Abstract
The orthopoxvirus (OPV) vaccinia virus (VACV) requires an intact F13L gene to produce enveloped virions (EV) and to form plaques in cell monolayers. Simultaneous introduction of an exogenous gene and F13L into F13L-deficient VACV results in expression of the foreign gene and restoration of plaque size. This is used as a method to rapidly generate VACV recombinants without the need for drug selection. However, whether other OPVs require the orthologs of F13L to generate EV and form plaques, whether F13L orthologs and EV are important for OPV pathogenesis in natural hosts, and whether a system based on F13L ortholog deficiency can be used to generate recombinant OPVs other than VACV have not been reported. The F13L ortholog in ectromelia virus (ECTV), the agent of mousepox, is EVM036. We show that ECTV lacking EVM036 formed small plaques and was highly attenuated in vivo but still induced strong antibody responses. Reintroduction of EVM036 in tandem with the DsRed gene resulted in a virus that expressed DsRed in infected cells but was indistinguishable from wild-type ECTV in terms of plaque size and in vivo virulence. Thus, our data show that, like F13L in VACV, EVM036 is required for ECTV plaque formation and that EVM036 and EV are important for ECTV virulence. Our experiments also suggest that OPVs deficient in F13L orthologs could serve as safer anti-OPV vaccines. Further, our results demonstrate that ECTV deficient in EVM036 can be exploited for the rapid generation of fully virulent ECTV expressing foreign genes of interest.
INTRODUCTION
Orthopoxviruses (OPVs) form two types of infectious particles. The intracellular mature virion (MV) consists of a core surrounded by a single-membrane bilayer. MVs are released to the extracellular milieu only after cell lysis, are the principal component of OPV viral stocks, and are thought to be important for the initial infection of a host. While most MVs remain within the cytosol, some are wrapped by a double trans-Golgi or early-endosome membrane, transported to the plasma membrane through microtubules, and exocytosed, losing the outer envelope in the process. Some of the resulting enveloped virions (EV) remain attached to the plasma membrane as cell-associated enveloped virions (CEVs), while others are released as extracellular enveloped virions (EEVs). EVs are required for the formation of plaques and dissemination within the host (26, 29). The F13L gene of VACV encodes vp37, a highly conserved protein in all OPVs that is essential for the envelopment of MVs to form EVs. Hence, VACV deficient in F13L (VACV-ΔF13L) is characterized by small plaques and slow growth in tissue culture (1). Recently, it has been shown that VACV-ΔF13L is highly attenuated in immunocompetent and in severe combined immunodeficient (SCID) mice challenged intranasally, intracutaneously (i.c.), or intravenously (i.v.) (16, 31). While these experiments suggest that F13L and EV are important for the pathogenesis of OPVs, a caveat is that VACV is not a natural pathogen of the mouse. Further indications of the importance of vp37 in the biology of OPVs come from studies using ST-246, a drug that prevents EV formation by specifically targeting vp37 (33). It has been shown that ST-246 prevents EV formation for several OPVs, including VACV, variola virus (VARV), cowpox virus (CPXV), camelpox virus, and ectromelia virus (ECTV) (33). Furthermore, ST-246 can be used for the early treatment of multiple animal species from various OPV infections, including mice with VACV, CPXV, and ECTV, rabbits with rabbitpox, and monkeys with MPXV and VARV (19). However, the role of vp37 orthologs in determining the size of OPV plaques other than VACV and their role in the virulence of OPVs in their natural hosts have not been confirmed using genetic approaches.
From a practical point of view, homologous recombination to reintroduce F13L together with a gene of interest into F13L-deficient VACV and screening for large plaques can be used for the rapid and efficient generation of recombinant VACV (2, 5, 14, 21). A similar approach has also been used to generate recombinant modified vaccinia Ankara (MVA) VACV (27, 28). However, a comparable system has not been exploited for any other species of OPV. An analogous method for the generation of fully virulent recombinant ECTV would be of interest for those in the field.
In ECTV vp37 differs from the VACV protein in just one amino acid (197 I→V). Here we used homologous recombination and a triple-selection scheme to generate ECTV (Moscow strain) deficient in EVM036, the F13L ortholog in ECTV. We found that, like VACV-ΔF13L, ECTV deficient in EVM036 (ECTV-Δ036) produced small plaques. In addition, ECTV-Δ036 was highly attenuated in vivo but induced a protective immune response in mousepox-susceptible mice. On the other hand, introduction of EVM036 together with an exogenous gene coding for the red fluorescent protein DsRed into ECTV-Δ036 resulted in a virus (ECTV-DsRed) that formed red fluorescent plaques of wild-type (WT) size. Moreover, ECTV-DsRed was similar to ECTV-WT in terms of growth in tissue culture and in vivo virulence.
MATERIALS AND METHODS
Viruses.
Virus stocks were produced and their growth and titers were determined as previously described (10, 11, 13, 32).
Mice and infections.
