Abstract
Canada is facing cancer crisis. Cancer has become the leading cause of death in Canada. Despite recent advances in cancer management and research, growing disparities in cancer care have been noticed, especially in socio-economically disadvantaged groups and under-served communities. With the rising incidence of cancer and the increasing numbers of minorities and of social disparities in general, and without appropriate interventions, cancer care disparities will become only more pronounced. This paper highlights the concepts and definitions of equity in health and health care and examines several health determinants that increase the risk of cancer. It also reviews cancer care inequity in the high-risk groups. A conceptual framework is proposed and recommendations are made for the eradication of disparities within the health care system and beyond.
Keywords: Cancer care, disparity, inequity, Canadian health care
1. INTRODUCTION
Cancer is the one of the major causes of death throughout the world, second only to the cardiovascular diseases. Every year about 10 million new cancer patients are diagnosed1. More than 16 million new cancer cases are expected by 2020, and it is estimated that cancer will then be the cause of more than 10 million deaths annually2. Canada is facing a cancer crisis. According to the Canadian Cancer Society, 40% of men and 45% of women are expected to develop cancer during their lifetime, and 24% and 29% respectively, to die from their disease3.
Many years of advancement in cancer research have led to the development of sophisticated screening and treatment methods that have contributed to significant improvements in the outcomes of people living with cancer. However, growing disparities in cancer care have been noticed, especially in socioeconomically disadvantaged groups and under-served communities. Disparities in cancer care result in presentations that are more advanced and outcomes that are substantially inferior in some groups4,5. Such disparity is not unexpected in developing countries, given the complexity and cost of modern cancer treatment. However, inequities in cancer care and differential cancer outcomes in socially disadvantaged groups in the United States and Canada warrant further investigation, because both countries have well-developed health care systems. In contrast to the United States, where inadequate health insurance coverage accounts for substantial disparity in cancer care, Canada offers universal health care to its citizens. A gap in cancer outcomes is nevertheless perceivable between various ethnic and social groups.
Health disparities not only result in avoidable death, disease, disability, anguish, and discomfort, but are also harmful for the health system and for Canadian society as a whole. Health disparities are not in harmony with Canadian values; they threaten the cohesiveness of society, weaken the sustainability of the health system, and damage the economy.
The present paper provides a Canadian perspective of disparities in cancer care. It begins with the concepts and definitions of equity in health and health care, and it then examines several health determinants that are associated with increased risk of cancer and differential outcomes in disadvantaged groups. A conceptual framework is proposed, and recommendations are made to eliminate disparities both within the health care system and beyond its confines.
2. DEFINITION AND CONCEPT OF HEALTH INEQUITY
2.1. What Is Health and Equity?
The World Health Organization6 defines “health” as a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. “Equity” means that people’s needs, rather than their social privileges, guide the distribution of opportunities for well-being.
2.2. Equity in Health and Health Care
Equity in health implies that “ideally everyone should have a fair opportunity to attain their full health potential and, more pragmatically, that no one should be disadvantaged from achieving this potential, if it can be avoided”6. Hence, equity in health means reducing avoidable gaps in health status and health services between groups with different levels of social privilege7.
Equity in health care is defined as equal access to available care for equal need, equal utilization for equal need, and equal quality of care for all8–10. The International Society for Equity in Health defines equity in health as “the absence of systematic and potentially remediable differences in one or more aspects of health across populations or population subgroups defined socially, economically, demographically, or geographically”11.
Health inequity is a difference that finds poor people, racial or ethnic minorities, or other socially disadvantaged groups systematically experiencing worse health than more advantaged social groups12.
3. UNDERSTANDING THE NATURE AND CAUSE OF DISPARITIES
There are at least 4 different ways that societies can create health inequities:
Social stratification
Exposure to risks
Vulnerabilities
Consequences (that is, differential access to health services or other social programs)
Inequity in cancer care takes place at various levels: primary and secondary prevention, diagnosis, treatment, and cancer research. Ensuring equitable access to cancer care is vital because of the time sensitivity of care and evolving complex treatment. Early diagnosis and prompt management are paramount in cancer care—hence, the more dramatic implications of poor access in that context. In the subsections that follow, we highlight various cancer risk factors and examine high-risk groups in the context of understanding the nature of health disparities.
