Abstract
Hemangiolymphangioma is an extremely rare malformation of both the lymphatic and blood vessels. To date, however, there are no reports in the literature of a hemangiolymphangioma of the testis. An 84-year-old man visited our hospital for investigation of a 1-month episode of a rapidly growing mass in his right scrotum. Scrotal ultrasonography revealed a multilobulated mass with septation in the testis. Testicular tumor markers were within the normal limit. Radical orchiectomy was performed. At surgery, a red, wide-based, nodular tumor was found on the testis. Histological examination of the resected specimen showed it to be a cavernous hemangiolymphangioma. Here we report this first case of a cavernous hemangiolymphangioma of the testis without cutaneous hemangiomatosis in an elderly patient.
Keywords: Hemangioma, Lymphangioma, Testis
Hemangiolymphangioma is an extremely rare malformation of both the lymphatic and blood vessels [1]. Although histologically it is a benign disorder, it has a propensity to invade underlying tissues and to recur locally [2]. Hemangiolymphangioma is usually a lymphatic-venous or lymphatic-capillary malformation. To our knowledge, there are no reports in the literature of a hemangiolymphangioma of the testis. Here we report this first case of a cavernous hemangiolymphangioma of the testis without cutaneous hemangiomatosis in an elderly patient.
CASE REPORT
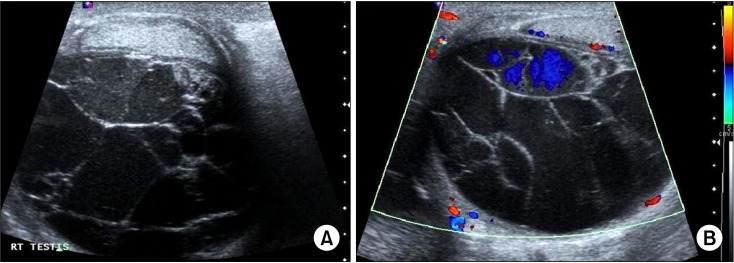
An 84-year-old man visited our hospital with a chief complaint of right scrotal swelling. He had a 1-month episode of a rapidly growing painless mass on his right scrotum. His past medical history was unremarkable, and he had no previous history of trauma or infection. He had no family history or personal history of vascular or lymphatic malformations. Physical examination revealed a nontender, hard, 6.0-cm mass in the testis of the right scrotum. There was an elastic, irregular, palpable hard mass on the testis. There were no features of cavernous diseases such as cutaneous port-wine hemangioma, varicose veins, or bony hypertrophy. The laboratory results, including complete blood count, serum electrolytes, and serum tumor markers, were all within the normal range. Scrotal ultrasonography (US) demonstrated a hypoechoic, multilobulated mass with septation in the right testis, and low blood flow was seen on color Doppler US (Fig. 1). There was no extension to the perineum or groin and no regional lymph adenopathy. Right radical orchiectomy by the inguinal approach was performed. At surgery, a red, wide-based, nodular tumor was found on the testis. The orchiectomy specimen weighed 35 g and measured 6.7×5.4×2.8 cm. The testis was diffusely thickened and showed dilated blood vessels filled with blood (Fig. 2). Histological examination of the resected specimen showed it to be a cavernous hemangiolymphangioma. Histopathological features of the testicular mass showed both hemangiomatous and lymphangiomatous components (Fig. 3). The postoperative course was uneventful and no recurrence was seen after 1 year.
FIG. 1.
(A) Scrotum ultrasonography showing a multilobulated mass with septation in the testis. (B) Low blood flow was seen on color Doppler ultrasonography.
FIG. 2.

Gross photograph of the testis after right radical orchiectomy. The testis was diffusely thickened and showed dilated blood vessels filled with blood.
FIG. 3.
