Abstract
Rift Valley fever virus strain MP-12 was generated by serial plaque passages of parental strain ZH548 12 times in MRC-5 cells in the presence of a chemical mutagen, 5-fluorouracil. As a result, MP-12 encoded 4, 9, and 10 mutations in the S, M, and L segments, respectively. Among them, mutations in the M and L segments were responsible for attenuation, while the MP-12 S segment still encoded a virulent phenotype. We performed high-throughput sequencing of MP-12 vaccine, ZH548, and recombinant MP-12 (rMP-12) viruses. We found that rMP-12 contains very low numbers of viral subpopulations, while MP-12 and ZH548 contain 2 to 4 times more viral genetic subpopulations than rMP-12. MP-12 genetic subpopulations did not encode the ZH548 sequence at the 23 MP-12 consensus mutations. On the other hand, 4 and 2 mutations in M and L segments of MP-12 were found in ZH548 subpopulations. Thus, those 6 mutations were no longer MP-12-specific mutations. ZH548 encoded several unique mutations compared to other Egyptian strains, i.e., strains ZH501, ZH1776, and ZS6365. ZH548 subpopulations shared nucleotides at the mutation site common with those in the Egyptian strains, while MP-12 subpopulations did not share those nucleotides. Thus, MP-12 retains unique genetic subpopulations and has no evidence of reversion to the ZH548 sequence in the subpopulations. This study provides the first information regarding the genetic subpopulations of RVFV and shows the genetic stability of the MP-12 vaccine manufactured in MRC-5 cells.
INTRODUCTION
Rift Valley fever (RVF) is endemic to sub-Saharan Africa and has spread into Egypt, Madagascar, Saudi Arabia, and Yemen (5, 29). RVF is characterized by high rates of abortion and fetal malformation in pregnant ruminants, acute lethal hepatitis in newborn ruminants, and febrile illness in humans (8, 32, 33). Less than 1% of RVF patients develop lethal hemorrhagic fever or neurological disorder with a poor prognosis, while 1 to 10% of patients develop partial or complete blindness due to retinal damage (11). The causative agent, Rift Valley fever virus (RVFV), belongs to the family Bunyaviridae, genus Phlebovirus, and is transmitted by mosquitoes (32). Floodwater Aedes species play a primary role in the maintenance of the virus in the environment by transovarial transmission, whereas other mosquito species belonging to the genus Culex or Anopheles have been identified as potential amplification vectors (21, 29). RVFV is classified as a category A high-priority pathogen by the National Institute of Allergy and Infectious Diseases (NIAID) and an overlap select agent by the U.S. Department of Health and Human Services (HHS) and the U.S. Department of Agriculture (USDA) in the United States, and handling of the virus requires a high- and maximum-containment facility, such as a biosafety level 3 enhanced (BSL-3E) or BSL-4 laboratory (22, 23).
The RVFV genome is comprised of a tripartite negative-stranded RNA genome, i.e., small (S), medium (M), and large (L) segments (32). The S segment encodes nucleocapsid (N) and nonstructural (NSs) genes in an ambisense manner. The M segment encodes a single M mRNA, which serves as a template for the 78-kDa protein, the nonstructural protein NSm, and two viral envelope proteins (Gn and Gc). The L segment encodes the RNA-dependent RNA polymerase (L protein). Two nonstructural proteins, i.e., NSs and NSm, are not essential for viral replication, while those proteins have biological functions in RVFV-infected cells. NSs is a major virulence factor of RVFV, which inhibits host general transcription, including that of the beta interferon gene, and promotes the degradation of double-stranded RNA (dsRNA)-dependent protein kinase (PKR) (13, 19, 20). The 78-kDa and NSm proteins are involved with apoptosis in cultured mammalian cells (35), while NSm interacts with the cleavage and polyadenylation specificity factor subunit 2 (Cpsf2), the peptidyl-prolyl cis-trans-isomerase (cyclophilin)-like 2 protein (Ppil2), and the synaptosome-associated protein of 25 kDa (SNAP-25) (9). It was also indicated that NSm is involved with dissemination in mosquito vectors (7).
Currently, no licensed RVF vaccines are available for humans or animals outside areas of endemicity, and the development of highly safe and efficacious veterinary and human vaccines for RVF is important for minimizing the impact of RVF in areas of both endemicity and nonendemicity (12); e.g., after identification of ruminants infected with RVFV, vaccination should be done for uninfected ruminants as well as workers who handle infected ruminants (e.g., viremic ruminants, aborted fetuses, or other animals with suspected RFV) during an outbreak. Currently, TSI-GSD-200 (formalin-inactivated vaccine for RVF derived from the Entebbe strain) is available as an Investigational New Drug vaccine for humans. Although the TSI-GSD-200 vaccine is safe, production is limited due to the need for the use of a high-containment facility, and three doses of vaccinations are recommended for protection from wild-type (wt) RVFV (16, 30). A live-attenuated vaccine is ideal for the rapid immunization of large groups of ruminants with a single-dose vaccination. Since an outbreak of RVF is unpredictable outside areas of endemicity, preparation of such a vaccine stock is important to prevent unnecessary panic in an emergency.
