Abstract
Background
Worsening renal function is common among patients hospitalized for acute decompensated heart failure (ADHF). When this occurs, subsequent management decisions often pit the desire for effective decongestion against concerns about further worsening renal function. There are no evidence-based treatments or guidelines to assist in these difficult management decisions. Ultrafiltration is a potentially attractive alternative to loop diuretics for the management of fluid overload in patients with ADHF and worsening renal function.
Methods and Results
The National Heart, Lung, and Blood Institute Heart Failure Clinical Research Network designed a clinical trial to determine if ultrafiltration results in improved renal function and relief of congestion compared with stepped pharmacologic care when assessed 96 hours after randomization in patients with ADHF and cardiorenal syndrome. Enrollment began in June 2008. This paper describes the rationale and design of the Cardiorenal Rescue Study in Acute Decompensated Heart Failure (CARRESS-HF).
Conclusions
Treating the signs and symptoms of congestion in ADHF is often complicated by worsening renal function. CARRESS-HF compares treatment strategies (ultrafiltration vs stepped pharmacologic care) for the management of worsening renal function in patients with ADHF. The results of the CARRESS-HF trial are expected to provide information and evidence as to the most appropriate approaches for treating this challenging patient population.
Keywords: Cardiorenal syndrome, congestion, diuretics, ultrafiltration, heart failure
Cardiorenal syndrome is a “disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other.”1 One widely recognized subtype of cardiorenal syndrome is kidney injury that occurs in the setting of acute decompensated heart failure (AHDF) and is often recognized by the presence of abnormal kidney function at the time of presentation or worsening renal function after initiation of acute therapies.1 Worsening renal function, often defined as an increase in creatinine of ≥0.3 mg/dL from baseline, occurs in 20%–30% of patients with ADHF and is associated with greater length of stay, hospital readmission, and death.2–4 Complicating our understanding of cardiorenal syndrome are recent observations that worsening renal function may be associated with improved clinical outcomes in some subgroups.5 The underlying pathophysiology of this increase in creatinine is poorly understood and probably multifactorial, reflecting comorbid conditions, acute therapies, impaired renal perfusion, sympathetic over-activity, oxidative injury, and endothelial dysfunction.1,6 Perhaps for this reason, there are no proven treatments or guidelines for patients who develop worsening renal function in the setting of ADHF. When renal function deteriorates during treatment of ADHF, subsequent management decisions often pit the desire for effective decongestion against concerns about further worsening of renal function. Common interventions for patients with worsening renal function include intensification or deescalation of loop diuretics or the use of vasodilators, positive inotropes, or ultrafiltration.
Ultrafiltration is a potentially attractive alternative to loop diuretics for the management of fluid overload in patients with ADHF and cardiorenal syndrome. It is a more effective means of restoring sodium balance than intravenous loop diuretics,7 has no effect on serum electrolytes, and results in rapid and predictable fluid removal.8–12 Moreover, ultrafiltration does not directly stimulate the neurohormonal system and appears to restore responsiveness to loop diuretics in patients with diuretic resistance.8–10,13
Rapid relief of venous congestion is associated with improved renal function in animal experiments and human studies, indicating that “congestion” of the kidney may significantly impact renal function in patients with ADHF, especially those who go on to develop cardiorenal syndrome.14–16
In the Ultrafiltration Versus Intravenous Diuretics for Patients Hospitalized for Acute Decompensated Heart Failure (UNLOAD) trial, venovenous ultrafiltration for up to 48 hours was compared with intravenous diuretics in patients hospitalized for ADHF.17 Patients were hospitalized with the primary diagnosis of decompensated heart failure and evidence of volume overload on physical examination. Patients with normal and decreased systolic function were included. Patients were randomized within 24 hours of hospitalization. Thus the 2 treatment arms represented early treatment strategies, not “rescue therapy.” Patients randomized to the standard-care arm were treated with intravenous diuretics (average daily dose 181 mg/d referenced to furosemide-equivalent doses). Patients in the ultrafiltration arm had all diuretics stopped and underwent ultrafiltration at volume removal rates of up to 500 mL/h for up to 48 hours at the discretion of the treating physician. Despite the aggressive use of diuretics in the comparison arm (3.3 L net fluid loss in the first 48 hours), ultrafiltration removed more fluid (4.6 L net fluid loss in the first 48 hours) and was associated with more weight loss and improved clinical outcomes 90 days after hospitalization. There was no significant difference in the incidence of worsening renal function between the 2 treatment groups, raising hopes that ultrafiltration might be an effective treatment for patients with impaired baseline renal function, diuretic resistance, or worsening renal function after hospitalization.