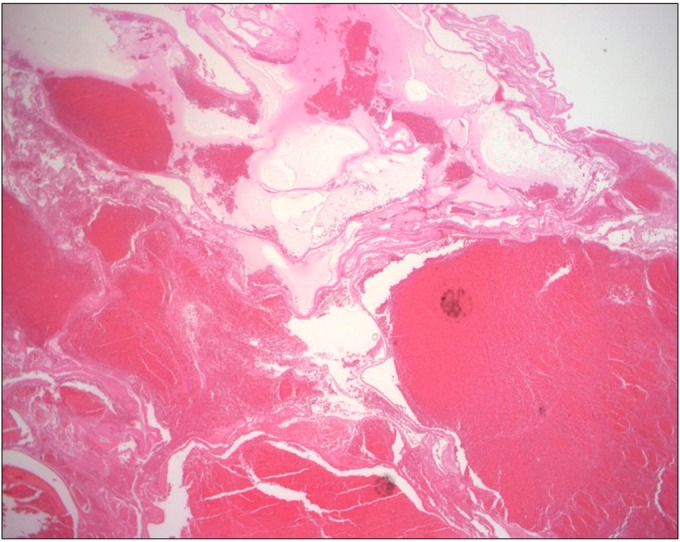
Histopathological features of the hemangiolymphangioma showing both hemangiomatous and lymphangiomatous components (H&E, ×100).
DISCUSSION
Hemangiolymphangiomas are mixed vascular malformations containing both vascular and lymphatic elements [1]. They belong to the group of low-flow vascular lesions and have radiologic features of both venous and lymphangial malformations. Although hemangiolymphangiomas occur relatively rarely, some cases have been reported as part of a congenital cavernous syndrome such as Klippel-Trenaunay-Weber syndrome [3]. Klippel-Trenaunay Weber syndrome is a rare congenital soft tissue anomaly characterized by the presence of multiple hemangiomas, asymmetric limb hypertrophy, and arteriovenous fistulas [3]. Although hemangiolymphangioma is considered a benign disorder, it has a tendency to infiltrate adjacent tissues and to recur locally. It can occur in a variety of anatomic locations, including the axilla, abdominal cavity, and extremities [4]. Our patient had cavernous hemangiolymphangioma of the testis without other lesions, making him an unusual case in the literature.
The coexistence of these two pathological entities suggests a possible common etiology and pathogenesis related to anomalies of lymphojugular sacs developing in embryos [5]. Although the diagnosis of hemangiolymphangioma is essentially made by pathologic study of the surgical specimen, modern radiological techniques, such as computed tomography scan, magnetic resonance imaging, and blood-pool scintigraphy using 99mtechnetium-human serum albumin combined with diethylenetriaminepenta-acetic acid studies, can show the vascular component of the mass before surgery and could be very helpful in diagnosis and in planning an appropriate surgical procedure [6]. In our case, we recommended that the patient undergo a computed tomography scan, but he did not want to undergo further costly imaging studies. He was a penniless older man.
The prognosis of hemangiolymphangioma is generally considered to be favorable, with only a rare incidence of malignant transformation [7]. Also, in our patient, the postoperative course was uneventful and no recurrence was seen after 1 year.
Cavernous hemangiomas are benign vascular tumors [8]. Cavernous hemangiomas of the testis are rare. Hemangiomas usually do not cause difficulty in diagnosis, because the patients present with a palpable scrotal mass. Furthermore, Doppler US is a helpful diagnostic tool to demonstrate the nature of the mass and to differentiate it from other testicular neoplasms. Histologically, they are composed of large vessels with dilated lumina and thin walls.
