Abstract
A 57-year-old man who had recently undergone a transrectal prostate biopsy for a rising prostate-specific antigen level developed postbiopsy necrotizing epididymo-orchitis (requiring orchiectomy) and then Gram-negative meningitis, despite fluoroquinolone administration for periprocedural prophylaxis and subsequent therapy. The causative organism proved to be a fluoroquinolone-resistant Escherichia coli strain from sequence type ST131.
CASE REPORT
A57-year-old man was admitted to the hospital in 2007 for fever, chills, headache, low back pain, nausea, and vomiting.
Eight weeks previously, he had undergone transrectal ultrasound-guided prostate (TRUSP) biopsy due to a rising prostate-specific antigen (PSA) level despite long-term dutasteride therapy (2+ years) and a trial of oral ciprofloxacin (500 mg orally twice daily for 20 days before biopsy). Transrectal ultrasound showed suspicious hypoechoic areas. Perioperative oral ciprofloxacin (500 mg twice daily) was given for 72 h, beginning just prior to the biopsy, which revealed moderate chronic prostatitis, without malignancy. No culture was done.
Five days postbiopsy, bilateral scrotal swelling developed. Sequential oral levofloxacin and amoxicillin-clavulanate therapy were tried, without benefit. By day 14 postbiopsy, worsening left testicular pain and swelling prompted hospital admission and intravenous levofloxacin and gentamicin therapy. Scrotal ultrasound showed absent blood flow to the left testicle. Urgent left orchiectomy revealed testicular ischemia from severe epididymo-orchitis. The patient was discharged on hospital day 3 with 5 days of oral levofloxacin, 500 mg daily. Intraoperative cultures yielded Escherichia coli resistant to ampicillin, fluoroquinolones, and gentamicin; intermediate to tobramycin and ampicillin-sulbactam; and susceptible to aztreonam, cephalosporins, carbapenems, piperacillin-tazobactam, and trimethoprim-sulfamethoxazole (Table 1).
TABLE 1.
Susceptibility profile of the patient's four Escherichia coli clinical isolatesa
| Agent | MIC (μg/ml) | Interpretation |
|---|---|---|
| Amikacin | 4 | Susceptible |
| Ampicillin | ≥32 | Resistant |
| Ampicillin-sulbactam | 16 | Intermediate |
| Aztreonam | ≤1 | Susceptible |
| Cefepime | ≤1 | Susceptible |
| Ceftazidime | ≤1 | Susceptible |
| Ceftriaxone | ≤1 | Susceptible |
| Ciprofloxacin | ≥4 | Resistant |
| Ertapenem | ≤0.5 | Susceptible |
| Gentamicin | ≥16 | Resistant |
| Imipenem | ≤1 | Susceptible |
| Levofloxacin | ≥8 | Resistant |
| Piperacillin-tazobactam | ≤4 | Susceptible |
| Tobramycin | 8 | Intermediate |
| Trimethoprim-sulfamethoxazole | ≤20 | Susceptible |
Isolates included (i) the initial orchiectomy isolate and, 6 weeks later, the (ii) urine, (iii) blood, and (iv) cerebrospinal fluid isolates. All isolates gave identical susceptibility testing results.
Five days before the index admission (i.e., approximately 7 weeks postbiopsy and 5 weeks postorchiectomy), the patient developed fever, chills, anorexia, nausea, emesis, low back pain, and severe headache. Upon presentation and admission, he was in distress from the headache and mild photophobia but otherwise appeared fairly well. Vital signs, physical examination, and screening blood tests were normal. Urine was cloudy, with ≥100 white blood cells (WBC), 11 to 20 red blood cells (RBC), and many bacteria per high-power field. Blood and urine cultures were collected. Intravenous levofloxacin, 750 mg daily, was begun.
On day 2, lumbar puncture yielded cerebrospinal fluid (CSF) containing 1,000 leukocytes (100% neutrophils) and 2,000 erythrocytes per microliter, 140 mg/dl protein, 9 mg/dl glucose, and Gram-negative bacilli on Gram stain. Admission blood cultures grew Gram-negative bacilli.
On day 3, the CSF and urine cultures also yielded Gram-negative bacilli. Therapy was changed from levofloxacin to ceftriaxone, 2 mg intravenously daily, which was continued for 14 days. The blood, urine, and CSF isolates all proved to be E. coli, with the same susceptibility pattern and MICs as the orchiectomy isolate from 6 weeks previously (Table 1). The patient recovered uneventfully.
Context.
Infectious complications following TRUSP biopsy are increasingly frequent, due largely to the widespread emergence of fluoroquinolone-resistant Escherichia coli (FQREC) strains (3, 14). Such strains may be selected for by any previous fluoroquinolone therapy, e.g., as used here, and by the fluoroquinolone prophylaxis that is conventionally used prior to TRUSP biopsy (3, 14). Presentations of post-TRUSP biopsy infection include urosepsis, prostatitis, and, rarely, meningitis, which can be fatal (12).