In spite of these promising results, the UNLOAD trial has been criticized for being small, unblinded, and inadequate regarding the dosing of diuretics for patients in the usual-care arm. In addition, ultrafiltration is expensive, requires systemic anticoagulation, and can lead to severe device-related complications, including air embolism, bleeding, and overly aggressive volume removal.18,19
Therefore, the purpose of the Cardiorenal Rescue Study in Acute Decompensated Heart Failure (CARRESS-HF) is to evaluate the efficacy and safety of ultrafiltration compared with stepped pharmacologic care for the treatment of patients with persistent congestion and worsening renal function.
Study Design
CARRESS-HF is a multicenter, prospective, randomized, controlled trial comparing slow continuous venovenous ultrafiltration to stepped pharmacologic care in patients admitted to the hospital with a primary diagnosis of ADHF who develop cardiorenal syndrome. This trial is part of the Heart Failure Clinical Research Network sponsored by the National Heart, Lung, and Blood Institute (NHLBI; clinicaltrials.gov identifier NCT00608491) and is being performed at 9 regional clinical centers and 5 additional centers invited to participate by the steering committee. All study-related activities are being coordinated by the Data Coordinating Center at the Duke Clinical Research Institute in Durham, North Carolina.
Objectives
The primary hypothesis of CARRESS-HF is that ultrafiltration results in improved renal function and relief of congestion compared with stepped pharmacologic care when assessed 96 hours after randomization in patients with ADHF and cardiorenal syndrome. Some of the prespecified secondary objectives are listed in Table 1.
Table 1.
Secondary Objectives of CARRESS-HF
|
Assessments at multiple time points include the following: Change in electrolytes will be assessed at 96 hours and 1 week; change in creatinine, blood urea nitrogen, and estimated glomerular filtration rate will be assessed at 96 hours, 1 week, and 30 and 60 days; change in C-reactive protein will be assessed at 96 hours, 1 week, and 60 days; change in weight will be assessed daily until discharge or day 7, whichever comes first, and 30 and 60 days; change in B-type natriuretic peptide will be assessed at 96 hours, 1 week, and 60 days; clinical decongestion will be assessed at 96 hours, 1 week, and 30 and 60 days.
Patient Population, Inclusion and Exclusion Criteria
This study was approved by an NHLBI-appointed Protocol Review Committee and Data and Safety Monitoring Board and by the local Institutional Review Boards of each participating site. Each patient must provide informed consent before enrollment. Outpatients are not eligible for this study. Only patients admitted to the hospital with a primary diagnosis of ADHF (regardless of ejection fraction) are eligible for enrollment and all patient must experience worsening renal function (defined as an increase in serum creatinine of ≥0.3 mg/dL from baseline) while demonstrating signs and symptoms of persistent congestion (Table 2). Worsening renal function can be documented up to 6 weeks before admission in the setting of escalating doses of diuretics or, if this information is unavailable, up to 7 days after admission.
Table 2.
Inclusion and Exclusion Criteria
Inclusion Criteria
|
Exclusion Criteria
|
Randomization and Treatment Interventions
Patients are randomized to the 2 treatment arms in a 1-to-1 fashion through an automated web-based system. The randomized allocations are based on a permuted block randomization scheme stratified by clinical site.
