Abstract
Purpose
Urologic injuries occur frequently during surgery in the pelvic cavity. Inadequate diagnosis and treatment may lead to severe complications and side effects. This investigation examined the clinical features of urologic complications following obstetric and gynecologic surgery.
Materials and Methods
We accumulated 47,318 obstetric and gynecologic surgery cases from 2007 to 2011. Ninety-seven patients with urological complications were enrolled. This study assessed the causative disease and surgical approach, type, and treatment method of the urologic injury.
Results
Of these 97 patients, 69 had bladder injury, 23 had ureteral injury, 2 had vesicovaginal fistula, 2 had ureterovaginal fistula, and 1 had renal injury. With respect to injury rate by specific surgery, laparoscopic-assisted radical vaginal hysterectomy was the highest with 3 of 98 cases, followed by radical abdominal hysterectomy with 15 of 539 cases. All 69 cases of bladder injury underwent primary suturing during surgery without complications. Of 14 cases with an early diagnosis of ureteral injury, 7 had a ureteral catheter inserted, 5 underwent ureteroureterostomy, and 2 underwent ureteroneocystostomy. Of nine cases with a delayed diagnosis of ureteral injury, ureteral catheter insertion was carried out in three cases, four cases underwent ureteroureterostomy, and two cases underwent ureteroneocystostomy.
Conclusions
Bladder injury was the most common urological injury during obstetric and gynecologic surgery, followed by ureteral injury. The variety of injured states, difficulty of diagnosis, and time to complete cure were much greater among patients with ureteral injuries. Early diagnosis and urologic intervention is important for better outcomes.
Keywords: Gynecologic surgical procedures, Iatrogenic disease, Urinary tract, Wounds and injuries
INTRODUCTION
The female genital and urinary tracts are anatomically closely related; therefore, the potential for injury to one must always be considered when operating on the other. Owing to improvements in gynecological and obstetric techniques that help to prevent urinary tract injury and an emphasis on immediate recognition and repair should any injury occur, long-term complications are less frequent nowadays. The risk of damage increases when the normal anatomy is altered by primary pathologic factors or when it is insufficiently identified during intraoperative complications, such as severe bleeding or pelvic adhesions. Urinary tract injury complicates an estimated 0.2 to 1% of all gynecologic procedures and pelvic operations [1]. However, if cases of indeterminate origin are included, it can be estimated that many more cases of urinary tract injury occur during pelvic surgery. The true incidence is difficult to ascertain from the literature because most studies review only patients who became symptomatic and required urologic intervention. Eighty-two percent of ureter injuries occur during pelvic surgery [2], and 75% of urinary tract injuries are due to gynecologic surgery [3]. Urinary tract injuries due to obstetric and gynecologic surgery are normally divided into two categories: acute complications such as bladder laceration or ureter laceration that can be identified immediately during the operation, and chronic complications such as vesicovaginal fistula, ureterovaginal fistula, and ureter stricture, which can occur later on. To avoid injury to the urinary tract, the gynecologist must have an accurate understanding of pelvic anatomy, use a meticulous and methodical surgical technique, and maintain a constant high degree of vigilance. In the case of ureter injury, early detection and treatment can prevent the deterioration of renal function and bring about a satisfactory prognosis [2], but nonsurgical treatment is the recommended first-line method in iatrogenic ureteral injuries with delayed diagnosis [4]. Increasingly, complex, minimally invasive endoscopic procedures are being carried out by urologists to treat pyelo-ureteric disorders.
This study was performed to investigate the clinical features of urologic complications such as iatrogenic ureter, bladder, and kidney injuries following obstetric and gynecologic surgery and to help to prevent future occurrences of urinary tract injury.