The main contributor to the recent upsurge in post-TRUSP biopsy infections and FQREC is E. coli sequence type ST131, a clonal group within E. coli phylogenetic group B2 that has emerged globally over the past decade as a disseminated cause of multidrug-resistant extraintestinal infections (14). Although best known for its association with extended-spectrum β-lactamases (ESBLs), especially CTX-M-15, in many regions, ST131 is encountered more frequently as an ESBL-negative but fluoroquinolone-resistant pathogen, accounting for two-thirds or more of FQREC clinical isolates (8).
ST131 has been documented to cause distinctive, severe infections in specific host groups, including pediatric septic arthritis and osteomyelitis (7), pyomyositis in neutropenic patients (13), emphysematous pyelonephritis and renal abscesses in diabetic patients (5), and neonatal meningitis (2). To date, however, neither has ST131 been reported to cause meningitis in an adult nor have the several reported post-TRUSP biopsy E. coli meningitis isolates (as reviewed in reference 12) been characterized beyond their antimicrobial susceptibility profile.
Given the prominence of ST131 in post-TRUSP biopsy infections, ST131's association with multidrug resistance, and the multidrug-resistant nature of the reported post-TRUSP biopsy E. coli meningitis isolates, such isolates might be predicted to be ST131. The case patient, who developed post-TRUSP biopsy E. coli meningitis, allowed us to test this hypothesis and to identify ways to better prevent and manage this problem.
Laboratory analysis.
Major E. coli phylogenetic group (A, B1, B2, D), presence of 62 virulence genes associated with extraintestinal pathogenic E. coli, and O and H types were defined by using established multiplex PCR-based assays (8). ST131 status was defined based on ST131-specific single nucleotide polymorphisms in gyrB and mdh and 7-locus multilocus sequence typing (8). Presence of genes encoding group 1 CTX-M ESBLs and CTX-M-15 was determined by PCR (10). Antimicrobial susceptibility testing was by Vitek II (in the clinical laboratory). XbaI pulsed-field gel electrophoresis (PFGE) was done according to a standardized protocol (9). Using BioNumerics (Applied Maths), the PFGE profile of the patient's isolate was compared to a large private PFGE library (J.R.J.) within which isolates were assigned to a particular pulsotype if ≥94% similar to that pulsotype's index isolate (9).
Findings.
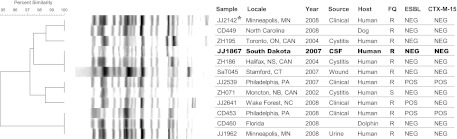
The patient's CSF isolate derived from phylogenetic group B2 and represented E. coli ST131. It exhibited the O25b rfb (O lipopolysaccharide) variant and the H4 fliC (flagellin) variant. Its virulence gene profile, which was typical of ST131 isolates generally (8), included the F10 papA allele (P fimbriae structural subunit) without papCEFG, iha (adhesin-siderophore receptor), fimH (type 1 fimbriae), sat (secreted autotransporter toxin), fyuA (yersiniabactin system), iutA (aerobactin system), kpsM II (group 2 capsule synthesis), kfiC (K5 capsular antigen), traT (serum resistance associated), usp (uropathogenic-specific protein), ompT (outer membrane protease), and malX (pathogenicity island marker). Its PFGE profile placed it within pulsotype 968 (Fig. 1), the most prevalent ST131-associated pulsotype in the private PFGE library (9), which is globally distributed and is associated with severe and distinctive infections (5, 7, 9, 11, 13). The strain's 10 nearest neighbors in the PFGE library were from multiple different locales, from humans and animals, and from diverse specimen types (Fig. 1), reflecting the broad geographical, host, and clinical range of this ST131-derived clonal lineage (9). No CTX-M group 1 or CTX-M-15 bla gene was detected in the patient's isolate, consistent with its susceptibility to extended-spectrum cephalosporins. Likewise, all but two of the nearest-neighbor comparator pulsotype 968 isolates were ESBL negative and lacked the corresponding genes (Fig. 1).
Fig 1.
Pulsed-field gel electrophoresis profiles of the patient's Escherichia coli meningitis isolate and closely related strains from sequence type ST131. Abbreviations: FQ, fluoroquinolone phenotype; R, resistant; S, susceptible; ESBL, extended-spectrum β-lactamase; NEG, negative; POS, positive. Shown are the patient's cerebrospinal fluid isolate (JJ1867; boldface), the index isolate for pulsotype 968 (JJ2142; asterisk), and the 10 next most similar isolates (relative to the patient's isolate) in a large private pulsotype library (J.R.J.). All isolates represent pulsotype 968. Note the broad geographic range of the isolates (which spans multiple widely distributed locales in the United States and Canada), the diversity of sources (blank = unknown), and the broad host range (human, dog, and dolphin).