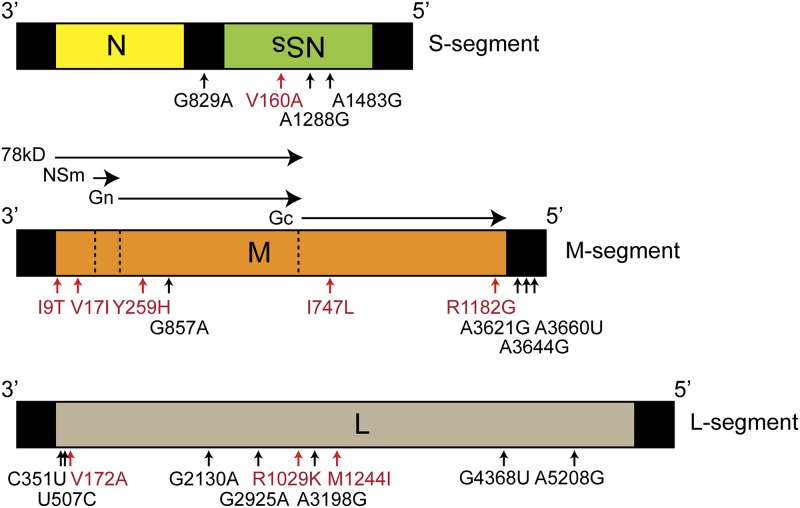
The MP-12 strain is the only RVFV strain used outside high-containment laboratories and can be handled at BSL-2 facilities. It is exempt from the select agent rule, is highly attenuated, and induces high levels of neutralizing antibodies in ruminants (25–28). The MP-12 strain has been developed by serial plaque passages of the Egyptian ZH548 strain 12 times in the presence of a chemical mutagen, 5-fluorouracil (6). As a result, MP-12 encodes a total of 23 mutations (9 amino acid substitutions) (Fig. 1). Although a previous study suggested that all S, M, and L segments of MP-12 are attenuated (31), a recent study using reverse genetics suggested that MP-12 is attenuated by M- and L-segment mutations, while the S segment encodes the virulent phenotype and the MP-12 NSs is functional (3). Therefore, MP-12 is attenuated by either of the following mutations: 5 amino acid changes or 4 silent mutations in the M segment or 3 amino acid changes or 7 silent mutations in the L segment. To better understand the stability of the potential attenuation mutations, we performed a high-throughput sequencing analysis of viral subpopulations of the MP-12 vaccine candidate. Furthermore, we also characterized subpopulations of the parental ZH548 strain and recombinant MP-12 (rMP-12) virus to compare the genetic subpopulations. As a result, we found that the MP-12 vaccine does not include detectable subpopulations encoding the ZH548 sequence at the 19 potential attenuation mutation sites in the M and L segments. On the other hand, 6 out of 19 mutations in the M and L segments were found in ZH548 subpopulations, suggesting that those mutations are no longer MP-12-specific mutations. We also found that MP-12 has genetic subpopulations distinct from those of ZH548, while recombinant MP-12, generated by reverse genetics, contains much smaller numbers of subpopulations than those of the MP-12 vaccine strain. This study provides the first information regarding viral subpopulations of RVFV. These results will be important to evaluate the risk of reversion to virulence and the attenuation mechanism of MP-12, as well as the genetic subpopulations of recombinant RVFV.
Fig 1.
Schematics of the three viral genome segments of the MP-12 vaccine strain. The 23 mutations in the MP-12 vaccine strain are shown. The S, M, and L segments encode 4, 9, and 10 mutations, respectively, in comparison with the sequence of parental strain ZH548. Amino acid substitutions are shown in red.
MATERIALS AND METHODS
Media, cells, and viruses.
BHK/T7-9 cells that express T7 RNA polymerase (15) were grown in minimal essential medium alpha containing 10% fetal bovine serum (Invitrogen). Penicillin (100 U/ml) and streptomycin (100 μg/ml) were added to the medium. BHK/T7-9 cells were selected in medium containing 600 μg/ml hygromycin B. RVFV strain ZH548 was isolated from human plasma/serum samples derived from a febrile patient during the 1977-1978 outbreak in Egyptian stock and passaged twice in suckling mouse brain, once in fetal rhesus lung (FRhL-1) cells, and once in VeroE6 cells (ZH548 reference collection vial at the University of Texas Medical Branch [UTMB]). In this study, ZH548 was amplified once in MRC-5 cell from an original ZH548 reference collection vial at UTMB. The MP-12 vaccine (Investigational New Drug status, TSI-GSD-223) was derived from the passage of strain ZH548 in FRhL-1 cells and subjected to 12 mutagenesis passages in MRC-5 cells for 12 rounds (1 round was 45 to 65 h of culture at a multiplicity of infection [MOI] of 0.1 with 5-fluorouracil, plaque purification, and amplification in MRC-5 cells without 5-fluorouracil) (6). Master seed was produced from the original MP-12 virus using certified MRC-5 cells in the Salk Institute, Government Service Division GMP facility, and subsequently, production seed was produced from the master seed in certified MRC-5 cells (Table 1). From the production seed, vaccine lot 7 was produced in certified MRC-5 cells, and lot 7-2-88 was produced by filtration and lyophilization of vaccine lot 7 (Table 1). We used reconstituted MP-12 vaccine lot 7-2-88 for high-throughput sequencing analysis without additional passages. rMP-12 was recovered from BHK/T7-9 cells by using a series of plasmids encoding cloned MP-12 S, M, and L segments as described previously (14) and passaged once in VeroE6 cells. The consensus sequences of both MP-12 lot 7-2-88 and rMP-12 are identical to reported sequences of the S segment (GenBank accession number DQ380154), M segment (GenBank accession number DQ380208), and L segment (GenBank accession number DQ375404).
TABLE 1.
Passage history of MP-12 vaccine
| Component | Source | Source vol | Production | Time of harvest (hpia) | No. of 150-cm2 flasksb | Yield |
|---|---|---|---|---|---|---|
| Original MP-12 strainc | Plaque purified clone after 12th mutagenesis | NAd | MRC-5 cells, 1 passage at 37°C | 48–72 | NA | NA |
| Master seed | Original MP-12 | 10−3 dilution, 1 ml/flask | MRC-5 cells, 1 passage at 37°C | 51 | 40 | >6.0 log10 PFU/ml (860 ml) |
| Production seed | Master seed | 10−2.5 dilution, 1 ml/flask | MRC-5 cells, 1 passage at 37°C | 50 | 60 | >6.0 log10 PFU/ml (1,750 ml) |
| Vaccine lot 7 | Production seed | 10−2 dilution, 1 ml/flask | MRC-5 cells, 1 passage at 35°C | 62 | 1,239 | 58,120 ml |
| Vaccine lot 7-2-88 | Vaccine lot 7 | 5.5 liters | Filtration, 0.45-μm-pore-size filter | 5 log10 PFU/ml, 9,360 vials (5.5 ml) (freeze-dried) |
hpi, hours postinfection.
Fifty milliliters per flask.
The production of original MP-12 was described by Caplen et al. (6).
NA, data not available.
High-throughput sequencing.
