementation studies completed to date have focused on secondary prevention (i.e. prevention of future fracture following an initial fracture event), multiple methods to improve osteoporosis screening in persons at risk of fracture have shown varying results. One non-randomized study used an interactive voice response intervention to offer self-scheduling resulted in only 3 of 1402 at-risk men and women scheduling a DXA [20]. In another study, at-risk women between ages 65–89 were randomized to one of three groups: (1) a mailing to at-risk women (mailing served as a referral for DXA imaging), (2) the mailing plus physician prompting, or (3) usual care [21]. The group that received the mailing only was very similar to the intervention groups in our study in that they received a letter that provided patients with the opportunity to self-schedule a DXA scan along with written information regarding osteoporosis. DXA completion increased significantly in both intervention groups when compared to the control group (RD: 10.6%, mailing only; 18.1%, mailing + physician prompting) [21]. Further analyses by the study authors showed that despite an incremental increase in DXA screening with the addition of physician prompting, no additional benefit above the mailings alone was seen for the number of patients started on osteoporosis treatment following the DXA scans [21]. Two other recent studies mailed letters to at-risk women (65 years or older without prior DXA or osteoporosis treatment) with an offer to self-schedule DXA scans [22, 23]. In each of these non-randomized studies, letters were sent either with reference to the PCPs’ knowledge of the letter [23] or from a rheumatologist at the medical facility [22]. If after 2–3 weeks the patients had not responded to the letter, phone calls were made by study personnel to inquire about the reason for the lack of response and to offer DXA scheduling during the call [22, 23]. Using this combination technique of letter plus phone call to the patient, DXA completion increased 13–26% [22, 23]. Our findings of 12–19% increase in DXA completion through use of a mailed letter and brochure are similar to the changes seen with these more intensive and costly interventions that used a letter plus a call or physician prompt.
It has been shown that both providers and patients are in need of further education regarding osteoporosis and treatment for prevention of fracture [24]. However, studies focusing on changing physician practices alone, largely through education, have resulted in less robust improvement in osteoporosis screening and treatment of persons at risk [25–31]. Efforts made to simply educate patients at risk of fracture without an active component (such as DXA self-scheduling) have been disappointing [32]. Although the results of our study do not completely reverse the problem the under use of DXA screening, this low-cost intervention is a process that could be extended to most clinical settings without extensive effort or expense.
It is unclear why our intervention did not lead to a larger number of scheduled DXA scans. Prior studies have indicated that patients are interested in gaining greater knowledge of preventative medical evaluations but persons of lower socioeconomic status or of African American race may be less likely to accept outreach efforts [23, 33]. We used patient stories and included an ethnically diverse educational brochure in our intervention materials in efforts of improving uptake by all targeted persons. A recent study that used patient story-telling in a video format succeeded in significantly improving blood pressure control in a group of racially diverse persons [34]. Further investigations into the benefit of such story-telling efforts in osteoporosis prevention are needed.
The generalizability of our study may be limited because the study was conducted within a single academic health system. However, our University health system has a large and robust primary care population treated across a diverse geography. Women who received the intervention and completed a DXA did tend to be younger, had greater recent use of mammography screening and, more frequent physician visits in the past year, and, thus, may be more engaged in their healthcare and preventive health screenings. We were limited in determining other factors that may have played a role in patient utilization of the DXA self-scheduling offer. There was also greater response to the intervention in women who received care where the DXA scan was located compared to women who received care at a satellite clinic and had to travel farther to get a DXA. Both distance from the imaging center and familiarity with the center likely played a role. These findings of higher use of DXA imaging associated with proximity to the DXA scanner location is similar to a prior study that indicated that distance from DXA imaging center was a significant predictor of receiving DXA testing [35]. We were unable to identify if DXA scans were completed at DXA facilities outside of the University health system and it is possible that additional DXA scans were scheduled by patients at a facility closer to their homes. An additional limitation was the requirement that PCPs were asked to review the proposed list of intervention women to determine medical necessity. With current Medicare guidelines recommending and covering a screening DXA in all women age 65 years and older [36], this step is unlikely to be required in all health systems.
Osteoporosis prevalence is increasing with the aging population, leading to a growing need to better identify affected patients prior to the feared outcome of fragility fracture. The risk of hip fracture in women aged 70–79 outweighs the combined risk of invasive breast cancer and cardiovascular events in all races except black women [37]. In older black women, the risk of hip fracture is similar to the risk of a cardiovascular event [37]. DXA scans are a routine part of health screening since they provide healthcare providers with an assessment of a patients’ relative risk of fracture and, thus, can aid in identifying patients that may benefit from the fracture risk-reducing affects of currently available osteoporosis treatments [7, 8]. Yet, despite the low risk of DXA imaging and the general recommendations from several groups for screening DXAs in all women over the age of 65 [3–5], most women do not undergo this screening test [6]. In our study, a simple patient education brochure and the opportunity for patients to self-schedule screening DXAs led to significant increase in DXA completion.