All patients are started on 2 L/d fluid restriction and 2 g/d sodium restriction. Decisions regarding the use of standard heart failure medications, such as angiotensin-converting enzyme inhibitors, beta-blockers, and digoxin, are left to the discretion of the treating physicians. However, investigators are encouraged to decrease the doses of these drugs if cardiorenal syndrome develops in temporal association with dose escalations.
Ultrafiltration
All loop diuretics are discontinued at the time of randomization and for the duration of the ultrafiltration intervention. Fluid status is managed exclusively by ultrafiltration using the Aquadex System 100 (CHF Solutions, Brooklyn Park, Minnesota) according to the manufacturer's specifications. The Aquadex System 100 is a simplified ultrafiltration device the size and weight of which is similar to a standard intravenous fluid pump. Blood is removed from the patient through an intravenous catheter at a maximum rate of 40 mL/min and a maximum filtration rate of 500 mL/h. The console monitors blood flow through the tubing and the blood circuit, alerting the user to abnormal conditions such as the obstruction of blood flow or air in the circuit. Operating the device requires the same nursing skill level and the amount of monitoring as that necessary for a blood transfusion and can be performed in the setting of an intensive care unit/cardiac care unit or monitored hospital floor.10
Ultrafiltration is initiated at a fluid removal rate of 200 mL/h after the placement of appropriate intravenous access and continued until the patient's signs and symptoms of congestion are optimized. The use of vasodilators or positive inotropic agents is prohibited unless deemed necessary for rescue therapy.
Ultrafiltration can be performed through the use of 2 peripheral intravenous catheters, a combination of an extended-length catheter placed in the antecubital fossa and a standard peripheral intravenous catheter, or, in some circumstances, a single dual-lumen peripheral intravenous catheter. Although central venous access is not necessary, it is sometimes acquired in patients hospitalized with ADHF, especially those who develop cardiorenal syndrome. In these instances, ultrafiltration can be performed using the introducer sheath or a triple-lumen catheter according to the manufacturer's specifications.
During ultrafiltration, patients receive heparin to achieve an activated partial thromboplastin time (PTT) 2.0—2.5 times normal to prevent clotting of the ultrafiltration circuit.
Justification for Ultrafiltration “Prescription”
A fluid removal rate of 200 mL/h applied for 24 hours results in 4.8 L fluid removal and a measureable net negative fluid balance of ~3.4 L, assuming the patient adheres to the 2 L fluid restriction mandated per protocol and produces at least 600 mL urine. These parameters were selected to maximize the likelihood that this degree of fluid removal will be well tolerated. In the UNLOAD trial, the average ultrafiltration rate was 241 mL/h over an average of 12.3 hours, resulting in ~3 L plasma water removal.17 This rate of fluid removal was well tolerated with no significant adverse hemodynamic effects and no significant difference in the percentage of patients who ultimately developed worsening renal function between the ultrafiltration and standard care groups. Marenzi et al11 measured the plasma refill rate (the rate of fluid volume transport from the interstitium to the intravascular space during ultrafiltration) in heart failure patients undergoing ultrafiltration at a rate of 530 mL/h for an average of 9 hours. The plasma refill rate began to drop after 4 L fluid removal but was still in excess of 400 mL/h. Therefore, it is anticipated that patients with significant persistent congestion as defined by the inclusion criteria should tolerate the ultrafiltration rate of 200 mL/h.
Stepped Pharmacologic Care
Intravenous diuretics are used to address signs and symptoms of congestion. To prevent heterogeneity in the treatment approach used for these patients and to ensure the use of appropriate diuretic doses, a stepped care algorithm developed by the Heart Failure Clinical Trials Network is provided to investigators (Table 3). At the time of randomization to stepped pharmacologic care, investigators are encouraged to decrease, increase, or continue current doses of diuretics depending on urine output and clinical response. This assessment is to be repeated daily until the signs and symptoms of congestion have been optimized. If signs and symptoms of congestion persist after the 96-hour end point, the stepped pharmacologic care algorithm should continue to be used as a guideline for ongoing treatment. Recommendations regarding the use of vasodilators and inotropes in the stepped pharmacologic care algorithm are based on blood pressure, ejection fraction, and the presence of right ventricular failure at 48 hours if urine output remains suboptimal. Investigators are encouraged to consider additional approaches such as hemodynamic-guided intravenous therapy, advanced mechanical support, dialysis, or ultrafiltration crossover at 72 hours and 96 hours if congestion persists and there is still inadequate urine output.