4. CANCER RISK FACTORS
There is ample evidence that most malignant disorders are environmentally driven and preventable13. Implementation of policies and programs for equal opportunity will require reliable and comparable analyses of the effect of cancer risk factors on various groups. More importantly, primary prevention through lifestyle modification and environmental interventions addressing various health determinants may offer the most cost-effective approach to reducing the cancer burden. Given that the many risk factors discussed in the subsections that follow are common to other diseases, it is conceivable that controlling such risk factors will have a positive impact on population health.
4.1. Smoking
Smoking is the leading cause of preventable death in the world, killing 5 million people every year. It is causally related to various malignancies, including lung, head-and-neck, upper gastrointestinal tract, and genitourinary cancers. Although smoking prevalence in Canada has continually declined, 17% of the Canadian population 15 years of age and older are current smokers14.
Tobacco use is strongly associated with low socio-economic status (ses)15. The prevalence of current smoking is greatest among adults with working-class jobs, low education levels, and low income or unemployment16,17.
4.2. Alcohol
There is an ample evidence of a correlation between chronic alcohol consumption and the development of cancer, including the upper aerodigestive tract and liver cancers. In addition, alcohol increases the risk for colorectal and breast cancer18,19. There is evidence that certain subgroups of the population, including socio-economically disadvantaged individuals, experience greater levels of alcohol-related death20,21.
4.3. Nutrition and Physical Activity
There is growing evidence that high body mass index and obesity and low physical activity, coupled with high intake of fat, meat, and dairy products, play an important role in the development of several malignancies, such as colorectal cancer, breast cancer, uterine cancer, and prostate cancer22,23. The higher risk of cancer in disadvantaged groups can be linked to food insecurity and meager access to elements of a healthy diet such as fresh fruits and vegetables and to facilities for physical fitness.
4.4. Sexual Behavior and Reproductive Health
Cervical cancer remains the third most common cancer among Canadian women 20–49 years of age. It is estimated that 10%–30% of the Canadian adult population is infected with the human papilloma virus, the main causal agent of cervical cancer24. Aboriginal youth are at an increased risk of unprotected sexual activity and, therefore, sexually transmitted infections and future risk of cancer25. Differences in sexual and reproductive behavior across socioeconomic groups and in access to vaccination against the human papilloma virus have been implicated as a cause of variation in the incidence rates of cervical cancer by ses.
4.5. Environmental Pollution
Environmental pollutants such as contaminants of air and water are known to be associated with an increased risk of cancer. There is evidence that individuals from lower social classes are exposed to higher levels of environmental pollutants than are individuals from higher social classes26.
5. HIGH-RISK POPULATIONS
It is known that cancer care disparities are not random, but rather differentially distributed among high-risk groups. Inequities in access to cancer services along the cancer care continuum, from screening to end-of-life care, are linked to a variety of socioeconomic, geographic, and demographic factors. The research on inequity in cancer care in Canada is sparse, and the quantity of research on access to care varies by point of service, equity determinates, and disease site27. Barriers to access can be sorted into 4 categories: availability of services, financial barriers, nonfinancial barriers to presentation of health care needs, and barriers to equitable treatment. In the subsections that follow, we review the evidence of disparities in various high-risk groups.
5.1. Socio-economic Status
Socio-economic status is typically measured based on educational achievement, occupational characteristics, income, accumulated wealth, living conditions, health insurance, or residence in geographic areas with particular social or economic conditions28–30. Socio-economic factors account for an estimated 50% of a person’s health status; health care service accounts for 25%31. The Canadian Council on Social Development reported that an estimated 4,886,000 people were living in poverty in 199932.
There is abundant evidence that ses is strongly related to access to and quality of preventive care, ambulatory care, and high-technology procedures31–33. A striking and consistent association between ses and various cancer risk factors such as smoking, physical inactivity, a less nutritious diet, and heavy alcohol consumption has been noted34. Apart from logistics barriers to access, people of lower ses are more likely to remain uninformed about early detection programs and disease management. In general, a lower ses is related to a lower health status, more health problems, and a shorter life expectancy.