Acknowledgments
This work was supported by an unrestricted educational grant from the Alliance for Better Bone Health and through funds from the University of Alabama at Birmingham Osteoporosis Clinic. Dr. Curtis receives support from the NIH (AR053351).
AHW: Study concept and design, Data acquisition, Analysis and Interpretation of data, Manuscript preparation and finalization
RCO: Study concept and design, Data acquisition, Analysis and Interpretation of data, Manuscript preparation and finalization
EK: Study concept and design, Manuscript preparation and finalization
LC: Study concept and design, Analysis and Interpretation of data, Manuscript preparation and finalization
SLM: Study concept and design, Interpretation of data, Manuscript preparation and finalization
KGS: Study concept and design, Analysis and Interpretation of data, Manuscript preparation and finalization
JRC: Study concept and design, Data acquisition, Analysis and Interpretation of data, Manuscript preparation and finalization
Footnotes
Disclosures
AHW: No disclosures
RCO: No disclosures
EK: No disclosures
LC: No disclosures
SLM: Consulting for Novartis, Genentech, and Amgen
KGS: Research and/or consulting: Merck, Novartis, Roche (consulting only), Eli Lilly, Amgen
JRC: Research and/or consulting: Merck, Novartis, Proctor & Gamble, Roche, Eli Lilly, Amgen
References
- 1.Johnell O, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20(7):1185–94. doi: 10.1359/JBMR.050304. [DOI] [PubMed] [Google Scholar]
- 2.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. Bmj. 1996;312(7041):1254–9. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154(5):356–64. doi: 10.7326/0003-4819-154-5-201103010-00307. [DOI] [PubMed] [Google Scholar]
- 4.Hodgson SF, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition, with selected updates for 2003. Endocr Pract. 2003;9(6):544–64. doi: 10.4158/EP.9.6.544. [DOI] [PubMed] [Google Scholar]
- 5.Clinician’s Guide to Prevention and Treatment of Osteoporosis. 2010 Available from: http://www.nof.org/sites/default/files/pdfs/NOF_ClinicianGuide2009_v7.pdf.
- 6.Curtis JR, et al. Longitudinal trends in use of bone mass measurement among older americans, 1999–2005. J Bone Miner Res. 2008;23(7):1061–7. doi: 10.1359/JBMR.080232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bone Health and Osteoporosis: A Report of the Surgeon General. 2004 Feb 22;2011 Available from: http://www.surgeongeneral.gov/library/bonehealth/chapter_8.html#Step1IdentifyAtRiskIndividualsWhoRequireFurtherEvaluation. [PubMed] [Google Scholar]
- 8.Recommendation Statement: Screening for Osteoporosis. 2011 Available from: http://www.uspreventiveservicestaskforce.org/uspstf10/osteoporosis/osteors.htm.
- 9.Majumdar SR, Soumerai SB. Why most interventions to improve physician prescribing do not seem to work. CMAJ. 2003;169(1):30–1. [PMC free article] [PubMed] [Google Scholar]
- 10.Majumdar SR, McAlister FA, Furberg CD. From knowledge to practice in chronic cardiovascular disease: a long and winding road. J Am Coll Cardiol. 2004;43(10):1738–42. doi: 10.1016/j.jacc.2003.12.043. [DOI] [PubMed] [Google Scholar]
- 11.King ES, et al. Promoting mammography use through progressive interventions: is it effective? Am J Public Health. 1994;84(1):104–6. doi: 10.2105/ajph.84.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gourlay ML, et al. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366(3):225–33. doi: 10.1056/NEJMoa1107142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Becker MH. The Health Belief Model and Sick Role Behavior. Health Education Monographs. 1974;2:409–419. [Google Scholar]
- 14.Janz NK, Champion VL, Stretcher VJ. The Health Belief Model. In: GK, Rimer BK, Lewis FM, editors. Health Behavior and Health Education, Theory, Research, and Practice. Jossey-Bass; 2002. [Google Scholar]
- 15.Rosenstock IM, V, Strecher J, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 16.Ashe M, et al. Wristwatch-distal radial fracture as a marker for osteoporosis investigation: a controlled trial of patient education and a physician alerting system. J Hand Ther. 2004;17(3):324–8. doi: 10.1197/j.jht.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Gardner MJ, et al. Interventions to improve osteoporosis treatment following hip fracture. A prospective, randomized trial. J Bone Joint Surg Am. 2005;87(1):3–7. doi: 10.2106/JBJS.D.02289. [DOI] [PubMed] [Google Scholar]