The Fox Chase Cancer Center Institutional Animal Care and Use Committee approved the experimental protocols involving animals. BALB/c and C57BL/6 (B6) mice were purchased from Taconic when they were 8 to 10 weeks of age and rested at least a week before use. Unless otherwise indicated, mice were infected with ECTV in the left footpad with 30 μl phosphate-buffered saline (PBS) containing 3 × 103 PFU or infected intraperitoneally (i.p.) with various numbers of PFU in 500 μl PBS. Following infection, mice were observed daily for signs of disease (lethargy, ruffled hair, weight loss, skin rash, and eye secretions) and imminent death (unresponsiveness to touch, lack of voluntary movements).
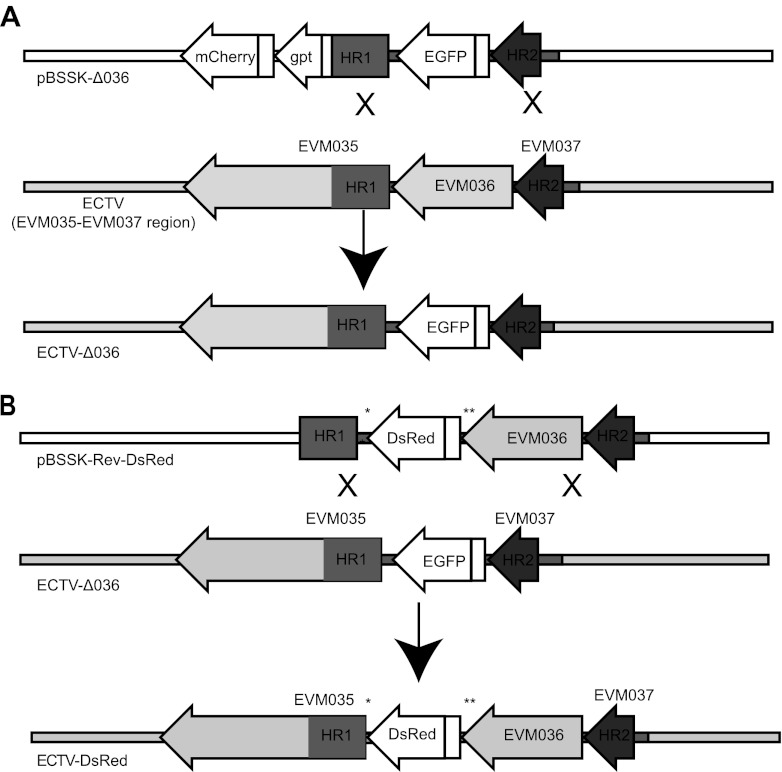
Generation of ECTV-Δ036 (Fig. 1A).
Fig 1.
Generation of ECTV-Δ036 and ECTV-DsRed using ECTV-Δ036 as a backbone. (A) Schematic representation of the ECTV region comprising EVM035 to EVM037, the plasmid pBSSK-Δ036 (used to induce the deletion of EVM036), and the resulting mutant virus ECTV-Δ036. (B) Schematic representation of the ECTV-Δ036 region comprising EVM035 to EVM037, the plasmid pBSSK-RevΔ036-DsRed (used to reintroduce EVM036 together with DsRed into ECTV-Δ036), and the resulting recombinant virus ECTV-DsRed. ECTV sequences are in gray, with a darker shade used for sequences involved in the homologous recombination (HR1 and HR2). Non-ECTV sequences are in white. **, region of EVM036 with synonymous mutations; *, the last 43 bp of EVM036 that were added as part of the EVM035 promoter.
ECTV Moscow DNA fragments comprising base pairs 46055 to 46581 (5′ to 3′) (homologous recombination 1 [HR1]) and 47749 to 48106 (HR2) according to the published sequence (4) were amplified by PCR and subcloned into plasmid pBluescript II SK− (pBSSK; Stratagene). Between HR1 and HR2 we placed the gene for enhanced green fluorescence protein (EGFP) under the control of the strong early/late 7.5 promoter. 5′ of HR1 we inserted the genes for the red fluorescent protein mCherry driven by the 7.5 promoter and the Escherichia coli gene gpt driven by the moderate-strength synthetic early/late elP1 promoter (17), both in reverse orientation. We named this plasmid pBSSK-Δ036. The gpt gene encodes xanthine guanine phosphoribosyl transferase, which allows viral replication to proceed in the presence of 25 μg/ml mycophenolic acid, 250 μg/ml xanthine, and 15 μg/ml hypoxanthine (MXH) (9). To generate ECTV-Δ036, pBSSK-Δ036 was transfected into B-SC-1 using Lipofectamine 2000 (Invitrogen) as directed by the manufacturer, and 4 h later the cells were infected with 0.01 PFU/cell ECTV-WT (ECTV Moscow strain, ATCC VR-1374). The cells were cultured until most of them appeared infected by cytopathic effect and displayed green/red fluorescence. The transfected/infected cultures were lysed by three cycles of freezing and thawing, and various dilutions were used to infect B-SC-1 cells in the presence of MXH to favor single-crossover events. Doubly (green/red) fluorescent plaques of wild-type size were collected and freeze-thawed three times, and the lysates were used to infect new cells in the presence of MXH. This process was iterated three times until all the plaques in the culture were green/red fluorescent. Next, the monolayers were infected in the absence of MXH, and small green (non-red) plaques were collected. After 13 cycles, all the plaques in a well were green fluorescent and small. We used the lysates of the selected plaques as templates and primers with the ECTV sequences 50258 to 50285 (5′ to 3′) and 50979 to 50953 in a PCR. The amplicon was sequenced, and the correct insertion of EGFP was confirmed. A clone with the correct insertion was amplified and named ECTV-Δ036.