Table 3.
Stepped Pharmacologic Care Treatment Algorithm
| Urine output (UO) goals to be assessed daily from randomization to 96 hours |
| UO > 5 L/d → Reduce current diuretic regimen if desired |
| UO 3–5 L/d → Continue current diuretic regimen |
| UO < 3 L/d → See diuretic grid |
| 24-hour assessment |
| UO recommendations as above |
| Advance to next step on grid if UO < 3 L/d |
| 48-hour assessment |
| UO recommendations as above |
| Advance to next step on grid if UO < 3 L/d |
| Consider dopamine or dobutamine at 2 μg/kg/h if SBP < 110 mm Hg and EF <40% or RV systolic dysfunction. |
| Consider nitroglycerin or nesiritide if SBP > 120 mm Hg (any EF) and severe symptoms |
| 72- and 96-hour assessments |
| UO recommendations as above |
| Advance to next step on grid if UO < 3 L/d |
| Consider dopamine or dobutamine at 2 μg/kg/hr if SBP < 110 mm Hg and EF <40% or RV systolic dysfunction. |
| Consider nitroglycerin or nesiritide if SBP > 120 mm Hg (any EF) and severe symptoms |
| Consider hemodynamic guided IV therapy, LVAD, dialysis, or ultrafiltration crossover |
| Diuretic Grid | |||
|---|---|---|---|
| Suggested Dose |
|||
| Current Dose | Daily Loop Dose | Thiazide | |
| A | <80 mg | 40 mg IV bolus + 5 mg/h | None |
| B | 81–160 mg | 80 mg IV bolus + 10 mg/h | 5 mg metolazone once daily |
| C | 161–240 mg | 80 mg IV bolus + 20 mg/h | 5 mg metolazone twice daily |
| D | >240mg | 80 mg IV bolus + 30 mg/h | 5 mg metolazone twice daily |
SBP, systolic blood pressure; EF, ejection fraction; RV, right ventricle; LVAD, left ventricular assist device; Loop, loop diuretic dose in furosemide equivalents.
Stopping Points for Randomized Interventions
There is no predetermined treatment duration; treatment is continued in both treatment arms until the signs and symptoms of congestion are optimized and there is no ongoing need for ultrafiltration or intravenous diuretics. Careful clinical monitoring is necessary in all patients with ADHF to maintain hemodynamic stability and reduce the likelihood of intravascular volume depletion. Vital signs, physical examination, symptoms, blood urea nitrogen, creatinine, basic electrolytes, and right atrial and pulmonary capillary wedge pressures, when available, will be assessed daily to assist in determining the optimal volume status for patients in both treatment arms. Ultrafiltration rates and the doses of diuretics may be decreased or temporarily discontinued at the discretion of the treating physician if there is a decrease in blood pressure or an increase in creatinine that is thought to be due to a transient episode of intravascular volume depletion. After the patient has stabilized, if congestion persists based on review of all available clinical data, the randomized treatment intervention (ultrafiltration or stepped pharmacologic care) is reinitiated until the patient's fluid status has been optimized. There is no need to reestablish the entry criteria for episodes of interrupted decongestive therapy. The transition to oral diuretics before discharge is left to the discretion of the treating physician and is continued in the outpatient setting as needed to maintain optimal fluid homeostasis. The primary end point of change in weight and change in creatinine will be assessed 96 hours after enrollment whether or not the randomized intervention has been completed.
Outcome Determinations and Statistical Considerations
The primary end point of this study is change in weight and change in creatinine from baseline to 96 hours. This bivariate response will be displayed on a two-dimensional grid with individual data points for each patient representing paired changes in both creatinine and weight 96 hours after randomization (Fig. 1). A confidence region for the average difference between treatment arms in this bivariate response can be described as an ellipse, and the 2 treatment arms will be compared statistically with the use of the Hotelling T-square, which is a multivariate analog of the 2-sample t test used with a single continuous variable.20
Fig. 1.