Comment.
The case patient experienced a series of unfortunate but avoidable events, including a questionably indicated 20-day course of ciprofloxacin therapy and TRUSP biopsy (both done because of a rising screening PSA level), subsequent necrotizing epididymo-orchitis due to FQREC, ineffective empirical therapy for this, subsequent orchiectomy, ineffective postoperative therapy, subsequent meningitis due to FQREC ST131, and delayed effective therapy for this. This illustrates how the widespread emergence of a new multidrug-resistant and virulent E. coli clonal group, ST131 (8), can interact with established practice patterns regarding antimicrobial therapy (e.g., routine use of fluoroquinolones regardless of recent and current culture results and the patient's antimicrobial history) and delivery of preventive services (e.g., routine PSA screening and TRUSP biopsy), resulting in highly morbid iatrogenic complications (3, 14).
E. coli ST131 caused this case patient's post-TRUSP biopsy meningitis and, presumably (based on chronology and antibiogram), also his epididymo-orchitis, bacteremia, and bacteriuria. ST131 also was the single most common cause of E. coli bacteremia post-TRUSP biopsy in a recent study from Australia (14), with pulsotype 968 predominating (J. R. Johnson, unpublished data). Although these observations might be interpreted as indicating enhanced virulence for ST131, and especially pulsotype 968, in the post-TRUSP biopsy context, other factors may be operative. For example, ST131 is also the predominant E. coli lineage among FQREC fecal surveillance isolates from men about to undergo prostate biopsy, where pulsotype 968 also predominates (Johnson, unpublished), suggesting that ST131's predominance among postbiopsy urinary tract infection (UTI) isolates may simply reflect its high prevalence within the fecal reservoir, the presumed source for post-TRUSP biopsy infections (4), rather than enhanced pathogenicity. Additionally, our patient's progression to extreme clinical manifestations may represent the natural history of ineffectively treated E. coli genitourinary infection, with ineffective treatment in this instance resulting from repeated reliance on agents to which the organism exhibited in vitro resistance. This is a predictable consequence of unrecognized resistance to the chosen antimicrobial regimen, particularly if a patient's recent antimicrobial exposure history and susceptibility data are not factored into drug selection.
This case represents a cautionary tale regarding key management principles that should be incorporated into routine clinical practice by providers, with support from the clinical microbiology laboratory, to avoid future such mishaps. First, in most locales, fluoroquinolone monotherapy is no longer acceptable for prophylaxis prior to TRUSP biopsy (14). Substitution or addition of a more broadly active empirical agent (selected based on current local cumulative susceptibility data) (1, 6, 15), or culture-guided therapy (4), is mandatory. Second, a patient who presents with suspected infection after receiving fluoroquinolone therapy for either prophylaxis or treatment should not receive empirical monotherapy with a fluoroquinolone or another agent (e.g., gentamicin) to which coselected resistance is likely. Third, discovery of in vitro resistance to an empirically selected antimicrobial regimen should prompt, at minimum, reassessment of the patient's clinical status, if not regimen change. Finally, according to the best available evidence (as assessed by the U.S. Preventive Services Task Force, http://www.uspreventiveservicestaskforce.org/prostatecancerscreening.htm), routine PSA screening should be avoided, which would avert many unnecessary TRUSP biopsies, with their attendant infectious and noninfectious risks.
Novel aspects of this report warrant mention. To our knowledge, it describes the first case of post-TRUSP biopsy meningitis from the United States, the first case of adult meningitis or epididymo-orchitis due to ST131, and the first molecular characterization of a post-TRUSP E. coli meningitis isolate. Limitations include the unavailability of the orchiectomy, blood, and urine isolates for molecular analysis and the inherent uncertainty regarding causal relationships.
In summary, this patient developed post-TRUSP biopsy epididymo-orchitis (leading to orchiectomy), bacteremia, bacteriuria, and Gram-negative meningitis, all presumably due to the same FQREC ST131 strain, in part because of overreliance on fluoroquinolones for prophylaxis and empirical therapy. The widespread prevalence of ST131 in the general population, its ability to cause serious disease, and its typically multidrug resistance profile oblige rethinking of many standard approaches to antimicrobial prophylaxis and therapy, especially involving the genitourinary tract. Close coordination between clinicians and the clinical microbiology laboratory is essential to optimal management.
ACKNOWLEDGMENTS
This material is based upon work supported by Office of Research and Development, Medical Research Service, Department of Veterans Affairs, grant number 1 I01 CX000192 01 (J.R.J.).