MATERIALS AND METHODS
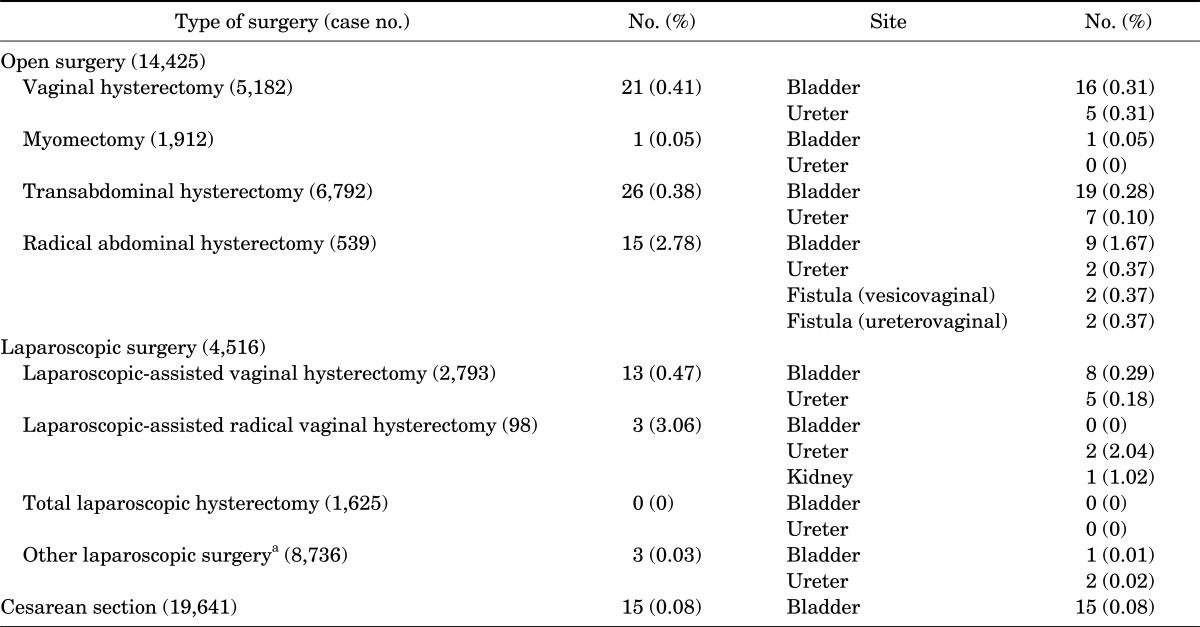
All patients who underwent obstetric and gynecologic surgeries in the pelvic cavity from 2007 through 2011 at Cheil General Hospital were analyzed. The total number of patients who underwent these surgeries was 47,318. Ninety-seven of these patients developed urological complications and were enrolled in this study (Table 1). All patients had a detailed history taken and a clinical examination performed.
TABLE 1.
Type of surgery performed in patients with urinary tract injury
a:Laparoscopic ovarian cystectomy and enucleation, laparoscopic endometriosis adhesiolysis, laparoscopic salpingectomy.
Through retrospective review, we researched the site of injury, etiologic characteristics of the injury, etiologic disease of obstetric and gynecologic surgery, and therapeutic success rate with respect to time of diagnosis and treatment of complications.
Urological complications were defined as laceration, transection, rupture, or ligation of the genitourinary tract found during surgery or as hydronephrosis and leakage of contrast media out of the urinary tract found after surgery that required interventional or surgical treatment. Success of the first repair was the criterion for successful treatment.
Patients were followed up in the outpatient clinic at 1, 3, and 6 months with complete urinalyses and urine cultures at each visit. Patients with positive urine cultures received appropriate antibiotic therapy. Follow-up intravenous urography was performed 3 months after treatment.
RESULTS
The most common type of urinary tract injury was bladder injury, including bladder laceration and vesicovaginal fistula. Of the 97 patients, 69 (71.8%) had bladder injury, 23 (23.9%) had ureteral injury, 2 (2.1%) had vesico-vaginal fistula, 2 (2.1%) had uretero-vaginal fistula, and 1 (1.0%) had renal injury (Table 1). Of the 23 cases with ureteral injury, 10 had lacerations, 7 had transections, and 6 had ligation. Thirteen of 23 had right ureteral injury and 10 had left ureteral injury. The right and left ureters were injured with similar frequency, and no patients had bilateral injury.
Laparoscopic-assisted radical vaginal hysterectomy had the highest rate of injury, with 3 (3.06%) of 98 cases. The incidence of urinary tract injury in relation to the type of surgery was 2.78% for radical abdominal hysterectomy, 0.47% for laparoscopic-assisted vaginal hysterectomy, 0.41% for vaginal hysterectomy, 0.38% for total abdominal hysterectomy, and 0.08% for cesarean section (Table 1).