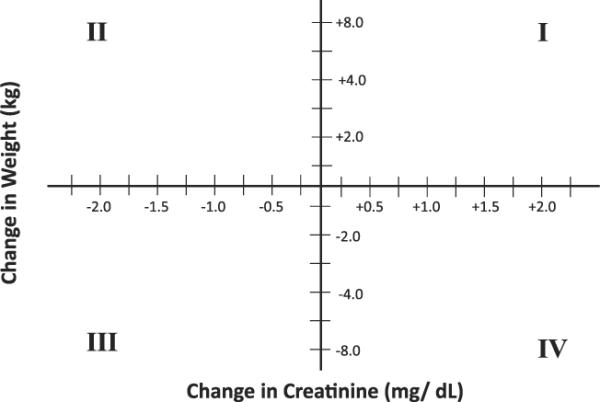
Two-dimensional grid for the primary end point of change in weight and change in creatinine 96 hours after enrollment. Each study subject's change in weight and change in creatinine will be plotted on the figure such that subjects in quadrant I will represent those with increased weight and increased creatinine and subjects in quadrant III will represent those with weight loss and a reduction in creatinine.
This novel bivariate end point was selected to reflect the importance of both decongestion and improved renal function in treating patients with decompensated heart failure. It allows for the integration of clinically important outcomes that may be in “opposite directions.” Weight loss is a measure of successful volume reduction therapy and is a desirable treatment outcome, whereas worsening renal function, as measured by an increase in creatinine, is an adverse outcome that often complicates volume reduction therapy. Evaluating these 2 important responses to treatment as a bivariate end point reflects clinically important responses to therapy and avoids the requirement of making adjustments in sample size to prevent a type 1 error that would be necessary if the end points were considered separately.21
The null hypothesis is that there is no difference between the treatment groups in this 2-dimensional end point. Based on data from the UNLOAD study,17 the standard deviation (SD) of change in weight at 96 hours is estimated to be 3.1—3.5 kg, and the SD of change in creatinine at 96 hours is estimated to be 0.55—0.75 mg/dL. A sample size of 100 patients per treatment arm will provide 90% power for detecting a difference between treatment groups in each of the primary end point variables (change in weight and change in creatinine at 96 hours) of one-half SD unit. Thus, if the SD of weight loss is 3.5 kg, or even as high as 4.0 kg, the study will have 90% power for detecting an average weight loss difference between groups of 2.0 kg. If the SD of change in creatinine is 0.6—0.7 mg/dL, the study will have 90% power to detect a difference between groups of 0.3—0.35 mg/dL. One hundred patients per arm will also provide adequate power for selected secondary end points of interest, such as net fluid loss and treatment failure. Assuming that the SD of net fluid loss over 96 hours is consistent with the recently published Diuretic Strategies in Patients with Acute Decompensated Heart Failure (DOSE) trial22 (~3,000 mL) the study will have >90% power for detecting a difference between arms of ≥1,000 mL. If the rate of treatment failure (defined in Table 1) in the stepped-care arm is ≥40% (consistent with the DOSE trial) 200 patients will provide 80% power for detecting a 50% reduction. This same power would apply also for an end point such as rehospitalization.
The primary end point measured at 96 hours will be analyzed on an intention-to-treat basis. Temporary interruptions of ultrafiltration or stepped pharmacologic care to address episodes of transient intravascular volume depletion are permitted in accordance with standard clinical practice; there is no separate analysis planned to account for these adjustments in volume reduction therapies. It is anticipated that there may be some crossovers from stepped pharmacologic care to ultrafiltration or from ultrafiltration to stepped pharmacologic care before the 96-hour end point. The number of crossovers will be documented to provide context for interpreting the primary results; however, treatment crossovers before the 96-hour assessment will be analyzed according to the intention-to-treat principle and thus will be included in the arm to which they were randomized. A supplementary analysis will be performed censoring patient measurements after the time of crossover to ultrafiltration or stepped pharmacologic care and carrying forward change in weight and change in creatinine at the time of crossover to the 96-hour primary end point. Safety end points are reported to and monitored by the Coordinating Center and an independent Data and Safety Monitoring Board appointed by the NHLBI.