- 18.Peterson BA, et al. The effects of an educational intervention on calcium intake and bone mineral content in young women with low calcium intake. Am J Health Promot. 2000;14(3):149–56. doi: 10.4278/0890-1171-14.3.149. [DOI] [PubMed] [Google Scholar]
- 19.Yarnall KS, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polinski JM, et al. Interactive voice response telephone calls to enhance bone mineral density testing. Am J Manag Care. 2006;12(6):321–5. [PubMed] [Google Scholar]
- 21.Lafata JE, et al. Improving osteoporosis screening: results from a randomized cluster trial. J Gen Intern Med. 2007;22(3):346–51. doi: 10.1007/s11606-006-0060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayoub WT, et al. Improving detection and treatment of osteoporosis: redesigning care using the electronic medical record and shared medical appointments. Osteoporos Int. 2009;20(1):37–42. doi: 10.1007/s00198-008-0635-x. [DOI] [PubMed] [Google Scholar]
- 23.Denberg TD, et al. An outreach intervention increases bone densitometry testing in older women. J Am Geriatr Soc. 2009;57(2):341–7. doi: 10.1111/j.1532-5415.2008.02111.x. [DOI] [PubMed] [Google Scholar]
- 24.Feldstein AC, et al. Harnessing stakeholder perspectives to improve the care of osteoporosis after a fracture. Osteoporos Int. 2008;19(11):1527–40. doi: 10.1007/s00198-008-0605-3. [DOI] [PubMed] [Google Scholar]
- 25.Curtis JR, et al. Challenges in improving the quality of osteoporosis care for long-term glucocorticoid users: a prospective randomized trial. Arch Intern Med. 2007;167(6):591–6. doi: 10.1001/archinte.167.6.591. [DOI] [PubMed] [Google Scholar]
- 26.Curtis JR, et al. Longitudinal patterns in the prevention of osteoporosis in glucocorticoid-treated patients. Arthritis Rheum. 2005;52(8):2485–94. doi: 10.1002/art.21194. [DOI] [PubMed] [Google Scholar]
- 27.Colon-Emeric C, et al. Prevalence and predictors of osteoporosis treatment in nursing home residents with known osteoporosis or recent fracture. Osteoporos Int. 2007;18(4):553–9. doi: 10.1007/s00198-006-0260-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colon-Emeric CS, et al. Randomized trial to improve fracture prevention in nursing home residents. Am J Med. 2007;120(10):886–92. doi: 10.1016/j.amjmed.2007.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Curtis JR, Saag KG. Prevention and treatment of glucocorticoid-induced osteoporosis. Curr Osteoporos Rep. 2007;5(1):14–21. doi: 10.1007/BF02938618. [DOI] [PubMed] [Google Scholar]
- 30.Davis DA, et al. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 31.Kiefe CI, et al. Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA. 2001;285(22):2871–9. doi: 10.1001/jama.285.22.2871. [DOI] [PubMed] [Google Scholar]
- 32.Solomon DH, et al. A randomized controlled trial of mailed osteoporosis education to older adults. Osteoporos Int. 2006;17(5):760–7. doi: 10.1007/s00198-005-0049-y. [DOI] [PubMed] [Google Scholar]
- 33.Denberg TD, Ross SE, Steiner JF. Patient acceptance of a novel preventive care delivery system. Prev Med. 2007;44(6):543–6. doi: 10.1016/j.ypmed.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 34.Houston TK, et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med. 2011;154(2):77–84. doi: 10.7326/0003-4819-154-2-201101180-00004. [DOI] [PubMed] [Google Scholar]
- 35.Curtis JR, et al. The geographic availability and associated utilization of dual-energy X-ray absorptiometry (DXA) testing among older persons in the United States. Osteoporos Int. 2009;20(9):1553–61. doi: 10.1007/s00198-008-0821-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Medicare Claims Processing Manual Chapter 18 - Preventive and Screening Services. 2011 Jun 14;2012 Available from: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c18.pdf. [Google Scholar]
- 37.Cauley JA, et al. Incidence of fractures compared to cardiovascular disease and breast cancer: the Women’s Health Initiative Observational Study. Osteoporos Int. 2008;19(12):1717–23. doi: 10.1007/s00198-008-0634-y. [DOI] [PMC free article] [PubMed] [Google Scholar]