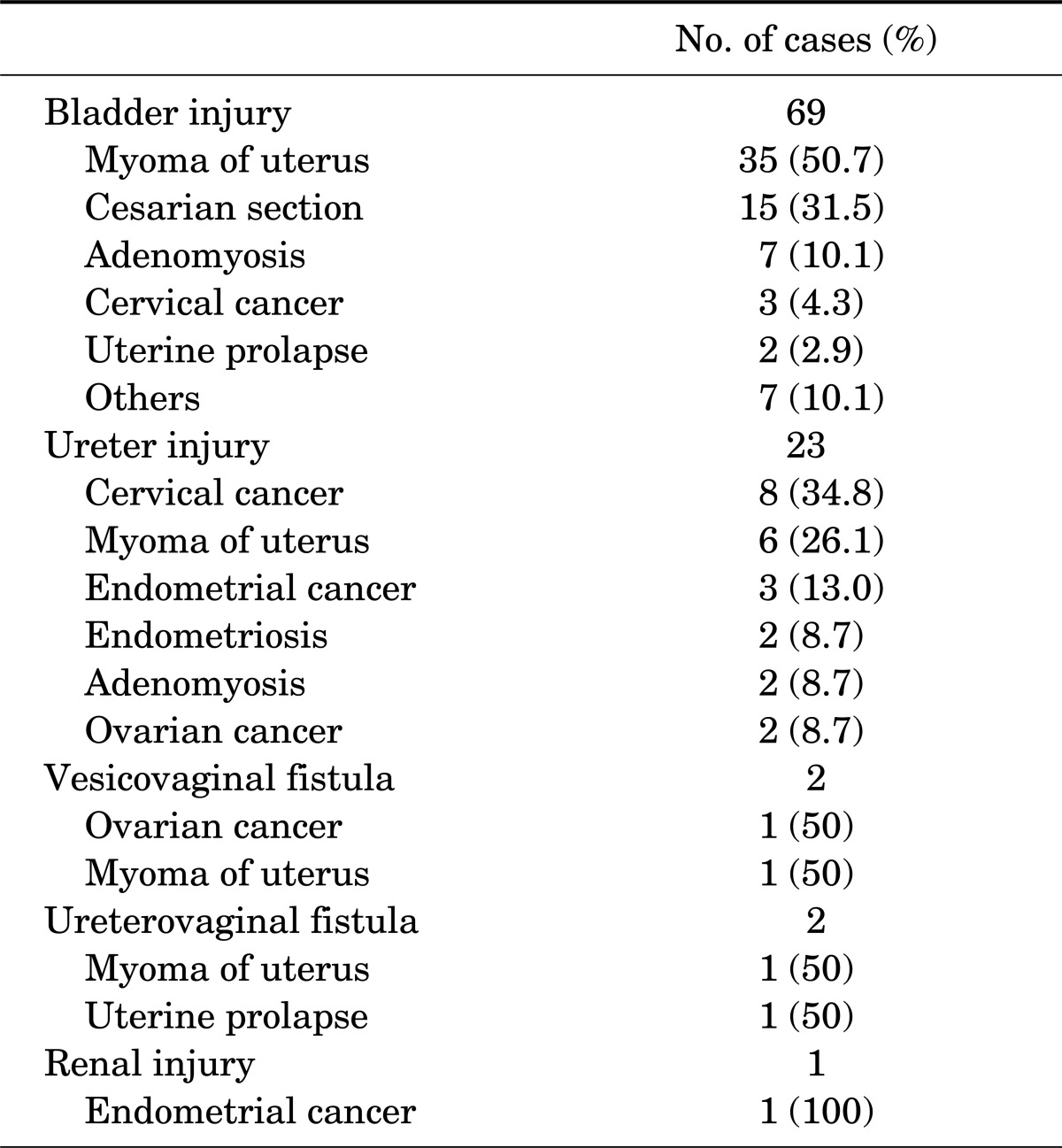
The indications for pelvic surgery in the bladder injury patients were uterine myoma (35 cases), cesarean section (15 cases), adenomyosis (7 cases), and cervical cancer (3 cases). The gynecological and obstetric diseases requiring surgery that were responsible for ureteral injuries were cervical cancer (8 cases), uterine myoma (6 cases), endometrial cancer (3 cases), and endometriosis, uterine myoma, and ovarian cancer (2 cases each). Vesicovaginal fistula resulted from treatment of ovarian cancer and uterine myoma in one patient each. Ureterovaginal fistula resulted from treatment of one case each of uterine myoma and uterine prolapse. One case of renal injury resulted from treatment of endometrial cancer (Table 2).