Current Status
Enrollment began in June 2008, and there were 180 patients randomized in CARRESS-HF by Nov 7, 2011. At the current rate at which patients are being recruited in the trial, target enrollment should be reached in the spring of 2012.
Conclusions
Worsening renal function occurs in 20%–30% of patients hospitalized with ADHF and is associated with poor outcomes. The clinical challenge of adequately addressing signs and symptoms of congestion is complicated by worsening renal function. There are no safety or efficacy data supporting common treatment approaches in this clinical setting, such as deescalation or intensification of loop diuretics, positive inotropes, other vasoactive drugs, or ultrafiltration. CARRESS-HF compares treatment strategies (ultrafiltration vs stepped pharmacologic care) for the management of worsening renal function in patients with ADHF. The results of the CARRESS-HF trial are expected to provide information and evidence as to the most appropriate approaches for treating this challenging patient population.
Acknowledgments
The authors acknowledge the contributions of Dr Lynn Warner Stevenson for her contributions to the overall CARRESS-HF study design and for her role in the development of the stepped pharmacologic care algorithm; Drs Eric Velazquez and Elizabeth Ofili for their role on the Publications and Presentations Committee of the Heart Failure Clinical Research Network; Dr Adrian Hernandez and the rest of the staff at the Duke Clinical Research Institute for their roles organizing this study at the Coordinating Center; and the members of the National Institutes of Health Protocol Review Committee and Data and Safety Monitoring Board assigned to this project for the Heart Failure Clinical Trials Network.
Funding: The Heart Failure Clinical Research Network is funded by the National Heart, Lung, and Blood Institute. Additional support provided by CHF Solutions in partnership with the NHLBI.
Clinical Trial Registration: Clinicaltrials.gov identifier NCT00608491.
Footnotes
Disclosures B Bart has served as an unpaid consultant for CHF Solutions.
S Goldsmith has received honoraria from CHF Solutions. All of the other authors report no potential conflicts of interest.
References
- 1.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–39. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 2.Butler J, Forman DE, Abraham WT, Gottlieb SS, Loh E, Massie BM, et al. Relationship between heart failure treatment and development of worsening renal function among hospitalized patients. Am Heart J. 2004;147:331–8. doi: 10.1016/j.ahj.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 3.Forman DE, Butler J, Wang Y, Abraham WT, O'connor CM, Gottlieb SS, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43:61–7. doi: 10.1016/j.jacc.2003.07.031. [DOI] [PubMed] [Google Scholar]
- 4.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Secular trends in renal dysfunction and outcomes in hospitalized heart failure patients. J Card Fail. 2006;12:257–62. doi: 10.1016/j.cardfail.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Testani JM, Chen J, McCauley BD, Kimmel SE, Shannon RP. Potential effects of aggressive decongestion during the treatment of decompensated heart failure on renal function and survival. Circulation. 2010;122:265–72. doi: 10.1161/CIRCULATIONAHA.109.933275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bock JS, Gottlieb SS. Cardiorenal syndrome: new perspectives. Circulation. 2010;121:2592–600. doi: 10.1161/CIRCULATIONAHA.109.886473. [DOI] [PubMed] [Google Scholar]