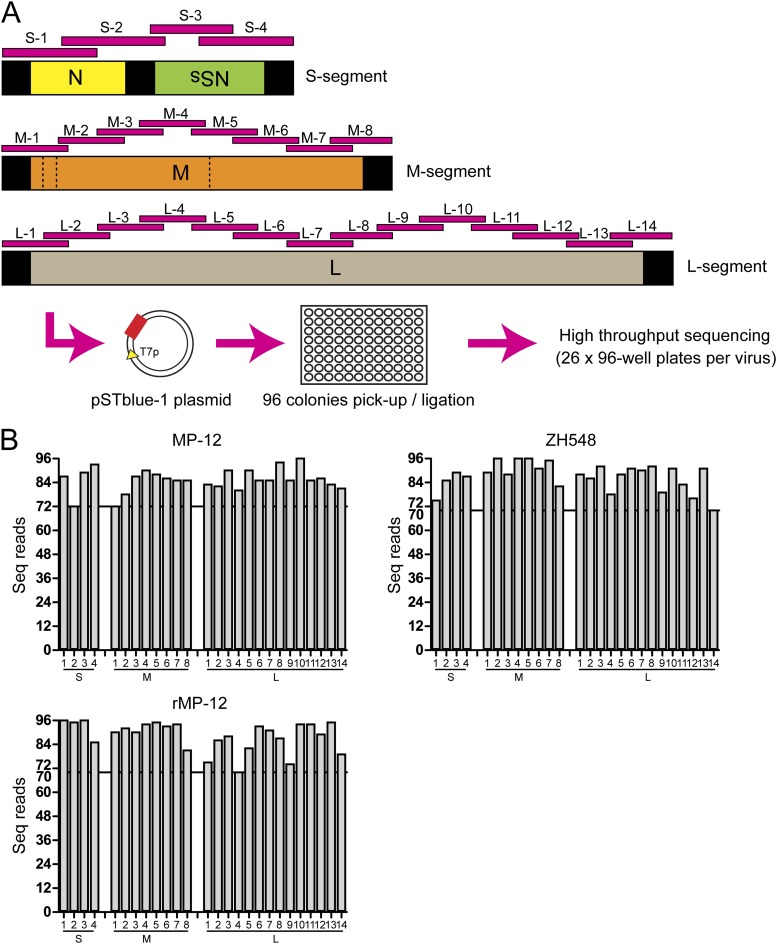
The MP-12 RVFV vaccine vial (1 × 105 PFU/ml, 300 μl), strain ZH548 with one passage in MRC-5 cells (5 × 105 PFU/ml, 300 μl), and recombinant MP-12 with one passage in VeroE6 cells (1 × 106 PFU/ml, 300 μl) were treated with 25 U of Benzonase nuclease (Novagen) at 37°C for 30 min to digest contaminated nonvirus RNAs. Viral RNA was then extracted by using TRIzol LS (Invitrogen) according to the manufacturer's instruction. The cDNA was synthesized with Superscript II and random primers (Invitrogen, Carlsbad, CA). A total of 26 PCR fragments covering the entire RVFV genome (S-1 to S-4, M-1 to M-8, and L-1 to L-14) was amplified from RVFV cDNA with Phusion DNA polymerase (New England BioLabs) and genome-specific primer pairs (Fig. 2A). The PCR was performed by use of the following condition: 98°C for 2 min, followed by 35 cycles of 98°C for 10 s, 55°C for 30 s, and 72°C for 30 s and a final 10-min extension at 72°C. The PCR product was cloned into the pSTBlue-1 Blunt vector using a Perfect Blunt cloning kit (Novagen). NovaBlue Singles competent Escherichia coli cells (Novagen) were transformed and plated on 10-cm agar plates with IPTG (isopropyl-β-d-thiogalactopyranoside)–X-Gal (5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside) solution (ChromoMax; Fisher BioReagents). Ninety-six white colonies were picked from each agar plate and transferred into 96-well plates according to the company's instructions (Beckman Coulter Genomics). Thus, we generated 26 96-well plates per virus. High-throughput sequencing was performed by Beckman Coulter Genomics. This was standard Sanger sequencing using automated DNA extraction and subsequent DNA sequencing with primer T7. Sequencing alignment and identification of mutations were performed by using Lasergene software (DNAStar, Inc.).
Fig 2.
High-throughput sequencing analysis of RVFV. (A) After incubation with Benzonase nuclease, virion-protected viral RNA was extracted and first-strand cDNA was synthesized. A total of 26 PCR fragments (S-1 to S-4, M-1 to M-8, and L-1 to L-14) were amplified and cloned into a blunt-end plasmid. Ninety-six E. coli colonies transformed with plasmid were picked and transferred into a 96-well plate. A total of 26 96-well plates per virus were analyzed by high-throughput sequencing (Beckman Coulter Genomics). (B) Coverage of sequencing per plate. At least 70 sequence (Seq) reads were obtained for each PCR fragment per 96-well plate.
Oligomers used for PCR.
For amplification of PCR fragments, the following oligomers were used: for the S segment, S20F (nucleotides [nt] 1 to 20) and S522R (nt 501 to 522) for S-1 (nt 522 bp), S465F (nt 465 to 486) and S1058R (nt 1058 to 1077) for S-2 (613 bp), S910F (nt 885 to 910) and S1343R (nt 1318 to 1343) for S-3 (459 bp), and S1279F (nt 1279 to 1305) and S1671R (nt 1671 to 1690) for S-4 (412 bp). For the M segment, M19F (nt 1 to 19) and M573R (nt 549 to 573) for M-1 (573 bp), M478F (nt 478 to 500) and M1041R (nt 1041 to 1060) for M-2 (583 bp), M999F (nt 999 to 1021) and S1566R (nt 1543 to 1566) for M-3 (568 bp), M1509F (nt 1509 to 1533) and M2047R (nt 2023 to 2047) for M-4 (539 bp), M1983F (nt 1983 to 2010) and M2515R (nt 2490 to 2515) for M-5 (533 bp), M2459F (nt 2459 to 2479) and M2995R (nt 2967 to 2995) for M-6 (537 bp), M2920F (nt 2920 to 2945) and M3397R (nt 3377 to 3397) for M-7 (478 bp), and M3356F (nt 3356 to 3376) and M3866R (nt 3866 to 3885) for M-8 (530 bp). For the L segment, L26F (nt 1 to 26) and L537R (nt 515 to 537) for L-1 (537 bp), L488F (nt 488 to 511) and L1034R (nt 1034 to 1057) for L-2 (570 bp), L1001F (nt 1001 to 1026) and L1545R (nt 1519 to 1545) for L-3 (545 bp), L1463F (nt 1463 to 1490) and L2009R (nt 1985 to 2009) for L-4 (547 bp), L1945F (nt 1945 to 1969) and L2458R (nt 2434 to 2458) for L-5 (514 bp), L2389F (nt 2389 to 2415) and L2882R (nt 2861 to 2882) for L-6 (494 bp), L2833F (nt 2833 to 2856) and L3384R (nt 3360 to 3384) for L-7 (552 bp), L3318F (nt 3318 to 3342) and L3854R (nt 3828 to 3854) for L-8 (537 bp), L3781F (nt 3781 to 3807) and L4292R (nt 4263 to 4292) for L-9 (512 bp), L4228F (nt 4228 to 4256) and L4799R (nt 4772 to 4799) for L-10 (572 bp), L4726F (nt 4726 to 4750) and L5260R (nt 5236 to 5260) for L-11 (535 bp), L5174F (nt 5174 to 5199) and L5700R (nt 5672 to 5700) for L-12 (527 bp), L5583F (nt 5583 to 5608) and L6102R (nt 6078 to 6102) for L-13 (520 bp), and L6016F (nt 6016 to 6042) and L6382R (nt 6382 to 6404) for L-14 (389 bp).