TABLE 2.
Etiological disease leading to obstetric and gynecologic operations
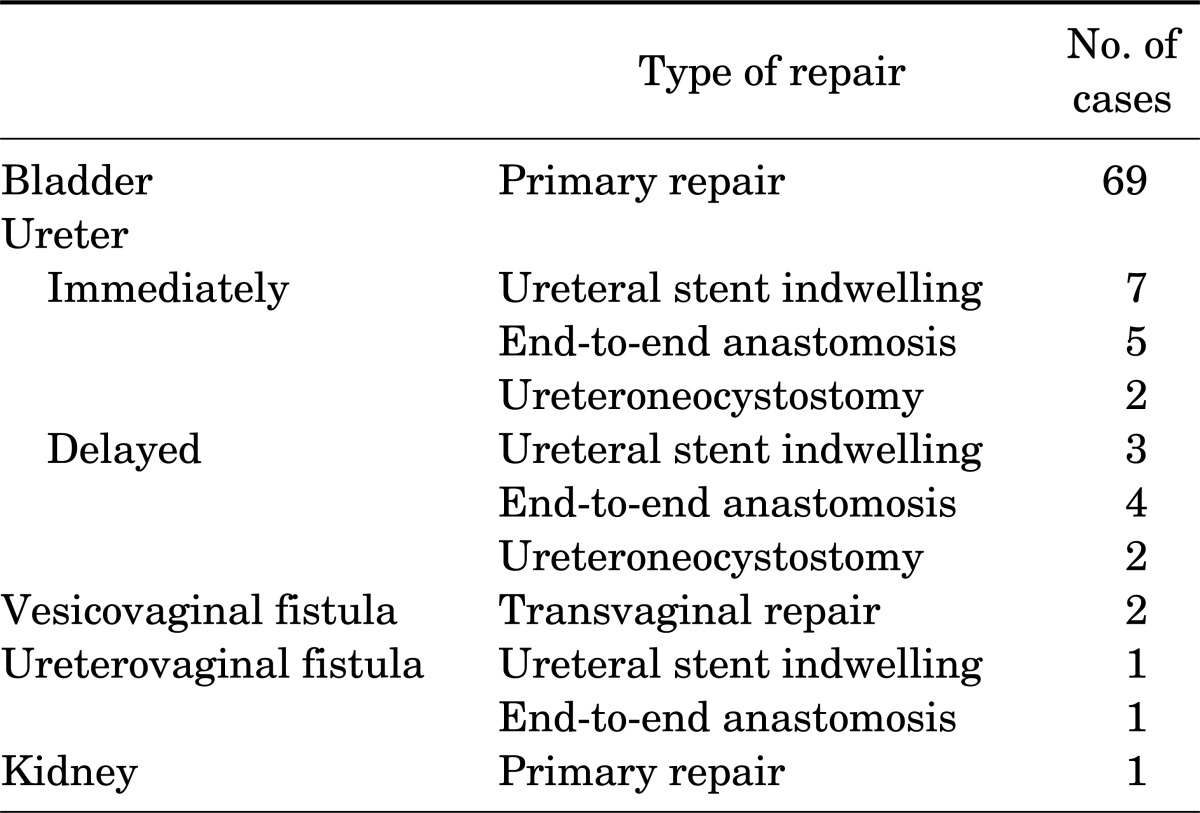
All 69 cases of bladder injury underwent combined transabdominal and transvaginal primary repair during surgery with a 100% success rate. Every patient received a urethral catheter, which was left indwelling for at least 10 to 14 days. Urethral catheters were removed only after confirming the absence of extravasation by cystogram.
Fourteen of 23 ureteral injuries were identified intraoperatively. Seven of these had a ureteral catheter inserted, five underwent ureteroureterostomy, and two cases had ureteroneocystostomy performed with no major complications. Of the remaining nine cases with delayed diagnosis of ureteral injury, ureteral catheter insertion was carried out in three cases, ureteroureterostomy in four cases, and ureteroneocystostomy in two cases. The success rate of ureteroureterostomy in the delayed diagnosis group was 50% (two of four cases). However, in the two cases with a failed initial ureteroureterostomy, one underwent ureteroneocystostomy and the other underwent ureteral balloon dilatation and the ureteral injury was successfully repaired in both. In the two cases in which ureteroneocystostomy was performed as a primary intervention, the success rate was 100%.