5.2. Rural Residence
In 2006, approximately 6 million Canadians were living in small towns and rural areas35. According to a Canadian Institute of Health Information report, the average life expectancy of rural Canadians lags behind that of their urban counterparts36.
Rural cancer patients have additional burdens unique to their residence, such as interference with family life, work, and financial security, which ultimately may influence quality of life differently than similar burdens do for residents in urban areas37. Access to treatment or decisions about treatment can also be affected by rural residence38.
It is also important to recognize that several characteristics of rural communities may be of benefit to individuals coping with cancer, such as close relationships with family, community members, and religious institutions39,40.
5.3. Ethnic Minorities and Immigrants
For many diseases, racial and ethnic minority populations are less likely to receive health care equal to that received by non-minority individuals. Factors that potentially contribute to the inferior cancer outcomes in ethnic minorities are poverty, lack of access to care, personal attitudes and beliefs, cultural issues, intercurrent medical problems, education, linguistic and literacy barriers, and poor expectations of cancer treatment outcome.
Between 1996 and 2006, the Aboriginal population increased by 45% compared with 8% for the non-Aboriginal population. In general, Aboriginal peoples experience more health-related problems than do non-Aboriginal people. Several Aboriginal health-related problems are linked to living conditions on reserves and the lower average income of Aboriginal people compared with that of other Canadians. Being no exception, cancer incidences—specifically, the incidences for preventable cancers such as lung cancer—are on the rise in Aboriginal populations, and survival after a diagnosis of cancer is poorer in those populations than in the general population41. For instance, in Ontario, although the rate of new cases of all types of cancer is generally lower in Aboriginal populations, incidence rates are similar or higher for lung, colorectal, kidney, and cervical cancers42.
Immigrants represent about 20% of the total population43. The general health of new immigrants is better on arrival than that of the average Canadian, but it tends to decline with time. Immigrants underutilize screening and prevention services. Different patterns of cancer incidence, mortality, and outcome have been noted among ethnic populations compared with the general population44.
5.4. Gender
It has been suggested that health is detrimentally affected by gender roles and statuses as they intersect with economic disparities, cultural, sexual, physical, and historical marginalization, and the strains of domestic and paid labour45. Although differential cancer outcomes have been reported in relation to gender46,47, Canadian research explicitly focusing on gender inequalities in cancer care is scarce.
6. RECOMMENDATIONS FOR ACTION
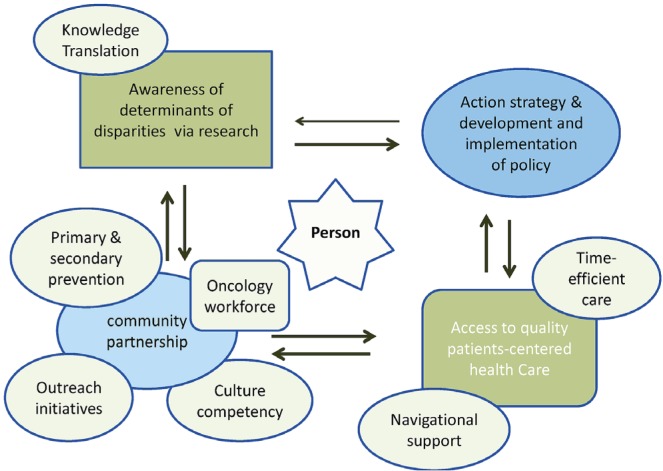
Eliminating cancer care disparities will require commitment to explore the extent of those disparities, to develop evidence-based policies that address root causes and major determinants of disparity, and to commit to ongoing assessments of interventions. Disparities in all aspects of health care should be investigated, including allocation of resources for health care, actual receipt of services, and quality of the services. We propose a conceptual framework to promote equity in cancer care, thereby improving population health (Figure 1). Its major components include research and application of that research to the development of strategies and policies, cultural competency, community partnership, and patient-centered care (Table i).
FIGURE 1.
Proposed framework to eliminate cancer care disparities.
