Human Immunodeficiency Virus (HIV) infection is a global pandemic. According to the data released by UNAIDS in 2007, India had 2.5 million people living with HIV infection.[1] Next to sub-Saharan Africa, it has the second largest burden of HIV-related illness. Though the main targets of HIV infection are the cells of the immune system, the nervous system is often damaged during the course of infection, not only by disease processes that are secondary to immune dysfunction but also by more fundamental effects of the retrovirus.
Neurological disease is the first manifestation of symptomatic HIV infection in roughly 10–20% of patients, while about 60% of patients with advanced HIV disease will have clinically evident neurological dysfunction.[2–4] Autopsy studies of patients with advanced HIV disease have demonstrated pathologic abnormalities of the nervous system in 75–90% of cases,[2,5,6] thus proving that the incidence of subclinical neurological disease is even higher. This may be explained by the fact that the central nervous system (CNS) is a sanctuary site for HIV infection and there is poor CNS penetration of antiviral drugs due to the presence of intact blood brain barrier.[2] We undertook this study to see the prevalence of the various neurological manifestations in HIV-positive admitted patients who presented to a tertiary hospital in our setup.
The study was carried out for a period of 1 year from November 2010 to October 2011 in the Gandhi ward of Department of Medicine, King George's Medical University, Lucknow, India. A total of 105 HIV-positive patients of more than 14 years of age who were admitted were enrolled in the study, of which 80 patients were suffering from Acquired Immunodeficiency Syndrome (AIDS). Out of the total 105 HIV-positive patients, 43 patients had neurological manifestations. Patients with HIV-unrelated developmental, neurological, medical, and neurobehavioral conditions that potentially impaired cognition were excluded from the study. Selected patients having neurological manifestations were subjected to detailed history, examination, and other routine and special investigations as required for that particular case's diagnosis and management. HIV was serologically confirmed by enzyme-linked immunosorbent assay (ELISA), and CD4 estimation was carried out by flow cytometer using Syflow counter. Informed consent was taken from each patient enrolled for the study, and the university ethical committee reviewed and approved the study.
A total of 105 HIV-infected patients were enrolled in the study. The mean age of all patients was 34.3±7.8 years, and the same was observed in the HIV-positive patients with neurological manifestations. The mean age of males in the study was 35.0±7.7 years and that of females was 31.11±7.6 years. Majority of patients (49.5%) were in the age group of 31–40 years, followed by 30.5% in the age group of 21–30 years. Male to female ratio was 4.5:1. Contact with commercial sex workers was the most common mode (75.24%) of transmission among males. 94.7% (18/19) females in the study got the infection from their HIV-positive husbands. Contaminated blood transfusion was the next most common mode of transmission (5.7%). One patient was an intravenous drug abuser, and in one patient no source of infection could be found.
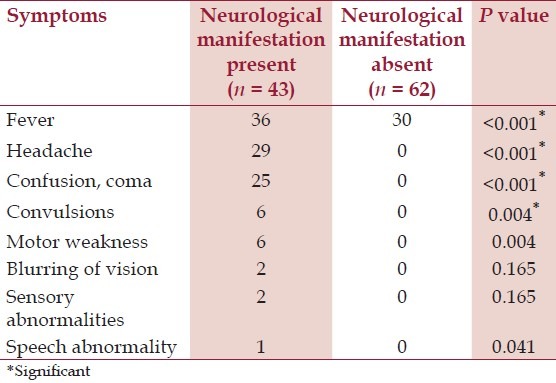
Out of the 105 patients enrolled in the study, 43 (40.9%) were suffering from neurological manifestations. Among the HIV-positive patients with neurological manifestations; fever was the most common presenting symptom (83.7%), followed by headache (67.4%), coma, or confusion (58.1%) and seizure (14.0%). Two patients presented with blurring of vision, both of which subsequently were found to be suffering from cytomegalovirus (CMV) retinitis. Meningitis was the leading cause of headache, coma, and seizures [Table 1].
Table 1.