Generation of ECTV-DsRed using ECTV-Δ036 as the backbone (Fig. 1B).
We first generated a plasmid, pBSSK-RevΔ036-MCS, in which a DNA fragment comprising EVM036 with 12 synonymous mutations in the last 43 bp (GAGAGATTGGGTATCTAGCCACAGTAAATCGTTGAAAATTTAA → CGTGACTGGGTCTCCAGTCACTCTAAAAGCTTGAAGATTTAA) and a multiple cloning site and the last 43 bp of EVM036 was placed between HR1 and HR2. We included the last 43 bp of EVM036 immediately after DsRed because they may be part of the EVM35 promoter. The synonymous mutations in EVM036 were to prevent recombination between identical repeats. To generate pBSSK-RevΔ036-MCS, we used three PCRs. The first two reactions, performed in parallel, used ECTV Mos DNA as the template. For the first PCR, we used the forward primer FP:49054–49082 (ttaatcccgggctgcagCCTATATGCCCTATTATCATACTGTCGAC; lowercase letters represent non-ECTV nucleotides [the PstI site is underlined], and uppercase letters represent ECTV nucleotides 49054 to 49082). The reverse primer was RP:49962–49578 (tgctagcggatccgcggccgcctcgagTATTTGAGAGAGATTGGGTATCTAGCCACAGTAAATCGTTGAAAATTTAAAAATAGAAAATAGAGACGTATAGAACACCATCATG; lowercase letters are non-ECTV nucleotides with multiple restriction sites, and uppercase letters represent ECTV sequence from nucleotide 49962 to 49578). The second PCR used the forward primer FP:49613-59mut (gccgcggatccgctagcacgcgtaagagctcggtaccTTAAATCTTCAAGCTTTTAGAGTGACTGGAGACCCAGTCACGTTCAA; lowercase letters represent non-ECTV sequences with several restriction sites, uppercase letters represent ECTV nucleotides 49613 to 49659, and boldface indicates synonymous mutations). The reverse primer was RP:51101–51077 (ttatatcgatgatatcGTGTTGTCTAACGTATTGGACATGCTTAT; lowercase indicates non-ECTV sequences, underlining indicates an EcoRV site, and uppercase represents ECTV sequences 51101 to 51077). The amplicons of the two PCRs were mixed, and a new PCR was performed using FP:49054–49082 and RP:51101–51077. The resulting amplicon was cloned into plasmid pBSSK− using EcoRV and PstI restriction enzymes to give the final product pBSSK-RevΔ036-MCS, which can be used to introduce any gene into ECTV. To specifically introduce DsRed, pBSSK-RevΔ036-MCS was digested with NheI, and a PCR amplicon comprising the sequences of the 7.5 promoter and DsRed was cloned using the In-Fusion PCR cloning system (Clontech) to generate the targeting vector pBSSK-RevΔ036-DsRed.
To generate ECTV-DsRed, B-SC-1 cells were transfected in six-well plates with pBSSK-RevΔ036-DsRed and infected with 0.1 PFU/cell ECTV-Δ036. When complete cytopathic effect was observed, the cells were collected, the viruses were released by three cycles of freeze-thawing, and 10-fold dilutions of the lysates were used to infect B-SC-1 cells in six-well plates. Large nonfluorescent plaques were selected. The process was iterated three times to yield pure large plaques. The resulting virus was amplified and named ECTV-DsRed. Correct insertion of DsRed was determined by PCR, as described above.
In vitro growth curves.
To measure single-step virus growth, monolayers of B-SC-1 cells were infected with ECTV-Δ036 or ECTV-DsRed at 5 PFU/cell. At various times, the cells and supernatants were collected and freeze-thawed three times, and various dilutions of the resulting lysates were used in duplicate to infect new monolayers of B-SC-1 cells in 12-well plates. Titers in the lysates were determined as previously. To determine multistep growth, the procedure was identical except that the B-SC-1 monolayers were infected with 0.01 PFU/cell of ECTV-Δ036 or ECTV-DsRed.
ELISA.