TABLE I.
Potential interventions to reduce disparities in cancer care
| Intervention | Recommendations |
|---|---|
| Action strategies | Address the health gradient in high-risk groups with respect to poverty, rural or remote location, language, and cultural barriers. |
| Promote primary and secondary cancer prevention by addressing key population health determinants. | |
| Research | Integrate important determinants of health such as demographic, cultural, and socio-economic contextual variables into the cancer databases. |
| Conduct focused research on cancer disparities, with ongoing surveillance. | |
| Involve diverse populations in clinical trials. | |
| Partnership | Partner with public, private, and volunteer programs and organizations and engage the active participation of diverse communities. |
| Incorporate a diverse oncology workforce in cancer care to meet the needs of racially and ethnically diverse patients. | |
| Person-centered care | Integrate person-centred, time-efficient, and quality care with navigational support that responds to the physical, social, emotional, informational, psychological, spiritual, and practical needs of patients. |
6.1. Action Strategies
Action strategies are required to address the health gradient across disadvantaged groups because of factors such as poverty, rural or remote location, and language and cultural barriers, thereby eliminating systemic barriers to quality cancer care and control. The current system of care is inadequate in addressing primary prevention and screening services and, thus, cancer control. Integrated concepts and innovative strategies related to population health determinants are important not only for a healthy population, but also to reduce the rising costs of health care.
6.2. Research
Enhanced support for research on cancer disparities and ongoing surveillance to assess the magnitude and pattern of health gaps over time in relation to policies that influence population health are critical. Information about important determinants of health such as demographic, cultural, and socio-economic contextual variables within cancer databases is vital to quality research and to the effectiveness of monitoring in a cancer control program. Furthermore, increased participation of racially and ethnically diverse populations in clinical trials is essential for reducing cancer care disparity.
6.3. Community, Organizations, and Health Sector Partnerships
Appropriate consultation with cultural and patient communities is crucial in cancer control and decision-making processes. A growing body of evidence consistently points to the importance of social connectedness, a nurturing community, and social networks in quality of life and cancer outcomes. Partnerships with public, private, and volunteer organizations and participation of community members are keys to success. Organizations such as the Canadian Partnership Against Cancer (http://www.partnershipagainstcancer.ca) are currently working with other groups across Canada to generate new knowledge and to accelerate the implementation of existing knowledge about cancer control. Networking and coordination with other programs and agencies for chronic disease or healthy living within the health regions and across the provinces are fundamental for effective action, organization of shared services, and avoidance of duplication.
6.4. Cultural Competency
Cultural competency is a fundamental element of an equitable system of care that respects the health beliefs, values, and behaviors of individuals and that enables the system to work effectively in cross-cultural situations. Incorporation of cultural competency as a core value into every public health institution at the individual and systemic levels is vital48,49. Removal of language barriers and increased training of the oncology workforce to meet the needs of racially and ethnically diverse cancer patients are keys to reducing disparities.
6.5. Access to Quality Person-Centred Care
Because the cancer experience can be very distressing, integrated person-centered quality care that responds to the physical, social, emotional, informational, psychological, spiritual, and practical needs of patients is vital. Enhanced patient involvement in care and navigational support are essential to ensuring coordination and continuity of care. Universal access to cancer treatment across Canada is imperative for equity. Hence, the Pan-Canadian Oncology Drug Review Program (http://www.pcodr.ca) is an important step toward promoting equal access to cancer treatment for all Canadians.
7. SUMMARY
Cancer treatment is complex, often involving various services, multiple health care professionals, and multiple settings. Such complexity makes provision of equitable care a challenge and necessitates a clear understanding of the root causes of disparities in cancer care. Broad community involvement, better understanding of and respect for the psychosocial and cultural beliefs of ethnic minorities, improvements in life circumstances, social support, increased community health education, outreach initiatives, encouragement of trust in the health system, and partnership against cancer are all keys (Table ii) to eliminating inequity in cancer care.
TABLE II.