Lymphangiomas are congenital lymphatic malformations thought to result from the failure of the sequestered embryonic lymph sacs to communicate with the venous system. Histologically, lymphangiomas are classified as capillary, cavernous, and cystic according to the size of the dilated lymphatic space within the tumor. Lymphangiomas occur most after puberty. About 95% of lymphangiomas occur in the neck and axilla, and the remaining 5% occur in the mediastinum, mesentery, retroperitoneum, and in bone [9]. Lymphangiomas in the scrotum are extremely rare [10]. Because lymphangiomas are multiseptated tumors, they appear as multiseptated hypoechoic masses on US. In our patient, the scrotal mass had a coexistence feature of hemangiomas and lymphangiomas. US demonstrated a hypoechoic, multilobulated mass with septation in the right testis. The testis was diffusely thickened and showed dilated blood vessels filled with blood. Histological examination of the resected specimen showed features of both hemangiomatous and lymphangiomatous components.
To our knowledge, this is an extremely rare case of cavernous hemangiolymphangioma of the testis. Therefore, we report this case as a reminder that hemangiolymphangioma can occur in the testis without cutaneous hemangiomatosis in older patients.
Footnotes
The authors have nothing to disclose.
References
- 1.Donnelly LF, Adams DM, Bisset GS., 3rd Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol. 2000;174:597–608. doi: 10.2214/ajr.174.3.1740597. [DOI] [PubMed] [Google Scholar]
- 2.Giacalone PL, Boulot P, Marty M, Deschamps F, Laffargue F, Viala JL. Fetal hemangiolymphangioma: a case report. Fetal Diagn Ther. 1993;8:338–340. doi: 10.1159/000263849. [DOI] [PubMed] [Google Scholar]
- 3.Paladini D, Lamberti A, Teodoro A, Liguori M, D'Armiento M, Capuano P, et al. Prenatal diagnosis and hemodynamic evaluation of Klippel-Trenaunay-Weber syndrome. Ultrasound Obstet Gynecol. 1998;12:215–217. doi: 10.1046/j.1469-0705.1998.12030215.x. [DOI] [PubMed] [Google Scholar]
- 4.Tseng JJ, Chou MM, Ho ES. Fetal axillary hemangiolymphangioma with secondary intralesional bleeding: serial ultrasound findings. Ultrasound Obstet Gynecol. 2002;19:403–406. doi: 10.1046/j.1469-0705.2002.00633.x. [DOI] [PubMed] [Google Scholar]
- 5.Vilanova JC, Barcelo J, Smirniotopoulos JG, Perez-Andres R, Villalon M, Miro J, et al. Hemangioma from head to toe: MR imaging with pathologic correlation. Radiographics. 2004;24:367–385. doi: 10.1148/rg.242035079. [DOI] [PubMed] [Google Scholar]
- 6.Cannard L, Lemelle JL, Gaconnet E, Champigneulle J, Mainard L, Claudon M. Dynamic MR imaging of bladder haemangioma. Pediatr Radiol. 2001;31:882–885. doi: 10.1007/s002470100012. [DOI] [PubMed] [Google Scholar]
- 7.Engel JD, Kuzel TM, Moceanu MC, Oefelein MG, Schaeffer AJ. Angiosarcoma of the bladder: a review. Urology. 1998;52:778–784. doi: 10.1016/s0090-4295(98)00286-6. [DOI] [PubMed] [Google Scholar]
- 8.Park JS, Chung DY, Kim SJ, Kim YS, Lee EJ, Park KH. Hemangioma of scrotum: a report of 3 cases. Korean J Urol. 1997;38:885–888. [Google Scholar]
- 9.Loberant N, Chernihovski A, Goldfeld M, Sweed Y, Vais M, Tzilman B, et al. Role of Doppler sonography in the diagnosis of cystic lymphangioma of the scrotum. J Clin Ultrasound. 2002;30:384–387. doi: 10.1002/jcu.10080. [DOI] [PubMed] [Google Scholar]
- 10.Hamada Y, Yagi K, Tanano A, Kato Y, Takada K, Sato M, et al. Cystic lymphangioma of the scrotum. Pediatr Surg Int. 1998;13:442–444. doi: 10.1007/s003830050364. [DOI] [PubMed] [Google Scholar]