Distribution of symptoms in patients with and without neurological manifestations
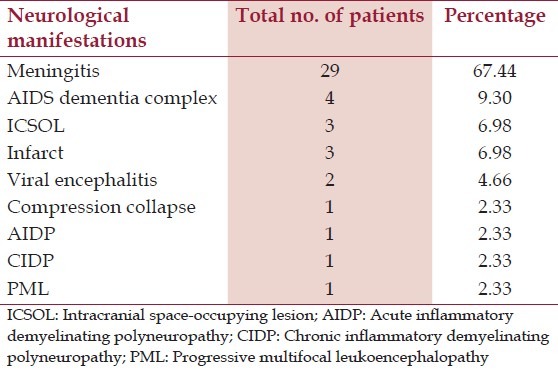
Meningitis was the most common neurological manifestation present in 29 (67.44%) patients, followed by AIDS dementia complex (ADC) in 4 patients (9.30%). Cranial nerve involvement was present in patient with chronic inflammatory demyelinating polyneuropathy (CIDP), and epidural hematoma was an additional finding in patient with pyogenic meningitis [Table 2]. Among the meningitis types, tubercular meningitis was the most common type present in 21 (70.0%) patients, followed by cryptococcal and pyogenic meningitis in 7 (23.3%) and 2 patients (6.7%), respectively. One case each of cryptococcal meningitis and pyogenic meningitis was a follow-through case of tuberculosis meningitis and was already on anti-tubercular therapy (ATT). In the intracranial space occupying lesion (ICSOL), one patient had tubercular abscess on computed tomography (CT) scan head, the second patient's CT scan showed ring-enhancing space occupying lesion leading to possibility of neurocysticercosis (NCC)/tuberculomas, and the third patient had multiple ring-enhancing lesions leading to possibility of toxoplasma. One patient (2.33%) presented with paraplegia due to L2–L3 vertebral compression collapse and was tubercular in nature. Tuberculosis was very common etiology (55.8%).
Table 2.
Neurological manifestations in HIV.positive patients
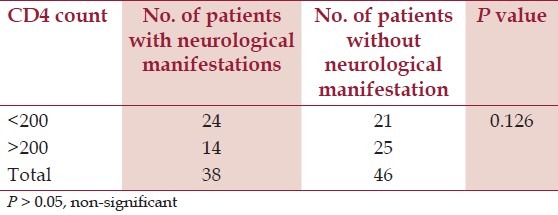
CD4 count could be done only in 84 patients in our study. In 38 HIV-infected patients with neurological manifestations, the mean CD4 count was 177.9±105.0, of which 24 (63.2%) patients had CD4 count less than 200. The remaining 46 HIV cases without neurological manifestation had mean CD4 count as 211.0±114.4, of which 21 (45.7%) had CD4 count less than 200 [Table 3]. The incidence of neurological manifestations increased with decrease in CD4 count. Eleven out of 20 (55%) patients with tubercular meningitis had CD4 count less than 200, but in cryptococcal meningitis 5 out of 6 (83.3%) patients had CD4 less than 100.
Table 3.
Distribution of patients according to CD4 count (n = 84)
All the cases in this study had infection with HIV-1. Infection with HIV-2 or dual infection was not seen. Other studies[7,8] have reported infection with HIV-2 in 3–9% of all HIV-infected persons. This difference in our study may be due to the possible geographic confinement of HIV-2 and also due to the fact that HIV-2 infection has more indolent course.
Mean age for all the cases was 34.3±7.8 years. The age distribution is comparable to the study done by Teja et al.[9] in which the median age was 36 years and most of the patients were in the age group of 30–40 years. The mean age in a study was 34.9±12 years.[10] Similarly in our study, maximum patients were in the age group of 31–40 years, followed by the age group of 21–30 years. Early clinical manifestation can be due to lack of effective anti-retroviral (ARV) compared to developed countries, and they succumb to this disease at an early age. Most of our patients are contracting the infection during adolescence, which is due to lack of sexual education and awareness of the spread of this disease.