Key points
| Cancer is a leading cause of death in Canada. |
| Cancer care gradient across Canada is an important population health determinant. |
| Socio-economic disadvantage groups, rural residents, Aboriginal, other ethnic minorities and immigrants are especially at high risk of disparity in cancer care. |
| Smoking, alcohol, food insecurity, lack of fitness, poverty, lack of access to care, attitudes and beliefs, inter-current medical problems, education, linguistic and literacy barriers, poor expectations of outcome of cancer treatment are potential factors lead to disparity. |
| Commitment to explore the extent of disparities, development of policies to address root causes, broad community involvement, better understanding and respect of psycho-social and cultural beliefs of ethnic minorities, improving life circumstances, building a trust of health system are all key to eliminate inequity in cancer care. |
8. ACKNOWLEDGMENT
The authors thank Dr. Bonnie Janzen of the Department of Community Health and Epidemiology at the University of Saskatchewan for helpful comments.
9. CONFLICT OF INTEREST DISCLOSURES
The authors have no financial conflicts of interest to disclose.
10. REFERENCES
- 1.Ferlay J, Bray F, Pisani P, Parkin DM. globocan 2002: cancer incidence, mortality and prevalence worldwide . International Agency for Research on Cancer (iarc) CancerBase No. 5, Ver. 2.0. Lyons, France: IARC Press; 2004. [Google Scholar]
- 2.United States, Department of Health and Human Services, Centers for Disease Control and Prevention (cdc) The Global Cancer Atlas Online [Web resource] Atlanta, GA: CDC; n.d. [Available online at: http://apps.nccd.cdc.gov/dcpcglobalatlas/Default.aspx; cited March 1, 2012] [Google Scholar]
- 3.Canadian Cancer Society’s Steering Committee on Cancer Statistics. Canadian Cancer Statistics 2012. Toronto, ON: Canadian Cancer Society; 2012. [Available for download at: http://www.cancer.ca/canada-wide/about%20cancer/cancer%20statistics.aspx; cited March 1, 2012] [Google Scholar]
- 4.Groman R, Ginsburg J, on behalf of the American College of Physicians Racial and ethnic disparities in health care: a position paper of the American College of Physicians. Ann Intern Med. 2004;141:226–32. doi: 10.7326/0003-4819-141-3-200408030-00015. [DOI] [PubMed] [Google Scholar]
- 5.Sheppard AJ, Chiarelli AM, Marrett LD, Mirea L, Nishri ED, Trudeau ME, on behalf of the Aboriginal Breast Cancer Study Group Detection of later stage breast cancer in First Nations women in Ontario, Canada. Can J Public Health. 2010;101:101–5. doi: 10.1007/BF03405573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whitehead M. The Concepts and Principles of Equity and Health. Copenhagen, Demark: World Health Organisation Regional Office for Europe; 1990. [Google Scholar]
- 7.Braveman P, Starfield B, Geiger HJ. World Health Report 2000: how it removes equity from the agenda for public health monitoring and policy. BMJ. 2001;323:678–81. doi: 10.1136/bmj.323.7314.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dahlgren G, Whitehead M. Policies and Strategies to Promote Equity in Health. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1992. [Google Scholar]
- 9.Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22:429–45. doi: 10.2190/986L-LHQ6-2VTE-YRRN. [DOI] [PubMed] [Google Scholar]
- 10.Mackenbach JP, Kunst AE. Measuring the magnitude of socioeconomic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44:757–71. doi: 10.1016/S0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- 11.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 12.Kunitz SJ. Sex, race and social role—history and the social determinants of health. Int J Epidemiol. 2007;36:3–10. doi: 10.1093/ije/dyl296. [DOI] [PubMed] [Google Scholar]
- 13.World Cancer Research Fund and American Institute for Cancer Research (aicr) Policy and Action for Cancer Prevention. Food, Nutrition, and Physical Activity: A Global Perspective. Washington DC: AICR; 2009. [Google Scholar]