Alignment of RVFV sequences.
For the alignment of RVFV sequences, we used the consensus full-genome sequences of the following strains available at GenBank: 1260/78, 1853/78, 2250/74, 2269/74, 2373/74, 73HB1230, 73HB1449, 74HB59, CAR R1622, Hv-B375, Zinga, ARD-38388, OS-1, OS-3, OS-8, OS-9, ANK-3837, ANK-6087, MgH824, SA-51, ZH548, ZH501, MP-12, ZC-3349, ZH-1776, ZM-657, ZS-6365, Kenya 56 (IB8), Ken 57 (Rintoul), Ken 83 (21445), Kenya 98 (00523), Saudi-2000 (10911), Entebbe, and Smithburn. All the GenBank accession numbers for these strains are available in reference 4.
Ethics statement.
All the recombinant DNAs and RVFVs were created upon the approval of the Notification of Use by the Institutional Biosafety Committee at UTMB. The wt RVFV ZH548 strain was used at the Robert E. Shope BSL-4 laboratory (UTMB) in accordance with NIH guidelines and U.S. federal law.
RESULTS AND DISCUSSION
High-throughput sequencing analysis of MP-12, ZH548, and rMP-12.
We performed high-throughput sequencing analysis of the MP-12 vaccine strain (no further passage from vaccine lot 7-2-88), strain ZH548 (one passage in MRC-5 cells from reference stock), and rMP-12 (one passage in VeroE6 cells from recovered stock). We removed RNA species susceptible to Benzonase nuclease. Thus, the remaining RNA species should be viral RNA protected by the viral envelope. A total of 26 PCR fragments were amplified using a high-fidelity polymerase from viral particle RNA of each of the MP-12, ZH548, and rMP-12 viruses and ligated into a blunt-end vector (Fig. 2A). After transformation, 96 bacterial colonies were separately seeded into a 96-well plate, and subsequently, high-throughput sequencing was performed (Beckman Coulter Genomics). In total, 26 × 96 sequences were obtained for each virus, and we confirmed at least 70 successful reads per PCR fragment (Fig. 2B). In this assay, we could detect 1.0% (1/96) to 1.4% (1/70) of minor subpopulations at a minimum. Using this method, sequences of viral subpopulations derived from MP-12 vaccine (1 × 105 PFU) could be successfully obtained without further viral amplification in cells, and more than 500 bp of sequence could be read per PCR fragment.
Viral genetic subpopulations of MP-12, ZH548, and rMP-12.
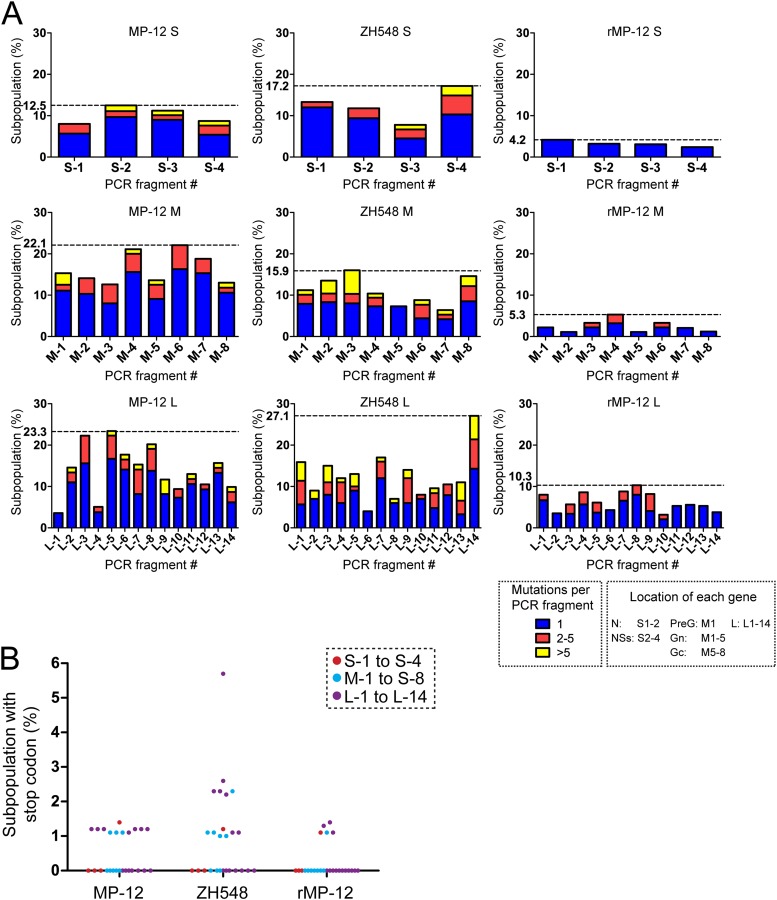
We first analyzed the percentage of viral genetic subpopulations in the MP-12 vaccine, ZH548, and rMP-12 viruses (Fig. 3A). At most, 12.5% (9 of 72), 22.1% (19 of 86), and 23.3% (21 of 90) of PCR fragments S-2, M-6, and L-5 had a sequence distinct from the MP-12 consensus sequence of the S segment (GenBank accession number DQ380154), M segment (GenBank accession number DQ380208), and L segment (GenBank accession number DQ375404), respectively. On the other hand, 87.5% (63 of 72), 77.9% (67 of 86), and 76.7% (69 of 90) were identical to the MP-12 consensus sequence of the S, M, and L segments, respectively. This suggests that MP-12 S, M, and L segments contain distinct genetic populations in 12, 22, and 23% of those genetic pools, respectively. On the other hand, 17.2% (15 of 87), 15.9% (14 of 88), and 27.1% (19 of 70) of ZH548 PCR fragments S-4, M-3, and L-14 had a sequence distinct from the ZH548 consensus sequence of the S segment (GenBank accession number DQ380151), M segment (GenBank accession number DQ380206), and L segment (GenBank accession number DQ375403), respectively. Furthermore, 4.2% (4 of 96), 5.3% (5 of 94), and 10.3% (9 of 87) of rMP-12 PCR fragments S-1, M-4, and L-8 had a sequence distinct from the MP-12 consensus sequence of the S, M, and L segments, respectively. Thus, the number of genetic subpopulations was observed to be L > M > S in MP-12, ZH548, and rMP-12. It was obvious that rMP-12 generated by a reverse genetics system contains a much lower number of genetic variations than the MP-12 or ZH548 strain.
Fig 3.
Viral genetic subpopulations. (A) The percentages of PCR fragments encoding distinct patterns of mutations are shown for the S, M, and L segments of MP-12, ZH548, and rMP-12. The maximum percentages of genetic subpopulations in each segment are indicated by dotted lines. The number of mutations per PCR fragment is shown in different colors. The locations of the N, NSs, Gn, Gc, and L ORFs are also indicated. (B) The percentages of PCR fragments encoding a stop codon(s) are shown for the S, M, and L segments, as indicated in the legend.