Male to female ratio in our study was 4.5:1. Other studies have reported this ratio varying from 3:1 to 6:1. In a study done by Teja et al.,[9] the ratio was 3.9:1, whereas another study has reported a ratio of 3:1.[10] However, the ratio is nearly 1:1 in North America and Africa.[11] In India, males are the bread earners and most of them harbor the disease from commercial sex workers, when they go far away from their family to earn their livelihood. Most of them are laborers and belong to low socioeconomic status. Females mostly contract this disease from their husbands; their health is neglected and they are unable to seek medical care due to gender bias and male dominance in our society. The major route of transmission of this infection among males is contact with commercial sex workers. However, in the United States, homosexual contact is the common route, but it is not so in India as this relationship is taboo.[11]
Neurological manifestations are common in HIV-infected persons. There has been considerable morbidity and increased mortality due to neurological complications, which can affect the nervous system at all levels and at all stages of HIV disease. In our study, out of a total of 105 patients, 40.9% had neurological involvement. Close to our findings, a study has reported 44.6% neurological manifestations present in HIV-infected patients of their studied cases.[12] In our study on HIV patients with neurological manifestation, fever was the most common symptom in 83.7% patients, followed by headache (67.4%), coma, or confusion (58%), and 14.0% patients presented with convulsions. These were comparable to the study done by Pal et al.[13] in which fever was the commonest symptom (92%), followed by confused or comatose state (71%), and 33% patients had convulsions. A study from the USA has also reported the presence of headache as a common symptom in their studied group; however, they were not different between HIV-seropositive and -seronegative subjects.[14] Seizures were a relatively frequent complication of HIV infection and may be a consequence of opportunistic infections, neoplasms, or HIV encephalopathy. However, in our study, only 14% presented with seizures. This is contrary to a finding reported in a study in which cerebral mass lesions were the most common cause responsible for 32% cases of new-onset seizures in patients with HIV infection.[15] This difference can be due to the small number of patients of ICSOL present in our study.
Among the neurological manifestations, meningitis was found in a majority of cases (67.4%) in our study, whereas other neurological manifestations were even less than 10% individually. Similar to our study, meningitis was found in 71.9% of HIV patients with neurological manifestation in another study.[16] Contrary findings have also been reported (17.8% of cases).[12] This is because patients visiting out-patient clinics formed the study group in that study, whereas our study group comprised only indoor patients who were admitted in critical condition. Our study shows that in neurologically manifested HIV patients, tubercular meningitis manifested more than cryptococcal meningitis (48.9% vs. 16.3%). Studies have reported tubercular meningitis to be present in 43.8% versus 28.1% and 25.1% versus 11.0% of cryptococcal meningitis.[9,16] Contrary to the above two studies, it has been reported in another study that cryptococcal meningitis was more common than tubercular meningitis (58% vs. 16%) in their group of patients.[12] The difference in the prevalence of tubercular and cryptococcal meningitis in various Indian studies can be due to the difference in prevalence of tuberculosis in various parts of the country. In our study, tuberculosis also manifested as tuberculoma, suspected tubercular abscess as ICSOL, and compression collapse due to Pott's spine, seen in one case each.
Tuberculosis was the leading cause of neurological disorders (55.8%) in our study, presenting as opportunistic as well as co-infection indicating the dual epidemic. Tuberculosis and HIV infection have profound impact on each other. HIV infection increases the risk of developing active tuberculosis by 15–30 times. According to NACO, tuberculosis is the commonest opportunistic infection, both pulmonary and extrapulmonary (62.2%) in India, which can explain its high incidence in HIV-infected individuals in India as compared to western countries. In another study, tuberculosis was present in 54.8% of all patients, which is close to our findings.[10] In our study, 13.3% had pulmonary tuberculosis and 41.9% had extrapulmonary tuberculosis including 7.6% of miliary tuberculosis. Extrapulmonary tuberculosis is common among HIV-positive patients as shown in various series; extrapulmonary tuberculosis, alone or in association with pulmonary disease, has been documented in 40–60% of all cases in HIV co-infected patients. In extrapulmonary tuberculosis, tubercular meningitis formed 47.7% in our study, and it has been also seen that in advanced diseases, Mycobacteria and meningitis are frequent.[17]
The mean CD4 count in patients with neurological manifestations was 191.71±117.7, and 64.7% of neurologically manifested HIV patients had CD4 count less than 200. With lowering of CD4 count accounts for more neurological disorders in HIV patients. Studies have also reported the presence of neurological complication as well as other clinical manifestations associated with decreased CD4 count and increased viral load. 55% of our patients with tubercular meningitis had CD4 count less than 200, but in cryptococcal meningitis 83% patients had CD4 less than 100.[18,19] This shows that irrespective of CD4, tubercular meningitis is the most opportunistic infection; however, prognosis is poor with low CD4. Similar to our findings, a study from the USA[20] has also stated that tuberculosis meningitis can occur at any CD4 count level, while cryptococcal meningitis usually occurs when CD4 count is less than 200.
