Abstract
Extramammary Paget disease (empd) is a relatively rare cutaneous disorder described as an apocrine gland tumour occurring in both a benign and a malignant form with metastatic potential. The areas of the body affected are the vulva, perianal region, penis, scrotum, perineum, and axilla, all of which contain apocrine glands. When empd affects the perianal region, it is called perianal Paget disease (ppd). All forms of empd, including ppd, are typically treated by wide surgical excision. Perianal Paget disease usually occurs later in life in patients who are often poor surgical candidates, but the available literature is scarce regarding other treatment modalities, including definitive radiotherapy. We contend that ppd can be safely and effectively treated with radiotherapy, and here, we present the case of a 75-year-old woman with ppd who was successfully so treated. A brief review of the literature concerning the diagnosis, natural history, and treatment of ppd is also included.
Keywords: Perianal Paget disease, extramammary Paget disease, radiotherapy
1. CASE DESCRIPTION
A 75-year-old white woman presented in 2001 with a history of several years of perianal irritation. The affected area was biopsied on several occasions, demonstrating pagetoid cells that were periodic acid–Schiff–positive, human melanoma black-45–negative, and cytokeratin high, with low positive material in the epidermis, consistent with extramammary Paget disease. The cells were also positive for carcinoembryonic antigen.
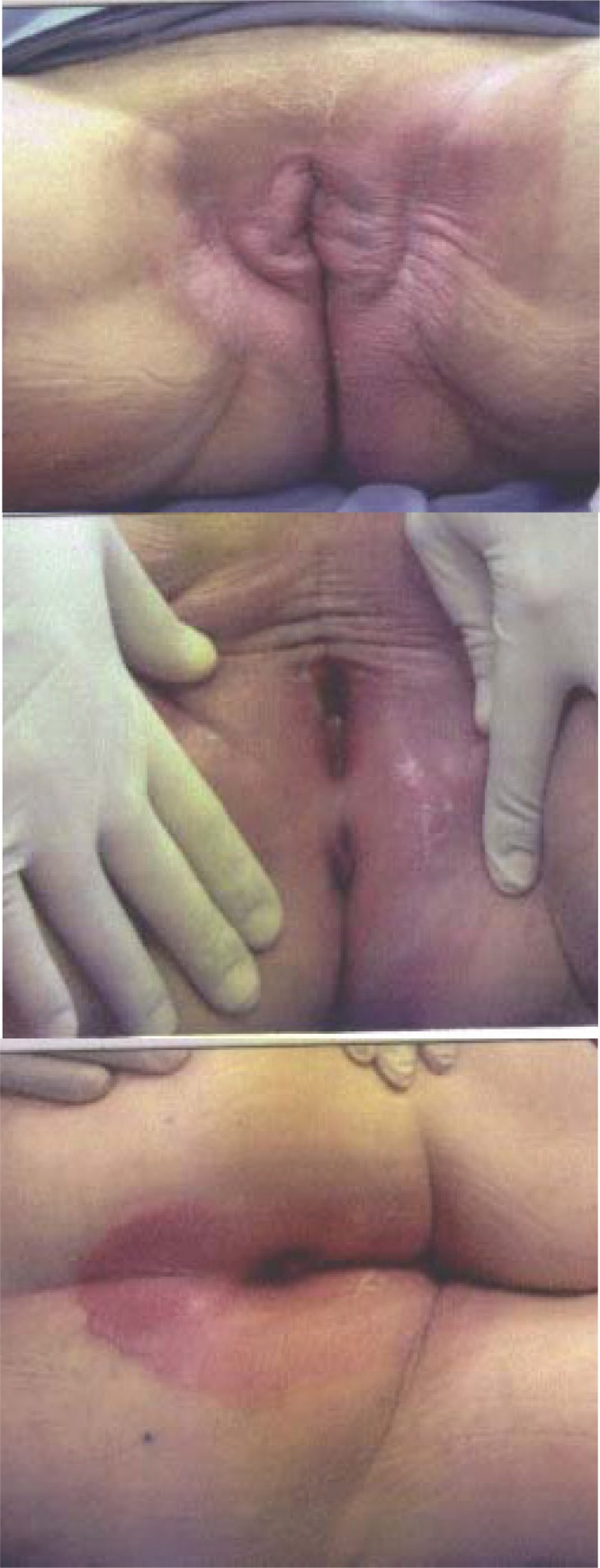
The affected area included the vulva, perineum, and intergluteal region. Despite topical application of steroids and fluorouracil creams, the patient continued to complain of excoriations, itching, and occasional pain. On clinical examination, the affected region showed thick, purplish, erythematous skin with areas of whitish discharge and raised edges, particularly at the junction between the perineum and the left thigh (Figure 1). There was no evidence of an underlying adnexal or rectal carcinoma, nor any lymphadenopathy in the groin region. A complete blood count, biochemical profile, and chest radiograph were unremarkable.