Next, we analyzed the number of mutations per PCR fragment (Fig. 3A). In the S segment, 0% (0 of 87), 1.4% (1 of 72), 1.1% (1 of 89), and 1.1% (1 of 93) of MP-12 PCR fragments S-1, S-2, S-3, and S-4, respectively, and 0% (0 of 75), 0% (0 of 85), 1.1% (1 of 89), and 2.3% (2 of 87) of ZH548 PCR fragments S-1, S-2, S-3, and S-4, respectively, encoded more than 5 mutations per PCR fragment, while none of the PCR fragments derived from the rMP-12 S segment encoded 2 or more mutations per PCR fragment. This finding suggests that the NSs gene has more mutations than the N gene in MP-12 and ZH548. In the M segment, MP-12 PCR fragments M-1 (2.8%; 2 of 72), M-4 (1.1%; 1 of 90), M-5 (1.1%; 1 of 88), and M-8 (1.2%; 1 of 85) and ZH548 PCR fragments M-1 (1.1%; 1 of 89), M-2 (3.1%; 3 of 96), M-3 (5.7%; 5 of 88), M-4 (1%; 1 of 96), M-6 (1.1%; 1 of 91), M-7 (1.1%; 1 of 95), and M-8 (2.4%; 2 of 82) encoded more than 5 mutations per PCR fragment, while none of the rMP-12 subpopulations encoded more than 5 mutations per PCR fragment. In the L segment, subpopulations of MP-12 PCR fragments L-2 (1.2%; 1 of 82), L-5 (1.1%; 1 of 90), L-6 (1.2%; 1 of 85), L-7 (1.2%; 1 of 85), L-8 (1.1%; 1 of 94), L-9 (3.5%; 3 of 85), L-11 (1.2%; 1 of 85), L-13 (1.2%; 1 of 83), and L-14 (1.2%; 1 of 81) and ZH548 PCR fragments L-1 (4.5%; 4 of 88), L-2 (2.3%; 2 of 86), L-3 (4.3%; 4 of 92), L-4 (1.3%; 1 of 78), L-5 (3.4%; 3 of 88), L-7 (1.1%; 1 of 90), L-8 (1.1%; 1 of 92), L-9 (2.5%; 2 of 79), L-11 (1.2%; 1 of 83), L-13 (4.4%; 4 of 91), and L-14 (5.7%; 4 of 70) encoded more than 5 mutations per PCR fragment, while none of the rMP-12 PCR fragments encoded more than 5 mutations per PCR fragment. We also noted that 8.0% (7 of 88), 10.2% (9 of 88), 8.9% (7 of 79), and 12.9% (9 of 70) of ZH548 PCR fragments M-3, L-1, L-9, and L-14 encoded 2 or more mutations per PCR fragment, respectively, while at most 7.1% (L-7, 6 of 85) of the PCR fragments derived from MP-12 or 4.1% (L-9, 3 of 74) of the PCR fragments derived from rMP-12 encoded 2 or more mutations per PCR fragment. These findings suggest that ZH548 has more frequent mutations in the subpopulations than MP-12 or rMP-12.
We noted that approximately 1 to 2% of the MP-12, ZH548, or rMP-12 PCR fragments encoding S, M, and L segments contained a stop codon(s) in the open reading frame (ORF) (Fig. 3B). In addition, 5.7% (4 of 70) of ZH548 PCR fragment L-14 sequences had a stop codon in the L ORF. Since the genome encoded a stop codon(s) in the Gn, Gc, or L ORF, which is essential for viral replication, it is possible that viral subpopulations encoding a stop codon(s) cause abortive infection.
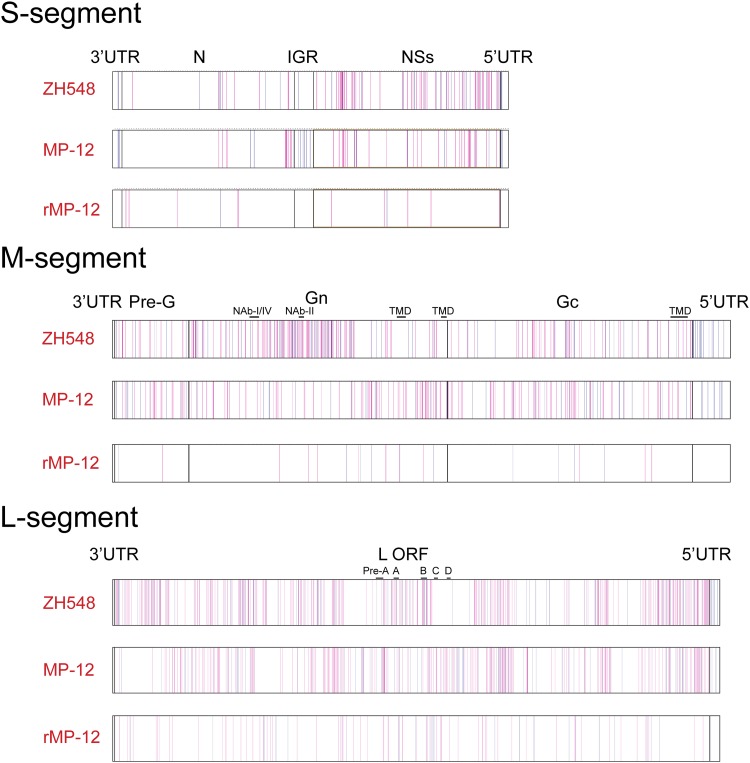
To better understand the distribution of mutations, we plotted each mutation found in each PCR fragment into the genome schematics of the S, M, and L segments (Fig. 4). The mutation represents the sequence different from the consensus sequence of MP-12 or ZH548 (see Materials and Methods). We found that the ZH548 M segment contained frequent mutations in the Gn ectodomain region. Although the Gn ectodomain of ZH548 encodes mutations at a high frequency, each ZH548 subpopulation encoded only a few amino acid substitutions in reported neutralizing epitope I, II, or IV (2, 17) (data not shown). On the other hand, MP-12 lacked such frequent mutations in the Gn ectodomain region (Fig. 4; see Fig. S1 in the supplemental material). These results suggest that ZH548 has viral subpopulations encoding mutations in the Gn ectodomain due to the selection pressure of host immune responses, while MP-12 lacks such populations due to the history of serial plaque purification and passages in MRC-5 cells. We also noted that both MP-12 and ZH548 contained a number of mutations in the NSs ORF, whereas they had low numbers of mutations in the N ORF (Fig. 4; see Fig. S1 in the supplemental material). This result suggests that viral subpopulations encoding mutations in the N gene were not favorably selected during viral replication, while those encoding mutations in the NSs gene could survive the selection. The rMP-12 genetic subpopulations had a much smaller number of mutations than those of MP-12 or ZH548 (Fig. 4; see Fig. S1 in the supplemental material). This indicates that recombinant RVFV recovered from plasmids contains only a minimum number of viral subpopulations. Although rMP-12 was amplified in VeroE6 cells once, it is not likely that VeroE6 cells support the genetic stability of MP-12 better than MRC-5 cells. Considering that the MP-12 vaccine strain has been passaged from the original MP-12 plaque 4 times at a low MOI in MRC-5 cells (Table 1) and the genetic diversity was comparable to that of ZH548, a lack of genetic diversity of rMP-12 is probably due to just one passage in VeroE6 cells of rMP-12 recovered from plasmid DNA.