HIV dementia or HIV encephalopathy or ADC is the nonfocal disorder characterized by preserved alertness. In our study, 9.3% patients presented with ADC. Two other studies have reported ADC to be present in 4.3%and 5% of HIV patients with neurological manifestations, respectively.[12,21] Studies from western countries have shown that 20–30% of patients with advanced HIV infection go on to develop ADC.[22] The prevalence in our study is low, probably because of it being a late manifestation of HIV disease and many patients succumbing to other complications before progressing to this stage in the underdeveloped countries.
Progressive multifocal leukoencephalopathy (PML) is one of the rare CNS-related disorders observed commonly in HIV patients, caused by JC virus. PML was present in only one patient (2.33%) in our study, who presented with seizures as first manifestation with CD4 count of 51. Another study has also reported that PML was present in only 5.2% patients.[16]
In conclusion, our study has shown that secondary neurological disorders were more common due to opportunistic infection, which can also be attributed to the fact that patients are not availing highly active anti-retroviral therapy (HAART) due to high cost of the drugs and lack of widespread availability of facility for HIV/AIDS center. Tuberculosis was the prominent etiology of all neurological disorders in HIV patients irrespective of immune status. Moreover, HIV itself presented as various neurological problems throughout the course of infection. The dual epidemic of tuberculosis and HIV has to be controlled immediately with emphasis on awareness of the disease progression and prevention. Our observations differed from those of developed countries, which may be attributed to the different socioeconomic status, culture, and unawareness of sexual education.
Acknowledgment
We would like to thank the residents and paramedical staff, pathologists, radiologist, and biochemist of the laboratory for their help and support.
References
- 1.UNAIDS. Press release: 2.5 million people in India living with HIV, according to new estimates. 2007 Jul 6th; [Google Scholar]
- 2.Levy RM, Bredesen DE, Rosenblum ML. Neurological manifestations of the acquired immunodeficiency syndrome (AIDS): Experience at UCSF and review of the literature. J Neurosurg. 1985;62:475–95. doi: 10.3171/jns.1985.62.4.0475. [DOI] [PubMed] [Google Scholar]
- 3.Koppel BS, Wormser GP, Tuchman AJ, Maayan S, Hewlett D, Jr, Daras M. Central nervous system involvement in patients with acquired immune deficiency syndrome (AIDS) Acta Neurol Scand. 1985;71:337–53. doi: 10.1111/j.1600-0404.1985.tb03211.x. [DOI] [PubMed] [Google Scholar]
- 4.Snider WD, Simpson DM, Nielsen S, Gold JW, Metroka CE, Posner JB. Neurological complications of acquired immune deficiency syndrome: Analysis of 50 patients. Ann Neurol. 1983;14:403–18. doi: 10.1002/ana.410140404. [DOI] [PubMed] [Google Scholar]
- 5.de la Monte SM, Ho DD, Schooley RT, Hirsch MS, Richardson EP., Jr Subacute encephalomyelitis of AIDS and its relation to HTLV-III infection. Neurology. 1987;37:562–9. doi: 10.1212/wnl.37.4.562. [DOI] [PubMed] [Google Scholar]
- 6.Rosenblum ML, Bredesen DE, Levy RM. Algorithms for the treatment of AIDS patients with neurological diseases. In: Rosenblum ML, Levy RM, Bredesen DE, editors. AIDS and the Nervous System. New York: Raven Press; 1988. pp. 389–96. [Google Scholar]