All four cases of vesicovaginal fistula and ureterovaginal fistula were cured after trans-vaginal primary suturing and ureteroureterostomy following percutaneous nephrostomy (Table 3). In the case of ureterovaginal fistula, ureteral catheter insertion and percutaneous nephrostomy were initially performed, followed by ureteroureterostomy after a set period to complete the repair.
TABLE 3.
Primary management of urinary tract injuries
DISCUSSION
Urinary tract injury is the most common complication of pelvic surgery. Its incidence is reported to be from 0.5 to 1.5%, and bladder injury is more common than ureter injury [2,5,6]. Most bladder injuries, but only one third of all ureter injuries, are identified during surgery. It has been reported that intraoperative cystoscopy reduces the occult ureter injury rate. The detection rate of ureter injury is 1.6 in 1,000 without cystoscopy, and 6.2 in 1,000 with cystoscopy [1], which implies that occult injury occurs more often than expected. In our study, the incidence of urinary tract injury during pelvic surgery was 0.2%. If it were possible to follow up all patients for an extended period of time, the actual incidence of urinary tract injury would certainly be higher.
Of the observed urinary tract injuries, 80% involved bladder laceration, and 74% of all cases of fistula involved vesicovaginal fistula. This suggests that the bladder is the most common site of urinary tract injury during pelvic surgery. The observed high incidence of bladder injury may be due to the fact that such injuries are easier to detect than injuries occurring at other sites.
The most common indication for pelvic surgery was leiomyoma of the uterus, and the most common type of surgery was transabdominal hysterectomy. Although urinary tract injury was most commonly associated with transabdominal hysterectomy, its rate of complication was 0.28%, which is not much higher than the rate for other pelvic procedures. Radical hysterectomy was associated with a 0.74% incidence of fistula formation, which was the highest among all types of pelvic surgery. This may be due not only to the fact that wide dissection was performed during surgery, but also that its main indication was gynecologic cancer, which can cause pelvic adhesion and changes in normal pelvic configuration. The incidence of urinary tract injury in vaginal hysterectomy was somewhat higher than average. This can be explained by the fact that it is hard to dissect the bladder with adhesions. The incidence of urinary tract injury during obstetric and gynecologic surgery could depend on the experience of the surgeon. Surprisingly, we found that experience of the surgeon, or lack thereof, did not correlate with the rate of urinary tract complications.
Intravenous pyelography prior to the operation was used to reduce the risk of urologic complications. However, performing intravenous pyelography in all patients is not cost-effective. In selected cases, it was found to aid in the detection of variant ureteral pathways [7].
Preoperative stent insertion was recommended when patients had a history of previous pelvic surgery or there was a strong suspicion of pelvic adhesion. This makes the identification of the ureter easier and makes it less prone to injury. However, its reported cost-effectiveness was lower than expected [8].
The most common sites of ureteral injury during hysterectomy are along the pelvic wall lateral to the uterine artery, the area of ureterovesical junction, and the base of infundibulopelvic ligament [9,10]. This procedure requires special attention during dissection. In cases of gynecologic surgery with severe pelvic adhesion, methylene blue injection or intraoperative cystoscopy is recommended because it is hard to directly identify ureter patency. When there is any suspicion of urinary tract injury, this procedure is very useful for preventing and identifying it. The timing of repair of ureteric injuries is somewhat controversial, with some urologists advocating immediate repair whereas others favor delayed repair [11]. It has been argued that recognition and repair of injury at the time of urinary tract injury or within a week of the injury allows for better results with fewer complications [11]. Intraoperatively recognized injuries are usually more easily repaired at the time without the need for a second surgical intervention. However, we found that postoperative diagnosis of ureteral injury and delayed repair had its own merits. In this situation, surgeons were able to find the borders of viable tissues more readily and were able to avoid unnecessary excision. As a result, the rate of bleeding complications was lower and suture tension was reduced [12].
The urinary tract-vaginal fistula, which was the most common complication detected after pelvic surgery, originates as the result of urine leakage from the vagina and was sometimes accompanied by fever, flank pain, and chills [13]. Our findings in this study were similar to those of others who reported that the duration from operation to appearance of symptoms was from 3 to 33 days [14]. In the cases of fistula that we treated, repair was performed and stent insertion was also included when the fistula was accompanied by ureter stricture.