Fig 4.
Distribution of mutations in RVFV subpopulations. Locations of silent mutations (blue) or amino acid substitutions (red) are shown as lines on schematics of the S, M, and L segments of ZH548, MP-12, and rMP-12. UTR, untranslated region; IGR, intergenic region; NAb-I/IV or NAb-II, neutralizing antibody epitopes (17); TMD, transmembrane domain; Pre-A, A, B, C, and D, polymerase motifs of RNA-dependent RNA polymerase.
MP-12 subpopulations do not contain ZH548 sequences at 23 consensus mutation sites.
MP-12 encodes 23 mutations compared to the sequence of the parental ZH548 strain: 4 in the S segment (1 amino acid change), 9 in the M segment (5 amino acid changes), and 10 in the L segment (3 amino acid changes). We evaluated whether the MP-12 vaccine contains genetic subpopulations encoding the ZH548 sequence at the 23 mutation sites. As shown in Table 2, we did not find any genetic subpopulations encoding ZH548 sequence at the 23 mutation sites. However, the codons encoding U795C (Gn), C4368U (L), or A5208G (L) were affected in some subpopulations, and these changes resulted in amino acid substitutions. Although the significance of those amino acid substitutions is unclear, the result suggests that MP-12 does not encode the ZH548 sequence in the consensus 23 mutation sites. Thus, the MP-12 vaccine manufactured by using certified MRC-5 is genetically stable.
TABLE 2.
Subpopulation analysis of 23 MP-12 consensus mutations
| Segment | Location | MP-12 mutationa |
Location at which mutation was observedb | Other ZH548 mutation observed in MP-12 populationc | MP-12 mutation observed |
|||
|---|---|---|---|---|---|---|---|---|
| Nucleotide (antiviral) | Nucleotide (viral) | Amino acid | ZH548 population | Other wt RVFV | ||||
| S | Intergenic region | G829A | C862U | <MP4j | − | − | ||
| NSs | A1178G | U513C | V160A | MP4 | − | − | ||
| NSs | A1288G | U403C | >MP8 | − | − | |||
| NSs | A1483G | U208C | MP3 | − | − | |||
| M | 78-kDa protein | U46C | A3840G | I9T | +d | − | ||
| 78-kDa protein | G69A | C3817U | V17I | +d | − | |||
| Gn | U795C | A3091G | Y259H | H259L | − | − | ||
| Gn | G857A | C3029U | − | +f | ||||
| Gc | A2259U | U1627A | I747L | +e | − | |||
| Gc | A3564G | U322C | R1182G | − | − | |||
| 5′ UTR | A3621G | U265C | + | +g | ||||
| 5′ UTR | A3644G | U242C | − | +h | ||||
| 5′ UTR | A3660U | U226A | − | − | ||||
| L | L | C351U | G6054A | − | − | |||
| L | U507C | A5898G | >MP8 | − | − | |||
| L | U533C | A5872G | V172A | MP3 | − | − | ||
| L | G2130A | C4275U | − | − | ||||
| L | G2925A | C3480U | − | − | ||||
| L | G3104A | C3301U | R1029K | − | − | |||
| L | A3198G | U3207C | − | − | ||||
| L | G3750A | C2655U | M1244I | MP3 | − | − | ||
| L | C4368U | G2037A | Y1450C | + | +i | |||
| L | A5208G | U1197C | G1730A | + | − | |||
Nucleotide mutations in antiviral and viral sense sequences and amino acid mutations in MP-12 sequence compared to parental strain ZH548 sequence.
Data from Vialat et al. (34).
Other amino acid substitution observed in the codon encoding the MP-12 mutation.
Mutations were located on the same PCR fragment.
Sixty-three percent of the ZH548 subpopulations encoded this sequence.
Strain 1853/78.
Strains 2269/74 and 73HB1230.
Strains Ken83, ARD-38388, and 2250/74.
Strain 2373/74.
ZH548 subpopulations contain 6 of 23 MP-12 mutations.
The occurrence of mutations during the passage of ZH548 in 5-fluorouracil was analyzed by Vialat et al., and mutations introduced at the later stage of passage were identified in the S and L segments (34) (Table 2). We hypothesized that the ZH548 subpopulation shares some of the MP-12-specific mutations. Since we know that the original plaque isolate of ZH548 has a virulent phenotype, such mutations are not responsible for the attenuation of MP-12 (6). We analyzed the subpopulations of strain ZH548 to find any of the 23 MP-12 mutations. As a result, 2 amino acid changes in the 78-kDa protein (I9T and V17I) on the same PCR fragment of the ZH548 subpopulations were identified, while 1 amino acid change in Gc (I747L) was found in 63% of the ZH548 subpopulations (Table 2). In addition, 1 silent mutation in the 5′ untranslated region (UTR) of the M segment and 2 silent mutations in the L-segment ORF were found in ZH548 subpopulations. Caplen et al. showed that ZH548 was gradually attenuated during passages in MRC-5 cells (6). Thus, our results suggest that the initial plaque purification picked the ZH548 subpopulation containing those six mutations and that those mutations are not responsible for the attenuation. In addition, we compared those 23 MP-12 mutations with other available full-genome sequences available as of 2012. As a result, G857A in Gn, A3621G and A3644G in the M-segment 5′ UTR, and C4368U in the L-segment ORF were found in other wt RVFV consensus sequences (Table 2). Thus, it is possible that those mutations are not responsible for the attenuation of MP-12. To identify the mutations responsible for MP-12 attenuation, recombinant ZH501 encoding each MP-12 mutation has been recovered, and a study to test the virulence of each mutant in mice is currently in progress.
The MP-12 subpopulation is distinct from other Egyptian wt RVFV strains.