We determine antibodies to ECTV in sera using an enzyme-linked immunosorbent assay (ELISA) with recombinant EVM135 protein (the ortholog of VACV A33R) as previously described (12). Briefly, 96-well flat-bottom radioimmunoassay/enzyme immunoassay plates (Corning) were coated with 100 ng of recombinant EVM135/A33R in 0.1 ml PBS at 4°C overnight. Plates were blocked for 2 h at 37°C with PBS containing 2% bovine serum albumin (BSA). Mouse sera were serially diluted in PBS containing 0.5% BSA and 0.05% Tween 20, and 0.1 ml was added to each well. The plates were incubated for 1 h at 37°C and washed three times with PBST (PBS with 0.05% Tween 20). Peroxidase-conjugated affinity-purified goat anti-mouse IgG (0.1 ml; γ chain specific; KPL Inc.) was added to each well diluted 1:2,000 in PBST, and wells were incubated for 0.5 h at 37°C and washed five times with PBST. Sure-Blue TMB 1-component microwell peroxidase substrate (50 μl; KPL Inc.) was added to each well, and the reaction was stopped by the addition of 0.1 ml of 0.12 M HCl. The optical density at 450 nm was determined using a microplate spectrophotometer (μQuant; Bio-Tec).
Statistical analysis.
We used the log-rank (Mantel-Cox) survival test, the two-tailed t test for two samples, or the nonparametric Mann-Whitney test as applicable using Prism software. All experiments to characterize the viruses were repeated a minimum of two times.
RESULTS
Generation of ECTV-Δ036 and ECTV-DsRed.
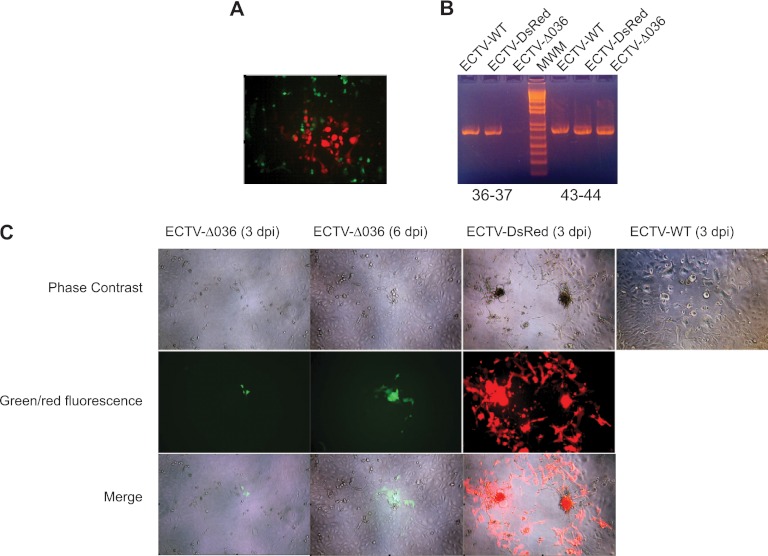
We generated ECTV-Δ036 by homologous recombination using plasmid pBSSK-Δ036 as the targeting vector and ECTV Moscow as the backbone. Because we expected that ECTV deficient in EVM036 would form small plaques and be overgrown by WT virus (1), we developed a method of triple selection (EGFP, mCherry, and gpt) (Fig. 1A) which is described in detail in Materials and Methods. We generated ECTV-DsRed from ECTV-Δ036, using homologous recombination and plasmid pBSSK-RevΔ036-DsRed (Fig. 1B), which is also described in Materials and Methods. Two days after the lysate of the transfection/infection was plated, some red plaques could be easily distinguished by fluorescence microscopy indicating successful recombination (Fig. 2A). Plaques were collected at 3 days postinfection (dpi). At the next cycle, only red plaques were visible, and selection was stopped at the third cycle. To verify the deletion of EVM036 in ECTV-Δ036 and its reinsertion in ECTV-DsRed, we performed PCR on lysates of cells infected with different viruses using the 5′-3′ primers ECTV:50258–50285 and ECTV:50979–50953 to amplify the junction between EVM036 and EVM037. The expected amplicon was found in lysates of cells infected with ECTV WT and ECTV-DsRed but not of those infected with EVM-Δ036. On the other side, primers designed to amplify the junction of EVM043 and EVM044 amplified similar fragments with the three viruses (Fig. 2B). Figure 2C shows microphotographs with phase contrast, green or red fluorescence, and merged images to highlight the different phenotypes of the plaques produced by ECTV-Δ036 and ECTV-DsRed on B-SC-1 cells. At 3 and 6 dpi, ECTV-Δ036 formed plaques that were not visible by phase contrast but could be distinguished as two or three green fluorescent cells. Conversely, a plaque formed by ECTV-DsRed at 3 dpi was easy to identify by phase contrast and was composed of many red fluorescent cells. An ECTV-WT plaque with phase contrast is also shown for comparison. Note that the microphotographs with ECTV-WT and ECTV-DsRed at 6 dpi are not shown because at this time the monolayers were destroyed.
Fig 2.