CONCLUSIONS
Bladder injury occurred very frequently as opposed to ureteral injury. The variety of injured states, difficulty of diagnosis, and time to complete cure were much greater among patients with ureteral injury. When a urologic complication develops, early diagnosis and early urologic intervention are necessary to prevent the occurrence of delayed urologic complications.
Footnotes
The authors have nothing to disclose.
References
- 1.Gilmour DT, Dwyer PL, Carey MP. Lower urinary tract injury during gynecologic surgery and its detection by intraoperative cystoscopy. Obstet Gynecol. 1999;94(5 Pt 2):883–889. doi: 10.1016/s0029-7844(99)00456-1. [DOI] [PubMed] [Google Scholar]
- 2.Aronson MP, Bose TM. Urinary tract injury in pelvic surgery. Clin Obstet Gynecol. 2002;45:428–438. doi: 10.1097/00003081-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Thompson JD. Operative injuries to the ureter: prevention, recognition, and management. In: Rock JA, Thompson JD, editors. TeLinde's operative gynecology. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 1997. pp. 1135–1174. [Google Scholar]
- 4.Lang EK, Lanasa JA, Garrett J, Stripling J, Palomar J. The management of urinary fistulas and strictures with percutaneous ureteral stent catheters. J Urol. 1979;122:736–740. doi: 10.1016/s0022-5347(17)56579-9. [DOI] [PubMed] [Google Scholar]
- 5.Frankman EA, Wang L, Bunker CH, Lowder JL. Lower urinary tract injury in women in the United States, 1979-2006. Am J Obstet Gynecol. 2010;202:495.e1–495.e5. doi: 10.1016/j.ajog.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozdemir E, Ozturk U, Celen S, Sucak A, Gunel M, Guney G, et al. Urinary complications of gynecologic surgery: iatrogenic urinary tract system injuries in obstetrics and gynecology operations. Clin Exp Obstet Gynecol. 2011;38:217–220. [PubMed] [Google Scholar]
- 7.Piscitelli JT, Simel DL, Addison WA. Who should have intravenous pyelograms before hysterectomy for benign disease? Obstet Gynecol. 1987;69:541–545. [PubMed] [Google Scholar]
- 8.Kuno K, Menzin A, Kauder HH, Sison C, Gal D. Prophylactic ureteral catheterization in gynecologic surgery. Urology. 1998;52:1004–1008. doi: 10.1016/s0090-4295(98)00382-3. [DOI] [PubMed] [Google Scholar]
- 9.Liapis A, Bakas P, Giannopoulos V, Creatsas G. Ureteral injuries during gynecological surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:391–393. doi: 10.1007/pl00004045. [DOI] [PubMed] [Google Scholar]
- 10.Neuman M, Eidelman A, Langer R, Golan A, Bukovsky I, Caspi E. Iatrogenic injuries to the ureter during gynecologic and obstetric operations. Surg Gynecol Obstet. 1991;173:268–272. [PubMed] [Google Scholar]
- 11.Selzman AA, Spirnak JP. Iatrogenic ureteral injuries: a 20-year experience in treating 165 injuries. J Urol. 1996;155:878–881. doi: 10.1016/s0022-5347(01)66332-8. [DOI] [PubMed] [Google Scholar]
- 12.Moriel EZ, Meirow D, Zilberman M, Farkas A. Experience with the immediate treatment of iatrogenic bladder injuries and the repair of complex vesico-vaginal fistulae by the transvesical approach. Arch Gynecol Obstet. 1993;253:127–130. doi: 10.1007/BF02767329. [DOI] [PubMed] [Google Scholar]
- 13.Lee RA, Symmonds RE, Williams TJ. Current status of genitourinary fistula. Obstet Gynecol. 1988;72(3 Pt 1):313–319. [PubMed] [Google Scholar]
- 14.Oh BR, Kwon DD, Park KS, Ryu SB, Park YI, Presti JC., Jr Late presentation of ureteral injury after laparoscopic surgery. Obstet Gynecol. 2000;95:337–339. doi: 10.1016/s0029-7844(99)00539-6. [DOI] [PubMed] [Google Scholar]