FIGURE 1.
Extensive perianal Paget’s disease in the perineum.
The patient was treated with a course of definitive electron-beam radiation therapy. Because of the extent of disease, the region was divided into two compartments and treated sequentially, without a treatment interruption. The anterior component, which was treated first, included the vulvovaginal area and anterior parts of the perineum. The posterior component—which was treated sequentially with the patient in a prone position—included the posterior perineum and the intergluteal and perianal regions. The match line of the two areas was carefully demarcated using tattoos. The cumulative dose was 6400 cGy delivered in 200 cGy fractions over 6.5 weeks. The treatment was well tolerated, with no need for major interruptions.
An early response was observed by the 4th week (Figure 2). This response was coupled with subjective improvement in the itching and disappearance of the excoriations. The response has been durable, with no evidence of recurrence at 5 years. However, with further follow-up, subcutaneous fibrosis and telangiectasia increased in a way more appreciated in this patient than in any other patient treated for skin cancer with a similar dose regimen (Figure 3). These side effects did not affect the patient’s quality of life.
FIGURE 2.
Early response observed by the 4th week on radiotherapy.
FIGURE 3.
(A,B) Complete regression at 5 years post radiotherapy, with notable telangiectasia and fibrosis.
2. DISCUSSION
Extramammary Paget disease (empd) is a rare cutaneous adenocarcinoma described as an apocrine gland tumour occurring in both a benign and a malignant form, with metastatic potential1. The areas of the body affected—vulva, perianal region, penis, scrotum, perineum, and axilla—generally contain large concentrations of apocrine glands. Sir James Paget first described intraepithelial carcinoma of the breast in 1874 and suggested that the disease might also be found in other areas2. The first case of empd was described by Crocker in 1888, and perianal empd—also called perianal Paget disease (ppd)—was first reported in 1893 by Darier and Coulillaud3. The most thorough literature search (conducted by Brown et al. in 2002) found 141 papers reporting a total of 279 cases of ppd in some form4.
Perianal Paget disease occurs more commonly in women and usually begins in or after the 5th decade5. In contrast to Paget disease of the nipple, which is commonly associated with an underlying ductal carcinoma, ppd is associated with subjacent or visceral primary malignancies (mainly of the rectum, cervix, or urethra) in only 20% of patients who present with the condition, and yet histologically, the two diseases are identical1. Of patients with empd, 24% have an associated underlying adnexal adenocarcinoma, which has been associated with a worse prognosis, with mortality rates up to 46% being reported6. Up to 12% of patients with empd have a concurrent internal malignancy that may be located nearby, and this incidence has been found to be greatest in patients with ppd6,7.
Patients with ppd tend to present with nonspecific symptoms such as pruritus ani, excoriation, pain with defecation, and bleeding. The clinical appearance is that of an erythematous plaque containing de-pigmented, crusted, or scaly areas which may weep fluid. The size of the plaque may range from less than 1 cm to much larger lesions encompassing the entire anogenital region. The margins of the region are usually well demarcated, slightly raised and erythematous, resembling contact dermatitis, eczema, or even a bacterial infection. Leukoplakia-like patches may develop in some patients. The duration of symptoms can be long, as demonstrated by this case. A history of multiple unsuccessful attempts at dermatologic treatment is usually present.
Microscopically, ppd is characterized by large basophilic or vacuolated cells in the epidermis. With their high mucin content, the Paget cells stain positively for acid and neutral mucopolysaccharides, and they may contain melanin granules5. They also contain low molecular weight cytokeratins and carcinoembryonic antigen, which can be identified using immunofluorescence or immunohistochemistry8.
Most dermatology textbooks recommend surgical excision as the “gold standard.” The recommended approaches are, for noninvasive lesions, extended surgical excision and, for invasive disease or lesions associated with an adnexal carcinoma, abdominoperineal excision or excision of rectum9. Primary treatment with radiation therapy is seldom used. Some authors have demonstrated results with topical imiquimod cream, but most consider wide surgical excision to be the treatment of choice. Indeed, some authors believe that radiotherapy has no role in the management of ppd because of high recurrence rates10. Wide local excision is often disfiguring and requires subsequent reconstruction of the tissue defect, a process that is prone to postoperative complications. Elderly patients, who are often undesirable surgical candidates, may benefit from primary radiotherapy as an alternative. Typically, the side effects from perianal radiotherapy include acute dermatitis, moist desquamation, and mild-to-late skin atrophy, all of which are manageable with moisturizing creams.