Identification of ECTV-Δ036 and ECTV-DsRed. (A) Microphotograph showing a red ECTV-DsRed plaque within ECTV-Δ036 (green)-infected cells 2 days after infection of B-SC-1 cells with a lysate of B-SC-1 cells infected with ECTV-Δ036 and transfected with pBSSK-RevΔ036-DsRed. (B) PCR analysis of lysates of the indicated viruses using primers to amplify the junction of EVM036 and EVM037 or the junction of EVM43 and EVM44. (C) Monolayer of B-SC-1 cells infected with the indicated viruses and visualized by microscopy on the indicated day postinfection.
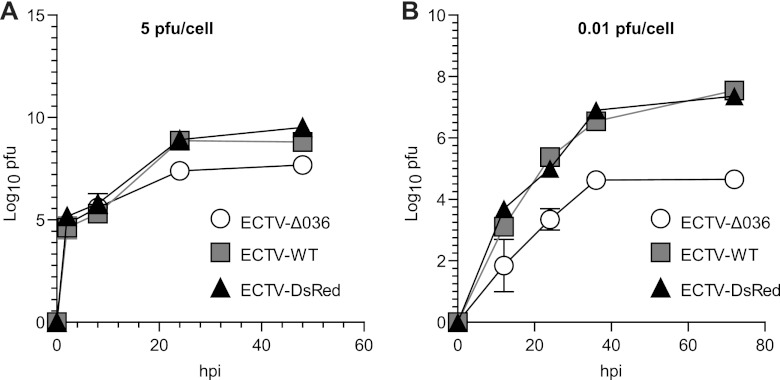
ECTV-Δ036 but not ECTV-DsRed grows poorly in tissue culture.
We next characterized the viruses for their ability to replicate in tissue culture. B-SC-1 cells were infected with ECTV-WT, ECTV-Δ036, and ECTV-DsRed with 5 PFU/cell to measure single-step growth (Fig. 3A) or 0.01 PFU/cell to measure multistep growth (Fig. 3B). At 5 PFU/cell, the three viruses produced similar numbers of infectious particles during the first 12 h of infection. At 0.01 PFU/cell, ECTV-WT and -DsRed produced similar amounts of infectious virus that were significantly higher than the amounts produced by ECTV-Δ036 at every time point. These data demonstrate that ECTV-Δ036 is defective in cell-to-cell spread but not in its ability to generate MVs.
Fig 3.
ECTV-Δ036 but not ECTV-DsRed grows poorly in tissue culture. B-SC-1 cells were infected with 5 (A) or 0.01 (B) PFU/cell of the indicated viruses. Amounts of cell-associated and free virus were determined at the indicated times after infection.
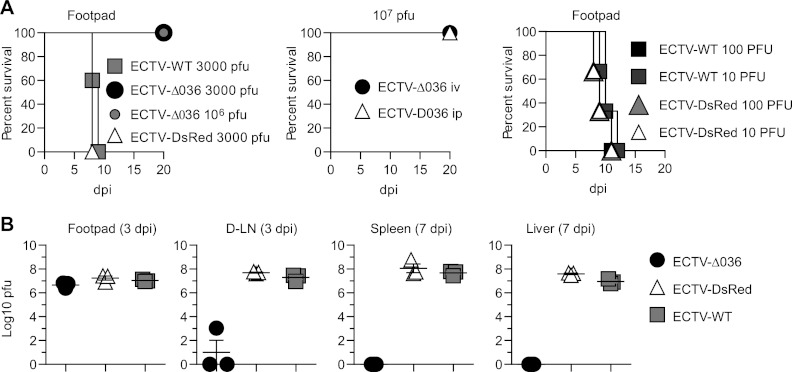
ECTV-Δ036 but not ECTV-DsRed is severely attenuated in vivo.
To study the contribution of EVM036 to ECTV virulence, BALB/c mice were infected in the footpad with ECTV-WT, -Δ036, or -DsRed. All the mice infected with ECTV-Δ36 survived the infection indefinitely without symptoms even with doses as high as 107 PFU i.p. On the other hand, as little 10 PFU of ECTV-DsRed or ECTV-WT in the footpad was 100% lethal (Fig. 4A). At 7 dpi with 3000 PFU in the footpad, virus titers were high for the three viruses in the footpad indicating in situ replication. However, the mice infected with ECTV-Δ036 had very little or no detectable virus in the draining lymph node (D-LN) and no detectable virus in livers and spleens, indicating poor or no lymphohematogenous spread. Conversely, all the mice infected with either ECTV-WT or ECTV-DsRed had similarly high virus loads in D-LN, livers, and spleens, demonstrating that ECTV-WT and ECTV-DsRed disseminated and replicated in vivo with high and similar efficiencies (Fig. 4B). Hence, EVM036 is required for the virulence of ECTV in immunocompetent mice, and ECTV-Δ036 can be used as a backbone to generate recombinant ECTV virus of WT virulence.
Fig 4.