- 14.Health Canada. Home > Health Concerns > Tobacco > Research > Tobacco Use Statistics > Canadian Tobacco Use Monitoring Survey (CTUMS) Ottawa, ON: Health Canada; 2011. Summary of Annual Results for 2010 [Web page] [Available online at: http://www.hc-sc.gc.ca/hc-ps/tobac-tabac/research-recherche/stat/_ctums-esutc_2010/ann_summarysommaire-eng.php; cited March 1, 2012] [Google Scholar]
- 15.Centers for Disease Control and Prevention Cigarette smoking among adults—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57:1221–6. [Erratum in: MMWR Morb Mortal Wkly Rep 2008;57:1281] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention Vital signs: current cigarette smoking among adults aged ≥ 18 years— United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1135–40. [PubMed] [Google Scholar]
- 17.Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in nhis 2000. Am J Public Health. 2004;94:269–78. doi: 10.2105/AJPH.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006;7:149–56. doi: 10.1016/S1470-2045(06)70577-0. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization (who) Global Status Report on Alcohol 2004. Geneva, Switzerland: WHO; 2004. [Google Scholar]
- 20.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 21.van Oers JA, Bongers IM, van de Goor LA, Garretsen HF. Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol. 1999;34:78–88. doi: 10.1093/alcalc/34.1.78. [DOI] [PubMed] [Google Scholar]
- 22.International Agency for Cancer Research (iarc) Fruit and Vegetables. Vol. 8. Lyon, France: IARC Press; 2003. iarc Handbooks of Cancer Prevention. [Google Scholar]
- 23.Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M, on behalf of the Comparative Risk Assessment Collaborating Group (Cancers) Causes of cancer in the world: comparative risk assessment of nine behavioral and environmental risk factors. Lancet. 2005;366:1784–93. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- 24.Public Health Agency of Canada (phac) Home > Health Promotion > Population Health > Investing In Prevention—The Economic Perspective [Web page] Ottawa, ON: PHAC; 2010. [Available at: http://www.phac-aspc.gc.ca/ph-sp/preveco-02-eng.php; cited March 1, 2012] [Google Scholar]
- 25.Wynne A, Currie CL. Social exclusion as an underlying determinant of sexually transmitted infections among Canadian Aboriginals. Pimatisiwin. 2011;9:113–27. [Available online at: http://www.pimatisiwin.com/online/wp-content/uploads/2011/08/06WynneCurrie.pdf; cited March 1, 2012] [Google Scholar]
- 26.Woodward A, Boffetta P. Environmental exposure, social class, and cancer risk Chapter 18. In: Kogevinas M, Pearce N, Susser M, Boffetta P, editors. Cancer Epidemiology—Social Inequalities and Cancer. Lyon, France: IARC Press; 1997. pp. 361–7. iarc Scientific Publications, no. 138. [PubMed] [Google Scholar]
- 27.Maddison AR, Asada Y, Urquhart R. Inequity in access to cancer care: a review of the Canadian literature. Cancer Causes Control. 2011;22:359–66. doi: 10.1007/s10552-010-9722-3. [DOI] [PubMed] [Google Scholar]
- 28.Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc Sci Med. 2002;54:1621–35. doi: 10.1016/S0277-9536(01)00331-8. [DOI] [PubMed] [Google Scholar]
- 29.Macintyre S, McKay L, Der G, Hiscock R. Socio-economic position and health: what you observe depends on how you measure it. J Public Health Med. 2003;25:288–94. doi: 10.1093/pubmed/fdg089. [DOI] [PubMed] [Google Scholar]
- 30.Mackenbach JP, Kunst AE, Cavelaars AE, Groenhof F, Geurts JJ. Socioeconomic inequalities in morbidity and mortality in western Europe. The EU Working Group on Socioeconomic Inequalities in Health. Lancet. 1997;349:1655–9. doi: 10.1016/S0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- 31.Standing Senate Committee on Social Affairs, Science and Technology. A Healthy, Productive Canada: A Determinant of Health Approach. Ottawa, ON: The Senate of Canada; 2009. Final Report of the Senate Subcommittee on Population Health. [Google Scholar]