Historically, the few reports of radiotherapy treatment for ppd lack adequate descriptions of the radiation sources, fields, doses, fractionation schedules, and treatment outcomes, making decision rationales difficult. However, more detailed cases of successful treatment with radiotherapy have recently been published4,5,11–18. Several investigators have made a strong case for the use of primary radiotherapy for curative intent in patients not considered suitable for surgery, and for the use of postoperative radiotherapy after resection4,5,11. Besa et al.11 observed a 36%–66% rate of positive margins after surgical excision alone in their series of 65 patients with empd of the perineal skin, and the actuarial local recurrence rate for patients treated with surgery was 40% within 5 years. They also noted the limited ability of surgery to adequately control a multicentric widespread process and the likelihood of surgery to be associated with considerable morbidity or functional impairment. Brown et al.4 suggested that, in cases in which surgery for ppd would result in significant loss of function (abdominoperineal resection and colostomy formation), keeping surgery as salvage treatment for cases of radiotherapy failure would seem an acceptable alternative. We agree with their view that radiotherapy should be considered an acceptable alternative to surgery for ppd, as in the case reported here, whether as primary treatment or after a surgical relapse. Table i reviews the literature for cases of ppd treated by radiotherapy in which dosage, modality, and outcome were described.
TABLE I.
Radiotherapy for perianal Paget disease (ppd)
| Reference |
Patient
|
History | Treatment type | Dose/fractions | Modality | Outcome | |
|---|---|---|---|---|---|---|---|
| Age | Sex | ||||||
| Lock et al., 197717 | 85 | Female | ppd 11×5 cm | Primary | 14.4 Gy/12 | Neutrons | No recurrence at 23 months |
| Secco et al., 198416 | 85 | Male | Chemoradiation | Primary | 30 Gy/15 | — | No recurrence at 30 months |
| Jensen et al., 198815 | — | — | — | — | 30 Gy | — | Local recurrence at 6 months |
| Thirlby et al., 199014 | 69 | Male | Incomplete resection and chemoradiation | Primary | 50 Gy/25 | 20 MeV electrons | No recurrence at 14 months |
| Brierley and Stockdale, 199112 | 76 | Female | — | Primary | 54 Gy/12 | 11 MeV electrons | No recurrence, died 13 months post rt |
| 84 | Female | — | Primary | 50 Gy/25 | 100 kV X-rays | No recurrence at 31 months | |
| Besa et al., 199211 | 72 | Female | ppd 4.5 cm | Primary | 56 Gy/28 | 60Co γ-rays | No recurrence at 21 months |
| Goldman et al., 199213 | 75 | Male | ppd 3×3.5 cm, incomplete excision | Adjuvant | 66 Gy/33 | — | No recurrence at 16 months |
| Amin, 19995 | 71 | Male | ppd 13×12 cm, 4 prior partial excisions | Recurrence | 50 Gy/10 | 300 kV X-rays | No recurrence at 10 years |
| Velenik et al., 200818 | 80 | Female | ppd 8×5 cm | Primary | 45 Gy/15 | 80 kV X-rays | No recurrence at 28 months |
rt = radiotherapy.
Most authors have reported using a photon or electron field directed to the affected region of the perineum to achieve local control. We chose to use electron beam for the purpose of sparing the deeper tissues, given that only superficial tissues were at risk. Based on their experience of 12 cases, Besa et al.11 recommended a dose of more than 50 Gy using a single appositional field for the treatment of empd. Based on experience with other types of adenocarcinoma (such as postoperative breast radiotherapy after complete tumour excision), Brown et al.4 also suggested that 50 Gy is likely the minimum dose required to eradicate microscopic disease. The patient described in the present report received 64 Gy to the affected areas. At 5-years of follow-up, the patient has shown acceptable radiation sequelae, with no loss of anal sphincter function—a side effect that often occurs with wide surgical excision in this region. The most notable radiation sequelae are cosmetic, consisting of a prominent telangiectasia and fibrosis in the area of the radiation field.
3. SUMMARY
Perianal Paget disease is a rare condition and remains a therapeutic challenge for clinicians. No randomized trials have yet been performed comparing surgical excision and radiation therapy. The previous reports that did include radiotherapy poorly described the technical details and outcome of treatment. We hope that by sharing our experience, radiotherapy will be seen to be an effective treatment modality in the treatment of ppd and an acceptable alternative to wide surgical excision in select patients.
4. ACKNOWLEDGMENT
We thank Mathew Dinzey for preparation of the photographs.
5. CONFLICT OF INTEREST DISCLOSURES
The authors have no financial conflicts of interest to declare.