ECTV-Δ036 but not ECTV-DsRed is severely attenuated in vivo. (A) BALB/c mice were infected with various doses of ECTV-WT, ECTV-Δ036, or ECTV-DsRed in the footpad, and survival was monitored. Experiments had 5 (left and middle) or 3 (right) mice/group. (B) Virus titers in the indicated organs of BALB/c mice (n = 3) at the indicated dpi. Each data point indicates an individual mouse (P < 0.0001 for values for all organs).
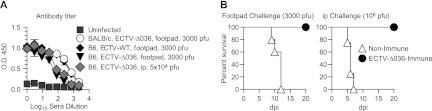
Challenge with ECTV-Δ036 induces a humoral immune response and protects susceptible mice from mousepox.
Since ECTV-Δ036 was highly attenuated in vivo and undetectable in organs, we next determined whether ECTV-Δ036 could induce antibody (Ab) responses. We inoculated mousepox-resistant C57BL/6 mice with 5 × 104 PFU ECTV-Δ036 i.p. or 3,000 PFU ECTV-WT in the footpad. Four weeks later, all the mice had similar levels of anti-ECTV antibodies in their sera, as determined in an ELISA, indicating that ECTV-Δ036 induced humoral immune responses (Fig. 5A). To determine whether ECTV-Δ036 could be used as a vaccine, susceptible BALB/c mice were infected with 3,000 PFU ECTV-Δ036 in the footpad and at 28 dpi were challenged with 3,000 PFU ECTV-WT in the other footpad or with 106 PFU intraperitoneally. All mice that received ECTV-Δ036 survived (Fig. 5B) without any symptoms of infection, while all control unimmunized mice succumbed, suggesting that OPVs deficient in F13L orthologs could be used as safe vaccine vectors in immunocompetent individuals.
Fig 5.
ECTV-Δ036 induces a humoral immune response and serves as a vaccine. (A) C57BL/6 mice were inoculated in the footpad with 3,000 PFU or i.p. with 104 PFU of the indicated viruses. Titers of Ab to the ECTV protein EVM135 were determined in serum at 30 dpi by ELISA. (B) BALB/c mice were infected in the footpad with 3000 PFU ECTV-Δ036 or left uninfected. At 28 dpi they were challenged with ECTV-WT, and survival at different dpi was determined. P = 0.0034.
DISCUSSION
ECTV is a natural mouse pathogen that serves as an excellent model of human smallpox and is also useful for studying viral pathogenesis, basic immunology, and vaccine efficacy (7). These types of studies frequently require the production of recombinant viruses with WT virulence. In the past, we have used homologous recombination and selection based on plaque fluorescence without drugs to replace a short fragment of ECTV (nucleotides 189898 to 189949) that lies in a large noncoding region of ECTV, with the sequences coding for EGFP being driven by the 7.5 promoter. This resulted in a virus, ECTV 189898− p7.5-EGFP, that had WT virulence but expressed cytosolic EGFP. However, the isolation of this recombinant took 7 months, and the system is useful only for recombinants that are fluorescent. More recently, we generated ECTV expressing firefly luciferase (ECTV-Luc) by replacing EGFP with luciferase in ECTV 189898− p7.5-EGFP and selecting nonfluorescent plaques. While this method is broadly applicable, selecting nonfluorescent plaques is very difficult and time-consuming. The Buller lab introduced the E. coli lacZ and mouse Il4 genes into the disrupted CHO gene using gpt as a transient selection marker (3). However, this method requires MXH selection, which in our hands requires many rounds of selection and is time-consuming. Others have replaced the thymidine kinase (TK) gene with the gene of interest followed by selection with xanthine-guanine phosphoribosyltransferase as performed with VACV (5), but this resulted in a severely attenuated virus (23). Jackson et al. used TK− ECTV as the backbone and inserted the interleukin 4 (IL-4) gene together with the herpes simplex virus (HSV) TK gene immediately downstream of the early promoter for the ECTV ortholog of VACV F7L. While this virus was highly virulent due to IL-4, the control virus with the HSV TK alone was less virulent than ECTV WT (18). We generated ECTV deficient in EVM036 and developed a system similar to the one already described for VACV deficient in F13L (2, 5) with the goal of simplifying and accelerating the production of ECTV recombinants with WT virulence. We found that like its VACV counterpart, ECTV-Δ036 has a small-plaque phenotype. We have also shown that ECTV-Δ036 can be used as a backbone for the rapid generation of recombinant ECTV viruses by selecting against its small-plaque phenotype. To be useful in pathogenesis studies, it was also important that the recombinants regain virulence. A possible difficulty was that the terminal sequences of EVM036 are part of the EVM035 promoter and the introduction of an intervening sequence between the two genes could have resulted in an attenuated virus due to EVM035 deficiency. To circumvent this problem, we performed a PCR site-directed mutagenesis in which we manipulated the nucleotides at the 3′ end of EVM036 without affecting translation and added the WT sequence between gene of interest and EVM035. We found that reintroduction of this silently mutated gene to its original location together with DsRed resulted in recombinant virus that formed WT-size plaques. Moreover, ECTV-DsRed was as virulent as ECTV-WT. Thus, the newly developed system provides a fast and efficient method to produce fully pathogenic recombinant ECTV. We have generated in the laboratory other nonfluorescent recombinants with similar success (data not shown) in as little as 3 weeks with little effort.