Dave Prentiss (VA Medical Center) prepared the figure. Chitrita DebRoy, John Holter, Elizabeth Palavecino, Daniel Sahm, and George Zhanel provided the comparator ST131 isolates for PFGE analysis, as shown in Fig. 1.
J. R. Johnson has received grants and/or consultancies from Merck, Rochester Medical, and Syntiron. The other authors have no conflicts with the present work.
Footnotes
Published ahead of print 26 September 2012
REFERENCES
- 1. Batura D, Rao GG, Bo Nielsen P, Charlett A. 2011. Adding amikacin to fluoroquinolone-based antimicrobial prophylaxis reduces prostate biopsy infection rates. BJU 107:760–764 [DOI] [PubMed] [Google Scholar]
- 2. Billig M, Lynfield R, Qin X, Johnson JR, Weissman SJ. 2008. Detection of emerging antibiotic-resistant strains among newborn sepsis Escherichia coli in Minnesota, 2005-08, abstr G2-1273. Abstr. 48th Annu. Intersci. Conf. Antimicrob. Agents Chemother. (ICAAC)-Infect. Dis. Soc. Am. (IDSA) 46th Annu. Meet. American Society for Microbiology and Infectious Diseases Society of America, Washington, DC [Google Scholar]
- 3. Carignan A, et al. 2012. Increasing risk of infectious complications after transrectal ultrasound-guided prostate biopsies: time to reassess antimicrobial prophylaxis? Eur. Urol. 62:453–459 [DOI] [PubMed] [Google Scholar]
- 4. Duplessis CA, et al. 2012. Rectal cultures before transrectal ultrasound-guided prostate biopsy reduce post-prostatic biopsy infection rates. Urol. 79:556–563 [DOI] [PubMed] [Google Scholar]
- 5. Ender PT, et al. 2009. Transmission of extended-spectrum beta-lactamase-producing Escherichia coli (sequence type ST131) between a father and daughter resulting in septic shock and emphysematous pyelonephritis. J. Clin. Microbiol. 47:3780–3782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ho HS, Ng LG, Tan YH, Yeo M, Cheng CW. 2009. Intramuscular gentamicin improves the efficacy of ciprofloxacin as an antibiotic prophylaxis for transrectal prostate biopsy. Ann. Acad. Med. Singapore 38:212–216 [PubMed] [Google Scholar]
- 7. Johnson JR, Anderson JT, Clabots C, Johnston B, Cooperstock M. 2010. Within-household sharing of a fluoroquinolone-resistant Escherichia coli sequence type ST131 strain causing pediatric osteoarticular infection. Pediatr. Infect. Dis. J. 29:474–475 [DOI] [PubMed] [Google Scholar]
- 8. Johnson JR, Johnston B, Clabots C, Kuskowski MA, Castanheira M. 2010. Escherichia coli sequence type ST131 as the major cause of serious multidrug-resistant E. coli infections in the United States (2007). Clin. Infect. Dis. 51:286–294 [DOI] [PubMed] [Google Scholar]
- 9. Johnson JR, et al. 2012. Comparison of Escherichia coli sequence type ST131 pulsotypes by epidemiologic traits, 1967–2009. Emerg. Infect. Dis. 18:598–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johnson JR, et al. 2012. Molecular epidemiology of Escherichia coli sequence type ST131 (O25:H4) and blaCTX-M-15 among extended-spectrum cephalosporinase-producing E. coli in the United States (2000–2009). Antimicrob. Agents Chemother. 56:2364–2370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Owens RC, et al. 2011. Community transmission in the United States of a CTX-M-15-producing sequence type ST131 Escherichia coli strain resulting in death. J. Clin. Microbiol. 49:3406–3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tufan ZK, et al. 2011. A life-threatening Escherichia coli meningitis after prostate biopsy. Urol. J. 8:69–71 [PubMed] [Google Scholar]
- 13. Vigil KJ, et al. 2010. Escherichia coli pyomyositis: an emerging entity among patients with hematologic malignancies. Clin. Infect. Dis. 50:374–380 [DOI] [PubMed] [Google Scholar]
- 14. Williamson DA, et al. 2012. Escherichia coli bloodstream infection after transrectal ultrasound-guided prostate biopsy: implications of fluoroquinolone-resistant sequence type 131 as a major causative pathogen. Clin. Infect. Dis. 54:1406–1412 [DOI] [PubMed] [Google Scholar]
- 15. Zaytoun OM, et al. 2011. Emergence of fluoroquinolone-resistant Escherichia coli as cause of postprostate biopsy infection: implications for prophylaxis and treatment. Urology 77:1035–1042 [DOI] [PubMed] [Google Scholar]