6. REFERENCES
- 1.Merot Y, Mazoujian G, Pinkus G, Momtaz-T K, Murphy GF. Extramammary Paget’s disease of the perianal and perineal regions. Evidence of apocrine derivation. Arch Dermatol. 1985;121:750–2. doi: 10.1001/archderm.1985.01660060064022. [DOI] [PubMed] [Google Scholar]
- 2.Paget J. On disease of the mammary areola preceding cancer of the mammary gland. St Bartholomew’s Hospital Report. 1874;10:87–9. [Google Scholar]
- 3.Darier J, Coulillaud P. Concerning a case of Paget disease of the perineal and scrotal area [French] Ann Dermatol Syphiligr (Paris) 1893;4:25–33. [Google Scholar]
- 4.Brown RS, Lankester KJ, McCormack M, Power DA, Spittle MF. Radiotherapy for perianal Paget’s disease. Clin Oncol (R Coll Radiol) 2002;14:272–84. doi: 10.1053/clon.2002.0092. [DOI] [PubMed] [Google Scholar]
- 5.Amin R. Perianal Paget’s disease. Br J Radiol. 1999;72:610–12. doi: 10.1259/bjr.72.858.10560346. [DOI] [PubMed] [Google Scholar]
- 6.Chanda JJ. Extramammary Paget’s disease: prognosis and relationship to internal malignancy. J Am Acad Dermatol. 1985;13:1009–14. doi: 10.1016/S0190-9622(85)70254-X. [DOI] [PubMed] [Google Scholar]
- 7.Helwig EB, Graham JH. Anogenital (extramammary) Paget’s disease. A clinicopathological study. Cancer. 1963;16:387–403. doi: 10.1002/1097-0142(196303)16:3<387::AID-CNCR2820160314>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 8.Beck DE, Fazio VW. Perianal Paget’s disease. Dis Colon Rectum. 1987;30:263–6. doi: 10.1007/BF02556169. [DOI] [PubMed] [Google Scholar]
- 9.Coldiron BM, Goldsmith BA, Robinson JK. Surgical treatment of extramammary Paget’s disease. A report of six cases and a reexamination of Mohs micrographic surgery compared with conventional surgical excision. Cancer. 1991;67:933–8. doi: 10.1002/1097-0142(19910215)67:4<933::AID-CNCR2820670413>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 10.Butler JD, Hersham MJ, Wilson CA, Bryson JR. Perianal Paget’s disease. J Royal Soc Med. 1997;90:688–9. doi: 10.1177/014107689709001217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Besa P, Rich TA, Delclos L, Edwards CL, Ota DM, Wharton JT. Extramammary Paget’s disease of the perineal skin: role of radiotherapy. Int J Radiat Oncol Biol Phys. 1992;24:73–8. doi: 10.1016/0360-3016(92)91024-H. [DOI] [PubMed] [Google Scholar]
- 12.Brierley JD, Stockdale AD. Radiotherapy: an effective treatment for extramammary Paget’s disease. Clin Oncol (R Coll Radiol) 1991;3:3–5. doi: 10.1016/S0936-6555(05)81030-1. [DOI] [PubMed] [Google Scholar]
- 13.Goldman S, Ihre T, Lagerstedt U, Svensson C. Perianal Paget’s disease: report of five cases. Int J Colorect Dis. 1992;7:167–9. doi: 10.1007/BF00360360. [DOI] [PubMed] [Google Scholar]
- 14.Thirlby RC, Hammer CJ, Jr, Galagan KA, Travaglini JJ, Picozzi VJ., Jr Perianal Paget’s disease: successful treatment with combined chemoradiotherapy. Report of a case. Dis Colon Rectum. 1990;33:150–2. doi: 10.1007/BF02055547. [DOI] [PubMed] [Google Scholar]
- 15.Jensen SL, Sjølin KE, Shokouh–Amiri MH, Hagen K, Harling H. Paget’s disease of the anal margin. Br J Surg. 1988;75:1089–92. doi: 10.1002/bjs.1800751113. [DOI] [PubMed] [Google Scholar]
- 16.Secco GB, Lapertosa G, Sertoli MR, Scarpati D, Riboli EB. Perianal Paget’s disease: case report of an elderly patient treated with polychemotherapy and radiotherapy. Tumori. 1984;70:381–3. doi: 10.1177/030089168407000414. [DOI] [PubMed] [Google Scholar]
- 17.Lock MR, Katz DR, Parks A, Thomson JP. Perianal Paget’s disease. Postgrad Med J. 1977;53:768–72. doi: 10.1136/pgmj.53.626.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Velenik V, Segedin B, Anderluh F, Oblak I, Strojan P. Radiotherapy for perianal Paget’s disease: a case report. Tumori. 2008;94:750–3. doi: 10.1177/030089160809400520. [DOI] [PubMed] [Google Scholar]