The use of VACV as the smallpox vaccine allowed the successful worldwide eradication of smallpox. Additionally, VACV is a popular vector used for other vaccines against pathogens like HIV (6, 8, 15, 24). Unfortunately, the current smallpox vaccine is unsafe for immunocompromised individuals and children.
Although ECTV-Δ036 was highly attenuated in immunocompetent but susceptible BALB/c mice, it induced humoral immune responses that were similar to those induced by ECTV-WT. Moreover, following ECTV-Δ036 immunization, BALB/c mice were fully protected from ECTV-WT challenge. These results are consistent with previous reports showing protective immunity after immunization with ECTV deficient in the ortholog of A36R (22) and with VACV LC16m8, which has a frameshift mutation in B5R (20, 30). Neither of these viruses produces EV. Thus, our findings warrant further exploration of mutants with alterations in F13L or its orthologs to develop a safer smallpox vaccine or vaccine vectors for other diseases.
EV are thought to be essential for cell-to-cell spread in tissue culture and for spread within the host (25, 29). In VACV, formation of EV is fully dependent on F13L. Thus, VACV deficient in F13L has a small-plaque phenotype (1). Very recently, it was also shown that VACV deficient in F13L is attenuated in immunocompetent and immunodeficient mice (31). However, whether the F13L ortholog has a similar role in other OPVs had never been explored. In this study, we showed that as in VACV, EVM036 is essential for cell-to-cell spread, as its deletion resulted in a virus that formed small plaques and produced significantly less viral progeny following infection of cells at low multiplicity. Furthermore, ECTV-Δ036 was highly attenuated in immunocompetent BALB/c mice, indicating that EVs are important for pathogenesis of an OPV in a natural host.
ACKNOWLEDGMENTS
We thank Fox Chase Cancer Center Laboratory Animal and Tissue Culture Facilities for their services, Glenn Rall for comments, and Holly Gillin for assistance in the preparation of the manuscript.
This work was supported by NIAID grant U19AI083008 to L.J.S. and NCI grant P30CA006927 to Fox Chase Cancer Center. The qPCR reagents and instrument were a generous gift from the Kirby Foundation.
Footnotes
Published ahead of print 3 October 2012
REFERENCES
- 1. Blasco R, Moss B. 1991. Extracellular vaccinia virus formation and cell-to-cell virus transmission are prevented by deletion of the gene encoding the 37,000-dalton outer envelope protein. J. Virol. 65:5910–5920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Blasco R, Moss B. 1995. Selection of recombinant vaccinia viruses on the basis of plaque formation. Gene 158:157–162 [DOI] [PubMed] [Google Scholar]
- 3. Chen N, et al. 2011. Poxvirus interleukin-4 expression overcomes inherent resistance and vaccine-induced immunity: pathogenesis, prophylaxis, and antiviral therapy. Virology 409:328–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen N, et al. 2003. The genomic sequence of ectromelia virus, the causative agent of mousepox. Virology 317:165–186 [DOI] [PubMed] [Google Scholar]
- 5. Earl PL, Moss B, Wyatt LS, Carroll MW. 2001. Generation of recombinant vaccinia viruses. Curr. Protoc. Mol. Biol. 43:16.17.1–16.17.19 [DOI] [PubMed] [Google Scholar]
- 6. Essajee S, Kaufman HL. 2004. Poxvirus vaccines for cancer and HIV therapy. Expert Opin. Biol. Ther. 4:575–588 [DOI] [PubMed] [Google Scholar]
- 7. Esteban DJ, Buller RM. 2005. Ectromelia virus: the causative agent of mousepox. J. Gen. Virol. 86:2645–2659 [DOI] [PubMed] [Google Scholar]
- 8. Esteban M. 2009. Attenuated poxvirus vectors MVA and NYVAC as promising vaccine candidates against HIV/AIDS. Hum. Vaccin. 5:867–871 [DOI] [PubMed] [Google Scholar]
- 9. Falkner FG, Moss B. 1988. Escherichia coli gpt gene provides dominant selection for vaccinia virus open reading frame expression vectors. J. Virol. 62:1849–1854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fang M, et al. 2011. CD94 is essential for NK cell-mediated resistance to a lethal viral disease. Immunity 34:579–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fang M, Roscoe F, Sigal LJ. 2010. Age-dependent susceptibility to a viral disease due to decreased natural killer cell numbers and trafficking. J. Exp. Med. 207:2369–2381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fang M, Sigal LJ. 2005. Antibodies and CD8+ T cells are complementary and essential for natural resistance to a highly lethal cytopathic virus. J. Immunol. 175:6829–6836 [DOI] [PubMed] [Google Scholar]