We also analyzed the nucleotide substitution pattern among genetic subpopulations of MP-12, ZH548, and rMP-12. The MP-12 subpopulations contain more A-to-G or U-to-G mutations than G-to-A or C-to-U mutations in the S, M, and L segments (data not shown). On the other hand, ZH548 encoded more G-to-A or C-to-U mutations than A-to-G or U-to-G mutations in the S, M, and L segments (data not shown). rMP-12 did not show a consistent pattern of nucleotide substitutions in the S, M, and L segments (data not shown). These results indicate that the MP-12 vaccine strain contains subpopulations with frequent A-to-G or U-to-G mutations in all segments which are distinct from ZH548 or rMP-12 subpopulations. Those A-to-G or U-to-C substitutions might be increased during continuous passages of MP-12 vaccine in MRC-5 cells. Adenosine deaminase acting on RNA (ADAR) catalyzes the C-6 deamination of A to I in dsRNA (1, 18). A-to-I editing results in an A-to-G mutation (or a U-to-C mutation in the complementary sense RNA) by replacing I with G. The nucleotide substitution pattern unique to MP-12 suggests that MP-12 has genetic populations distinct from wt strain ZH548.
RVFV wild-type strains ZH548, ZH501, and ZH1776 were isolated from human RVF patients in Zagazig Hospital during the 1977-1978 RVFV outbreak in Egypt (24), while strain ZS6365 was isolated from sheep during the same outbreak (10). The ZH548 strain encodes several mutations compared to the sequences of the other Egyptian strains. To identify the differences in viral subpopulations between MP-12 and ZH548, we compared the consensus sequences among 4 Egyptian RVFV strains (ZH548, ZH501, ZH1776, and ZS6365) and analyzed whether the subpopulations of ZH548 or MP-12 encode the mutations shared by those strains (Table 3). We found 8 mutations in the S segment, 12 mutations in the M segment, and 21 mutations in the L segment. Among those mutations, 2 mutations (nt 369 and 461) in the S segment, 1 mutation (nt 715) in the M segment, and 6 mutations (nt 822, 1057, 1427, 3768, 5406, and 6303) in the L segment were unique to ZH548. Interestingly, ZH548 subpopulations encoded the mutations in the S segment at nt 369 and 461, the M segment at nt 715, and the L segment at nt 1427, 3768, and 6303. Also, ZH548 subpopulations encoded U at nt 716 in the S segment, which is unique to ZH501. These results suggest that ZH548 is derived from the same origin as ZH501, ZH1766, and ZS6365 and several mutations became dominant in the viral populations. Interestingly, MP-12 subpopulations did not contain those mutations, confirming that MP-12 is derived from a single plaque of a ZH548 subpopulation, and the subpopulations were generated during MRC-5 cell passages.
TABLE 3.
Comparison of ZH548 and MP-12 subpopulations with other Egyptian strains
| Segment | Location | Nucleotide position at antiviral sense sequence | Nucleotide |
|||||
|---|---|---|---|---|---|---|---|---|
| Egyptian RVFV strains |
ZH548 subpopulation | MP-12 subpopulation | ||||||
| ZH548 | ZH501 | ZH1776 | ZS6365 | |||||
| S | N | 77 | U | —a | C | — | — | — |
| N | 369 | U | C | C | C | C | — | |
| N | 420 | G (Ile)b | — | A (Val) | — | — | — | |
| N | 461 | G | A | A | A | A | — | |
| N | 599 | A | G | — | G | — | — | |
| N | 716 | C | U | — | — | U | — | |
| NSs | 1208 | U (Lys) | — | C (Arg) | C | — | — | |
| NSs | 1570 | G | — | A | — | — | — | |
| M | Gn | 715 | U (Leu) | A (Gln) | A (Gln) | A (Gln) | A (Gln) (57%) | |
| Gn | 1439 | C | — | U | — | — | — | |
| Gn | 1717 | A (Asp) | — | — | G (Gly) | — | — | |
| Gn | 1824 | A (Ile) | G (Val) | — | — | — | — | |
| Gc | 2234 | G | — | — | A | — | — | |
| Gc | 2324 | C | — | U | U | — | — | |
| Gc | 2711 | U | C | — | — | — | — | |
| Gc | 2981 | C (Asp) | U (Asp) | — | — | — | A (Glu) | |
| Gc | 3017 | U | — | — | C | — | — | |
| Gc | 3545 | C | — | U | U | — | — | |
| 5′ UTR | 3655 | U | C | — | — | — | — | |
| 5′ UTR | 3678 | A | G | — | — | — | — | |
| L | L | 822 | A | C | C | C | — | — |
| L | 1057 | C | U | U | U | — | — | |
| L | 1173 | C | U | — | — | — | — | |
| L | 1427 | G (Ser) | A (Asn) | A (Asn) | A (Asn) | A (Asn) | — | |
| L | 1496 | G (Arg) | — | — | A (Lys) | — | — | |
| L | 1560 | C | — | U | — | — | — | |
| L | 2370 | G | — | A | — | — | — | |
| L | 3385 | A (Ser) | G (Gly) | — | — | — | — | |
| L | 3768 | U | C | C | C | C | — | |
| L | 4019 | C (Thr) | — | U (Ile) | — | — | — | |
| L | 4305 | A | — | — | G | — | — | |
| L | 4413 | C | U | — | — | — | — | |
| L | 5172 | A (Gln) | — | — | G (Gln) | C (His) | — | |
| L | 5238 | A | — | G | — | — | — | |
| L | 5286 | G | — | — | A | — | — | |
| L | 5406 | G | A | A | A | — | — | |
| L | 5495 | C (Ser) | — | U (Leu) | U (Leu) | — | — | |
| L | 5783 | A (Lys) | G (Arg) | — | — | — | — | |
| L | 6207 | C | — | U | — | — | — | |
| L | 6250 | C | — | U | U | — | — | |
| 5′ UTR | 6303 | G | A | A | A | A | — | |
—, sequence identical to that of ZH548.
Amino acids in parentheses indicate the amino acid encoded by the corresponding codon. A lack of amino acids in parentheses indicates no amino acid substitution.
In summary, the MP-12 vaccine strain is genetically stable after the manufacturing process in MRC-5 cells, whereas 6 of 23 mutations in MP-12 were derived from parental ZH548 subpopulations. Further modification of the MP-12 vaccine by using reverse genetics may be required to incorporate a nonreversible attenuation mutation(s) and a marker for differentiating infected from vaccinated animals (DIVA). Information obtained in this study will be useful for development of modified MP-12 vaccines in MRC-5 cells or other cell substrates.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by grant R01 AI08764301-A1 (NIH/NIAID) and funding from the Sealy Center for Vaccine Development at UTMB.