- 7.Kulshreshtha R, Mathur A, Chattopadhya D, Chaturvedi UC. HIV-2 prevalance in Uttar Pradesh. Indian J Med Res. 1996;103:131–3. [PubMed] [Google Scholar]
- 8.Pfutzner A, Dietrich U, von Eichel U, von Briesen H, Brede HD, Maniar JK, et al. HIV-1 and HIV-2 infection in high risk population in Bombay, India. Evidence of spread of HIV-2 and presence of a divergent HIV-1 subtype. J Acquir Immune Defic Syndr. 1992;5:972–7. [PubMed] [Google Scholar]
- 9.Teja VD, Talasila SR, Vemu L. Neurologic Manifestations of HIV infection: An Indian hospital based study. Indian J Med Res. 2005;121:377–94. [Google Scholar]
- 10.Sircar AR, Tripathi AK, Choudhary SK, Misra R. Clinical profile of AIDS: A study at a referral hospital. J Assoc Physicians India. 1998;46:775–8. [PubMed] [Google Scholar]
- 11.Fauci AS, Lane HC. Human immunodeficiency virus disease: AIDS and related disorders. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al., editors. Harrison's Principle of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008. pp. 1137–204. [Google Scholar]
- 12.Wadia RS, Pujari SN, Kothari S, Udhar M, Kulkarni S, Bhagat S, et al. Neurological manifestations of HIV Disease. J Assoc Physicians India. 2001;49:343–8. [PubMed] [Google Scholar]
- 13.Pal J, Karmakar PS, Ray A, Saha S, Roy K, Talukdar A, et al. Opportunistic infections of central nervous system in AIDS. J Indian Med Assoc. 2009;107:446–9. [PubMed] [Google Scholar]
- 14.Berger JR, Stein N, Pall L. Headache and human immunodeficiency virus infection: A case control study. Eur Neurol. 1996;36:229–33. doi: 10.1159/000117255. [DOI] [PubMed] [Google Scholar]
- 15.Holtzman DM, Kaku DA, So YT. New onset seizure associated with HIV infection: Causation and clinical feature in 100 cases. Am J Med. 1989;87:173–7. doi: 10.1016/s0002-9343(89)80693-x. [DOI] [PubMed] [Google Scholar]
- 16.Attili SVS, Gulati AK, Singh VP, Varma DV, Rai M, Sundar S. Diarrhea, CD4 counts and enteric infections in a hospital - based cohort of HIV-infected patients around Varanasi, India. BMC Infect Dis. 2006;6:39. doi: 10.1186/1471-2334-6-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raviglione MC, O’Brien RJ. Tuberculosis. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al., editors. Harrison's Principle of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008. pp. 1006–20. [Google Scholar]
- 18.Gochitashvili N, Tsertsvadze T, Gatserelia L, Abashidze L, Sharvadze L. Relationship of neurological manifestations, CD4+ lymphocyte count and plasma viral load in HIV infected patients. Georgian Med News. 2005;121:51–5. [PubMed] [Google Scholar]
- 19.Bolokadze N, Gabunia P, Ezugbaia M, Gatserelia L, Khechiashvili G. Neurological complications in patients with HIV/AIDS. Georgian Med News. 2008;165:34–8. [PubMed] [Google Scholar]
- 20.Vinnard C, Macgregor RR. Tuberculous meningitis in HIV-infected individuals. Curr HIV/AIDS Rep. 2009;6:139–45. doi: 10.1007/s11904-009-0019-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deshpande AK, Patnaik MM. Nonopportunistic neurologic manifestations of the human immunodeficiency virus: An Indian study. Med Gen Med. 2005;7:2. [PMC free article] [PubMed] [Google Scholar]
- 22.Navia B, Jordan BD, Price RW. The AIDS Dementia Complex: Clinical features. Ann Neurol. 1986;19:517–24. doi: 10.1002/ana.410190602. [DOI] [PubMed] [Google Scholar]