- 7.Ali SS, Olinger CC, Sobotka PA, Dahle TG, Bunte MC, Blake D, et al. Loop diuretics can cause clinical natriuretic failure: a prescription for volume expansion. Congest Heart Fail. 2009;15:1–4. doi: 10.1111/j.1751-7133.2008.00037.x. [DOI] [PubMed] [Google Scholar]
- 8.Agostoni P, Marenzi G, Lauri G, Perego G, Schianni M, Sganzerla P, et al. Sustained improvement in functional capacity after removal of body fluid with isolated ultrafiltration in chronic cardiac insufficiency: failure of furosemide to provide the same result. Am J Med. 1994;96:191–9. doi: 10.1016/0002-9343(94)90142-2. [DOI] [PubMed] [Google Scholar]
- 9.Agostoni PG, Marenzi GC, Pepi M, Doria E, Salvioni A, Perego G, et al. Isolated ultrafiltration in moderate congestive heart failure. J Am Coll Cardiol. 1993;21:424–31. doi: 10.1016/0735-1097(93)90685-t. [DOI] [PubMed] [Google Scholar]
- 10.Jaski BE, Ha J, Denys BG, Lamba S, Trupp RJ, Abraham WT. Peripherally inserted veno-venous ultrafiltration for rapid treatment of volume overloaded patients. J Card Fail. 2003;9:227–31. doi: 10.1054/jcaf.2003.28. [DOI] [PubMed] [Google Scholar]
- 11.Marenzi G, Lauri G, Grazi M, Assanelli E, Campodonico J, Agostoni P. Circulatory response to fluid overload removal by extra-corporeal ultrafiltration in refractory congestive heart failure. J Am Coll Cardiol. 2001;38:963–8. doi: 10.1016/s0735-1097(01)01479-6. [DOI] [PubMed] [Google Scholar]
- 12.Ronco C, Ricci Z, Bellomo R, Bedogni F. Extracorporeal ultrafiltration for the treatment of overhydration and congestive heart failure. Cardiology. 2001;96:155–68. doi: 10.1159/000047399. [DOI] [PubMed] [Google Scholar]
- 13.Guazzi MD, Agostoni P, Perego B, Lauri G, Salvioni A, Giraldi F, et al. Apparent paradox of neurohumoral axis inhibition after body fluid volume depletion in patients with chronic congestive heart failure and water retention. Br Heart J. 1994;72:534–9. doi: 10.1136/hrt.72.6.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Firth JD, Raine AE, Ledingham JG. Raised venous pressure: a direct cause of renal sodium retention in oedema? Lancet. 1988;1:1033–5. doi: 10.1016/s0140-6736(88)91851-x. [DOI] [PubMed] [Google Scholar]
- 15.Mullens W, Abrahams Z, Francis GS, Sokos G, Taylor DO, Starling RC, et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009;53:589–96. doi: 10.1016/j.jacc.2008.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jessup M, Costanzo MR. The cardiorenal syndrome: do we need a change of strategy or a change of tactics? J Am Coll Cardiol. 2009;53:597–9. doi: 10.1016/j.jacc.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 17.Costanzo MR, Guglin ME, Saltzberg MT, Jessup ML, Bart BA, Teerlink JR, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007;49:675–83. doi: 10.1016/j.jacc.2006.07.073. [DOI] [PubMed] [Google Scholar]
- 18.Kazory A, Ejaz AA, Ross EA. The UNLOAD trial: a “nephrologic” standpoint. J Am Coll Cardiol. 2007;50:820. doi: 10.1016/j.jacc.2007.04.070. [DOI] [PubMed] [Google Scholar]
- 19.Kazory A, Ross EA. Contemporary trends in the pharmacological and extracorporeal management of heart failure: a nephrologic perspective. Circulation. 2008;117:975–83. doi: 10.1161/CIRCULATIONAHA.107.742270. [DOI] [PubMed] [Google Scholar]
- 20.Hotelling H. The generalization of Student ratio. Ann Math Stat. 1931;2:360–78. [Google Scholar]
- 21.Zanolla L, Zardini P. Selection of endpoints for heart failure clinical trials. Eur J Heart Fail. 2003;5:717–23. doi: 10.1016/s1388-9842(03)00101-6. [DOI] [PubMed] [Google Scholar]
- 22.Felker GM, Lee KL, Bull DA, Redfield MM, Stevenson LW, Goldsmith SR, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364:797–805. doi: 10.1056/NEJMoa1005419. [DOI] [PMC free article] [PubMed] [Google Scholar]