Footnotes
Published ahead of print 3 October 2012
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1. Bass BL. 2002. RNA editing by adenosine deaminases that act on RNA. Annu. Rev. Biochem. 71:817–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Battles JK, Dalrymple JM. 1988. Genetic variation among geographic isolates of Rift Valley fever virus. Am. J. Trop. Med. Hyg. 39:617–631 [DOI] [PubMed] [Google Scholar]
- 3. Billecocq A, et al. 2008. RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology 378:377–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bird BH, Khristova ML, Rollin PE, Ksiazek TG, Nichol ST. 2007. Complete genome analysis of 33 ecologically and biologically diverse Rift Valley fever virus strains reveals widespread virus movement and low genetic diversity due to recent common ancestry. J. Virol. 81:2805–2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. 2009. Rift Valley fever virus. J. Am. Vet. Med. Assoc. 234:883–893 [DOI] [PubMed] [Google Scholar]
- 6. Caplen H, Peters CJ, Bishop DH. 1985. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J. Gen. Virol. 66:2271–2277 [DOI] [PubMed] [Google Scholar]
- 7. Crabtree MB, et al. 2012. Infection and transmission of Rift Valley fever viruses lacking the NSs and/or NSm genes in mosquitoes: potential role for NSm in mosquito infection. PLoS Negl. Trop. Dis. 6:e1639 doi:10.1371/journal.pntd.0001639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Daubney R, Hudson JR. 1931. Enzootic hepatitis or Rift Valley fever: an undescribed virus disease of sheep cattle and man from east Africa. J. Pathol. Bacteriol. 34:545–579 [Google Scholar]
- 9. Engdahl C, Naslund J, Lindgren L, Ahlm C, Bucht G. 2012. The Rift Valley fever virus protein NSm and putative cellular protein interactions. Virol. J. 9:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grobbelaar AA, et al. 2011. Molecular epidemiology of Rift Valley fever virus. Emerg. Infect. Dis. 17:2270–2276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ikegami T, Makino S. 2011. The pathogenesis of Rift Valley fever. Viruses 3:493–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ikegami T, Makino S. 2009. Rift Valley fever vaccines. Vaccine 27(Suppl 4):D69–D72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ikegami T, et al. 2009. Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog. 5:e1000287 doi:10.1371/journal.ppat.1000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ikegami T, Won S, Peters CJ, Makino S. 2006. Rescue of infectious Rift Valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J. Virol. 80:2933–2940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ito N, et al. 2003. Improved recovery of rabies virus from cloned cDNA using a vaccinia virus-free reverse genetics system. Microbiol. Immunol. 47:613–617 [DOI] [PubMed] [Google Scholar]
- 16. Kark JD, Aynor Y, Peters CJ. 1985. A Rift Valley fever vaccine trial. 2. Serological response to booster doses with a comparison of intradermal versus subcutaneous injection. Vaccine 3:117–122 [DOI] [PubMed] [Google Scholar]
- 17. Keegan K, Collett MS. 1986. Use of bacterial expression cloning to define the amino acid sequences of antigenic determinants on the G2 glycoprotein of Rift Valley fever virus. J. Virol. 58:263–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keegan LP, Leroy A, Sproul D, O'Connell MA. 2004. Adenosine deaminases acting on RNA (ADARs): RNA-editing enzymes. Genome Biol. 5:209 doi:10.1186/gb-2004-5-2-209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Le May N, et al. 2004. TFIIH transcription factor, a target for the Rift Valley hemorrhagic fever virus. Cell 116:541–550 [DOI] [PubMed] [Google Scholar]
- 20. Le May N, et al. 2008. A SAP30 complex inhibits IFN-beta expression in Rift Valley fever virus infected cells. PLoS Pathog. 4:e13 doi:10.1371/journal.ppat.0040013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Linthicum KJ, Davies FG, Kairo A, Bailey CL. 1985. Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J. Hyg. (Lond.) 95:197–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mandell RB, Flick R. 2011. Rift Valley fever virus: a real bioterror threat. J. Bioterror. Biodef. 2:108 doi:10.4172/2157-2526.1000108 [Google Scholar]
- 23. Mandell RB, Flick R. 2010. Rift Valley fever virus: an unrecognized emerging threat? Hum. Vaccin. 6:597–601 [DOI] [PubMed] [Google Scholar]
- 24. Meegan JM. 1979. The Rift Valley fever epizootic in Egypt 1977-78. 1. Description of the epizootic and virological studies. Trans. R. Soc. Trop. Med. Hyg. 73:618–623 [DOI] [PubMed] [Google Scholar]
- 25. Morrill JC, et al. 1991. Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine 9:35–41 [DOI] [PubMed] [Google Scholar]
- 26. Morrill JC, et al. 1987. Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am. J. Vet. Res. 48:1042–1047 [PubMed] [Google Scholar]
- 27. Morrill JC, Mebus CA, Peters CJ. 1997. Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am. J. Vet. Res. 58:1104–1109 [PubMed] [Google Scholar]
- 28. Morrill JC, Mebus CA, Peters CJ. 1997. Safety of a mutagen-attenuated Rift Valley fever virus vaccine in fetal and neonatal bovids. Am. J. Vet. Res. 58:1110–1114 [PubMed] [Google Scholar]
- 29. Pepin M, Bouloy M, Bird BH, Kemp A, Paweska J. 2010. Rift Valley fever virus (Bunyaviridae: Phlebovirus): an update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet. Res. 41:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pittman PR, et al. 1999. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: a 12-year experience. Vaccine 18:181–189 [DOI] [PubMed] [Google Scholar]
- 31. Saluzzo JF, Smith JF. 1990. Use of reassortant viruses to map attenuating and temperature-sensitive mutations of the Rift Valley fever virus MP-12 vaccine. Vaccine 8:369–375 [DOI] [PubMed] [Google Scholar]
- 32. Schmaljohn C, Nichol ST. 2007. Bunyaviridae, p 1741–1789 In Knipe DM, et al. (ed), Fields virology, 5th ed Lippincott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 33. Swanepoel R, Coetzer JAW. 2004. Rift Valley fever, p 1037–1070 In Coetzer JAW, et al. (ed), Infectious diseases of livestock with special reference to southern Africa, 2nd ed Oxford University Press, Cape Town, South Africa [Google Scholar]
- 34. Vialat P, Muller R, Vu TH, Prehaud C, Bouloy M. 1997. Mapping of the mutations present in the genome of the Rift Valley fever virus attenuated MP12 strain and their putative role in attenuation. Virus Res. 52:43–50 [DOI] [PubMed] [Google Scholar]
- 35. Won S, Ikegami T, Peters CJ, Makino S. 2007. NSm protein of Rift Valley fever virus suppresses virus-induced apoptosis. J. Virol. 81:13335–13345 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.