- 32.Canadian Council on Social Development. Poverty Statistics [Web page] Ottawa, ON: Canadian Council on Social Development; 2002. [Available online at: http://www.ccsd.ca/factsheets/fs_pov9099.htm; cited March 1, 2012] [Google Scholar]
- 33.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–98. doi: 10.1161/01.CIR.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 34.The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academy Press; 2002. Committee on Assuring the Health of the Public in the 21st Century. Understanding population health and it determinants. Chapter 2. [Available online at: http://www.nap.edu/openbook.php?record_id=10548&page=46; cited March 1, 2012] [Google Scholar]
- 35.Canadian Institute for Health Information (cihi) How Healthy Are Rural Canadians? An Assessment of Their Health Status and Health Determinants. Ottawa, ON: CIHI; 2006. [Available online at: http://www.phac-aspc.gc.ca/publicat/rural06/pdf/rural_canadians_2006_report_e.pdf; cited March 1, 2012] [Google Scholar]
- 36.Kondro W. Health of rural Canadians lags behind urban counterparts. CMAJ. 2006;175:1195. doi: 10.1503/cmaj.061306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reid–Arndt SA, Cox CR. Does rurality affect quality of life following treatment for breast cancer? J Rural Health. 2010;26:402–5. doi: 10.1111/j.1748-0361.2010.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hegney D, Pearce S, Rogers–Clark C, Martin–McDonald K, Buikstra E. Close, but still too far. The experience of Australian people with cancer commuting from a regional to a capital city for radiotherapy treatment. Eur J Cancer Care (Engl) 2005;14:75–82. doi: 10.1111/j.1365-2354.2005.00525.x. [DOI] [PubMed] [Google Scholar]
- 39.Bjorklund RW, Pippard JL. The mental health consumer movement: implications for rural practice. Community Ment Health J. 1999;35:347–59. doi: 10.1023/A:1018714024063. [DOI] [PubMed] [Google Scholar]
- 40.Rogers–Clark C. Living with breast cancer: the influence of rurality on women’s suffering and resilience, a postmodern feminist inquiry. Aust J Adv Nurs. 2002;20:34–9. [PubMed] [Google Scholar]
- 41.Marrett LD, Jones CR, Wishart K. First Nations Cancer Research and Surveillance Priorities for Canada. Workshop Report; September 23–24, 2003; Ottawa, Ontario. Ottawa, ON: Cancer Care Ontario; 2004. [Available online at: https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=13688; cited March 1, 2012] [Google Scholar]
- 42.Cancer Care Ontario (cco) Surveillance and Aboriginal Cancer Care Units. Toronto, ON: CCO; 2007. [Google Scholar]
- 43.Statistics Canada. Home > Census > 2006 Census: Analysis series > Findings > 2006 Census: Immigration in Canada: A Portrait of the Foreign-born Population, 2006 Census: Highlights [Web page] Ottawa, ON: Statistics Canada; n.d. [Available online at: http://www12.statcan.ca/census-recensement/2006/as-sa/97-557/p1-eng.cfm; cited March 1, 2012] [Google Scholar]
- 44.Palaty C, on behalf of the Planning Committee of the National Forum . Cancer Care for All Canadians: Improving Access and Minimizing Disparities for Vulnerable Populations in Canada. Vancouver, BC: BC Cancer Agency; 2007. [Google Scholar]
- 45.Spitzer DL. Engendering health disparities. Can J Public Health. 2005;96(suppl 2):S78–96. doi: 10.1007/BF03403704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Doyal L. Gender equity in health: debates and dilemmas. Soc Sci Med. 2000;51:931–9. doi: 10.1016/S0277-9536(00)00072-1. [DOI] [PubMed] [Google Scholar]
- 47.Moss NE. Gender equity and socioeconomic inequality: a framework for the patterning of women’s health. Soc Sci Med. 2002;54:649–61. doi: 10.1016/S0277-9536(01)00115-0. [DOI] [PubMed] [Google Scholar]
- 48.Betancourt JR. Cultural competency: providing quality care to diverse populations. Consult Pharm. 2006;21:988–95. doi: 10.4140/TCP.n.2006.988. [DOI] [PubMed] [Google Scholar]
- 49.Kagawa-Singer M, Kassim–Lakha S. A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes. Acad Med. 2003;78:577–87. doi: 10.1097/00001888-200306000-00006. [DOI] [PubMed] [Google Scholar]