- 13. Fang M, Sigal LJ. 2006. Direct CD28 costimulation is required for CD8+ T cell-mediated resistance to an acute viral disease in a natural host. J. Immunol. 177:8027–8036 [DOI] [PubMed] [Google Scholar]
- 14. Galindo I, Lorenzo MM, Blasco R. 2001. Set of vectors for the expression of histidine-tagged proteins in vaccinia virus recombinants. Biotechniques 30:524–526, 528–529 [DOI] [PubMed] [Google Scholar]
- 15. Gherardi MM, Esteban M. 2005. Recombinant poxviruses as mucosal vaccine vectors. J. Gen. Virol. 86:2925–2936 [DOI] [PubMed] [Google Scholar]
- 16. Grosenbach DW, et al. 2010. Efficacy of ST-246 versus lethal poxvirus challenge in immunodeficient mice. Proc. Natl. Acad. Sci. U. S. A. 107:838–843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Holzer GW, Falkner FG. 1997. Construction of a vaccinia virus deficient in the essential DNA repair enzyme uracil DNA glycosylase by a complementing cell line. J. Virol. 71:4997–5002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jackson RJ, et al. 2001. Expression of mouse interleukin-4 by a recombinant ectromelia virus suppresses cytolytic lymphocyte responses and overcomes genetic resistance to mousepox. J. Virol. 75:1205–1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jordan R, Leeds JM, Tyavanagimatt S, Hruby DE. 2010. Development of ST-246(R) for treatment of poxvirus infections. Viruses 2:2409–2435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kidokoro M, Tashiro M, Shida H. 2005. Genetically stable and fully effective smallpox vaccine strain constructed from highly attenuated vaccinia LC16m8. Proc. Natl. Acad. Sci. U. S. A. 102:4152–4157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lorenzo MM, Galindo I, Blasco R. 2004. Construction and isolation of recombinant vaccinia virus using genetic markers. Methods Mol. Biol. 269:15–30 [DOI] [PubMed] [Google Scholar]
- 22. Lynn H, et al. 2012. Loss of cytoskeletal transport during egress critically attenuates ectromelia virus infection in vivo. J. Virol. 86:7427–7443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Panchanathan V, Chaudhri G, Karupiah G. 2005. Interferon function is not required for recovery from a secondary poxvirus infection. Proc. Natl. Acad. Sci. U. S. A. 102:12921–12926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pantaleo G, Esteban M, Jacobs B, Tartaglia J. 2010. Poxvirus vector-based HIV vaccines. Curr. Opin. HIV AIDS 5:391–396 [DOI] [PubMed] [Google Scholar]
- 25. Payne LG. 1980. Significance of extracellular enveloped virus in the in vitro and in vivo dissemination of vaccinia. J. Gen. Virol. 50:89–100 [DOI] [PubMed] [Google Scholar]
- 26. Roberts KL, Smith GL. 2008. Vaccinia virus morphogenesis and dissemination. Trends Microbiol. 16:472–479 [DOI] [PubMed] [Google Scholar]
- 27. Sanchez-Puig JM, Blasco R. 2005. Isolation of vaccinia MVA recombinants using the viral F13L gene as the selective marker. Biotechniques 39:665–674 [DOI] [PubMed] [Google Scholar]
- 28. Sanchez-Puig JM, Lorenzo MM, Blasco R. 2012. Isolation of recombinant MVA using F13L selection. Methods Mol. Biol. 890:93–111 [DOI] [PubMed] [Google Scholar]
- 29. Smith GL, Vanderplasschen A, Law M. 2002. The formation and function of extracellular enveloped vaccinia virus. J. Gen. Virol. 83:2915–2931 [DOI] [PubMed] [Google Scholar]
- 30. Sugimoto M, et al. 1985. Gene structures of low-neurovirulent vaccinia virus LC16m0, LC16m8, and their Lister original (LO) strains. Microbiol. Immunol. 29:421–428 [DOI] [PubMed] [Google Scholar]
- 31. Vliegen I, Yang G, Hruby D, Jordan R, Neyts J. 2012. Deletion of the vaccinia virus F13L gene results in a highly attenuated virus that mounts a protective immune response against subsequent vaccinia virus challenge. Antiviral Res. 93:160–166 [DOI] [PubMed] [Google Scholar]
- 32. Xu RH, Fang M, Klein-Szanto A, Sigal LJ. 2007. Memory CD8+ T cells are gatekeepers of the lymph node draining the site of viral infection. Proc. Natl. Acad. Sci. U. S. A. 104:10992–10997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yang G, et al. 2005. An orally bioavailable antipoxvirus compound (ST-246) inhibits extracellular virus formation and protects mice from lethal orthopoxvirus challenge. J. Virol. 79:13139–13149 [DOI] [PMC free article] [PubMed] [Google Scholar]